Abstract
Objective
To determine if adjusted mortality, walking ability or return home differed after hip fracture surgery between Canada and the USA.
Design
Secondary analysis of the Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair (FOCUS) trial data.
Setting
Data were collected from 47 American and Canadian hospitals.
Participants
Overall, 2016 subjects with a hip fracture (USA = 1222 (60.6%); Canada = 794 (39.4%)) were randomized to a liberal or restrictive transfusion strategy. Subjects were 50 years and older, with cardiovascular disease and/or risk factors and hemoglobin <100 g/L within 3 days post-surgery. The average age was 82 years and 1527(76%) subjects were females.
Intervention
Demographics, health status and health services data were collected up to 60 days post-surgery and mortality to a median of 3 years post-surgery.
Main outcomes
Mortality, inability to walk and return home.
Results
US subjects had higher adjusted mortality than Canadians at 30 days (odds ratio = 1.78; 95% confidence interval: 1.09–2.90), 60 days (1.53; 1.02–2.29) and up to 3 years (hazard ratio = 1.25; 1.07–1.45). There were no differences in adjusted outcomes for walking ability or return home at 30 or 60 days post-surgery. Median hospital length of stay was longer (P < 0.0001) in Canada (9 days; interquartile range: 5–18 days) than the US (3 days; 2–5 days). US subjects (52.9%) were more likely than Canadians (16.8%) to be discharged to nursing homes for rehabilitation (P < 0.001).
Conclusions
Adjusted survival favored Canadians post hip fracture while walking ability and return home were not different between countries. The reason(s) for mortality differences warrant further investigation.
Keywords: hip fracture, health services, mortality, patient outcomes
Introduction
There are many medical treatment similarities between Canada and the United States (US), especially in those requiring technical expertise in surgical care. However, patients are managed differently post-surgically, due, at least in part, to the fact that health-care coverage differs substantially between countries with Canada providing universal health insurance coverage and the USA providing a mix of private, for-profit and non-profit, and public care with variable individual coverage. There is much recent interest in comparing patient outcomes and health service variation across health systems internationally [1–7]. Most research to date comparing international outcomes for conditions such as hip fracture have used administrative databases or retrospective review of hospital records [3, 6, 7]. While these data are often population-based, they may be limited in their ability to adjust for diverse case-mix [8] including pre-fracture status, living arrangements and comorbidities (including dementia) and frequently only measure mortality rather than outcomes such as the ability to walk or return home after a hip fracture. Prospectively collected data provide higher quality measures to compare these additional patient outcomes between the two countries.
As hip fracture is one of the most common reasons for injury-related hospitalization of older persons [9–12], and is associated with high morbidity and mortality [13–15], it is an excellent clinical model to compare outcomes between countries. Between 19 July 2004 and 28 February 2009, we performed a randomized controlled trial with the primary aim of comparing two transfusion thresholds (80 vs. 100 g/L) in hip fracture patients in the USA and Canada [16]. These data allowed cross-country comparison of patient outcomes and health-care delivery at 30 and 60 days postoperatively as well as longer-term mortality at a median of 3 years after hip fracture [17].
The main objectives of this secondary analysis of the Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair (FOCUS) trial data were to compare, after adjustments for case-mix measures, USA and Canadian subjects’ outcomes including short- and long-term mortality, inability to walk independently and return home. We also evaluated acute care health services delivery in both countries.
Methods
We performed an exploratory, secondary analysis of data from 2016 subjects enrolled in the FOCUS trial. FOCUS was a randomized controlled trial designed to evaluate the effect of red blood cell transfusion strategies on mortality, function and morbidity in patients with cardiovascular disease or risk factors who underwent surgery for hip fracture. The methods and results have been published previously [16–18].
