Abstract
Introduction
Radiotherapy can diminish quality of life (QoL) for prostate cancer patients. Our objective was to evaluate the effect of radiotherapy on QoL in men aged 75 years or older treated with radiotherapy for a localized prostate cancer, and to identify predictors of reduced QoL.
Patients and methods
We prospectively administered a battery of geriatric (MNA, GDS, Get up and Go Test, CIRS-G, ADL, IADL, MMSE), toxicity (IPSS; IIEF 5), and QoL (QLQ C30) screening tests in 100 elderly patients before and two months after prostate cancer radiotherapy (NCT 02876237). Patients ≥ 75 years undergoing radiotherapy with a curative intent for localized prostate cancer with or without androgen deprivation therapy (ADL) were eligible for study inclusion. Correlations between patient-assessed QoL and tumor characteristics, radiotherapy treatment or CGA parameters were sought using the Fisher or the Mann and Whitney tests. Changes in QoL parameters over time were analyzed using the Wilcoxon signed-rank test.
Results
At study entry, scores for IADL impairments were present in 51%, reduced autonomy in activities of daily living in 16%, cognitive impairment found in 20%, depression-related symptoms in 31%, and 66% of patients had significant co-morbidities. Eight percent were judged to be at risk of fall and 2% were found to be undernourished. Severely impaired (IPSS ≥ 20) urinary function was observed in 11.2% and 13.5% of patients before and two months after completion of radiotherapy respectively. Significantly decreased QoL (> 20 points) at two months after treatment was found in 13% of patients and a moderate but clinically relevant reduction (10 to 20 points) in 17% of patients. No tumor characteristic, treatment, or oncogeriatric parameter was predictive of reduced QoL following prostate cancer radiotherapy.
Conclusion
Despite sometimes markedly diminished oncogeriatric parameters, prostate cancer radiotherapy was generally well tolerated in these elderly patients. We found no predictive factor to determine which patients would experience impaired quality of life following radiotherapy.
Introduction
Prostate cancer mostly occurs in elderly men (aged ≥ 75 years) in whom it represents a major cause of impaired quality of life and is a leading cause of cancer mortality [1]. Localized prostate cancer in the elderly is mostly treated with androgen deprivation therapy (ADT) and/or radiotherapy, and surgery is only rarely recommended [2]. Although severe radiotherapy-induced toxicity is unusual in younger patients, occurring in fewer than 5% of them, curative radiotherapy is often believed to be less well tolerated in the elderly. Older patients tend to present with impaired urinary and digestive function that risk being by aggravated by radiotherapy. For this reason, only a minority of patients older than 75 with localized high-risk prostate cancer receive any local treatment. The majority receive palliative treatment (ADT or no therapy at all) [3], despite evidence showing significantly improved survival when radiotherapy is added to ADT [4,5].
The quality of life of patients undergoing intensity-modulated radiation therapy (IMRT) for prostate cancer often diminishes immediately after therapy [6,7], but most symptoms resolve within 6 months and long term quality of life is usually comparable to that prior to therapy [8–10]. Radiotherapy (and ADT) are particularly associated with increased asthenia and decreased social, physical and cognitive functioning at two months after treatment [6]. Retrospective studies suggest that prostate cancer radiotherapy is quite well tolerated in older patients [11,12], but despite the large burden of localized prostate cancer, prospective studies of quality of life after radiotherapy in this potentially fragile population are lacking.
The selection of elderly patients for risk-adapted oncology treatments remains a challenge for oncogeriatric study. Geriatric screening instruments offer one avenue of assistance to the clinician who wishes to orientate the fragile patient prior to any oncologic intervention [13]. Comprehensive Geriatric assessment (CGA) enables precise scoring of daily activities, risk of fall, undernutrition, depression, and comorbidities to help predict whether aggressive cancer treatments will be tolerated. Although CGA is largely used prior to medical interventions, such as chemotherapy [14] or ADT [15–17], specific studies of older prostate cancer patients undergoing radiotherapy are mostly retrospective, lack precise oncogeriatric evaluation [18–21] or focused on toxicity (assessed by physicians) and not on patient’s related quality of life [22].
We carefully analyzed the geriatric characteristics of a group of older patients and prospectively assessed toxicity and quality of life in order to be able to determine which factors might be predictive of poorly-tolerated radiotherapy.
Patients and methods
We recruited patients with localized prostate cancer aged 75 or more for whom a multidisciplinary tumour board had recommended local prostate radiotherapy with curative intent, alone, or combined with ADT, to a prospective multicenter cohort study (NCT 02876237). Patients were recruited by radiation oncologists during the first consultation, after the multidisciplinary tumor board and before starting radiation therapy. Patients undergoing salvage prostate bed radiotherapy following surgery were also included. There was no exclusion criteria regarding general conditions. The study was approved by the appropriate ethics committees, the Comité Consultatif sur le Traitement de l’Information en matière de Recherche dans le domaine de la Santé (CCTIRS) and the Commission Nationale Informatique et Liberté (CNIL). All patients gave consent for participating to the collection and analysis of data of this study.
All patients underwent a complete comprehensive Geriatric Assessment (CGA) by a geriatrician prior to initiation of radiotherapy. The past medical, personal and social history, current medication, body mass index, and home to study center distance were documented. The Cumulative Illness Rating Scale for Geriatrics (CIRS-G) [23], Activities of Daily Life (ADL) [24] and Instrumental Activities of Daily Life (IADL) [25], Mini Mental State Examination (MMSE) [26], mini Geriatric Depression Scale (GDS) [27], Mini Nutritional Assessment (MNA) [28], and the get up and go test (GUAGT) [29] were performed and the scores recorded. See Annexe 1 for details.
