Abstract
Background
Roux-en-Y gastric bypass (RYGB) in adolescence results in substantial bodyweight reduction and cardiometabolic benefits into young adulthood. Knowledge gaps remain in understanding psychosocial health.
Objective
Describe trajectories of weight and psychosocial health in adolescents who underwent RYGB into young adulthood.
Setting
Academic Pediatric Medical Center.
Methods
Fourteen adolescents (presurgery: mean body mass index = 59.2 ± 8.9; mean age = 16.0 ± 1.3 yr; 64.3% female) participated in 2 sequential observational studies. Height and weight were measured, and participants completed measures of weight-related quality of life (WRQOL), mental health, and adaptive functioning at presurgery and 6, 12, 18, 24, and 72+ months post-surgery. Substance use behaviors were assessed at 72+ months.
Results
Modeling demonstrated rapid improvement in body mass index and WROQL across post-operative year 1, followed by stabilization and modest weight regain/WRQOL decline (P < .001), with 50% remaining severely obese. Presurgery, 11 adolescents presented with symptoms outside of the normal range for ≥ 1 mental health domain. Postoperative profiles indicated either remittance (n = 5) or persistent symptomatology (n = 6: anxious/depressed, withdrawn/depressed, and/or thought problems) in young adulthood. No new incidence of mental health vulnerability occurred in young adults not already identified preoperatively. Adaptive functioning and substance use were within normal range.
Conclusions
Although adolescent RYGB resulted in improvement in weight and WRQOL into young adulthood, mental health trajectories were more variable, with some experiencing positive change while others experienced persistent mental health vulnerability. Research focused on larger contemporary samples using a controlled design is critical to inform targets for prevention and intervention to optimize both physical and psychosocial health outcomes in this younger patient population.
Keywords: Adolescent, Young adult, Bariatric surgery, Psychosocial
Bariatric surgery is emerging as a safe and efficacious weight loss tool for adolescents resulting in substantial bodyweight reduction, cardiometabolic benefits, and improved quality of life [1–5]. Most recently, investigative teams in Sweden [6] and the United States [7] have demonstrated the longer term (≥5 yr) benefits of Rouxen-Y gastric bypass (RYGB) specifically, as adolescent patients transitioned to young adulthood.
Unlike the adult bariatric patient, an adolescent’s post-operative course cuts across a transitional period in psychosocial development, as patients age into young adulthood. Hallmarks of this period include rapid change, increasing independence, educational/vocational transitions, and exploration in relationships/identity. In addition, mental health disorders and substance use emerge as significant public health concerns [8]. A majority of individuals navigate these developmental phases relatively unscathed, while others are launched on trajectories of varying psychosocial risk and competence. Arguably, the improved health outcomes resulting from bariatric surgery could lead to positive changes in psychosocial and developmental trajectories for adolescents with severe obesity, a known subgroup at psychosocial risk [9].
We provided the first view of adolescent psychosocial outcomes following RYGB, prospectively demonstrating that along with reduction in body mass index (BMI), significant improvements occurred in weight-related quality of life (WRQOL) and depressive symptoms at 1 year and largely maintained at 2 years [10,11]. An investigative team from Sweden reported similar trends for adolescent patients 1 and 2 years following RYGB but expanded the outcome scope by also demonstrating reductions in anxiety symptoms and externalizing behaviors (i.e., anger/disruptive, oppositional) [12,13]. For both teams, a persistence of clinical range depressive symptomatology for some patients was evident (14%–19%). These initial adolescent findings are consistent with adult RYGB studies at 2–3 years postoperatively, including the Longitudinal Assessment of Bariatric Surgery consortium, suggesting variable outcomes (reduction versus persistence) for patients presenting with anxiety and depression [14,15]. For the adolescent patient, we lack an empirical understanding of longer-term (i.e., >24 mo) psychosocial outcomes, resulting in undefined critical targets as well as timing of prevention and intervention efforts to optimize outcomes during the transition to young adulthood.