FOCUS trial
Subjects were recruited between 2004 and 2009 at 47 participating USA and Canadian clinical centers. We enrolled subjects who were 50 years and older with a hip fracture and cardiovascular disease or cardiovascular risk factors with hemoglobin concentration <100 g/L within 3 days following surgical repair. Subjects were randomized to a liberal or restrictive transfusion strategy. The following baseline characteristics and medical history were collected by research staff during hospitalization: age; sex; pre-admission residence; histories of: coronary artery disease, congestive heart failure, hypertension, peripheral vascular disease, cerebrovascular disease, kidney disease, diabetes mellitus, dementia and the American Society of Anesthesiology (ASA) risk score as a measure of pre-operative sickness. Surgical procedure used to repair the hip was recorded as was anesthesia type. Surgical hospital length of stay (LOS) was determined from the time of randomization (within 3 days of surgery) to a maximum of 30 days post-randomization. Discharge destination was recorded at discharge from the surgical hospital. Mortality, inability to ambulate across a room (10 feet or 3.01 m) without human assistance (with/without an assistive device), and return to home (for those admitted from the community) were ascertained via telephone query at the 30 and 60 days follow-up time points. As an ancillary study to FOCUS, long-term mortality was ascertained by linking the study patients to national death registries in the USA (National Center for Health Statistics National Death Index (NDI)) and Canada (Statistics Canada Mortality Database (CMDB)) at a median of 3 years after hip fracture [17]. Outcomes were ascertained on 1999 (99%) of subjects.
Current analysis
Baseline characteristics and health services delivery were compared between US and Canadian subjects using chi-square statistics for categorical variables and t-tests for continuous variables. For health services, we evaluated surgical fixation, anesthetic type, surgical hospital LOS (following study randomization) and discharge destination from the surgical hospital (within 30 days of randomization). Discharge destination was not synonymous with return to home at 30 and 60 days, but rather, reflected the destination of the patient at the time of discharge from the surgical hospital (i.e. may include rehabilitation, skilled nursing facilities or other in-patient care settings as well as return directly home). Because LOS and discharge destinations are mediated by the organization of health-care services within each country, they were not included as covariates in the adjusted outcome analyses. The relationship between potential confounding variables, identified a-priori as: age, sex, race, nursing home residence prior to hospitalization, dementia, cardiovascular disease or risk factors, diabetes, kidney disease, cancer and ASA risk score, and each of the study outcomes, were examined. ASA risk scores of one (lowest risk) and two were combined into a single category as there were very few subjects with a score of one.
Unadjusted odds ratios for USA compared to Canadian subjects were determined for each of these primary outcomes (mortality; a composite outcome of inability to walk/death; and return home) at 30 and 60 days post-randomization. Return to home reflected the current residence of the patient at 30 and 60 days post-randomization (i.e. after discharge from rehabilitation hospitals, etc.). Those subjects who were in a nursing home at the time of the hip fracture were excluded from the residence at 30 and 60 days analysis as there was no expectation that these individuals would return to the community.
Logistic regression modeling determined association of country with outcome measures, with adjustment for potential confounding using the variables defined a-priori as described previously. The model for each outcome included country and allowed stepwise selection of the candidate variables (P ≤0.05 for both entry and to remain). As this was an exploratory analysis, stepwise selection was used to balance the trade-offs among over-fitting, missing signal and leading the direction of the model. Candidate variables for the stepwise models were defined as the potential confounders that were statistically associated (P < 0.05) with outcome in unadjusted comparisons. In addition, we included the trial randomization allocation in all adjusted models. Thus, although all models started with the same set of potential candidate variables, only those that were statistically associated with the outcome were retained in the final models for each outcome.
Cox proportional hazards modeling determined the association of country with long-term survival. Proportional hazards survival functions that were direct adjusted to the overall means of covariates in the model across both countries were produced for the USA and Canada. Finally, we also evaluated the nested effect of centers within countries, which did not affect results (nor were nested centers significantly associated with outcomes), so these models were not reported. Sample size was determined based on the primary outcome in the trial [16]. All analyses were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC).
