Abstract
There is a suspected but unproven association between long-term exposure to ambient air pollution and mental health. The aim of this study is to investigate the association between long-term exposure to ambient air pollution and subjective stress, depressive disorders, health-related quality of life (QoL) and suicide. We selected 124,205 adults from the Korean Community Health Survey in 2013 who were at least 19 years old and who had lived in their current domiciles for > five years. Based on the computer-assisted personal interviews to measure subjective stress in daily life, EuroQoL-5 dimensions, depression diagnosis by a doctor, suicidal ideation, and suicidal attempts, we evaluated the risk of mental disorders using multiple logistic regression analysis according to the quartiles of air pollutants, such as particulate matter <10μm (PM10), nitrogen dioxide (NO2), carbon monoxide (CO), and sulfur dioxide, using yearly average concentration between August 2012 and July 2013. The prevalence of high stress, poor QoL, depressiveness, diagnosis of depression, and suicide ideation was positively associated with high concentrations of PM10, NO2, and CO after adjusting for confounding factors. Men were at increased risk of stress, poor QoL, and depressiveness from air pollution exposure than were women. The risk of higher stress or poor QoL in subjects < age 65 increased with air pollution more than did that in subjects ≥ age 65. Long-term exposure to ambient air pollution may be an independent risk factor for mental health disorders ranging from subjective stress to suicide ideation.
Introduction
Ambient air pollution is composed of a heterogeneous mixture of compounds, including particulate matter (PM), nitrogen dioxide (NO2), carbon monoxide (CO), and sulfur dioxide (SO2). These particles are composed of both solid and liquid components that originate from multiple sources, including vehicle exhaust, road dust, and windblown soil [1].
A growing body of evidence indicates that elevated levels of air pollution are associated with mental disorders such as depression and suicide. Elderly subjects experienced the aggravation of their depressive symptoms after 3-day exposure to air pollutants [2]. Emergency department visits for depressive episode were associated with increased levels of air pollutants during 0–3 days in 4,985 Korean elderly patients with cardiovascular or respiratory disease [3]. Emergency department visits with depressive disorders and suicide attempts showed associations with CO, NO2, SO2, and PM10 in 27,047 Canadians [4, 5]. However, these associations were different according to seasons [6] or represent only sort-term exposure to air pollutants. Although a few studies have addressed the incidence of mental health disorders in patients with long-term exposure to air pollution, the association between newly diagnosed major depressive disorder and PM ≤ 2.5μm has been minimally assessed [7]. A study of increased suicide rate after 4 weeks’ exposures to air pollution did not adjust for known risk factors [8]. Moreover, there is inconsistent evidence that ambient air pollution is associated with depressive symptoms among older adults ≥ 65 years of age living in a metropolitan area of U.S. or European general population [9, 10].
In other words, there was insufficient evidence to support an association between long-term exposure to ambient air pollution and mental health status in general population. Therefore, for this study, we used nationwide population data to investigate the association between long-term exposure to ambient air pollution and mental health status, including subjective stress, depressive disorders, health-related quality of life and suicide.
Materials and methods
Study participants
For this study, we evaluated data from the Korean Community Health Survey (KCHS) 2013, which has been collected by the Korea Centers for Disease Control and Prevention annually since 2008. We collected the data via computer-assisted personal interviews with 900 people in each of the 253 community units between August and October in 2013, including 17 metropolitan areas and provinces. Study participants aged 19 or older in each area who were selected by the probability proportional sampling method and the systematic sampling method [11]. Among total surveyed 228,781 adults in 2013, we selected subjects who had lived in the same domicile for > five years. After we matched the domicile code of participants and the location code of air pollution surveillance station because of using same code system, we ultimately analyzed 124,205 persons (unweighted number).
Air pollutant variables
We obtained the daily average concentrations of hourly measured particulate matter <10 μm (PM10), NO2, CO, and SO2 as air pollutant variables at nationwide air pollution surveillance stations from the Korean Air Pollutants Emission Service. We calculated quartiles of air pollutants using yearly average concentration between August 2012 and July 2013. These air pollutant measurements followed the standard reference protocol of the Korean Air Pollutants Emission Service [12]. PM10 had been measured using beta-ray attenuation method (MEZUS-610, KENTEK, Daejeon, Korea). NO2 had been measured using chemiluminescence method (MEZUS-210, KENTEK). CO had been measured using non-dispersive infrared (MEZUS-310, KENTEK). SO2 had been measured using UV fluorescence (MEZUS-110, KENTEK). We obtained meteorological data, including temperature, rainfall, and wind speed, from the National Meteorological Office in the same period [13, 14].
Mental health variables
The KCHS surveyed mental health-related indicators. These indicators were defined as subjective daily stress, the EuroQol-5 dimensions (EQ-5D) index, the presence or absence of depressiveness (such as a feeling of sadness or hopelessness lasting more than two consecutive weeks), physician’s diagnosis of depression, suicidal ideation, or a suicide attempt during the past year. We assessed subjective stress on a four-point rating scale (“very much,” “a lot,” “a little bit,” “rarely”). Ultimately, we defined participants with subjective stress as those who responded with “very much” or “a lot” of stress. The EQ-5D index is broadly applied to evaluate health-related quality of life in five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression), and each dimension has one of three possible responses (no problems, some problems, or extreme problems). The EQ-5D index generates a single value from each dimension using the following weighted health scores: worst possible = 0; best possible = 1, and a score below zero equates to a health status worse than death [15]. We defined the fourth quartile of the EQ-5D index (which was 0.913 in this study) as a group with poor quality of life.