The present pilot study extended our original prospective observation of short-term psychosocial health and BMI outcomes following RYGB in adolescents [11] to their young adulthood, when patients were 6 or more years post-RYGB. In addition to WRQOL, psychosocial health was broadened to mental health (i.e., psychopathology, substance use) and adaptive functioning (i.e., age-normative milestones). Exploration of intraindividual and group trajectories aimed to illustrate continuity and change over time.
Methods
Participants and procedures
Fourteen adolescents who underwent RYGB at one pediatric academic medical center (2004–2005) participated in 2 sequential observational studies [7,11]. These studies resulted in the continuous tracking of BMI, WRQOL, mental health, and adaptive functioning from presurgery (or “0,” within 30 d before RYGB) to postoperative assessments at 6-, 12-, 18-, 24-, and 72+ months.
As previously described [11], 100% of 16 consecutive adolescents meeting presurgery inclusion criteria (i.e., ages 14–17 yr, no developmental delay) agreed to participate (mean presurgery age = 16.2 ± 1.4 yr). Psychosocial measures and height/weight measurements were completed during a study visit either at the clinical center (0–12 mo: 100%; 18 mo: 46%; 24 mo: 57%), during home visits (18 mo: 7%; 24 mo: 36%), or from questionnaires mailed with height/weight self-reported (18 mo: 47%; 24 mo: 7%).
Fourteen of the original 16 (87.5%) participated at “72+ months” (6.3–9.7 yr from time of surgery) as part of a larger cohort in a comprehensive long-term follow-up study [7] that included developmentally appropriate versions of the same assessments from the earlier time points. Of the 2 (1 male, 1 female) who did not participate at 72+ months, one actively declined while the other was nonresponsive. Both were white, with a presurgery age > 17 and a BMI > 59. Participants were compensated at each study visit and reimbursed for reasonable travel expenses. The Institutional Review Board approved both studies.
Measures
BMI and percent weight loss
Participants’ height and weight were used to calculate BMI and classifications of overweight (BMI 25–29.9 kg/m2) and obesity (Class I, BMI = 30.0–34.9 kg/m2; Class II, BMI = 35.0–39.9 kg/m2; Class III, BMI ≥40 kg/m2). Percent weight loss was calculated as ([weightfollow-up − weightpresurgery]/weightpresurgery) × 100.
WRQOL
Serial assessments of WRQOL were completed using the Impact of Weight on Quality of Life-Kids (IWQOL-Kids [16]; 0–24 mo) and the Impact of Weight on Quality of Life-Lite (IWQOL-Lite [17]; 72+ mo). The IWQOL-Kids (ages 11–19 yr) has a total score and 4 subscales (physical comfort, body esteem, social life, and family relations). The IWQOL-Lite (ages > 18 yr) provides a total score and 5 subscales (physical function, self-esteem, sexual life, public distress, and work). Raw scores were converted to standardized scores (range 0–100), with higher scores indicating better WRQOL. Both measures discriminate between weight status groups and are responsive to weight loss and weight gain.
Mental health
Serial assessments of self-reported mental health symptomatology (“in the past 6 months”) were completed using the Achenbach System of Empirically Based Assessment. Participants completed the Youth Self-Report (YSR; for ages 11–18 yr [18]) from presurgery to 24 months and the Adult Self-Report (ASR; for ages 18–59 yr [19]) at 72 months. YSR and ASR broadband summary scales (total problems, internalizing, externalizing) and syndrome subscales (anxious/depressed, withdrawn/depressed, somatic complaints, thought problems, attention problems, rule-breaking behavior, aggressive behavior, social problems [YSR], intrusive [ASR]) were reported using age- and gender-normative T scores based on nationally representative nonreferred samples of adolescents (ages 11–18 yr) and adults (ages 18–35 yr). Higher T scores indicate greater symptomatology, with cut-offs established above the normal range (broad-band: T = 60–63 borderline, T >63 clinical; narrow-band: T = 65–69 borderline, T >69 clinical). The ASR (72+ mo) also includes substance use scales (tobacco, alcohol, and drug use in past 6 mo) and a mean substance use T score (T = 65–69 borderline, T > 69 clinical).