Results
There were 1 222 (60.6%) subjects enrolled in the USA and 794 (39.4%) in Canada. At baseline, subjects in the USA were less likely to have dementia (USA: 25.1%; Canada: 41.4%), cerebrovascular disease (USA: 19.0%; Canada: 29.0%), and to reside in nursing homes prior to their hip fracture (USA: 7.6%; Canada 15.3%). More US subjects were males (USA: 25.9%; Canada: 21.8%), had kidney disease (USA: 9.9%; Canada: 6.2%), and had a history of cancer (USA: 20.1%; Canada: 15.8%). No other significant differences were noted between US and Canadian subjects (Table 1).
Table 1.
Country comparison of baseline participant characteristics
| United States, N = 1222 | Canada, N = 794 | ||
|---|---|---|---|
| n (%) | n (%) | P valuea,b | |
| Liberal treatment arm | 609 (49.8) | 398 (50.1) | 0.93 |
| Male | 316 (25.9) | 173 (21.8) | 0.04 |
| White race | 1120 (91.7) | 771 (97.1) | <0.001 |
| Age (mean years)b | 81.1 ± 9.3 | 82.3 ± 8.2 | 0.002 |
| Nursing home prior to admission | 93 (7.6) | 121 (15.3) | <0.001 |
| Comorbidities | |||
| Coronary artery disease | 505 (41.3) | 300 (37.8) | 0.11 |
| Congestive heart failure | 222 (18.2) | 129 (16.2) | 0.28 |
| Peripheral vascular disease | 140 (11.5) | 79 (9.9) | 0.31 |
| Cerebrovascular disease | 243 (19.0) | 230 (29.0) | <0.001 |
| Treated hypertension | 1003/1215 (82.6) | 642/793 (81.0) | 0.37 |
| Treated diabetes | 329/1215 (27.1) | 179/793 (22.6) | 0.02 |
| Treated hypercholesterolemia | 516/1210 (42.6) | 191/793 (24.1) | <0.001 |
| Current smoker | 135/1214 (11.1) | 94/793 (11.9) | 0.62 |
| Creatinine > 2.0 | 120/1213 (9.9) | 49/791 (6.2) | 0.004 |
| Chronic lung disease | 215/1218 (17.7) | 162/792 (20.4) | 0.13 |
| History of dementia | 306/1220 (25.1) | 328/792 (41.4) | <0.001 |
| History of cancer | 245/1219 (20.1) | 125/792 (15.8) | 0.02 |
| Type of fracturec | |||
| Femoral neck | 507/1220 (41.6) | 347/792 (43.8) | 0.33 |
| Intertrochanteric | 665/1220 (54.5) | 369/792 (46.6) | <0.001 |
| Subtrochanteric | 79/1220 (6.5) | 104/792 (13.1) | <0.001 |
| Reverse oblique | 13/1220 (1.1) | 8/792 (1.0) | 1.00 |
| American Society of Anesthesiologists risk score | 0.07 | ||
| 1 and 2 combined | 204/1193 (17.1) | 158/746 (21.2) | |
| 3 | 830/1193 (69.6) | 488/746 (65.4) | |
| 4 | 159/1193 (13.3) | 100/746 (13.4) | |
aFisher's exact or chi square tests for categorical variables.
bPlus–minus values are means ± SD, Student’s t test P-value.
cPatients may have had more than one type of fracture.