Clinical target volumes and organ-at-risk volumes were determined according to the GETUG (Groupe d’Etude des Tumeurs Urogenital, french group for genito-urinary tumors study) recommendations for prostate [30], prostatic bed [31] and pelvic lymph node [32] contouring. Radiotherapy was delivered to a total dose of 74.8–80 Gy in 34 to 40 fractions to the prostate or 66 Gy in 33 fractions to the prostatic bed. In high-risk patients, pelvic lymph nodes received 46–54.4 Gy in 23 to 34 fractions. Hypofractioned radiotherapy to the prostate (60 Gy in 20 fractions) was allowed in accordance with the PROFIT trial guidelines [33]. Dose constraints for the rectum and the bladder followed the Quantec recommendations [34,35].
Patients with an intermediate prognosis according to D’Amico’s classification were eligible for 3–6 months of concurrent and adjuvant hormonal therapy, which was extended to 2 to 3 years in high risk patients [36]. ADT was to be administered prior to or on the first day of radiotherapy.
Patients completed the International Prostate Symptom Score (IPSS), the International Index of Erectile Function (IIEF-5), the core and prostate cancer–specific modules of the European Organization for Research and Treatment of Cancer (EORTC) quality of life (QoL) questionnaires (QLQ-C30 version 3.0) at the first consultation (before radiotherapy) and at two months after treatment. We did not monitor quality of life during radiotherapy because very different radiotherapy protocols were used (between 20 to 40 fractions in 4 and 8 weeks), instead focusing on early (2 months) assessment after radiotherapy. Items were combined according to EORTC criteria into several scales ranging from 1 to 100. The higher the score for global health and function, the better the QoL; the higher the score for symptoms, the poorer the QoL.
Correlations between patient-assessed QoL, their treatment, and CGA parameters were sought using the Fisher test for linear association (categoric variables) or the Mann and Whitney test (continuous variables). The significance threshold was p < 0.05, except for changes in QoL from baseline. A 10-point change in QoL was considered to be moderate but clinically relevant, severe for a 20-point change in score, and statistically significant if p < 0.01 [37,38]. These changes in QoL parameters over time (decrease on functional scoring and increase on symptoms scoring) were analyzed using the Wilcoxon signed-rank test.
Results
Assessment at study entry
One hundred patients presenting with intermediate (49%) or high-risk prostate cancer (48%) were recruited in 11 different cancer centers (Table 1). Their median age was 77.5 years (mean 78.4; range 75–89). The median distance between the patient’s home and radiotherapy center was 28 km (mean 32 km; range 4–147). The ADT was administered in 50% of patients. Severely (IPSS 20–35) or moderately impaired urinary function (IPSS 8–19) was observed in 11.2% (10/89) and 44.9% (40/89) of patients respectively. Among 78 patients who responded to the IIEF questionnaire which assesses sexual activity and erectile function, sexual activity was present in 26 patients (33.3%), among whom eight (10.3%) experienced normality or only minor dysfunction (IIEF 16–25), nine (11.5%) moderate dysfunction (IIEF 11–15), and nine (11.5%) severe dysfunction (IIEF 5–10). The CIRS-G revealed comorbidity in 66/100 patients, with 51/100 of patients presenting moderate to severe cardiovascular comorbidities. A GDS score ≥ 1 revealed depressive symptoms in 31/100 of patients. The activities of daily life (ADL score > 6) and Instrumental Activities of Daily Life (IADL score > 7) were impaired in 16/100 and 51/100 of patients respectively. Cognitive disorders (MMSE < 27) were revealed in 20/100 of patients. The calculated risk of fall (GUAGT <0) was 8/100 and undernutrition (MNA ≤17) was found in 2/100 of patients.
Table 1. Patient characteristic N = 100.
