Abstract
Objectives
To explore paediatric hospital staff members’ perceptions of the emerging benefits and challenges of the huddle, a new safety improvement initiative, as well as the barriers and facilitators to its implementation.
Design
A qualitative study was conducted using semi-structured interviews to explore staff perspectives and experiences.
Setting
Situation Awareness For Everyone (SAFE), a safety improvement programme, was implemented on a sample of National Health Service (NHS) paediatric wards from September 2014 to June 2016. Previously untested in England, the huddle was a central component of the programme.
Participants
Semi-structured interviews were conducted with 76 staff members on four wards ~4 months after the start of the programme.
Results
A thematic analysis showed that staff perceived the huddle as helping to increase their awareness of important issues, improve communication, facilitate teamwork, and encourage a culture of increased efficiency, anticipation and planning on the ward. Challenges of the huddle included added pressure on staff time and workload, and the potential for junior nurses to be excluded from involvement, thus perhaps inadvertently reinforcing medical hierarchies. Staff also identified several barriers and facilitators to the huddle process, including the importance of senior nursing and medical staff leadership and managing staff time and capacity issues.
Conclusions
The findings point towards the potential efficacy of the huddle as a way of improving hospital staff members’ working environments and clinical practice, with important implications for other sites seeking to implement such safety improvement initiatives.
Keywords: quality improvement, qualitative methods, risk management, children, hospital care
Situation awareness is a core feature of the safety culture in high reliability organizations. Translated into a healthcare setting, the presence of effective situation awareness means that staff gather information, recognize its significance, and systematically report on the information in real time to facilitate a shared and timely understanding of potential risk [1, 2]. Delayed recognition and diagnosis of patient deterioration and lack of good communication have been highlighted as key factors to be addressed in building safe healthcare services [3, 4].
To facilitate the development of situation awareness in a healthcare setting, the huddle process has been adopted from other high reliability industries [2], organizations with the potential for large-scale harm that succeed in minimizing risk and errors [5]. In healthcare, the huddle process involves staff of varying occupations and seniority having a brief meeting at frequent time intervals to share information about patients, as part of other patient safety strategies being implemented at the site [6]. The aim of the huddle is to enable detection of risk of deterioration and other issues in real time, followed by the development of a shared understanding among staff members and the mitigation of the risk [7]. As a transformational process, the huddle aims to break down the silos between different professional groups that can hinder safety [8].
To date, the use and implementation of the huddle in healthcare has been evaluated primarily by researchers at Cincinnati Children’s Hospital Medical Center [1, 2, 7]. It was found that when staff had increased situation awareness using ‘a reliable system to identify, mitigate, and escalate risk’ (p. 298), which included the huddle, rates of ‘unsafe’ transfers to the intensive care unit at the hospital were reduced by almost 50% [1]. In a qualitative study of huddle implementation, the researchers reported that the huddle was perceived by staff as leading to improved efficiency and quality of information sharing, increased accountability, empowerment, a heightened sense of community, and a culture of collaboration, all of which could work together to promote patient safety [2]. Challenges associated with huddle implementation included issues around time and personnel resources [2]. Interventions developed in the United States do not often translate easily into other contexts [9]. The question to be addressed is whether the huddle could be applied to the context of clinical care in England.
Aims
The Situation Awareness For Everyone (SAFE) programme aimed to introduce and evaluate huddle implementation in England. The overarching aim of SAFE was to enhance staff situation awareness using the huddle as the key intervention, along with other safety interventions such as the Situation Background Assessment Recommendation communication tool (SBAR) [10] and paediatric early warning systems (PEWS) [11]. In this way, it was hypothesized that SAFE would improve the ward safety culture.
The aims of our study were to:
Qualitatively explore staff perceptions of the emerging benefits and challenges of the huddle
Gain an understanding of staff perceptions of the barriers and facilitators to the implementation of the huddle
Method
Setting for the study
An evaluation framework was developed to assess the impact of SAFE on patient safety, patient and parent experience of care, and staff working environments [12]. As part of the qualitative evaluation of SAFE, semi-structured interviews were undertaken with hospital staff at four of the 12 National Health Service (NHS) sites involved in SAFE across England. The sites consisted of two district general hospitals (DGH) and two specialist children’s hospitals (SCH). Two of the wards were situated in the north and two in the south of England. Three were paediatric inpatient wards encompassing a range of specialities (one also contained a high dependency unit; HDU), and the fourth was a HDU. The number of beds on each ward ranged from 15 to 25.