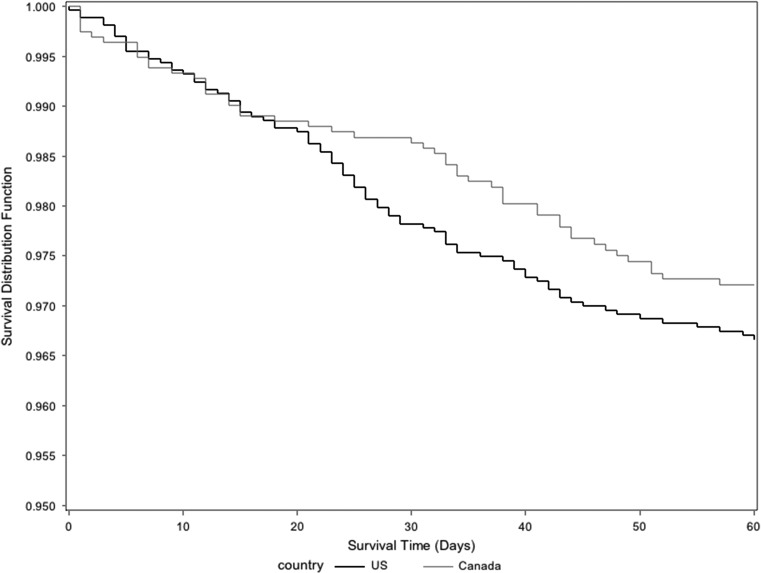
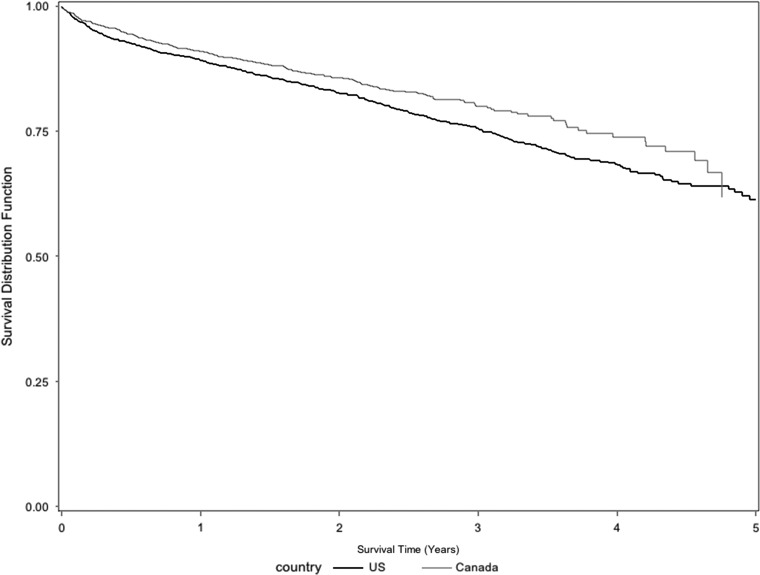
Table 2 reports the unadjusted and adjusted analyses. Country was not significantly associated with mortality at any of the evaluation time periods (USA compared to Canada) in the unadjusted analyses. However, country was significantly associated with mortality at 30 days (USA compared to Canada: odds ratio = 1.78; 95% confidence interval: 1.09–2.90) and at 60 days (USA compared to Canada: odds ratio = 1.53; 95% confidence interval: 1.02–2.29) after adjustment for confounders. Examination of the adjusted survival plots (Figs 1 and 2) demonstrated similar survival until 20 days; after 20 days, the rate of survival favored subjects in Canada out to 3 years (USA compared to Canada: hazard ratio = 1.25; 95% confidence interval: 1.07–1.45). Very few subjects were followed after 4 years in Canada, so the survival estimates for these time points are not very reliable in Canadian subjects as can be seen by the large drops in survival curves at single time points.
Table 2.