| Age | % |
| 75–79 | 72 |
| 80–85 | 24 |
| ≥ 85 | 2 |
| BMI | |
| underweight (<18) | 2 |
| normal (18–25) | 27 |
| overweight (25–30) | 50 |
| obesity (>30) | 21 |
| Number of medications | |
| 0–3 | 58 |
| > 3 | 42 |
| Distance to radiotherapy center | |
| < 30 km | 54 |
| 30 à 60 km | 27 |
| ≥ 60 km | 19 |
| Clinical stage | |
| low | 3 |
| Intermediate | 49 |
| high | 48 |
| Geriatric problems | |
| Depression | 31 |
| Impaired GUAGT | 8 |
| Denutrition | 2 |
| Comorbidities | 66 |
| ADL impairment | 16 |
| IADL impairment | 51 |
| Cognitive impairment | 20 |
| Radiotherapy | |
| prostate | 76 |
| prostate bed | 24 |
| ADT | |
| yes | 50 |
| no | 50 |
BMI: body mass index
ADL: activities of daily life
IADL: instrumental activities of daily life
ADT: androgen deprivation therapy
Assessment following radiotherapy
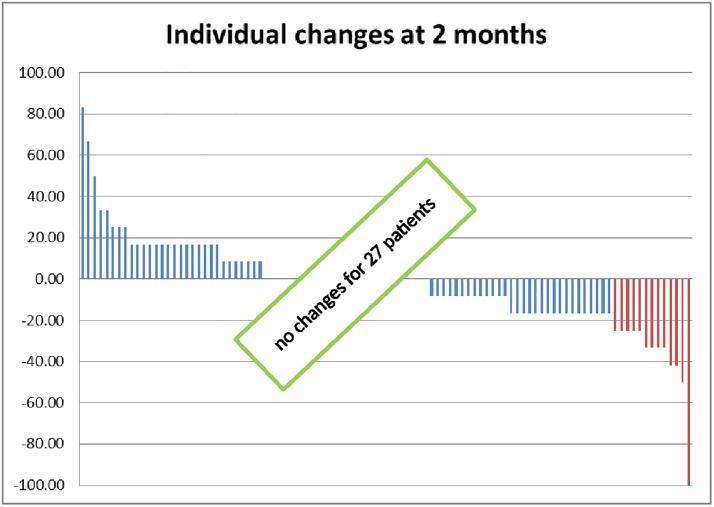
Two months after radiotherapy had concluded urinary function was assessed using the IPSS questionnaire in 89 patients. Severely (IPSS 20–35), moderately (IPSS 8–19), or only mildly impaired or normal function (IPSS <8) was noted in 13.5% (12/89), 44.9% (40/89) and 41.6% (37/89) of patients respectively. Similarly, among 71 patients who responded to a further IIEF questionnaire, sexual activity was maintained in 17 patients (23.9%). Among these, two (2.8%) experienced normal or only minor dysfunction (IIEF 16–25), four (5.6%) moderate impairment (IIEF 11–15) and eleven (15.5%) severe impairment (IIEF 5–10) of erectile function. We analyzed self-reported QoL following radiotherapy in 100 patients (see Fig 1 and Table 2). According to the core QoL questionnaire, general QoL was moderately decreased (loss of 10 to 20 points) in 17 patients (17%) and markedly decreased (loss ≥ 20 points) in another 13 patients (13%). On an individual basis (Table 2), the most frequent important (variation > 20 points) QoL alterations were diarrhea (21 patients), constipation (14), role functioning (20), fatigue (18) dyspnea (17) and insomnia (17).
Fig 1. Individual changes in global QoL.
Questions 29 and 30 in EORTC QLQ C30 questionnaires enable to calculated a score (from 0 to 100) for global QoL. Variations of this score before and 2 months after radiotherapy are reported here for each patient. There is an important decrease of QoL (≥ 20 points) for 13 patients and a moderate decrease in QoL (10 to 20 points) in 17 patients.
Table 2. Variation of quality of life and symptoms parameters N = 100.
| Variation 10–20 (%) | Variation ≥ 20 (%) | Variation ≥ 10 (%) | |
|---|---|---|---|
| Global Health | 17 | 13 | 30 |
| Physical functioning | 5 | 9 | 14 |
| Role functioning | 12 | 20 | 32 |
| Emotional functioning | 7 | 4 | 11 |
| Cognitive functioning | 16 | 5 | 21 |
| Social functioning | 16 | 12 | 28 |
| Fatigue | 22 | 18 | 40 |
| Nausea / Vomiting | 1 | 3 | 4 |
| Pain | 12 | 11 | 23 |
| Dyspnoea | 0 | 17 | 17 |
| Insomnia | 0 | 17 | 17 |
| Appetite loss | 0 | 11 | 11 |
| Constipation | 0 | 14 | 14 |
| Diarrhoea | 0 | 21 | 21 |
| Financial difficulties | 0 | 4 | 4 |
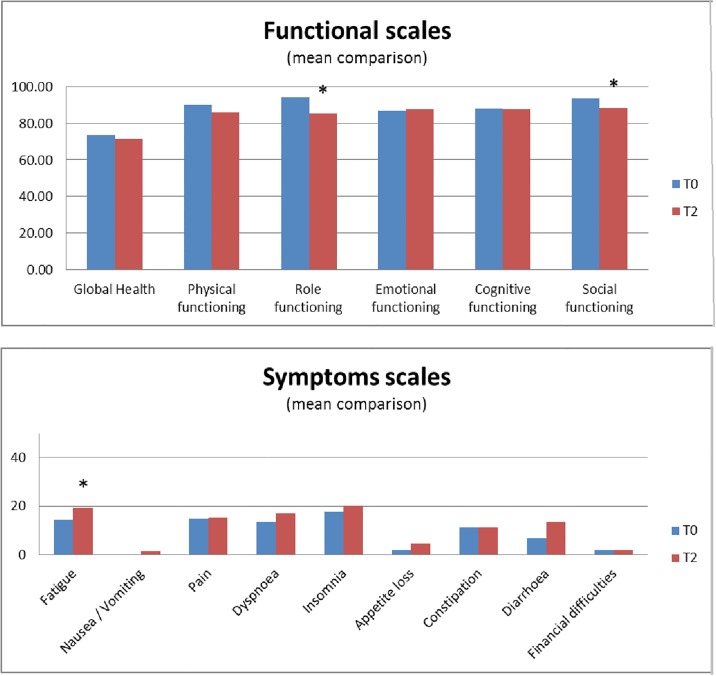
We then analyzed mean score comparisons of each item on the QLQ C30 questionnaire between baseline and two months (Fig 2a and 2b). Significant (p<0.01) impairment in role (mean loss -9, p = 0.0001) and social functioning (mean loss -4.9, p = 0.0044) was observed at two months compared with baseline. On the symptom scales, only fatigue (mean increase +4.6, p = 0.0029) was significantly increased at two months.
Fig 2. For each item of QLQ C30 questionnaire, we compare mean score before and 2 months after radiotherapy.
For functional scales (Fig 2a), a high score is related to better QoL and for symptoms scores (Fig 2b), high score is related to high symptoms and worth QoL. Statistically significant variations.