Other variables
We categorized patients as non-smokers, former smokers (smoked at one time but not currently), or current smokers (smoking daily or intermittently at the time of the survey). We defined alcohol consumption by drinking frequency of one time per week. We defined physical activity by intensity and frequency. Active group was doing moderate intense activity ≥ three times per week or vigorous activity ≥ one time per week. Inactive group was defined when participant was not met these criteria. Vigorous physical activity included running (jogging), climbing, fast biking, fast swimming, soccer, basketball, jumping rope, squash, or singles tennis, as well as occupational activities such as carrying heavy objects [16]. We also obtained the following demographic information: years of education (< 9, 9–12, or > 12); marital status (married/with partner, not married, or divorced/widowed); current employment status (employed or retired/unemployed); household income (< 7,000,000 won/year or ≥ 7,000,000 won/year); hours of sleep duration (< 7, 7–9, or > 9); religion (yes or no); residence (rural or urban); and medical history according to physicians’ diagnoses, including hypertension, diabetes mellitus, dyslipidemia, stroke, myocardial infarction, ischemic heart disease, asthma, and arthritis. We divided participants’ length of residence into four groups, 5 ≤ Q1 < 10 years, 10 ≤ Q2 < 15 years, 15 ≤ Q3 < 20 years, or Q4 ≥ 20 years, after excluding those who had lived in their areas for < 5 years.
Ethical considerations
The institutional review board (IRB) at the Korean Centers for Disease Control and Prevention approved the study protocol, and all of the participants provided written informed consent. The IRB at Gangnam Severance Hospital, Yonsei University College of Medicine approved this study as well (IRB File Number: 3-2017-0153).
Statistical analyses
We conducted all analyses considering the survey weight. Continuous variables are presented as means with standard errors, and categorical variables are presented as percentages. We conducted a univariate analysis to find out the association between the characteristics of participants and mental health status. We then evaluated mental disorder risk using multiple logistic regression analysis after adjusting for age, sex, smoking, drinking, physical activity, education, marital status, employment, household income, sleep duration, residence, and medical history (hypertension, diabetes mellitus, dyslipidemia, stroke, myocardial infarction, ischemic heart disease, asthma, arthritis). We conducted stratified analyses to investigate the possible effect modification by sex and age (divided by age 65) in subgroup analysis. EQ-5D index was skewed distributed. We showed the meteorological data including mean temperature, rainfall and wind speed and the level of air pollutant in 2013 in S1 Table. The nationwide values of ambient air pollutants are also presented as means with standard deviations, medians and ranges in S1 Table. Therefore, it was analyzed using logarithmic transformation. We conducted all analyses using SAS software 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
The demographic, socioeconomic characteristics, health-related behaviors, and past medical history of the study population are summarized in Table 1. The mean age was 48.2 years, and the study population was 50.1% women. Approximately 70% of participants had lived in the same domicile for > 15 years.
Table 1. Baseline characteristics of study population.
| Variables | Total | Men | Women |
|---|---|---|---|
| Age, years | 48.2±0.04 | 47.0±0.06 | 49.4±0.05 |
| Smoking | |||
| Never | 61.2 | 41.6 | 80.7 |
| Former | 16.1 | 30.9 | 1.3 |
| Current | 22.7 | 27.5 | 18.0 |
| Alcohol intake | |||
| Never or less than one time per week | 87.1 | 85.4 | 88.8 |
| More than one time per week | 12.9 | 15.6 | 11.2 |
| Physical activity | |||
| Active | 44.5 | 46.2 | 42.8 |
| Inactive | 55.5 | 53.8 | 57.2 |
| Education | |||
| < 9 years | 22.4 | 19.1 | 25.7 |
| 9–12 years | 31.8 | 33.0 | 30.6 |
| > 12 years | 45.9 | 47.9 | 43.7 |
| Marital status | |||
| Married/with partner | 65.0 | 67.3 | 62.7 |
| Not married | 22.9 | 26.9 | 18.9 |
| Divorced/widowed | 12.1 | 5.8 | 18.4 |
| Employment | |||
| Employed | 62.8 | 77.5 | 48.2 |
| Retired/unemployed | 37.2 | 22.5 | 51.8 |
| Household income | |||
| < 7,000,000 won/year | 70.0 | 69.0 | 70.9 |
| ≥7,000,000 won/year | 30.0 | 31.0 | 29.1 |
| Sleep time, hours | |||
| < 7 hours | 48.7 | 47.6 | 49.8 |
| 7–9 hours | 48.1 | 48.7 | 47.5 |
| > 9 hours | 3.2 | 3.7 | 2.7 |
| Religion, yes | 28.2 | 20.6 | 35.7 |
| Residence of urban | 79.7 | 79.6 | 79.8 |
| Hypertension | 19.5 | 19.3 | 19.7 |
| Diabetes mellitus | 7.4 | 8.0 | 6.9 |
| Dyslipidemia | 11.2 | 10.7 | 11.7 |
| Stroke | 1.4 | 1.6 | 1.3 |
| Myocardial infarction | 1.0 | 1.2 | 0.8 |
| Ischemic heart disease | 1.4 | 1.3 | 1.5 |
| Asthma | 2.4 | 2.1 | 2.7 |
| Arthritis | 9.6 | 4.1 | 15.0 |
| Length of residence | |||
| 5–10 years | 14.4 | 13.9 | 14.9 |
| 10–15 years | 13.7 | 13.2 | 14.2 |
| 15–20 years | 11.0 | 10.9 | 11.1 |
| ≥ 20 years | 60.8 | 62.0 | 59.8 |
| Subjective stress | 27.5 | 32.0 | 23.0 |
| Poor quality of life | 21.7 | 18.4 | 32.9 |
| Depressiveness | 6.2 | 4.2 | 8.0 |
| Depression diagnosis | 2.5 | 1.3 | 3.7 |
| Suicidal ideation | 8.8 | 6.6 | 11.3 |
| Suicide attempt | 0.4 | 0.4 | 0.5 |
Data was shown by mean and standard error or percentage. Physical active group was defined as moderate intense activity ≥ 3 times per week or vigorous activity ≥1 time per week. Inactive group was not met these criteria. Length of residence with same domicile was counted. Medical history was defined as a physician’s diagnosis. The subjects with subjective stress were defined as those responding with “very much” or “a lot” of stress. The fourth quartile of the EuroQol-5 dimensions index was defined as a group with poor quality of life.
The association between the characteristics of participants and mental health status was shown in Table 2. Mental health status was associated with various sociodemographic feature, health-related behaviors and medical factor. The risk of subjective stress decreased older age, education less than 12 years or unemployed participants. Subjects with current smoking and alcohol drinking more than one time per week represented a low risk of depressiveness and depression diagnosis by doctor.