Adaptive functioning
The YSR [18] and ASR [19] were utilized to assess adolescent (0–24 mo) and adult (72+ mo) adaptive functioning, with lower scores indicating greater impairment in meeting age-salient demands. YSR social and activities scales (T <31 clinical; T = 31–35 borderline) and school scale (i.e., mean performance in academic patients from failing “0” to above average “3”) raw scores are summed for a total competence score (T < 37 clinical; T = 37–40 borderline). ASR scales include friends, spouse/partner, family, job, and education, and a mean adaptive summary score (T <31 clinical; T = 31–35 borderline). At 72+ months, participants also completed a school/work history form documenting their academic history, current living situation (i.e., with parents, partner, friends), and current employment status.
Data analysis
Measures were scored based on instrument guidelines. Intraindividual scores, mean scores, as well as frequencies were calculated. Hierarchical linear modeling using SPSS (version 22) estimated the average growth trajectories of BMI and Total WRQOL over time. Given the variation in time between presurgery and 72+ month assessments (i.e., mean = 7.8 ± 1.0 yr), correlations of time with change in these outcome measures were examined. Time was not significantly associated with presurgery to 72+ months difference scores for BMI (r = −0.17, P = .57) or Total WRQOL (r = −0.10, P = .75) and thus was not controlled for in hierarchical linear modeling analyses. For mental health, substance use, and adaptive functioning, YSR/ASR borderline and clinical categories were combined to denote prevalence of behaviors outside of the normal range based on age- and gender-specific normative samples.
Results
Participants
Participants (n = 14) were predominantly female (n = 9, 64.3%) and white (n = 12, 85.7%). Mean presurgery age was 16.0 ± 1.3 years (range = 13.7–18.1). Mean age at 72+ month was 23.8 ± 1.6 years (range 20.7–26.4). Participation rates were strong at earlier time points (6 mo: 85.7%; 12–24 mo: 100%).
BMI and weight status
Participant-specific trajectories, mean BMI change, and weight classification frequencies over time are presented in Fig. 1A and Table 1. Presurgery, 100% of participants were classified in obesity Class III. Mean percent weight loss from 0 to 72+ months was −29.1% ± 14.9, with a +7.0% rate of regain from 24 months to 72+ months (mean % change BMI = −28.6 ± 14.8, +6.6% regain). Two achieved overweight status by 72+ months. The majority remained clinically obese (>Class I) if not severely obese (n = 7, 50% Class III). Modeling of BMI over time indicated that as a group, there was a significant quadratic (i.e., nonlinear) effect F (1, 49) = 116.3 (P < .001). Specifically, there was a substantial initial reduction in BMI, with a deceleration (i.e., slowing in the rate of change) by 12 months and evidence of modest weight regain by 72+ months.
Fig. 1.