Predictive factors for impaired patient-reported outcomes
We wished to determine whether any clinical parameter or geriatric score was predictive for impaired QoL parameters (Table 3). No parameter was found significantly predictive for a deterioriation in general QoL. Better QoL at baseline was associated with more moderate alterations in QoL at two months after radiotherapy had concluded (p = 0.012).
Table 3. Predictive factors for moderate changes in quality of life.
| No QoL decrease > 10 points(n = 70) | QoL decrease > 10 points(n = 30) | p | |
|---|---|---|---|
| Age | 78 [75–89] | 77 [75–88] | 0.933 |
| Distance | 28 [4–147] | 19 [5–85] | 0.687 |
| BMI | 27.4 [20.5–42.9] | 25.9 [19.8–34.9] | 0.187 |
| Number of medications | 3 [0–6] | 2 [0–6] | 0.873 |
| QLQ-C30 T0 | 75.0 [0–100] | 83.3 [50.0–100] | 0.012 |
| Clinical stage | 0.721 | ||
| Low | 3 | 0 | |
| Intermediate | 33 | 15 | |
| High | 34 | 15 | |
| Radiotherapy | 0.153 | ||
| prostate | 56 | 20 | |
| prostatic bed | 14 | 10 | |
| ADT | 0.614 | ||
| No | 33 | 16 | |
| Yes | 36 | 14 | |
| Depression | 0.422 | ||
| No | 50 | 19 | |
| Yes | 20 | 11 | |
| Risk of fall | 0.699 | ||
| No | 55 | 24 | |
| Yes | 5 | 3 | |
| Denutrition | 0.3 | ||
| No | 70 | 29 | |
| Yes | 0 | 1 | |
| Comorbidities | 1 | ||
| No | 24 | 10 | |
| Yes | 46 | 19 | |
| Urinary symptoms | 0.576 | ||
| Light | 25 | 14 | |
| Moderate | 29 | 11 | |
| High | 8 | 2 | |
| ADL impairments | 0.138 | ||
| No | 56 | 28 | |
| Yes | 14 | 2 | |
| IADL impairments | 1 | ||
| No | 34 | 15 | |
| Yes | 36 | 15 | |
| Cognitive impairment | 0.749 | ||
| No | 59 | 27 | |
| Yes | 10 | 3 | |
| Urinary symptoms at 2 months | 0.177 | ||
| Mild | 25 | 12 | |
| Moderate | 31 | 9 | |
| Severe | 6 | 6 | |
Discussion
The decision as to whether to recommend local treatment for prostate cancer in the elderly remains challenging, and prospective data on the tolerability of radiotherapy in this population were lacking. Our comprehensive and systematic evaluation of a large representative cohort confirms that a substantial proportion of these patients are indeed at risk of fatigue and impaired QoL following radiotherapy. However, our most important finding is that despite numerous comorbidities and frequently impaired geriatric parameters, more than 70% of older patients undergoing radiotherapy maintain their overall QoL immediately after completion of radiotherapy. No geriatric, patient or treatment-related parameters were predictive of impaired QoL following radical radiotherapy.
The majority of these elderly patients presented with impaired geriatric parameters. More than half of our patients about to undergo radiotherapy had some pre-existing restriction in IADL. Moreover, two thirds of patients presented with comorbidities, especially cardiovascular comorbidities, which may affect ADT tolerance [36]. Unsuspected memory loss problems were discovered in one in five patients, and depression in almost one in three patients, which may also be aggravated by ADT [39]. These fragilities were usually found in metastatic cancer patients [40,41]. This underlines the utility of CGA prior to initiation of curative radiotherapy treatment, in order to provide appropriate overall care in this vulnerable population. The vulnerabilities of geriatric prostate cancer patients undergoing radiotherapy differ from those of metastatic patients undergoing chemotherapy [42]. Numerous studies have insisted upon the importance of nutritional status prior to drug administration, both for the tolerability of chemotherapy, and survival [43,44]. In our study, malnutrition was practically absent. Geriatric screening questionnaires place considerable weight on the evaluation of the nutritional status: on the G8 three questions out eight relate to nutrition [45]. Similarly impaired GUAGT is often sought by geriatricians [43] but was found in fewer than 10% of our patients. This suggests that a screening tool like G8 may be insufficient to fully evaluate the occult vulnerabilities in these elderly patients and that fuller CGA is needed, in accordance with other recent findings [22].
Despite impaired geriatric parameters, radiotherapy was well tolerated and the QoL maintained in a large proportion of patients. Urinary function was overall well preserved following radiotherapy (severe urinary symptoms in 11.2% of patients prior to radiotherapy compared with 13.5% after). This result contrasts with previous studies showing that increased age (>70) is a risk factor for increased urinary toxicity [46,47]. Longer follow-up is needed to fully assess long-term urinary toxicity. Important (> 20 points) acute diarrhea occurred in 21% of patients. Older patients are also at higher risk of digestive toxicity [48,49]. In a minority of patients (less than 20%), radiotherapy potentially increased fatigue, which consequently decreased social and leisure interactions. The source of fatigue during radiotherapy is multiple: comorbidities, transportation to the radiotherapy center, nocturia or ADT. Fatigue is very common in men with prostate cancer, particularly in those receiving ADT, and is a common side effect of prostate cancer radiotherapy [50,51], but whether this fatigue is greater in older patients remains unproven.