Qualitative data collection at the four sites took place at three timepoints: Start of programme implementation (Time 1; 4 months after the start of SAFE); mid-way through implementation (Time 2; 6 months later); end of implementation (Time 3; 6 months after Time 2). The focus of this study is on the Time 1 interviews with staff. Staff at the sites had been informed at the outset of SAFE that use of the huddle was intended to improve teamwork, communication and awareness of problems. Although patient deterioration was highlighted as being the focus of discussions in the huddle, teams were also informed that they could discuss any issues that operationally would make the service safer and more effective.
Participants
Seventy-six interviews were conducted with staff (82% female, 18% male) across the four wards (16–22 at each site), by the research assistants working on the SAFE evaluation, under the supervision of the qualitative research lead. Three sampling strategies were used: Opportunistic sampling to recruit staff who were available during site visits; purposive sampling to recruit staff representing a range of occupations and seniority; snowball sampling, involving staff suggesting others who might be interested in participating. The final sample is further described in Table 1.
Table 1.
The final sample of staff members interviewed in our study, broken down by site and occupation
| Profession | Site | |||
|---|---|---|---|---|
| DGH 1 | DGH 2 | SCH 1 | SCH 2 | |
| Consultants | 3 | 2 | 1 | 1 |
| Registrars and Junior Doctors | 0 | 3 | 0 | 2 |
| Sisters | 1 | 0 | 2 | 8 |
| Nurses | 6 | 9 | 11 | 9 |
| Administration and Housekeeping Staff | 1 | 1 | 1 | 0 |
| Ward Managers and Matrons | 1 | 1 | 1 | 0 |
| Healthcare Assistants | 0 | 1 | 1 | 0 |
| Othera | 4 | 2 | 2 | 2 |
| Total | 16 | 19 | 19 | 22 |
aIncludes specialisms such as physiotherapists, play therapists and school staff.
Ethical approval was granted by the Dulwich Research Ethics Committee (REC reference: 14/LO/0875). Informed consent was obtained from all participants.
Data collection
A semi-structured interview schedule was devised by the qualitative research lead, with input from the wider evaluation team, which covered several topics, including perceived benefits and challenges, perspectives on the practicalities of implementation and perceptions of barriers and facilitators. The interviews were either conducted face-to-face at the sites or over the telephone, and ranged from 7 to 52 min in length (M = 15.42, SD = 7.14). All interviews were audio-recorded and transcribed verbatim.
Data analysis
All of the interview transcripts were uploaded into NVivo Version 10, a computer-assisted qualitative data management software package [13]. In the initial stages of the data analysis process, the content of 75% of the transcripts was coded by the first and second authors (EmS and EvS) into predefined, top-down categories in NVivo: ‘Benefits’; ‘Challenges’; ‘Barriers’; ‘Facilitators’. A thematic analysis was then conducted to identify and analyse bottom-up themes in the content coded to each of these predefined categories [14]. EmS focused on the content coded to ‘Benefits’ and ‘Facilitators’, developing a preliminary set of themes relating to these categories, and EvS focused on ‘Challenges’ and ‘Barriers’. EmS then recoded a subset of the content coded to the latter categories to test and refine EvS’ emerging thematic frameworks, and EvS did the same with the former. Following this initial analysis of 75% of the transcripts, the thematic frameworks were then further tested against the remaining 25% of the transcripts. Minimal additional refinements were made, which enhanced the authors’ confidence in the robustness of their frameworks.