Country comparison of unadjusted and adjusted non-mortality and mortality outcomes
| United States, N = 1222 | Canada, N = 794 | |||||
|---|---|---|---|---|---|---|
| n (%) | n (%) | Unadjusted OR (95% CI) | Adjusted odds ratioa (95% CI) | |||
| Short term | ||||||
| Death | ||||||
| At 30 days | 62/1209 (5.1) | 33/786 (4.2) | 1.23 (0.80, 1.90) | 1.78 (1.09, 2.90) | ||
| At 60 days | 89/1212 (7.3) | 53/787 (6.7) | 1.10 (0.77, 1.56) | 1.53 (1.02, 2.27) | ||
| Not walking/death | ||||||
| At 30 days | 546/1209 (45.2) | 394/786 (50.1) | 0.82 (0.68, 0.98) | 1.04 (0.85, 1.28) | ||
| At 60 days | 407/1212 (33.6) | 291/787 (37.0) | 0.86 (0.71, 1.04) | 1.17 (0.94, 1.46) | ||
| Home | ||||||
| At 30 daysb | 552/1115 (49.5) | 305/667 (45.7) | 1.16 (0.96, 1.41) | 1.06 (0.86, 1.31) | ||
| At 60 daysb | 759/1119 (67.8) | 427/664 (64.3) | 1.17 (0.96, 1.43) | 1.04 (0.84, 1.30) | ||
| Long term | ||||||
| United Statesb N = 1213 | Canadac, N = 789 | |||||
| Deaths/person years follow-up | Deaths/person years follow-up | Unadjusted HR (95% CI) | Adjusted hazards ratio (95% CI) | |||
| Mortality | 552/3013 | 289/1586 | 1.04 (0.91, 1.21) | 1.25 (1.07,1.45) | ||
aDeath at 30 days adjusted for sex, age, admitted from a nursing home, creatinine > 2.0, dementia and ASA rating.
Note that the presence of cerebrovascular disease was not significant in the 30-day univariate/adjusted stepwise multivariate analysis and thus, was not included in the final adjusted model.
Death at 60 days adjusted for sex, age, admitted from a nursing home, cerebrovascular disease, creatinine > 2.0, dementia and ASA rating.
Inability to walk at 30 and 60 days and home at 30 and 60 days adjusted for age, admitted from a nursing home, cerebrovascular disease, creatinine > 2.0, dementia and ASA rating.
bLimited to those who were not in a nursing home prior to admission (United States, N = 1129; Canada, N = 673).
cMedian follow-up 3.6 years; interquartile range: 2.7–4.4 years.
dMedian follow-up 2.6 years; interquartile range: 1.9–3.3 years
Figure 1.
Adjusted survival curve for first 60 days for Canada and the USA. Adjusted for sex, age, pre-residence nursing home, creatinine > 2.0, dementia, ASA rating. Cerebrovascular disease as one of the adjusted variables.
Figure 2.
Adjusted long-term survival curves for Canada and the USA. Adjusted for sex, age, pre-residence nursing home, creatinine > 2.0, dementia, ASA rating.
In unadjusted analyses of non-mortality outcomes, the only study outcome that statistically differed between the USA and Canada was the composite outcome of inability to walk independently/death at 30 days (USA compared to Canada: odds ratio = 0.82; 95% confidence interval: 0.68–0.98). But in the adjusted analyses, country had no independent association with inability to walk/death or return home at either 30 or 60 days.
Surgical procedures performed in each country were similar, but general anesthesia was administered more commonly in the USA. The median LOS in the surgical hospital following randomization was significantly longer (P < 0.001) in Canada (9 days, interquartile range: 5–18 days) compared to the USA (3 days, interquartile range: 2–5 days). Although both countries commonly discharged patients to rehabilitation hospitals, the USA was much more likely to discharge to nursing homes, which includes skilled nursing facilities, (n = 545; 52.9%) than Canada (n = 133; 16.8%) (P < 0.001), where such short term rehabilitation in nursing homes is uncommon. Canada was also much more likely to have subjects who were still in hospital at 30 days (n = 98; 12.4%) than the USA (n = 3; 0.2%) (P < 0.001) (Table 3).
Table 3.