Table 2. Univariate analysis for the association between the characteristics of participant and mental health status.
| Subjective stress | Poor quality of life | Depressiveness | Depression diagnosis by doctor | Suicidal ideation | Suicide attempt | |
|---|---|---|---|---|---|---|
| Age | 0.991 (0.990,0.992) | 1.049(1.048,1.051) | 1.010 (1.009,1.012) | 1.021 (1.019,1.024) | 1.024 (1.022,1.025) | 1.007 (1.001,1.013) |
| Women | 1.005 (0.977,1.034) | 2.325 (2.256,2.396) | 1.926 (1.819,2.039) | 2.765 (2.523,3.029) | 1.731 (1.654,1.811) | 1.301 (1.059,1.600) |
| Current smoking | 1.591 (1.539,1.646) | 1.713 (1.645,1.784) | 0.916 (0.857,0.980) | 0.783 (0.707,0.867) | 0.996 (0.944,1.051) | 2.090 (1.699,2.573) |
| Alcohol (≥1/week) | 1.303 (1.259,1.348) | 1.619 (1.555,1.686) | 0.880 (0.822,0.943) | 0.632 (0.566,0.705) | 0.951 (0.900,1.004) | 1.570 (1.254,1.967) |
| Physically inactive | 1.101 (1.068,1.134) | 1.757 (1.700,1.815) | 1.122 (1.061,1.187) | 1.381 (1.270,1.502) | 1.323 (1.264,1.386) | 1.454 (1.179,1.974) |
| Education, ≤ 12 years |
0.939 (0.911,0.967) | 2.818 (2.720,2.921) | 1.594 (1.502,1.692) | 2.280 (2.070,2.511) | 2.273 (2.155,2.398) | 3.100 (2.414,3.980) |
| Divorced/widowed | 1.091 (1.057,1.125) | 1.324 (1.282,1.368) | 1.405 (1.330,1.485) | 1.395 (1.284,1.516) | 1.309 (1.250,1.371) | 1.589 (1.297,1.947) |
| Unemployed | 0.728 (0.706,0.750) | 2.949 (2.858,3.044) | 1.759 (1.665,1.859) | 2.784 (2.566,3.020) | 1.736 (1.659,1.816) | 2.010 (1.638,2.468) |
| Household income < 7,000,000 |
1.077 (1.038,1.117) | 1.714 (1.643,1.788) | 1.453 (1.349,1.564) | 1.728 (1.542,1.936) | 1.608 (1.509,1.713) | 2.312 (1.693,3.158) |
| Sleep time <7,or ≥9 |
1.518 (1.474,1.564) | 1.443 (1.399,1.488) | 1.493 (1.412,1.579) | 1.586 (1.461,1.721) | 1.509 (1.443,1.579) | 1.952 (1.584,2.405) |
| Residence of urban | 1.030 (0.989,1.073) | 0.795 (0.761,0.829) | 1.083 (1.005,1.167) | 1.069 (0.949,1.204) | 0.847 (0.797,0.900) | 0.888 (0.686,1.149) |
| Hypertension | 0.962 (0.918,1.018) | 2.905 (2.810,3.003) | 1.381 (1.299,1.469) | 1.883 (1.731,2.049) | 1.793 (1.708,1.882) | 1.559 (1.246.1.950) |
| Diabetes Mellitus | 1.023 (0.969,1.079) | 2.754 (2.625,2.888) | 1.512 (1.390,1.645) | 2.056 (1.829,2.310) | 1.956 (1.828,2.093) | 2.205 (1.636,2.973) |
| Dyslipidemia | 1.175 (1.125,1.228) | 2.170 (2.082,2.261) | 1.658 (1.546,1.779) | 2.747 (2.511,3.006) | 1.776 (1.674,1.885) | 1.614 (1.260.2.068) |
| Stroke | 1.316 (1.182,1.465) | 9.142 (8.160,10.243) | 2.523 (2.172,2.931) | 3.513 (2.941,4.197) | 3.402 (3.024,3.828) | 4.156 (2.718,6.353) |
| Myocardial infarction | 1.158 (1.020,1.316) | 4.391 (3.903,4.940) | 2.297 (1.938,2.723) | 2.730 (2.158,3.453) | 2.733 (2.354,3.172) | 3.237 (1.847,5.675) |
| Ischemic heart disease | 1.142 (1.025,1.272) | 4.276 (3.879,4.713) | 2.195 (1.874,2.571) | 3.885 (3.267,4.621) | 2.712 (2.397,3.069) | 2.344 (1.357,4.049) |
| Asthma | 1.495 (1.368,1.635) | 2.844 (2.615,3.094) | 2.629 (2.327,2.970) | 3.073 (2.594,3.642) | 2.763 (2.498,3.055) | 2.554 (1.681,3.882) |
| Arthritis | 1.219 (1.165,1.276) | 7.433 (7.114,7.767) | 2.440 (2.279,2.613) | 3.747 (3.434,4.088) | 2.949 (2.789,3.118) | 2.405 (1.876,3.083) |
Physically inactive group was defined when participant was doing moderate intense activity < three times per week or vigorous activity < one time per week; years of education (≤ 12, or > 12); marital status (married/with partner, not married, or divorced/widowed); current employment status (employed or retired/unemployed); household income (< 7,000,000 won/year or ≥ 7,000,000 won/year); hours of sleep duration (7–9, and <7 or > 9); residence (rural or urban); and medical history according to physicians’ diagnoses, including hypertension, diabetes mellitus, dyslipidemia, stroke, myocardial infarction, ischemic heart disease, asthma, and arthritis.