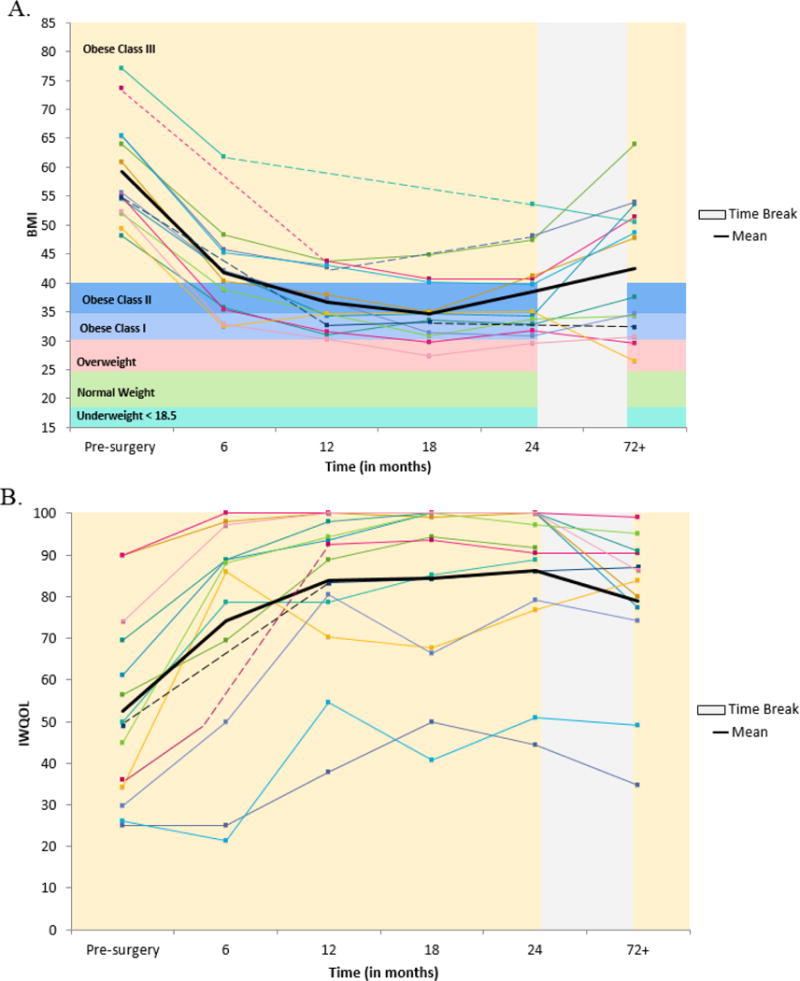
Participant-specific trajectories of (A) body mass index and (B) weight-related quality of life from baseline/presurgery to 72+ months after Roux-en-Y gastric bypass.
Table 1.
Body mass index (BMI), percent change in weight, and weight related quality of life from adolescence to young adulthood for Roux-en-Y Gastric Bypass patients (n=14).
| Pre-surgery M±SD or n (%) |
6 months M±SD |
12 months M±SD |
18 months M±SD |
24 months M±SD or n (%) |
72±months M±SD or n (%) |
|
|---|---|---|---|---|---|---|
| BMIa | 59.2 ± 8.9 | 41.8 ± 8.1 | 36.7 ± 5.1 | 34.7 ± 5.0 | 38.4 ± 7.5 | 42.5 ± 11.6 |
| Percent Change in Weightb | – | −29.2 ± 5.4 | −36.3 ± 4.0 | −38.7 ± 6.2 | −36.0 ± 6.5 | −29.1 ± 14.9 |
|
| ||||||
| BMI Classificationsc | ||||||
| Overweight | – | – | – | – | 1 (7.7) | 2 (14.3) |
| Class I Obesity | – | – | – | – | 5 (38.5) | 4 (28.6) |
| Class II Obesity | – | – | – | – | 2 (15.4) | 1 (7.1) |
| Class III Obesity | 14 (100) | – | – | – | 5 (38.5) | 7 (50) |
|
| ||||||
| IWQOL-Kidsd | ||||||
| Total | 52.6 ± 22.0 | 74.3 ± 27.6 | 83.8 ± 18.6 | 84.4 ± 20.2 | 86.1 ± 18.1 | – |
| Physical Comfort | 35.7 ± 23.6 | 75.4 ± 23.9 | 88.1 ± 16.3 | 88.7 ± 16.1 | 90.8 ± 15.7 | – |
| Body Esteem | 31.9 ± 30.7 | 62.3 ± 36.6 | 71.6 ± 29.6 | 72.5 ± 34.7 | 74.1 ± 30.3 | – |
| Social Life | 57.7 ± 33.9 | 76.4 ± 33.0 | 84.8 ± 21.4 | 85.7 ± 21.4 | 88.9 ± 19.8 | – |
| Family Relations | 93.2 ± 13.9 | 89.2 ± 25.2 | 96.7 ± 7.7 | 95.5 ± 16.7 | 96.1 ± 13.3 | – |
| IWQOL-Lited | ||||||
| Total | – | – | – | – | – | 79.0 ± 19.0 |
| Physical Function | – | – | – | – | – | 85.9 ± 13.0 |
| Self-Esteem | – | – | – | – | – | 60.5 ± 29.9 |
| Sex Life | – | – | – | – | – | 81.8 ± 29.0 |
| Public Distress | – | – | – | – | – | 77.1 ± 29.2 |
| Work | – | – | – | – | – | 91.7 ± 14.2 |
Note: IWQOL=Impact of Weight on Quality of Life; M=mean; SD=standard deviation
Missing data at 6 months (n=2); at 12 months (n=1); at 18 months (n=2); at 24 months (n=1).