Despite acute toxicity, overall QoL was maintained or improved in 70% of patients and only 13% of patients complained of severely (> 20 points) decreased QoL at two months. These favourable results are similar to studies in younger patients, where radiotherapy combined with 6-months of androgen-depriving therapy did not profoundly alter physical or mental health as compared to active monitoring [52]. We previously evaluated longitudinal QoL following IMRT in a younger population (median age 73, range [50–80]), and found a similar pattern where quality of life was moderately impaired at two months but then returned to baseline after six months [6,9]. Other studies have also showed moderate but transient impaired QoL immediately after radiotherapy in younger patients [10,53,54]. However, more patients experienced moderately (17% vs 5.2%) or markedly (13% vs 10.5%) impaired overall QoL in this geriatric series than in our younger patient series. The impact of age on impairment of QoL remains an open question.
We hypothesized that a CGA prior to the initiation of radiotherapy, together with comprehensive collection of patient- and treatment-related data would enable us to predict decreased QoL at two months after radiotherapy had ended. Neither baseline oncogeriatric parameters, patient or tumor characteristics, distance to radiotherapy center, nor the use of ADT were correlated to severely (>20 points) or moderately (>10 points) impaired QoL. This might be explained by a quite limited sample and/or by the low number of patients experiencing decreased QoL. Some authors showed that higher levels of comorbidity diseases were predictive of decreased long-term global QoL following radiotherapy and ADT [55]. Others confirms our findings with difficult for CGA outcomes to predict significant acute radiotherapy toxicity [22]. We will pursue the analysis over a longer follow-up period and repeat CGA during follow up to evaluate the impact of geriatric characteristics on subsequent QoL following radiotherapy.
The generalizability of our study may be limited by a potential selection bias. In France, all patients who are candidates for radical radiotherapy treatment must be discussed at a multidisciplinary board meeting. During these meetings, the urologists often propose active monitoring or ADT for very fragile older patients. Considering the potential selection bias, we asked the investigators in each center. We can summarise as follow: about 5% of the patients we considered too frail for radiotherapy during multidisciplinary tumor board. Patients over 75 represent between 40% and 50% of all patients treated by radiotherapy for a localised prostate cancer. Successful recruitments were very different between the eleven centers, between 100% to 50%, and patient’s refusal was often due to important distances between home and radiotherapy center. Our patient population does not therefore reflect the general population of older men with prostate cancer. However, our study was not restricted to teaching hospitals (where tertiary referral may produce an atypical patient population) and more importantly, our CGA revealed that a large number of patients were considered to have CGA impairments. Our study is therefore reasonably representative of the population of patients whose life expectancy suggests that they may benefit from radical radiotherapy. Our study was restricted to acute toxicity and early evaluation of reported outcomes. We focused on an early time point (two months after treatment) because our previous study showed that QoL worsened immediately following radiotherapy but returned to baseline 18 months after completion of IMRT. However, delayed intestinal toxicity affecting QoL may occur years after completion of radiotherapy [52]. We therefore need to validate our results after longer follow-up. Another potential limitation of our study is that the CGA may have revealed treatable problems whose correction prior to radiotherapy may have reduced the impact of this treatment on QoL. To avoid this bias, a clinical trial randomizing CGA should be performed, as has been done in lung cancer [56].
Conclusion
Localized prostate cancer of older men is a common clinical situation and the role of radical radiotherapy is controversial. Most patients are currently treated by active monitoring or ADT only. Our study is the first to extensively evaluate geriatric parameters prior to initiation of radiotherapy and longitudinally assess for QoL parameters following treatment. Our data suggest that QoL is mostly well conserved soon after radiotherapy, with or without ADT, even in this often debilitated patient population. This means that if there is a reasonable prospect that local radiotherapy will enhance the patient’s life expectancy, the fear of iatrogenic decreased QoL need not inhibit the decision to treat. An extensive CGA prior to initiation of radiotherapy can reveal comorbidities that may worsen after radiotherapy combined with ADT. We found no particular predictive factors for which older patients were most at risk of decreased QoL following radiotherapy. Further evaluation of long-term QoL is needed.