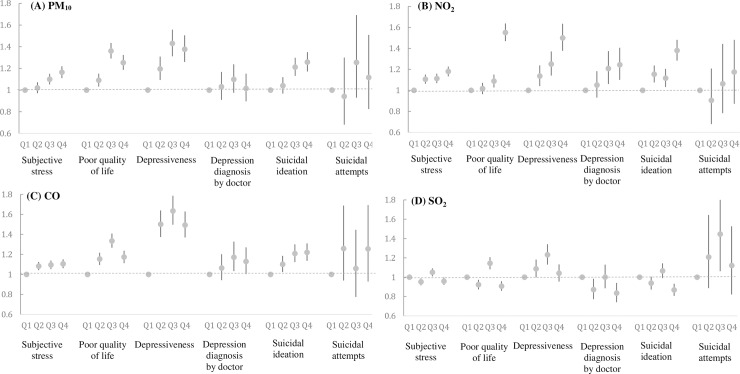
The risk of a mental disorder according to the air pollutant quartile is represented in Fig 1. After we adjusted for confounding factors, there were positive associations between PM10, NO2, CO exposure and mental health status except suicidal attempts. The risk of depressiveness increased at the third quartile of CO exposure (odds ratio [OR]; 95% confidence interval [CI]: 1.635(1.497, 1.786)), the highest quartile of NO2 (1.501(1.377, 1.635)) and the third quartile of PM10 (1.335(1.267, 1.408)). There was no association between SO2 exposure and mental health status.
Fig 1. The odds ratios and 95% confidence intervals of a mental health disorder according to the air pollutant quartile.
(A) PM10 (B) NO2 (C) CO (D) SO2.
Compared with women, men had increased prevalence of subjective stress with exposure to PM10 and prevalence of poor QoL with exposure to CO and SO2 in Table 3. And depressiveness in men also increased with exposure to NO2, CO and SO2. The risk of depression diagnosis by doctor and suicidal ideation had no difference according to sex (Ps > 0.05). The effect of SO2 was inconsistent according to the quartiles.
Table 3. Air pollution and mental health status according to sex.
| Subjective stress | Poor quality of life | Depressiveness | Depression diagnosis by doctor | Suicidal ideation | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | |
| PM10 | ||||||||||
| Q4 | 1.121(1.062, 1.183) | 1.089(1.036,1.145) | 1.256(1.175,1.337) | 1.236(1.137, 1.344) | 1.342(1.158,1.556) | 1.385(1.248,1.536) | 0.978(0.758,1.263) | 1.022(0.886,1.179) | 1.241(1.109,1.388) | 1.256(1.154,1.368) |
| Q3 | 1.078(1.028,1.131) | 1.033(0.981, 1.087) | 1.360(1.278,1.446) | 1.338(1.233, 1.451) | 1.442(1.250,1.662) | 1.409(1.275,1.557) | 1.076(0.849,1.363) | 1.101(0.960,1.262) | 1.246(1.117,1.391) | 1.175(1.081,1.277) |
| Q2 | 1.005(0.955,1.058) | 0.998(0.945, 1.053) | 1.088(1.020,1.159) | 1.078(0.989, 1.175) | 1.208(1.040,1.403) | 1.184(1.066,1.314) | 1.034(0.804,1.331) | 1.026(0.890,1.182) | 1.013(0.899,1.141) | 1.051(0.965,1.144) |
| Q1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| p-inter action | 0.009 | 0.593 | 0.741 | 0.969 | 0.583 | |||||
| NO2 | ||||||||||
| Q4 | 1.205(1.140, 1.274) | 1.161(1.104,1.220) | 1.587(1.458, 1.727) | 1.518(1.426,1.617) | 1.707(1.479,1.970) | 1.389(1.252,1.542) | 1.280(1.010, 1.623) | 1.223(1.066,1.403) | 1.319(1.177,1.478) | 1.402(1.286,1.529) |
| Q3 | 1.119(1.057, 1.184) | 1.108(1.053,1.167) | 1.140(1.042, 1.274) | 1.057(0.989,1.129) | 1.440(1.238,1.675) | 1.158(1.038,1.291) | 1.125(0.879, 1.440) | 1.241(1.069,1.441) | 1.074(0.957,1.205) | 1.134(1.031,1.247) |
| Q2 | 1.139(1.079, 1.202) | 1.072(1.021,1.126) | 1.054(0.972, 1.142) | 0.996(0.937,1.059) | 1.146(0.991,1.325) | 1.128(1.017,1.251) | 1.005(0.783, 1.290) | 1.059(0.929,1.208) | 1.045(0.943,1.158) | 1.197(1.098,1.304) |
| Q1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| p-inter action | 0.054 | 0.391 | 0.011 | 0.765 | 0.205 | |||||
| CO | ||||||||||
| Q4 | 1.123(1.064, 1.186) | 1.091(1.038,1.147) | 1.196(1.123,1.274) | 1.135(1.045, 1.232) | 1.535(1.338,1.663) | 1.524(1.375,1.689) | 1.204(0.946, 1.533) | 1.100(0.964,1.256) | 1.318 (1.178,1.476) | 1.162(1.069,1.263) |
| Q3 | 1.111(1.051, 1.173) | 1.085(1.032,1.140) | 1.433(1.346,1.526) | 1.186(1.091, 1.290) | 1.697(1.465,1.966) | 1.584(1.424,1.763) | 1.091(0.852, 1.397) | 1.197(1.039,1.378) | 1.290(1.148, 1.450) | 1.152(1.057, 1.256) |
| Q2 | 1.089(1.032, 1.150) | 1.079(1.027,1.134) | 1.212(1.139,1.290) | 1.065(0.980, 1.158) | 1.389(1.176,1.593) | 1.369(1.112,1.643) | 0.999(0.776, 1.286) | 1.086(0.951,1.241) | 1.163(1.034, 1.307) | 1.061(0.975, 1.155) |
| Q1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| p-inter action | 0.580 | <0.001 | 0.045 | 0.633 | 0.324 | |||||
| SO2 | ||||||||||
| Q4 | 0.944(0.894, 0.997) | 0.973(0.925,1.023) | 0.909(0.852,0.970) | 0.905(0.835,0.981) | 1.146(0.933,1.323) | 0.986(0.891,1.091) | 0.944(0.738, 1.208) | 0.804(0.701,0.922) | 0.879(0.785,0.984) | 0.861(0.791,0.938) |
| Q3 | 1.042(0.986, 1.101) | 1.059(1.008,1.114) | 1.145(1.074,1.220) | 1.129(1.037,1.229) | 1.345(1.162,1.557) | 1.171(1.059,1.294) | 1.082(0.848, 1.379) | 0.977(0.849,1.125) | 1.091(0.972,1.224) | 1.045(0.959,1.139) |
| Q2 | 0.939(0.890, 0.991) | 0.962(0.917,1.010) | 0.972(0.912,1.035) | 0.851(0.783,0.925) | 1.013(0.876,1.172) | 1.131(1.025,1.248) | 1.018(0.797, 1.302) | 0.834(0.729,0.955) | 0.909(0.812,1.018) | 0.962(0.885,1.047) |
| Q1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| p-inter action | 0.738 | 0.017 | 0.002 | 0.527 | 0.488 | |||||
Bold characteristics means P–value <0.05 among the values with p-interaction < 0.05. EQ-5D index was analyzed by logarithmic transformation. Adjustment for age, smoking, drinking, physical activity, education, marital status, employment, household income, sleep duration, residence and medical history (hypertension, diabetes mellitus, dyslipidemia, stroke, myocardial infarction, ischemic heart disease, asthma, arthritis).