Missing data at 6 months (n=3); at 12 months (n=1); at 18 months (n=2); at 24 months (n=1). Percent change in weight is defined as ((weightpost-surgery − weightpre-surgery)/weightpre-surgery)×100.
Missing data at 24 months (n=1). BMI Classification defined as: Overweight: BMI = 25.0-29.9 kg/m2; Class I Obesity: BMI = 30.0-34.9 kg/m2; Class II Obesity: BMI 35.0-39.9kg/m2; Class III Obesity: BMI = ≥ 40.0 kg/m2.
Missing data at 6 months (n=2); Missing data at 6± years (n=2).
WRQOL
Participant-specific trajectories, mean change in total WRQOL, as well as WRQOL sub-scale means are presented in Fig. 1B and Table 1. Modeling of total scores (n = 12) over time indicated that as a group, there was a significant quadratic effect F (1, 56) = 88.4 (P < .001). There was substantial initial improvement in WRQOL, with a deceleration by 12 months and evidence of some modest decline in WRQOL by 72+ months.
Mental health
Group means and prevalence rates on YSR/ASR scales are reported in Table 2. With one exception (i.e., presurgery internalizing T score in the borderline range), group means for all mental health domains and across all time-points were within the normal range based on age- and gender- specific normative samples.
Table 2.
Mental health, adaptive functioning, and substance abuse domains from adolescence to young adulthood for Roux-en-Y Gastric Bypass patients (n=14).
| Youth Self-Report (YSR)/Adult Self-Report (ASR) | Pre-surgery M±SD n (%) |
6 months M±SD |
12 months M±SD |
18 months M±SD |
24 months M±SD n (%) |
72+ months M±SD n (%) |
|---|---|---|---|---|---|---|
| Total Problemsa,b | 62.6 ± 10.1 | 54.2 ± 10.1 | 53.1 ± 11.1 | 52.7 ± 13.9 | 52.9 ± 11.8 | 54.6 ± 12.1 |
| 9 (64.3) | 5 (35.7) | 5 (35.7) | ||||
| Internalizing | 63.9 ± 13.2 | 55.1 ± 11.0 | 51.4 ± 12.6 | 53.6 ± 14.1 | 53.1 ± 14.4 | 57.3 ± 13.8 |
| 9 (64.3) | 5 (35.7) | 6 (42.9) | ||||
| Anxious/Depressed | 63.0 ± 12.5 | 57.8 ± 10.1 | 55.5 ± 6.4 | 57.9 ± 9.2 | 56.9 ± 8.7 | 60.4 ± 11.0 |
| 4 (28.6) | 3 (21.4) | 5 (35.7) | ||||
| Withdrawn/Depressed | 64.1 ± 13.0 | 58.0 ± 10.2 | 55.1 ± 55.4 | 58.1 ± 8.0 | 56.6 ± 9.8 | 55.6 ± 7.0 |
| 6 (42.9) | 1 (7.1) | 3 (21.4) | ||||