Country comparison of surgical care and health services delivery
| United States, N = 1222 | Canada, N = 794 | P-valuea,b | |
|---|---|---|---|
| Type of repair | 0.21 | ||
| Arthroplasty | 413/1102 (37.5) | 315/758 (41.6) | |
| Extramedullary ORIF | 429/1102 (38.9) | 279/758 (36.8) | |
| Intramedullary ORIF | 260/1102 (23.6) | 164/758 (21.6) | |
| General anesthesia | 714 (58.6) | 395 (49.8) | <0.001 |
| Days from randomization to hospital dischargec | 3 (2–5) | 9 (5–18) | <0.001 |
| Discharge destination | <0.001 | ||
| Home | 103 (8.4) | 125 (15.8) | |
| Retirement home | 65 (5.3) | 22 (1.1) | |
| Rehabilitation hospital | 365 (29.9) | 292 (36.9) | |
| Nursing home (including skilled nursing facilities in the USA) | 645 (52.9) | 133 (16.8) | |
| Acute care | 13 (1.1) | 98 (12) | |
| Still in hospital at 30 days | 3 (0.2) | 98 (12) | |
| Died in hospital | 16 (1.3) | 18 (2.3) |
aFisher's Exact or Chi Square Tests for categorical variables.
bPlus–minus values are means ± SD, Student’s t test P-value.
cData on days to discharge are missing for two US patients and three Canadian; values are medians with interquartile ranges, Wilcoxon test P-value.
Discussion
We found significantly better adjusted survival in Canadian relative to US subjects within 30 days of hip fracture, which was sustained out to a median of 3 years post hip fracture. Despite differences in mortality, there was no difference in either walking ability or return home at either 30 or 60 days post hip fracture between countries after case-mix adjustment. Examination of the 60-day survival curves demonstrates similar mortality rates for the first 20 days, which likely reflects comparable perioperative hospital care. The survival curves then begin to diverge between countries after 20 days when most subjects were discharged from the hospital. Our unadjusted analysis of health services suggests that surgical management of hip fracture patients is similar across countries. However, Canadian subjects had substantially longer stays in the surgical hospital with more varied discharge destinations than the USA and more than 10% of Canadian subjects remained in hospital at 30 days after surgery. In contrast, US subjects had a short surgical hospital LOS and >80% were discharged to either rehabilitation facilities or nursing homes that included skilled nursing facilities.
One previous study comparing hip fracture patient outcomes between Canada and USA in the 1990s found that in-hospital mortality was higher in Canada when comparing two US States and two Canadian provinces [19]. However, the analysis was performed 2 decades ago, focused on in-hospital mortality and used administrative data that may not have captured co-morbidity as well as our prospectively collected data in FOCUS.
A 2007 systematic review comparing 38 studies on diverse conditions including cancer, coronary artery disease, chronic medical illnesses and surgical procedures between Canada and the USA reported that most studies reported equivocal outcomes or better outcomes in Canada [3]. Of note, results in this systematic review were heterogeneous and many of the studies were considered low quality by the reviewers. Further, there may be other reasons for our reported differences in survival between countries. Our data would suggest, at least for hip fracture patients, the difference may not be related to hospital care based on the similar mortality rates within the first 20 days after hip fracture.
Recent comparisons have found that Americans have lower life expectancy than Canadians [1, 20, 21]. Alternative explanations for these overall survival differences include variation in; post-discharge health-care services, socio-economic status and/or cultural characteristics between countries. These possibilities require further investigation. A recent comparison of European Union countries also demonstrated differences in patient outcomes and LOS after hip fracture, but could not provide in-depth analysis of why these variations exist [6, 22]. A systematic review of medical practice variation in Organization for Economic Cooperation and Development (OECD) countries highlighted the need for more studies that target health conditions that have clinical importance, are resource intensive and have decision-maker and public awareness [2]; hip fractures in older adults would certainly meet these criteria.
Our study has a number of strengths. This was a large cohort of complex patients from almost 50 different centers across North America. We had detailed prospectively collected information on pre-fracture health and comorbidities, which allowed us to perform extensive case-mix adjustment. Further, we had excellent ascertainment of outcomes, including walking ability and return home at 30 and 60 days post-surgery. Mortality was also verified from multiple reliable sources. These data allowed more detailed comparisons, including non-mortality outcomes, between countries. Very few Canadian subjects were under follow up after four years. The Kaplan–Meier curves we used compute death incidence only among those under follow up at a given time, producing consistent curves even when some subjects have less follow up information than others. In addition, the proportional hazards models stratify-slice the comparisons by time and only compare incidence among those subjects under follow up at a given point in time.