Results
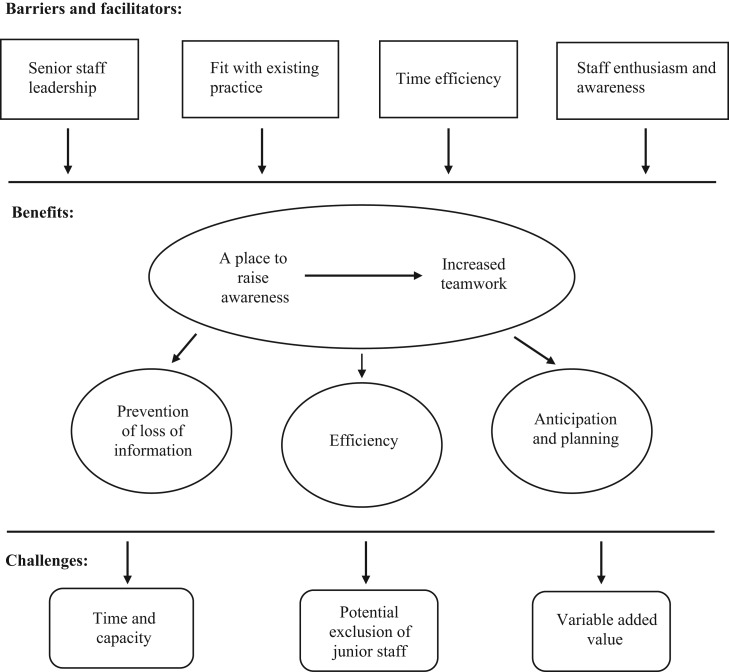
The main themes derived from the interviews, relating to the benefits, challenges, barriers and facilitators to huddle implementation from staff members’ perspectives are described below, and summarized in Table 2. Fig. 1 depicts the relationships between the themes.
Table 2.
The main themes relating to the benefits, challenges, barriers and facilitators to huddle implementation from staff members’ perspectives, with their approximate prevalence within the dataset indicated as a percentage of interviewees
| Main themes | ||
|---|---|---|
| Benefits | Challenges | Barriers/Facilitators |
| A place to raise awareness (85%) | Time and capacity issues (65%) | Senior staff leadership (20%) |
| Increased teamwork (65%) | Potential exclusion of junior staff (40%) | Fit with existing practice (35%) |
| Prevention of loss of information (45%) | Variable added value (5%) | Balancing time and capacity (75%) |
| Efficiency (40%) | Staff awareness and enthusiasm (55%) | |
| Anticipation and planning (60%) | ||
Figure 1.
The relationships between the main themes relating to the benefits, challenges, barriers and facilitators to huddle implementation from staff members’ perspectives.
Aim 1: To explore staff perceptions of the emerging benefits and challenges of the huddle
Interviewees described how the huddle had provided them with a valuable opportunity to formally share information and raise issues with a range of colleagues on the ward at set times throughout the day or shift, including highlighting the most ill or at-risk patients, reporting safeguarding concerns and issues raised by parents, and discussing staffing and patient flow issues. According to interviewees, such discussions would otherwise have taken place in a more haphazard or ‘hit and miss’ manner prior to the implementation of the huddle. Thus, as interviewees indicated, the huddle served to remind staff to regularly share information, and ensured that a range of perspectives could be clarified within the wider staff group at one point in time, to avoid misinterpretation of information heard ‘on the grapevine’. In this way, interviewees also described how the huddle had helped the staff group collectively to ensure that they were prepared to deal with adverse events should they arise, essentially giving staff the opportunity to jointly formulate a plan or structure for the day or shift on the ward, as well as for individual patients.
Nursing and medical staff members mentioned that taking part in the huddle had made them feel more like one team working together on the ward, rather than separate teams.
‘I think it helps that boundary between medical staff and nursing staff, it sort of links them a little bit more… having that time to discuss patients it’s usually something that the medical team would do together and the nursing team would do together in different ways’ (Nurse)
Nursing staff members also alluded to feeling more supported by senior colleagues now, and described how having a regular medical staff presence on the ward because of the instigation of SAFE and the huddle had meant that communication between nurses and doctors was now much more efficient, as nurses did not have to spend so much time trying to contact doctors to ask them to come to the ward. In turn, from the medical staff team’s perspective, taking part in the huddle at the start of the shift had ensured that they would know from the nursing staff team which patients they needed to see quickly and urgently, which could then help them to effectively organize their ward round according to patient need.