| Somatic Complaints | 64.1 ± 11.9 | 55.0 ± 6.4 | 56.9 ± 7.8 | 55.8 ± 7.5 | 57.8 ± 10.4 | 62.0 ± 13.6 |
| 5 (35.7) | 3 (21.4) | 5 (35.7) | ||||
| Externalizing | 55.2 ± 10.3 | 50.4 ± 9.2 | 51.9 ± 9.8 | 50.7 ± 11.8 | 50.4 ± 8.9 | 51.4 ± 11.8 |
| 4 (28.6) | 2 (14.3) | 3 (21.4) | ||||
| Aggressive Behavior | 57.0 ± 9.2 | 53.3 ± 4.2 | 54.7 ± 5.2 | 55.4 ± 6.1 | 53.5 ± 4.5 | 55.2 ± 8.2 |
| 3 (21.4) | 0 | 2 (14.3) | ||||
| Rule-Breaking Behavior | 57.0 ± 6.1 | 55.0 ± 4.5 | 55.3 ± 5.0 | 54.9 ± 5.1 | 54.3 ± 4.9 | 54.7 ± 8.5 |
| 2 (14.3) | 1 (7.1) | 1 (7.1) | ||||
| Intrusive (ASR only) | – | – | – | – | – | 54.6 ± 7.6 |
| 2 (14.3) | ||||||
| Other Syndromes | ||||||
| Thought Problems | 61.4 ± 10.1 | 56.3 ± 7.1 | 54.6 ± 7.1 | 55.5 ± 8.2 | 53.9 ± 5.2 | 57.7 ± 7.5 |
| 5 (35.7) | 1 (7.1) | 4 (28.6) | ||||
| Attention Problems | 61.4 ± 10.3 | 58.1 ± 9.1 | 58.3 ± 6.0 | 57.4 ± 8.2 | 57.9 ± 7.0 | 57.8 ± 8.3 |
| 7 (50.0) | 2 (14.3) | 1 (7.1) | ||||
| Social Problems (YSR only) | 62.9 ± 9.5 | 57.9 ± 7.9 | 57.1 ± 6.7 | 56.5 ± 7.1 | 57.1 ± 8.1 | – |
| 6 (42.9) | 4 (28.6) | |||||
|
| ||||||
| Adaptive Functioning | ||||||
|
| ||||||
| YSR Competence Scalesc | ||||||
| Activities | 44.9 ± 11.0 | 40.2 ± 9.8 | 45.1 ± 10.8 | 42.2 ± 11.1 | 42.1 ± 12.6 | – |
| Social | 47.1 ± 11.0 | 48.3 ± 10.8 | 46.9 ± 10.2 | 47.4 ± 10.1 | 48.9 ± 9.6 | – |
| Academic | 2.1 ± 0.8 | 2.4 ± 0.7 | 2.2 ± 0.7 | 2.5 ± 0.5 | 2.3 ± 0.5 | – |
| Total Competence | 44.9 ± 12.9 | 44.3 ± 14.4 | 45.9 ± 13.0 | 43.5 ± 12.0 | 45.0 ± 10.8 | – |
| ASR Competence Scales | ||||||
| Friend | – | – | – | – | – | 50.9 ± 6.7 |
| Spouse/Partner (n=7) | – | – | – | – | – | 53.0 ± 5.5 |
| Family | – | – | – | – | – | 47.9 ± 7.1 |
| Job (n=8) | – | – | – | – | – | 42.1 ± 9.0 |
| Education (n=4) | – | – | – | – | – | 54.0 ± 6.9 |
| Mean Adaptive | – | – | – | – | – | 48.6 ± 8.2 |
| ASR Substance Use | ||||||
| Tobacco times per day | – | – | – | – | – | 53.9 ± 5.2 |
| Alcohol days drunk | – | – | – | – | – | 51.2 ± 3.1 |
| Drugs days used | – | – | – | – | – | 52.8 ± 10.4 |
| Mean substance use | – | – | – | – | – | 53.4 ± 6.7 |
Note: M=mean; SD=standard deviation; Means and SDs are provided as T scores for all scales except the academic scale.