However, there are some notable limitations. The distributions of patient characteristics differed between countries. More Canadian patients than US patients had a history of dementia, stroke and admission from nursing home. These differences were likely due to Canadian research ethics boards permitting proxy consent more frequently than US ethics boards since patients with dementia, stroke history and/or from nursing homes tend to be less able to provide their own informed consent. We would have expected a higher mortality in Canadian patients resulting from greater frequency of patients with dementia. However, mortality was not different between countries in the unadjusted analyses. But substantial mortality differences between countries emerged and attained statistical significance after case-mix adjustment (which included nursing home residence prior to hip fracture and dementia as potential confounding variables). Our study population was also chosen from subjects enrolled in a clinical trial that targeted patients with cardiovascular disease or cardiovascular risk factors; therefore the results may not generalize to all patients with hip fractures. LOS and discharge destination from the surgical hospital are related to organization of health-care services within countries [4, 6]. We did not evaluate how the overall management of patient care varied between Canada and the US based on the pre-specified parameters of patient care collected by the FOCUS trial data. As a consequence, we are unable to clearly attribute the survival difference between countries to health system differences as we did not assess health services delivery after discharge from the surgical hospital. Further research is essential to identify if post-discharge health service utilization or other health indicators contributes to survival differences between the USA and Canada.
In summary, after case-mix adjustment, we found that Canadian subjects survived longer following hip fracture than did their American counterparts, yet subjects in both countries had similar non-mortality outcomes. Surgical care was similar between countries, but Canadians had longer surgical hospital LOS than did Americans and discharge destinations varied substantially between countries. Future research should investigate differences in the delivery of health care, both within and outside the surgical hospital setting, to determine what impact the organization of health services may have on patient outcomes after hip fracture as well as consider other indicators that could affect survival.
Funding
This work was supported in part by grants from the National Heart, Lung, and Blood Institute (U01 HL073958, U01 HL074815). The data analysis presented in this article, although using the database established by Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair (FOCUS), was a pre-specified analysis of the FOCUS protocol. No formal funding for this analysis was received from any source. L.A.B. receives salary support from the Canadian Institutes of Health Research as a New Investigator and from the Faculty of Rehabilitation Medicine as the David Magee Endowed Chair in Musculoskeletal Research. J.S.M. reports grants from National Heart Lung and Blood Institute and National Institute on Aging during the conduct of the study; he also received consulting fees while conducting and preparing the paper for this study from: Ammonett, American Orthopaedic Association, Eli Lilly, Novartis, Pluristem, Sanofi, Scholar Rock Viking, and a grant from Eli Lilly. D.M.R. reports working as a consultant for Palladian Health.
References
- 1. OECD Health Statistics 2015 http://stats.oecd.org/index.aspx? DataSetCode=HEALTH_STAT. (16 May 2016, date last accessed).