The risk of higher stress and poor QoL with PM10 in subjects < age 65 were significantly increased than that in subjects ≥ age 65 in Table 4. Subjects < age 65 with high quartiles of PM10, NO2, CO and SO2 had a higher risk of poor QoL than subjects ≥ age 65. In the higher levels of air pollutants, the risk of depressiveness, depression diagnosis by doctor and suicidal ideation increased, however, there had no significant difference according to age 65.
Table 4. Air pollution and mental health status according to age.
| Subjective stress | Poor quality of life | Depressiveness | Depression diagnosis by doctor | Suicidal ideation | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age ≥ 65 | Age < 65 | Age ≥ 65 | Age < 65 | Age ≥ 65 | Age < 65 | Age ≥ 65 | Age < 65 | Age ≥ 65 | Age < 65 | |
| PM10 | ||||||||||
| Q4 | 0.940(0.872, 1.014) | 1.150(1.101,1.201) | 0.949(0.867, 1.038) | 1.338(1.277,1.456) | 1.329(1.137,1.555) | 1.383(1.246,1.535) | 0.866(0.707,1.059) | 1.061(0.910,1.237) | 1.192(1.067, 1.331) | 1.269(1.165,1.382) |
| Q3 | 0.986(0.918, 1.060) | 1.062(1.018,1.108) | 1.101(1.012, 1.198) | 1.473(1.383,1.569) | 1.327(1.142,1.542) | 1.446(1.310,1.600) | 0.907(0.752,1.049) | 1.154(0.996,1.338) | 1.211(1.094, 1.341) | 1.206(1.108,1.312) |
| Q2 | 0.919(0.854, 0.988) | 1.025(0.979,1.073) | 1.006(0.926, 1.094) | 1.122(1.049,1.201) | 1.189(1.028,1.376) | 1.200(1.079,1.334) | 1.027(0.856,1.232) | 1.022(0.874,1.194) | 1.054(0.945, 1.175) | 1.033(0.945,1.130) |
| Q1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| p-inter action | <0.001 | <0.001 | 0.688 | 0.218 | 0.765 | |||||
| NO2 | ||||||||||
| Q4 | 1.182(1.095,1.277) | 1.171(1.120,1.225) | 1.203(1.101,1.314) | 1.706(1.598,1.821) | 1.550(1.341,1.792) | 1.478(1.337,1.633) | 1.071(0.884,1.299) | 1.289(1.107,1.501) | 1.319(1.177,1.478) | 1.702(1.286,1.529) |
| Q3 | 1.189(1.101,1.284) | 1.093(1.044,1.144) | 0.843(0.771,0.923) | 1.207(1.127,1.294) | 1.334(1.144,1.556) | 1.223(1.098,1.362) | 1.123(0.929,1358) | 1.231(1.049,1.444) | 1.074(0.957,1.205) | 1.134(1.031,1.247) |
| Q2 | 1.096(1.023,1.174) | 1.109(1.061,1.160) | 0.932(0.861,1.009) | 1.068(0.999,1.141) | 1.101(0.963,1.258) | 1.139(1.027,1.262) | 0.974(0.818,1.153) | 1.080(0.929,1.254) | 1.045(0.943,1.158) | 1.197(1.098,1.304) |
| Q1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| p-inter action | 0.060 | <0.001 | 0.662 | 0.893 | 0.181 | |||||
| CO | ||||||||||
| Q4 | 1.091(1.014,1.173) | 1.111(1.063,1.162) | 0.971(0.890,1.061) | 1.249(1.172,1.332) | 1.626(1.398,1.891) | 1.463(1.322,1.618) | 1.213(1.006,1.462) | 1.110(0.961,1.284) | 1.115(0.999, 1.244) | 1.255(1.152,1.368) |
| Q3 | 1.060(0.984,1.142) | 1.098(1.051,1.148) | 0.999(0.916,1.090) | 1.470(1.379,1.567) | 1.600(1.368,1.872) | 1.635(1.475,1.811) | 1.094(0.898,1.331) | 1.187(1.020,1.382) | 1.145(1.027, 1.277) | 1.229(1.125,1.343) |
| Q2 | 1.097(1.019,1.182) | 1.069(1.025,1.116) | 0.997(0.913,1.089) | 1.234(1.157,1.316) | 1.473(1.260,1.721) | 1.504(1.359,1.666) | 1.103(0.905,1.343) | 1.050(0.905,1.218) | 1.027(0.920, 1.147) | 1.131(1.035,1.236) |
| Q1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| p-inter action | 0.758 | <0.001 | 0.329 | 0.602 | 0.265 | |||||
| SO2 | ||||||||||
| Q4 | 0.994(0.921,1.072) | 0.955(0.914,0.998) | 0.934(0.855,1.022) | 0.902(0.846,0.961) | 1.272(1.094,1.479) | 0.987(0.894,1.089) | 0.977(0.804,1.187) | 0.901(0.775,1.043) | 0.947(0.850,1.056) | 0.839(0.771,0.914) |
| Q3 | 1.041(0.962,1.126) | 1.047(1.002,1.095) | 1.025(0.934,1.125) | 1.181(1.109,1.258) | 1.341(1.149,1.563) | 1.203(1.091,1.326) | 0.987(0.817,1.191) | 1.195(0.944,1.271) | 1.022(0.916,1.141) | 1.074(0.986,1.169) |
| Q2 | 0.957(0.889,1.030) | 0.947(0.907,0.989) | 0.995(0.910,1.086) | 0.908(0.851,0.969) | 1.193(1.027,1.386) | 1.066(0.968,1.175) | 0.954(0.781,1.166) | 0.935(0.805,1.085) | 0.934(0.841,1.038) | 0.942(0.865,1.026) |
| Q1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| p-inter action | 0.500 | <0.001 | 0.092 | 0.825 | 0.104 | |||||
Bold characteristics means P–value <0.05 among the values with p-interaction < 0.05. EQ-5D index was analyzed by logarithmic transformation. Adjustment for sex, smoking, drinking, physical activity, education, marital status, employment, household income, sleep duration, residence and medical history (hypertension, diabetes mellitus, dyslipidemia, stroke, myocardial infarction, ischemic heart disease, asthma, arthritis)
Discussion
In this study, we used Korean nationwide population-based data to identify associations between long-term exposure to ambient air pollutants and mental health status. After considering mental health-related confounding factors such as socioeconomic status, health-related behavior and medical history, air pollutants may be an independent predictor of mental health status, ranging from subjective stress level to suicidal ideation.