Missing data: At 6 months (n=2). Mental health from pre-surgery through 24 months post-surgery was assessed using the YSR; at 6+ years, the ASR was used. Means and SDs are provided as T scores for all broadband and syndrome scales.
Percentages of participants exceeding borderline cutoffs are provided at pre-surgery, as well as at 24 months and 6+ years post-surgery.
Missing data: At 6 months (n=2–3); at 12 months (n=2); at 18 months (n=1–2); at 24 months (n=1).
Participant-specific courses of syndrome scores outside of the normal range at presurgery, 24 months, and 72+ months are summarized below and limited to the 7 syndromes assessed across both measures (anxious/depressed, withdrawn/depressed, thought problems, attention problems, rule-breaking behavior, aggressive behavior). While somatic complaints prevalence was high (n = 5, 35.7% at presurgery and 72+ mo), it was excluded given potential confounds in populations with chronic medical conditions [20]. Three participants (21.4%) scored in the normal range for their age/gender on all syndrome subscales at presurgery, 24 months, and 72+ months. Eleven met syndrome elevations on one or more subscales at presurgery (mean #syndromes = 2.5, range 1–6) with varying mental health vulnerability profiles postoperatively. Of these 11, 5 (45.5%) reported remitting symptomatology (i.e., 4 in the normal range by 24 mo and 1 by 72+ mo). An additional 2 reported remitting symptomatology at 24 months but presented with one syndrome at 72+ months. The remaining 4 (28.5%) maintained at least one syndrome elevation across all 3 time-points. Co-morbidity was high at 72+ months for these 4 participants (2 with 2 syndromes; 1 with 4; 1 with 6). Across participants and time, the most common elevations were for anxious/depressed, withdrawn/depressed, and thought problems. The highest category for remittance was attention problems.
Substance use
At 72+ months, group mean T scores for the mean substance use scale as well as the tobacco, alcohol, and drug subscales fell in the normal range (Table 2). Only one participant reported behaviors outside of the normal range, with clinical range elevations for the drug and mean substance use scales.
Adaptive functioning
Group mean YSR/ASR T scores for adaptive functioning fell within the normal range across time (Table 2). Presurgery, 5 of 14 met criterion for adaptive functioning outside the normal range (35.7%, total competence ≤40). At 72+ months, 2 of these participants continued to meet criterion for adaptive functioning impairment, 1 in the “job” domain and a second for the overall adaptive score. All were high school graduates (1 with high school equivalence diploma), with 8 continuing beyond high school. At 72+ months, 7 were attending school (5 college, 2 graduate school), 3 were working, and 4 were not in school and “looking for work.” Nine reported being single, 6 lived with their parents, and 4 of the 9 females reported being a parent.
Discussion
Preliminary evidence suggests that following RYGB, along with substantial and durable weight loss, adolescents reported marked and sustained improvements in WRQOL into young adulthood (i.e., at mean = 7.8 ± 1.0 post-operative yr). These young adult IWQOL-Lite values were similar to those reported by adult RYGB patients 6 years postoperatively [21]. Areas of greater relative impairment (i.e., weight-related self-esteem and public distress) were consistent with young adult values on the instrument validation sample [22]. However, individual plots (Figs. 1A and 1B) indicate patterns of WRQOL variability, along with most adolescent patients remaining obese, if not severely obese, as young adults.