Supporting information
(XLSX)
(DOC)
Acknowledgments
Funded by Unité de Concertation en Onco-Gériatrie (UCOG) des Pays-de-la-Loire.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the Unité de Concertation en Onco-Gériatrie (UCOG) des Pays-de-la-Loire (institutionnal funding). NCT 02876237 (https://www.oncopl.fr/oncogeriatrie). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, Rosso S, Coebergh JWW, Comber H, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer Oxf Engl 1990. 2013;49: 1374–1403. doi: 10.1016/j.ejca.2012.12.027 [DOI] [PubMed] [Google Scholar]
- 2.Droz J-P, Aapro M, Balducci L, Boyle H, Van den Broeck T, Cathcart P, et al. Management of prostate cancer in older patients: updated recommendations of a working group of the International Society of Geriatric Oncology. Lancet Oncol. 2014;15: e404–414. doi: 10.1016/S1470-2045(14)70018-X [DOI] [PubMed] [Google Scholar]
- 3.Bechis SK, Carroll PR, Cooperberg MR. Impact of age at diagnosis on prostate cancer treatment and survival. J Clin Oncol. 2011;29: 235–241. doi: 10.1200/JCO.2010.30.2075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Locke JA, Dal Pra A, Supiot S, Warde P, Bristow RG. Synergistic action of image-guided radiotherapy and androgen deprivation therapy. Nat Rev Urol. 2015;12: 193–204. doi: 10.1038/nrurol.2015.50 [DOI] [PubMed] [Google Scholar]
- 5.Bekelman JE, Mitra N, Handorf EA, Uzzo RG, Hahn SA, Polsky D, et al. Effectiveness of androgen-deprivation therapy and radiotherapy for older men with locally advanced prostate cancer. J Clin Oncol. 2015;33: 716–722. doi: 10.1200/JCO.2014.57.2743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marchand V, Bourdin S, Charbonnel C, Rio E, Munos C, Campion L, et al. No impairment of quality of life 18 months after high-dose intensity-modulated radiotherapy for localized prostate cancer: a prospective study. Int J Radiat Oncol Biol Phys. 2010;77: 1053–1059. doi: 10.1016/j.ijrobp.2009.06.024 [DOI] [PubMed] [Google Scholar]
- 7.Yoshimura K, Kamoto T, Nakamura E, Segawa T, Kamba T, Takahashi T, et al. Health-related quality-of-life after external beam radiation therapy for localized prostate cancer: intensity-modulated radiation therapy versus conformal radiation therapy. Prostate Cancer Prostatic Dis. 2007;10: 288–292. doi: 10.1038/sj.pcan.4500923 [DOI] [PubMed] [Google Scholar]
- 8.Sanda MG, Dunn RL, Michalski J, Sandler HM, Northouse L, Hembroff L, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008;358: 1250–1261. doi: 10.1056/NEJMoa074311 [DOI] [PubMed] [Google Scholar]
- 9.Goineau A, Marchand V, Rigaud J, Bourdin S, Rio E, Campion L, et al. Prospective evaluation of quality of life 54 months after high-dose intensity-modulated radiotherapy for localized prostate cancer. Radiat. 2013;8: 53 doi: 10.1186/1748-717X-8-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lips IM, van Gils CH, van der Heide UA, Kruger AEB, van Vulpen M. Health-related quality of life 3 years after high-dose intensity-modulated radiotherapy with gold fiducial marker-based position verification. BJU Int. 2009;103: 762–767. doi: 10.1111/j.1464-410X.2008.08117.x [DOI] [PubMed] [Google Scholar]
- 11.Nguyen TD, Azria D, Brochon D, Poortmans P, Miller RC, Scandolaro L, et al. Curative external beam radiotherapy in patients over 80 years of age with localized prostate cancer: a retrospective rare cancer network study. Crit Rev Oncol Hematol. 2010;74: 66–71. doi: 10.1016/j.critrevonc.2009.04.004 [DOI] [PubMed] [Google Scholar]
- 12.Pignon T, Horiot JC, Bolla M, van Poppel H, Bartelink H, Roelofsen F, et al. Age is not a limiting factor for radical radiotherapy in pelvic malignancies. Radiother Oncol. 1997;42: 107–120. [DOI] [PubMed] [Google Scholar]
- 13.Soubeyran P, Bellera C, Goyard J, Heitz D, Curé H, Rousselot H, et al. Screening for vulnerability in older cancer patients: the ONCODAGE Prospective Multicenter Cohort Study. PloS One. 2014;9: e115060 doi: 10.1371/journal.pone.0115060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gerritse FL, Meulenbeld HJ, Roodhart JML, van der Velden AMT, Blaisse RJB, Smilde TJ, et al. Analysis of docetaxel therapy in elderly (⩾70years) castration resistant prostate cancer patients enrolled in the Netherlands Prostate Study. Eur J Cancer Oxf Engl 1990. 2013; doi: 10.1016/j.ejca.2013.06.008 [DOI] [PubMed] [Google Scholar]
- 15.Lee CE, Kilgour A, Lau YKJ. Efficacy of walking exercise in promoting cognitive-psychosocial functions in men with prostate cancer receiving androgen deprivation therapy. BMC Cancer. 2012;12: 324 doi: 10.1186/1471-2407-12-324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thorsen L, Nilsen TS, Raastad T, Courneya KS, Skovlund E, Fosså SD. A randomized controlled trial on the effectiveness of strength training on clinical and muscle cellular outcomes in patients with prostate cancer during androgen deprivation therapy: rationale and design. BMC Cancer. 2012;12: 123 doi: 10.1186/1471-2407-12-123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dale W. “Staging the aging” when considering androgen deprivation therapy for older men with prostate cancer. J Clin Oncol. 2009;27: 3420–3422. doi: 10.1200/JCO.2009.22.9104 [DOI] [PubMed] [Google Scholar]