Our results were similar to those of a previous Korean study in which emergency department visits for depressive episodes in patients with a past history of depressive disorder were associated with recent air pollutant levels [3]. However, our study findings confirmed the associations between subjective stress in daily life or suicide attempts in the general population and long-term exposure to ambient air pollutants. In a three-year study from the National Health Insurance database, there was an association between major depressive disorder and PM2.5 [7]. However, we additionally assessed the effects of SO2, NO2, and CO on mental health status, and thereby, we confirmed the associations between long-term exposure to ambient air pollutants including PM10, NO2, and CO and subjective stress, poor QoL, depressiveness, and suicide ideation.
In this study, we found no clear linear correlation between the risk of mental health disorders and the air pollutant concentration quartile. We believe that the reason for this finding is a threshold effect at low levels of air pollutants; if the concentration is above a certain cut-off value, a significant effect may be similar. We also identified a weak association between depression diagnosis by a physician and ambient air pollution quartile. This association may decrease after adjustment of the known risk factors for depression diagnosis, but a strong association between air pollution and parameters of other mental health status was maintained. Therefore, air pollution may be an unknown risk factor in other mental health parameters. In addition, undiagnosed depressive patients may have other risk factors. In generally, it was known that the risk of mental health disorder was higher in women and the elderly, but air pollution may be an important risk factor for men or persons < 65 years old because these groups may be exposed to air pollution more frequently with high activity [17, 18]. Except the rate of subjective stress, women’s mental health status showed more poor than men in this study, though the rates of suicide attempt were similar. It has been proposed that men’s mental health status may be masked by alcohol and physical violence, and their diagnosis of depression may be underdiagnosed [19]. Accordingly, known confounding factors may be correlated with women’s diagnosed depression from the previous studies [19]. Therefore, air pollutants, as a new association factor of mental health status, may be found out an independent risk factor and enhanced the risk for men. Further research is needed to support any such causal relationship or biological difference. In this study, there was no association between suicide attempts and air pollution exposure. Suicide attempts represent acute symptom worsening, which may be more influenced by short-term rather than long-term exposure to ambient air pollutants [5, 20].
Air pollutants may be strong inflammatory agents in psycho-endocrine-immune connections through an inflammatory process; cyclooxygenase-2, interleukin-1β and particulate-matter–associated lipopolysaccharides [21]. Exposure to air pollutants leads to elevated hippocampal pro-inflammatory cytokine expression, and in addition, there are architectural changes in the dendrites of the hippocampus that can increase depressive-like behaviors in animal models [22]. Neuroinflammation caused by exposure to air pollution can alter innate immune responses and even influence human neurodegenerative disease [21].
Particulate and gaseous pollutants coexist in the air and may induce adverse health effects. PM rarely exists by itself within the ambient environment because gaseous, semi-volatile, and volatile compounds (i.e., aldehydes and polycyclic aromatic hydrocarbons) are constantly changing and interacting. Many vapor-phase compounds attach to the surface of PM and/or by themselves form secondary aerosolized particles [1]. The concentrations of PM10 and NO2 are highly correlated because they share the same pathway as that for depression and neurologic disorders [23]; in contrast, NO2 and SO2 may have different physiologic influences on human health. Although both are gaseous molecules, NO2 is poorly soluble in water, whereas SO2 is highly water soluble [24].
This study has a number of strengths. For one, we used large, heterogeneous, nationwide population-based data. We also considered a wide range of known covariates related to depression, including socioeconomic status [25]. Therefore, we were able to determine the effects of ambient air pollution as an independent risk factor for poor mental health. In particular, previously known risk factors were related to women and the elderly, but this study confirmed that air pollution was a risk factor for mental health disorders in men and individuals < 65 years old.
This study also has several limitations. First, it was not possible to establish causality between air pollution and mental health disorders in this cross-sectional study. Second, we matched the community and air pollutant levels using participants’ home territories. Therefore, if participants worked far from their domiciles, the matching would not have accurately reflected air pollutant levels at their dwellings. Third, we focused on each pollutant and its respective effect on mental health status. However, the adverse effects of pollution on mental health may be caused by unmeasured pollutants, such as PM2.5 or ozone [26], or combinations of multiple pollutants [6], which the effects of complex mixtures of constituent toxins on mental health cannot be explained in this study. Additionally, KCHS did not include the surveyed day to protect personal information, which linked each other. Weather condition may affect the level of air pollution and human activity, however, we cannot adjust them [13]. However, KCHS surveyed during three months, which had stable weather conditions from August to October without monsoon. Therefore, the weather effect would be relatively minimized. Lastly, the prevalence of depression in this study (2.49%) was lower than that found in previous studies of Koreans (3.7%) and Canadians (3.9%) [27, 28]. Therefore, we may have underestimated the prevalence of mental health disorders in these nationwide population-based KCHS data.