- 2. Corallo AN, Croxford R, Goodman DC, Bryan EL, Srivastava D, Stukel TA. A systematic review of medical practice variation in OECD countries. Health Policy 2014;114:5–14. [DOI] [PubMed] [Google Scholar]
- 3. Guyatt GH, Devereaux P, Lexchin J, Stone SB, Yalnizyan A, Himmelstein D et al. A systematic review of studies comparing health outcomes in Canada and the United States. Open Med 2007;1:e27–36. [PMC free article] [PubMed] [Google Scholar]
- 4. Heijink R, Engelfriet P, Rehnberg C, Kittelsen SAC, Hakkinen U. A window on geographic variation in health care: insights from EuroHOPE. Health Econ 2015;24:164–77. [DOI] [PubMed] [Google Scholar]
- 5. Kaul P, Armstrong PW, Chang WC, Naylor CD, Granger CB, Lee KL et al. Long-term mortality of patients with acute myocardial infarction in the United States and Canada: comparison of patients enrolled in Global Utilization of Streptokinase and t-PA for Occluded Coronary Arteries (GUSTO)-I. Circulation 2004;110:1754–60. [DOI] [PubMed] [Google Scholar]
- 6. Medin E, Goude F, Melberg HO, Tediosi F, Belicza E, Peltola M. European regional differences in all-cause mortality and length of stay for patients with hip fracture. Health Econ 2015;24:53–64. [DOI] [PubMed] [Google Scholar]
- 7. Tedesco D, Hernandez-Boussard T, Carretta E et al. Evaluating patient safety indicators in orthopedic surgery between Italy and the USA. Int J Qual Health Care 2016. Sep;28:486–91. [DOI] [PubMed] [Google Scholar]
- 8. Forster AJ, Bernard B, Drosler SE et al. A World Health Organization field trial assessing a proposed ICD-11 framework for classifying patient safety events. Int J Qual Health Care 2017;29:548–56. [DOI] [PubMed] [Google Scholar]
- 9. Public Health Agency of Canada. Seniors’ falls in Canada: second report 2016. http://www.phac-aspc.gc.ca/seniors-aines/publications/public/index-eng.php (15 May 2016, date last accessed).
- 10. Ciesla DJ, Pracht EE, Tepas JJ III, Cha JY, Langland-Orban B, Flint LM. The injured elderly: a rising tide. Surgery 2013;154:291–8. [DOI] [PubMed] [Google Scholar]
- 11. Gill TM, Murphy TE, Gahbauer EA, Allore HG. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol 2013;178:418–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kannus P, Sievanen H, Palvanen M, Jarvinen T, Parkkari J. Prevention of falls and consequent injuries in elderly people. Lancet 2005;366:1885–93. [DOI] [PubMed] [Google Scholar]
- 13. Braithwaite RS, Col NF, Wong JB. Estimating hip fracture morbidity, mortality and costs. J Am Geriatr Soc 2003;51:364–70. [DOI] [PubMed] [Google Scholar]
- 14. Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. J Am Med Assoc 2009;302:1573–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 2004;15:897–902. [DOI] [PubMed] [Google Scholar]
- 16. Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med 2011;365:2453–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Carson JL, Sieber F, Cook DR, Hoover DR, Noveck H, Chaitman BR et al. Liberal versus restrictive blood transfusion strategy: 3-year survival and cause of death results from the FOCUS randomised controlled trial. Lancet 2015;385:1183–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Carson JL, Terrin ML, Magaziner J, Chaitman BR, Apple FS, Heck DA et al. Transfusion trigger trial for functional outcomes in cardiovascular patients undergoing surgical hip fracture repair (FOCUS). Transfusion 2006;46:2192–206. [DOI] [PubMed] [Google Scholar]
- 19. Ho V, Hamilton BH, Roos LL. Multiple approaches to assessing the effects of delays for hip fracture patients in the United States and Canada. Health Serv Res 2000;34:1499–518. [PMC free article] [PubMed] [Google Scholar]
- 20. Kulkarni SC, Levin-Rector A, Ezzati M, Murray CJ. Falling behind: life expectancy in US counties from 2000 to 2007 in an international context. Pop Health Metrics 2011;9:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Salomon JA, Wang H, Freeman MK, Vos T, Flaxman AD, Lopez AD et al. Healthy life expectancy for 187 countries, 1990-2010: a systematic analysis for the Global Burden Disease Study 2010. Lancet 2012;380:2144–62. [DOI] [PubMed] [Google Scholar]
- 22. Guida P, Iacoviello M, Passantino A, Scrutinio D. Intra-hospital correlations among 30-day mortality rates in 18 different clinical and surgical settings. Int J Qual Health Care 2016;28:793–801. [DOI] [PubMed] [Google Scholar]