- 18.Bekelman JE, Mitra N, Efstathiou J, Liao K, Sunderland R, Yeboa DN, et al. Outcomes after intensity-modulated versus conformal radiotherapy in older men with nonmetastatic prostate cancer. Int J Radiat Oncol Biol Phys. 2011;81: e325–334. doi: 10.1016/j.ijrobp.2011.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Namiki S, Ishidoya S, Kawamura S, Tochigi T, Arai Y. Quality of life among elderly men treated for prostate cancer with either radical prostatectomy or external beam radiation therapy. J Cancer Res Clin Oncol. 2010;136: 379–386. doi: 10.1007/s00432-009-0665-6 [DOI] [PubMed] [Google Scholar]
- 20.Nanda A, Chen M-H, Moran BJ, Braccioforte MH, Dosoretz D, Salenius S, et al. Predictors of prostate cancer-specific mortality in elderly men with intermediate-risk prostate cancer treated with brachytherapy with or without external beam radiation therapy. Int J Radiat Oncol Biol Phys. 2010;77: 147–152. doi: 10.1016/j.ijrobp.2009.04.085 [DOI] [PubMed] [Google Scholar]
- 21.Fung C, Dale W, Mohile SG. Prostate cancer in the elderly patient. J Clin Oncol. 2014;32: 2523–2530. doi: 10.1200/JCO.2014.55.1531 [DOI] [PubMed] [Google Scholar]
- 22.Osborne GEC, Appleyard SA, Gilbert DC, Jones CI, Lorimer C, Villanueva M, et al. Comprehensive Geriatric Assessment in Men Aged 70 Years or Older with Localised Prostate Cancer Undergoing Radical Radiotherapy. Clin Oncol R Coll Radiol G B. 2017;29: 609–616. doi: 10.1016/j.clon.2017.05.003 [DOI] [PubMed] [Google Scholar]
- 23.Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41: 237–248. [DOI] [PubMed] [Google Scholar]
- 24.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. STUDIES OF ILLNESS IN THE AGED. THE INDEX OF ADL: A STANDARDIZED MEASURE OF BIOLOGICAL AND PSYCHOSOCIAL FUNCTION. JAMA. 1963;185: 914–919. [DOI] [PubMed] [Google Scholar]
- 25.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9: 179–186. [PubMed] [Google Scholar]
- 26.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12: 189–198. [DOI] [PubMed] [Google Scholar]
- 27.Clément JP, Nassif RF, Léger JM, Marchan F. [Development and contribution to the validation of a brief French version of the Yesavage Geriatric Depression Scale]. L’Encephale. 1997;23: 91–99. [PubMed] [Google Scholar]
- 28.Guigoz Y, Lauque S, Vellas BJ. Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment. Clin Geriatr Med. 2002;18: 737–757. [DOI] [PubMed] [Google Scholar]
- 29.Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil. 1986;67: 387–389. [PubMed] [Google Scholar]
- 30.Beckendorf V, Guerif S, Le Prisé E, Cosset J-M, Bougnoux A, Chauvet B, et al. 70 Gy versus 80 Gy in localized prostate cancer: 5-year results of GETUG 06 randomized trial. Int J Radiat Oncol Biol Phys. 2011;80: 1056–1063. doi: 10.1016/j.ijrobp.2010.03.049 [DOI] [PubMed] [Google Scholar]
- 31.Carrie C, Hasbini A, de Laroche G, Richaud P, Guerif S, Latorzeff I, et al. Salvage radiotherapy with or without short-term hormone therapy for rising prostate-specific antigen concentration after radical prostatectomy (GETUG-AFU 16): a randomised, multicentre, open-label phase 3 trial. Lancet Oncol. 2016;17: 747–756. doi: 10.1016/S1470-2045(16)00111-X [DOI] [PubMed] [Google Scholar]
- 32.Sargos P, Guerif S, Latorzeff I, Hennequin C, Pommier P, Lagrange J-L, et al. Definition of lymph node areas for radiotherapy of prostate cancer: A critical literature review by the French Genito-Urinary Group and the French Association of Urology (GETUG-AFU). Cancer Treat Rev. 2015;41: 814–820. doi: 10.1016/j.ctrv.2015.10.005 [DOI] [PubMed] [Google Scholar]
- 33.PROFIT—Prostate Fractionated Irradiation Trial—ClinicalKey [Internet]. [cited 24 Aug 2016]. https://www.clinicalkey.fr/#!/content/clinical_trial/24-s2.0-NCT00304759
- 34.Michalski JM, Gay H, Jackson A, Tucker SL, Deasy JO. Radiation dose-volume effects in radiation-induced rectal injury. Int J Radiat Oncol Biol Phys. 2010;76: S123–129. doi: 10.1016/j.ijrobp.2009.03.078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Viswanathan AN, Yorke ED, Marks LB, Eifel PJ, Shipley WU. Radiation dose-volume effects of the urinary bladder. Int J Radiat Oncol Biol Phys. 2010;76: S116–122. doi: 10.1016/j.ijrobp.2009.02.090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Martin JM, Supiot S, Berthold DR. Pharmacotherapeutic management of locally advanced prostate cancer: current status. Drugs. 2011;71: 1019–1041. doi: 10.2165/11591500-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 37.Osoba D, Rodrigues G, Myles J, Zee B, Pater J. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol. 1998;16: 139–144. doi: 10.1200/JCO.1998.16.1.139 [DOI] [PubMed] [Google Scholar]
- 38.Guren MG, Dueland S, Skovlund E, Fosså SD, Poulsen JP, Tveit KM. Quality of life during radiotherapy for rectal cancer. Eur J Cancer Oxf Engl 1990. 2003;39: 587–594. [DOI] [PubMed] [Google Scholar]