Conclusions
Long-term exposure to ambient air pollution was a risk factor of a wide range of potential mental health disorders. Future investigations must not only include more studies to determine the mechanisms of action but also examine the effect of demographic characteristics. This information is helpful to make a policy to control air pollution and to understand the action of air pollutant on the body correctly.
Supporting information
Particulate matter <10 μm (PM10); Sulfur dioxide (SO2); Nitrogen dioxide (NO2); Carbon monoxide (CO). Temperature, rainfall and wind speed were shown at Seoul (Lat.(N) 37°34´, Long.(E) 126°57´). Korea Meteorological Administration, Seoul, Korea (Aug. 2012- July. 2013) http://www.kma.go.kr/repositary/sfc/pdf/sfc_ann_2013.pdf.
(DOCX)
Acknowledgments
The authors would like to thank the Korea Centers for Disease Control and Prevention for the data obtained from the 2013 Community Health Survey and the National Institute of Environmental Research.
Data Availability
Data are available from the Korea Centers for Disease Control and Prevention for the data obtained from the 2013 Community Health Survey and the National Institute of Environmental Research. Researchers interested in the data can request access by sending a proposal to the data access committee at the following link: https://chs.cdc.go.kr/chs/sub05/sub05_02.jsp;jsessionid=7Oz5P2fE0QxHWIHlUREfDtxJ4NBdgVmlzOanpQNiB1QE6XuDMKGPiVOlXaelhKQn.KCDCWAS02_servlet_PUB2.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Sun Q, Hong X, Wold LE. Cardiovascular effects of ambient particulate air pollution exposure. Circulation. 2010;121(25):2755–65. doi: 10.1161/CIRCULATIONAHA.109.893461 ; PubMed Central PMCID: PMCPMC2924678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lim YH, Kim H, Kim JH, Bae S, Park HY, Hong YC. Air pollution and symptoms of depression in elderly adults. Environmental health perspectives. 2012;120(7):1023–8. Epub 2012/04/20. doi: 10.1289/ehp.1104100 ; PubMed Central PMCID: PMCPMC3404652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cho J, Choi YJ, Suh M, Sohn J, Kim H, Cho SK, et al. Air pollution as a risk factor for depressive episode in patients with cardiovascular disease, diabetes mellitus, or asthma. Journal of affective disorders. 2014;157:45–51. Epub 2014/03/04. doi: 10.1016/j.jad.2014.01.002 . [DOI] [PubMed] [Google Scholar]
- 4.Szyszkowicz M, Rowe BH, Colman I. Air pollution and daily emergency department visits for depression. International journal of occupational medicine and environmental health. 2009;22(4):355–62. Epub 2009/01/01. doi: 10.2478/v10001-009-0031-6 . [DOI] [PubMed] [Google Scholar]
- 5.Szyszkowicz M, Willey JB, Grafstein E, Rowe BH, Colman I. Air pollution and emergency department visits for suicide attempts in vancouver, Canada. Environmental health insights. 2010;4:79–86. Epub 2010/11/17. doi: 10.4137/EHI.S5662 ; PubMed Central PMCID: PMCPMC2978939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oudin A, Astrom DO, Asplund P, Steingrimsson S, Szabo Z, Carlsen HK. The association between daily concentrations of air pollution and visits to a psychiatric emergency unit: a case-crossover study. Environmental health: a global access science source. 2018;17(1):4 Epub 2018/01/13. doi: 10.1186/s12940-017-0348-8 ; PubMed Central PMCID: PMCPMC5763570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim KN, Lim YH, Bae HJ, Kim M, Jung K, Hong YC. Long-Term Fine Particulate Matter Exposure and Major Depressive Disorder in a Community-Based Urban Cohort. Environmental health perspectives. 2016;124(10):1547–53. Epub 2016/04/30. doi: 10.1289/EHP192 ; PubMed Central PMCID: PMCPMC5047772 interests. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim Y, Myung W, Won HH, Shim S, Jeon HJ, Choi J, et al. Association between air pollution and suicide in South Korea: a nationwide study. PloS one. 2015;10(2):e0117929 Epub 2015/02/19. doi: 10.1371/journal.pone.0117929 ; PubMed Central PMCID: PMCPMC4333123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y, Eliot MN, Koutrakis P, Gryparis A, Schwartz JD, Coull BA, et al. Ambient air pollution and depressive symptoms in older adults: results from the MOBILIZE Boston study. Environmental health perspectives. 2014;122(6):553–8. Epub 2014/03/13. doi: 10.1289/ehp.1205909 ; PubMed Central PMCID: PMCPMC4050499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zijlema WL, Wolf K, Emeny R, Ladwig KH, Peters A, Kongsgard H, et al. The association of air pollution and depressed mood in 70,928 individuals from four European cohorts. International journal of hygiene and environmental health. 2016;219(2):212–9. Epub 2015/12/20. doi: 10.1016/j.ijheh.2015.11.006 . [DOI] [PubMed] [Google Scholar]
- 11.Seo J, Choi B, Kim S, Lee H, Oh D. The relationship between multiple chronic diseases and depressive symptoms among middle-aged and elderly populations: results of a 2009 korean community health survey of 156,747 participants. BMC public health. 2017;17(1):844 Epub 2017/10/27. doi: 10.1186/s12889-017-4798-2 ; PubMed Central PMCID: PMCPMC5657127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun Taek Kim. Quality control of Air pollution Monitoring System and establishment of Data Evaluation Scheme(I). Korean Air Pollutants Emission Service2015.