In terms of the challenges associated with huddle implementation, interviewees described perceiving added pressure on their time and workload from having to attend the huddle on top of their usual meetings and responsibilities or having to cover other staff members’ duties while they were attending the huddle. In addition, interviewees on some of the wards mentioned that junior nurses had not always been invited to attend the huddle or had not yet been able to attend the huddle due to their busy work schedules and obligation to stay at the patient’s bedside. It was also felt that there could be a sense among junior nurses of feeling ‘too junior’ or ‘not important enough’ to attend the huddle.
Finally, interviewees on some of the wards implied that they had not yet seen much obvious impact of the huddle on the ward environment or on their clinical practice. For instance, for one interviewee, this was because they had as yet been unable to attend the huddle due to its timing. On the other hand, another interviewee felt that this minimal impact could be due to the relatively small size of their ward, as in their opinion this potentially made the huddle less necessary than perhaps it would be on a larger ward with more staff from different teams to update and more patients to keep track of.
‘The benefits for me I think are more limited because it’s quite unusual for something to come up in the huddle that we didn’t already know about’ (Consultant)
However, other medical and nursing staff members at this site did not share this view, commenting primarily on the utility of the huddle in terms of raising awareness and facilitating teamwork within the wider staff group. Moreover, interviewees at other sites questioned whether having multiple speciality medical teams feeding into a large ward could in fact make it more challenging to implement the huddle in a time efficient manner.
‘We’re just trialling it with one team of doctors at the moment. But if we’re then doing that with all the specialities on the ward, that would take so long’ (Nurse)
Aim 2: To gain an understanding of the barriers and facilitators to the implementation of the huddle
Interviewees described how the huddle generally required consultant or senior nursing staff member leadership and instigation to take place.
I think [to get the doctors on board] that needs to come from the consultants really, same as for the nurses. I think some nurses are really good at it and other nurses think, ‘Ah I don’t need to do that, what’s the point’, so I think it kind of needs to come from management almost, ‘This is what we are doing and we need to do it’ (Nurse)
Interviewees also indicated that to facilitate successful implementation, the project needed to fit with and enhance rather than alienate existing ward practices, such as through establishing an appropriate time for the huddle so that it fit with the daily routine of the ward. However, lack of staff time and capacity was a key barrier to huddle implementation identified by interviewees, including having competing responsibilities and priorities, which could make it difficult to engage with the huddle on top of their other existing duties.
‘It’s just when the ward’s so busy it’s getting people there to, and although you know it’s only a two-minute job, it’s when you’ve got five other things that need to happen at the same time’ (Nurse)
According to interviewees, ways of tackling this barrier included ensuring the time efficiency of the huddle, which could be achieved through organization and standardization of the huddle, such as through use of a script to structure the information discussed, and teamwork, such as in terms of staff updating each other on concerns to bring to the huddle or on outcomes from the huddle if they were unable to attend.
Yet, interviewees on some of the wards described how lack of awareness of the huddle among the wider staff group had meant that the huddle did not always happen during night shifts or over weekends, and had meant that not all staff, particularly junior nursing staff members, attended the huddle when it did happen. Interviewees felt that staff enthusiasm for and awareness of the huddle often relied on investment from senior staff in inspiring, educating, and encouraging others to be involved, as well as from staff understanding the benefits, relevance and importance of the huddle and seeing this in action over time.
‘It’s like pushing a boulder up the hill. If you take your foot off the pedal, it’s going to hit you back in the face, so you’ve got to keep pushing to try and change it’ (Consultant)
Discussion
To date and to our knowledge, our study is the first to qualitatively evaluate the implementation of the huddle in paediatric healthcare settings in the United Kingdom. The staff members interviewed in our study indicated that the huddle was a forum that had provided a crucial opportunity to raise concerns, develop awareness and prevent information loss. A key consequence was the promotion of a culture of increased teamwork, efficiency and planning on the ward. It is possible to see how these benefits could impact on the way that patients are managed, such as with the timely development of a shared awareness among the wider staff group of clinical conditions of patients and potential risk. Our findings reflect those reported in two previous qualitative studies in the United States on the perceived impact of the huddle [2, 7], as well as those reported in a qualitative evaluation of the benefits and challenges of PEWS scores [15]. As one would expect with the introduction of a new process, there were also some challenges to huddle implementation identified by the staff members in our study, including perceptions of increased pressure on time and workload. Nonetheless, interviewees indicated that practice, standardization and structure could mitigate against this.