- 39.Dinh KT, Reznor G, Muralidhar V, Mahal BA, Nezolosky MD, Choueiri TK, et al. Association of Androgen Deprivation Therapy With Depression in Localized Prostate Cancer. J Clin Oncol. 2016;34: 1905–1912. doi: 10.1200/JCO.2015.64.1969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Aparicio T, Jouve J-L, Teillet L, Gargot D, Subtil F, Le Brun-Ly V, et al. Geriatric factors predict chemotherapy feasibility: ancillary results of FFCD 2001–02 phase III study in first-line chemotherapy for metastatic colorectal cancer in elderly patients. J Clin Oncol. 2013;31: 1464–1470. doi: 10.1200/JCO.2012.42.9894 [DOI] [PubMed] [Google Scholar]
- 41.Caillet P, Canoui-Poitrine F, Vouriot J, Berle M, Reinald N, Krypciak S, et al. Comprehensive geriatric assessment in the decision-making process in elderly patients with cancer: ELCAPA study. J Clin Oncol. 2011;29: 3636–3642. doi: 10.1200/JCO.2010.31.0664 [DOI] [PubMed] [Google Scholar]
- 42.Terret C, Albrand G, Droz JP. Geriatric assessment in elderly patients with prostate cancer. Clin Prostate Cancer. 2004;2: 236–240. [DOI] [PubMed] [Google Scholar]
- 43.Soubeyran P, Fonck M, Blanc-Bisson C, Blanc J-F, Ceccaldi J, Mertens C, et al. Predictors of early death risk in older patients treated with first-line chemotherapy for cancer. J Clin Oncol. 2012;30: 1829–1834. doi: 10.1200/JCO.2011.35.7442 [DOI] [PubMed] [Google Scholar]
- 44.Blanc-Bisson C, Fonck M, Rainfray M, Soubeyran P, Bourdel-Marchasson I. Undernutrition in elderly patients with cancer: target for diagnosis and intervention. Crit Rev Oncol Hematol. 2008;67: 243–254. doi: 10.1016/j.critrevonc.2008.04.005 [DOI] [PubMed] [Google Scholar]
- 45.Liuu E, Canouï-Poitrine F, Tournigand C, Laurent M, Caillet P, Le Thuaut A, et al. Accuracy of the G-8 geriatric-oncology screening tool for identifying vulnerable elderly patients with cancer according to tumour site: the ELCAPA-02 study. J Geriatr Oncol. 2014;5: 11–19. doi: 10.1016/j.jgo.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 46.Wortel RC, Incrocci L, Pos FJ, van der Heide UA, Lebesque JV, Aluwini S, et al. Late Side Effects After Image Guided Intensity Modulated Radiation Therapy Compared to 3D-Conformal Radiation Therapy for Prostate Cancer: Results From 2 Prospective Cohorts. Int J Radiat Oncol Biol Phys. 2016;95: 680–689. doi: 10.1016/j.ijrobp.2016.01.031 [DOI] [PubMed] [Google Scholar]
- 47.Cozzarini C, Fiorino C, Da Pozzo LF, Alongi F, Berardi G, Bolognesi A, et al. Clinical factors predicting late severe urinary toxicity after postoperative radiotherapy for prostate carcinoma: a single-institute analysis of 742 patients. Int J Radiat Oncol Biol Phys. 2012;82: 191–199. doi: 10.1016/j.ijrobp.2010.09.027 [DOI] [PubMed] [Google Scholar]
- 48.Longobardi B, Berardi G, Fiorino C, Alongi F, Cozzarini C, Deli A, et al. Anatomical and clinical predictors of acute bowel toxicity in whole pelvis irradiation for prostate cancer with Tomotherapy. Radiother Oncol. 2011;101: 460–464. doi: 10.1016/j.radonc.2011.07.014 [DOI] [PubMed] [Google Scholar]
- 49.Perna L, Alongi F, Fiorino C, Broggi S, Cattaneo Giovanni M, Cozzarini C, et al. Predictors of acute bowel toxicity in patients treated with IMRT whole pelvis irradiation after prostatectomy. Radiother Oncol. 2010;97: 71–75. doi: 10.1016/j.radonc.2010.02.025 [DOI] [PubMed] [Google Scholar]
- 50.Langston B, Armes J, Levy A, Tidey E, Ream E. The prevalence and severity of fatigue in men with prostate cancer: a systematic review of the literature. Support Care Cancer. 2013;21: 1761–1771. doi: 10.1007/s00520-013-1751-5 [DOI] [PubMed] [Google Scholar]
- 51.Lilleby W, Stensvold A, Dahl AA. Fatigue and other adverse effects in men treated by pelvic radiation and long-term androgen deprivation for locally advanced prostate cancer. Acta Oncol. 2016;55: 807–813. doi: 10.3109/0284186X.2015.1127417 [DOI] [PubMed] [Google Scholar]
- 52.Donovan JL, Hamdy FC, Lane JA, Mason M, Metcalfe C, Walsh E, et al. Patient-Reported Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. N Engl J Med. 2016; doi: 10.1056/NEJMoa1606221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zelefsky MJ, Poon BY, Eastham J, Vickers A, Pei X, Scardino PT. Longitudinal assessment of quality of life after surgery, conformal brachytherapy, and intensity-modulated radiation therapy for prostate cancer. Radiother Oncol. 2016;118: 85–91. doi: 10.1016/j.radonc.2015.11.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kerleau C, Guizard A-V, Daubisse-Marliac L, Heutte N, Mercier M, Grosclaude P, et al. Long-term quality of life among localised prostate cancer survivors: QALIPRO population-based study. Eur J Cancer Oxf Engl 1990. 2016;63: 143–153. doi: 10.1016/j.ejca.2016.05.020 [DOI] [PubMed] [Google Scholar]
- 55.Geinitz H, Thamm R, Scholz C, Heinrich C, Prause N, Kerndl S, et al. Longitudinal analysis of quality of life in patients receiving conformal radiation therapy for prostate cancer. Strahlenther Onkol. 2010;186: 46–52. doi: 10.1007/s00066-009-2023-7 [DOI] [PubMed] [Google Scholar]
- 56.Gajra A, Loh KP, Hurria A, Muss H, Maggiore R, Dale W, et al. Comprehensive Geriatric Assessment-Guided Therapy Does Improve Outcomes of Older Patients With Advanced Lung Cancer. J Clin Oncol; doi: 10.1200/JCO.2016.67.5926 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.