- 13.Choi Y, Ghim YS. Assessment of the clear-sky bias issue using continuous PM10 data from two AERONET sites in Korea. Journal of environmental sciences (China). 2017;53:151–60. Epub 2017/04/05. doi: 10.1016/j.jes.2016.02.020 . [DOI] [PubMed] [Google Scholar]
- 14.Ayanlade A, Oyegbade EF. Influences of wind speed and direction on atmospheric particle concentrations and industrially induced noise. SpringerPlus. 2016;5(1):1898 Epub 2016/11/16. doi: 10.1186/s40064-016-3553-y ; PubMed Central PMCID: PMCPMC5084142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee YK, Nam HS, Chuang LH, Kim KY, Yang HK, Kwon IS, et al. South Korean time trade-off values for EQ-5D health states: modeling with observed values for 101 health states. Value Health. 2009;12(8):1187–93. doi: 10.1111/j.1524-4733.2009.00579.x . [DOI] [PubMed] [Google Scholar]
- 16.Kim J, Kim H. Demographic and Environmental Factors Associated with Mental Health: A Cross-Sectional Study. Int J Environ Res Public Health. 2017;14(4). doi: 10.3390/ijerph14040431 ; PubMed Central PMCID: PMCPMC5409632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hong J, Zhong T, Li H, Xu J, Ye X, Mu Z, et al. Ambient air pollution, weather changes, and outpatient visits for allergic conjunctivitis: A retrospective registry study. Scientific reports. 2016;6:23858 Epub 2016/04/02. doi: 10.1038/srep23858 ; PubMed Central PMCID: PMCPMC4817244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mannucci PM, Franchini M. Health Effects of Ambient Air Pollution in Developing Countries. Int J Environ Res Public Health. 2017;14(9). Epub 2017/09/13. doi: 10.3390/ijerph14091048 ; PubMed Central PMCID: PMCPMC5615585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seidler ZE, Dawes AJ, Rice SM, Oliffe JL, Dhillon HM. The role of masculinity in men's help-seeking for depression: A systematic review. Clin Psychol Rev. 2016;49:106–18. Epub 2016/10/26. doi: 10.1016/j.cpr.2016.09.002 . [DOI] [PubMed] [Google Scholar]
- 20.Kim C, Jung SH, Kang DR, Kim HC, Moon KT, Hur NW, et al. Ambient particulate matter as a risk factor for suicide. The American journal of psychiatry. 2010;167(9):1100–7. Epub 2010/07/17. doi: 10.1176/appi.ajp.2010.09050706 . [DOI] [PubMed] [Google Scholar]
- 21.Calderon-Garciduenas L, Solt AC, Henriquez-Roldan C, Torres-Jardon R, Nuse B, Herritt L, et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid beta-42 and alpha-synuclein in children and young adults. Toxicol Pathol. 2008;36(2):289–310. doi: 10.1177/0192623307313011 . [DOI] [PubMed] [Google Scholar]
- 22.Fonken LK, Xu X, Weil ZM, Chen G, Sun Q, Rajagopalan S, et al. Air pollution impairs cognition, provokes depressive-like behaviors and alters hippocampal cytokine expression and morphology. Molecular psychiatry. 2011;16(10):987–95, 73. Epub 2011/07/06. doi: 10.1038/mp.2011.76 ; PubMed Central PMCID: PMCPMC3270364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maes M, Kubera M, Obuchowiczwa E, Goehler L, Brzeszcz J. Depression's multiple comorbidities explained by (neuro)inflammatory and oxidative & nitrosative stress pathways. Neuro endocrinology letters. 2011;32(1):7–24. Epub 2011/03/17. . [PubMed] [Google Scholar]
- 24.Greenberg N, Carel RS, Derazne E, Tiktinsky A, Tzur D, Portnov BA. Modeling long-term effects attributed to nitrogen dioxide (NO2) and sulfur dioxide (SO2) exposure on asthma morbidity in a nationwide cohort in Israel. Journal of toxicology and environmental health Part A. 2017;80(6):326–37. Epub 2017/06/24. doi: 10.1080/15287394.2017.1313800 . [DOI] [PubMed] [Google Scholar]
- 25.Pun VC, Manjourides J, Suh H. Association of Ambient Air Pollution with Depressive and Anxiety Symptoms in Older Adults: Results from the NSHAP Study. Environmental health perspectives. 2017;125(3):342–8. Epub 2016/08/16. doi: 10.1289/EHP494 ; PubMed Central PMCID: PMCPMC5332196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kioumourtzoglou MA, Power MC, Hart JE, Okereke OI, Coull BA, Laden F, et al. The Association Between Air Pollution and Onset of Depression Among Middle-Aged and Older Women. American journal of epidemiology. 2017;185(9):801–9. Epub 2017/04/04. doi: 10.1093/aje/kww163 ; PubMed Central PMCID: PMCPMC5411676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patten SB, Williams JV, Lavorato DH, Wang JL, McDonald K, Bulloch AG. Descriptive epidemiology of major depressive disorder in Canada in 2012. Canadian journal of psychiatry Revue canadienne de psychiatrie. 2015;60(1):23–30. Epub 2015/04/18. doi: 10.1177/070674371506000106 ; PubMed Central PMCID: PMCPMC4314053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oh DH, Kim SA, Lee HY, Seo JY, Choi BY, Nam JH. Prevalence and correlates of depressive symptoms in korean adults: results of a 2009 korean community health survey. J Korean Med Sci. 2013;28(1):128–35. doi: 10.3346/jkms.2013.28.1.128 ; PubMed Central PMCID: PMCPMC3546091. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Particulate matter <10 μm (PM10); Sulfur dioxide (SO2); Nitrogen dioxide (NO2); Carbon monoxide (CO). Temperature, rainfall and wind speed were shown at Seoul (Lat.(N) 37°34´, Long.(E) 126°57´). Korea Meteorological Administration, Seoul, Korea (Aug. 2012- July. 2013) http://www.kma.go.kr/repositary/sfc/pdf/sfc_ann_2013.pdf.
(DOCX)
Data Availability Statement
Data are available from the Korea Centers for Disease Control and Prevention for the data obtained from the 2013 Community Health Survey and the National Institute of Environmental Research. Researchers interested in the data can request access by sending a proposal to the data access committee at the following link: https://chs.cdc.go.kr/chs/sub05/sub05_02.jsp;jsessionid=7Oz5P2fE0QxHWIHlUREfDtxJ4NBdgVmlzOanpQNiB1QE6XuDMKGPiVOlXaelhKQn.KCDCWAS02_servlet_PUB2.