As the SAFE programme allowed contextualization of implementation, there were differences in the ways in which the huddle was implemented at the different sites and some of the staff members’ perceptions of challenges reflected this. For example, the ‘exclusion’ of junior nursing staff members could have been the result of local design of implementation, in that across the sites the huddle usually took place away from the patients’ bedsides, which meant that on the wards with a HDU specialty, nurses who could not leave the patient’s bedside were then unable to attend. This implies that the location of the huddle is important and for these sites ideally should be close to the clinical area, with attention to patient confidentiality. Yet, there also seemed to be a feeling among junior nurses on some of the wards that they had not yet been invited by senior management to attend the huddle. This could reflect the ongoing reinforcement of the medical hierarchy inherent in the healthcare system and indicate that potentially SAFE was seen on some of the wards at this early implementation timepoint as being more oriented towards senior members of staff. This could also imply a lack of understanding that the huddle is intended to be non-hierarchical [7], and could mean that senior staff members on these wards may need to make a more concerted effort to involve junior staff members in the initiative. Emphasizing the importance and value of input from all staff members (regardless of discipline) to patient care, and encouraging flat hierarchies have been put forward as key recommendations for facilitating effective teamwork and communication in a healthcare setting [8]. Perhaps evidence at these sites of the flattening of the hierarchy because of the huddle may also emerge over time as implementation continues and is refined [7].
In terms of the barriers and facilitators to huddle implementation, our findings suggest that successful implementation of a new safety improvement initiative like the huddle needs: Senior medical and nursing staff leadership or ‘championing’; to blend in with and enhance rather than alienate existing ward practices; staff to have the time and capacity to implement the initiative, which perceptions of the benefits of the initiative, teamwork, and the time efficiency of the initiative can facilitate; staff to have enthusiasm towards and awareness of the initiative, how it works, and its rationale, which can take time and can also be influenced by senior staff leadership.
Previous research exploring the implementation process of quality improvement initiatives in healthcare settings has similarly cited the importance of senior medical staff leadership in ensuring the successful implementation of such initiatives [16, 17]. The ‘fit’ of a new initiative with the local context, staff needs and existing ward practices has also been a key recommendation in quality improvement practice [18, 19]. In addition, further in line with our findings, previous research has highlighted how staff perceptions of the importance of, necessity of, or the potential problems with a new intervention can affect how willing staff are to engage with such an initiative [18]. Thus, explaining why an intervention is necessary and providing clear instruction for its implementation is crucial to increasing staff support for implementation [18].
Limitations
The sites in our study were selected to offer a representation of paediatric settings in England. Nonetheless, there may be limitations to the transferability of our findings to other wards, although there was relatively minimal cross-site variation in our findings. Our sample may also have included an overrepresentation of staff with more positive views of the huddle, as staff with more negative views may have felt less comfortable about being interviewed. Moreover, as staff were interviewed during their working hours, this meant that at times the interviews followed a more structured format, rather than semi-structured, with less time available to follow up on ideas that participants expressed. Thus, while a relatively large sample of interviews was conducted, there was variation in terms of the level of depth reached by the interviewer.
Conclusions
Our findings suggest the potential efficacy of the huddle as a way of improving hospital staff members’ working environments and clinical practice, as previously reported in the United States. Future research could explore possible changes over time in staff experiences and perceptions of the benefits the huddle, including how or if staff manage to overcome the challenges and barriers faced during initial implementation. Overall, the cross-site barriers and facilitating factors that emerged from the interviews with the staff members in our study are applicable to other sites seeking to implement a new quality improvement initiative, as well as to sites seeking to implement the huddle. The findings can be used to provide guidance for implementation, which would then need to be tested locally considering different cultural contexts and settings in healthcare.
Funding
This work was supported by the Health Foundation and WellChild. SAFE was a Health Foundation funded programme; both the implementation of SAFE and the evaluation were funded by the Health Foundation. This work was also supported by funding from WellChild; the funding was specifically to support evaluation work around perspectives of parents and young people and to support patient and parent involvement in the research.
Conflict of interest statement
P.L. led the implementation of the SAFE programme and contributed to the literature review for this paper. P.L. was not involved in the data collection nor data analysis for this paper.
Acknowledgements
The authors would like to thank the staff members at the four hospitals who generously shared their experiences and views with us. We also thank the other members of the evaluation team for their contributions to this study—Dawid Gondek, Dr Jacqueline Hayes and Amy Ramsay. The project implementation was led by the Royal College of Paediatrics and Child Health (RCPCH) and supported by the UCL Partners Academic Health Science Network. M.L., M.W. and J.D. were partly supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) North Thames at Bart’s Health NHS Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR, or the Department of Health.
References
- 1. Brady PW, Muething S, Kotagal U et al. Improving situation awareness to reduce unrecognized clinical deterioration and serious safety events. Pediatrics 2013;131:298–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Goldenhar LM, Brady PW, Sutcliffe KM et al. Huddling for high reliability and situation awareness. BMJ Qual Saf 2013;0:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. National Patient Safety Agency (2009). Review of Patient Safety for Children and Young People: http://www.nrls.npsa.nhs.uk/resources/?entryid45=59864 (February 2017, date last accessed).
- 4. Okuyama A, Wagner C, Bijnen B. Speaking up for patient safety by hospital-based health care professionals: a literature review. BMC Health Serv Res 2014;14:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. The Health Foundation (2011). High Reliability Organisations: http://www.health.org.uk/sites/health/files/HighReliabilityOrganisations.pdf (October 2017, date last accessed).
- 6. Taitz J. Building a culture of safety in pediatrics and child health. Curr Treat Options Pediatr 2015;1:253–61. [Google Scholar]
- 7. Provost SM, Lanham HJ, Leykum LK et al. Health care huddles: managing complexity to achieve high reliability. Health Care Manage Rev 2015;40:2–12. [DOI] [PubMed] [Google Scholar]
- 8. Weller J, Boyd M, Cumin D. Teams, tribes and patient safety: overcoming barriers to effective teamwork in healthcare. Postgrad Med J 2014;90:149–54. [DOI] [PubMed] [Google Scholar]
- 9. Dixon-Woods M, Leslie M, Tarrant C et al. Explaining matching Michigan: an ethnographic study of a patient safety program. Implement Sci 2013;8:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. NHS Institute for Healthcare Improvement (2017). SBAR Toolkit: http://www.ihi.org/resources/Pages/Tools/sbartoolkit.aspx (February 2017, date last accessed)
- 11. Lambert V, O’Shea MT, Walshe C et al. (2014). A Systematic Literature Review to Support the Development of a National Clinical Guideline - Paediatric Early Warning System (PEWS). http://health.gov.ie/wp-content/uploads/2014/03/PEWS-Sytematic-Literature-Review-Oct-2014.pdf (February 2017, date last accessed).
- 12. Deighton J, Edbrooke-Childs J, Stapley E et al. Realistic evaluation of Situation Awareness for Everyone (SAFE) on paediatric wards: study protocol. BMJ Open 2017;6:e014014 10.1136/bmjopen-2016-014014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bazeley P, Jackson K. Qualitative Data Analysis With NVivo; Vol. 2 London, UK: Sage Publications Ltd., 2013. [Google Scholar]
- 14. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. [Google Scholar]
- 15. Tucker KM, Brewer TL, Baker RB et al. Prospective evaluation of a pediatric inpatient early warning scoring system. J Spec Pediatr Nurs 2008;14:79–85. [DOI] [PubMed] [Google Scholar]
- 16. Guinane CS, Davis NH. The science of Six Sigma in hospitals. Am Heart Hosp J 2004;2:42–8. [DOI] [PubMed] [Google Scholar]
- 17. Leape LL, Rogers G, Hanna D et al. Developing and implementing new safe practices: voluntary adoption through statewide collaboratives. BMJ Qual Saf 2006;15:289–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bergs J, Lambrechts F, Simons P et al. Barriers and facilitators related to the implementation of surgical safety checklists: a systematic review of the qualitative evidence. BMJ Qual Saf 2015;24:776–86. [DOI] [PubMed] [Google Scholar]
- 19. Hart CK, Dykes C, Thienprayoon R et al. Change management in quality improvement: the softer skills. Curr Treat Options Pediatr 2015;1:372–9. [Google Scholar]