Longer-term mental health trajectories for this cohort of adolescent RYGB patients can be summarized as follows. First, only a minority reported healthy psychological status before RYGB (i.e., no syndrome elevations outside of the normal range), and these adolescents maintained their healthy status as young adults. Said differently, there was no new incidence of mental health vulnerability (i.e., outside of normal range on one or more syndrome scale) in young adult patients not already identified by their adolescent preoperative status. Second, and in contrast, for those adolescents who reported any mental health vulnerabilities presurgically, postoperative improvements to an overall healthy range of functioning occurred in almost half by young adulthood (i.e., 5 of 11 participants). Furthermore, these improvements were most often observed earlier in the postoperative course (i.e., by 24 mo) versus later in young adulthood. Third, the remaining half (i.e., 6 of 11 adolescents) with presurgical depressive, anxiety, and/or disordered thinking syndromes tended to persist in these symptom profiles as young adults, even with signs of temporary alleviation of symptoms at 24 months. These findings extend initial concerns regarding persistent mental health needs for some adolescent RYGB patients at 2 years postoperatively [12], to later time-points 6 years and beyond when they are young adults. Overall, these trends may suggest that, on average, adolescents are more likely to persist in their preoperative mental health status as young adults, whether healthy or vulnerable, versus show improvement in the longer term following RYGB.
In terms of adaptive functioning, the majority of adolescents were “doing well” in meeting common age-salient demands of life (i.e., education, social relations, work) which continued to young adulthood. Substance use behaviors, while limited to cross-sectional assessment in young adulthood were within the normative range, with only one exception.
From a clinical perspective, adolescents who are approved for and undergo RYGB with psychosocial vulnerabilities preoperatively, and depressive and/or anxiety symptoms specifically, will benefit from provider discussions about their need for monitoring postoperatively and in the longer term as they transition to adult care settings. This proves particularly important for this patient population, as young adults are a known age group who lack a usual source of care (i.e., primary care provider) and are more likely to seek medical assistance through emergency departments or walk-in clinics [23]. As a result, young adults may infrequently receive preventative healthcare and mental health screening [24]. Moreover, the presence and persistence of adolescent/young adult psychopathology, independent of bariatric surgery, is a known risk factor for life challenges (i.e., employment, education, residential stability [8]) and is also a potential correlate to known risks in this age group (i.e., substance use [8], suicidal behaviors [25]). These young adult risks have been identified as clinical concerns in this patient population based on the initial adolescent and adult bariatric experience [26–29].
Although sample size dictates the preliminary nature of these findings, use of a prospective standardized protocol of contiguous measurement, a widely used measure of mental health with nationally based age-and gender-normative reference values, and high rates of recruitment/retention underscore this study’s contribution. These patient-reported outcomes were from one clinical center where practice was limited to RYGB at enrollment. Consistent with national bariatric surgery trends, the sample was primarily white and female. Presurgery BMI and psychopathology rates were higher than a more contemporary multisite sample (surgery 2008 or later) using the same protocol (i.e., study eligibility, timing of enrollment) [30]. Psychosocial approval processes may have grown more stringent over time, or more likely, patients with less psychosocial impairment and lower BMI, are now seeking/being referred for and undergoing bariatric surgery.
Replications with larger contemporary samples are needed. Ongoing ancillary work within the Teen Longitudinal Assessment of Bariatric Surgery consortium will prove critical, as it includes long-term follow-up with adolescents who have undergone RYGB or sleeve gastrectomy, a current procedure for this age group with promising outcomes [2]. The inclusion of a nonoperative comparison group will allow a more definitive demonstration of surgical treatment’s benefits and risks for adolescent severe obesity. Recognizing that the laparoscopic adjustable band for adolescent patients has also been a focus of considerable work [3–5,31], long-term psychosocial outcome studies are critically needed, particularly given differing treatment demands and weight loss outcome trajectories associated with this device-based intervention [2]. Finally, from an analytical standpoint, the reliance on reporting group mean (summary) scores would suggest that, as a group, participants were functioning within normal limits for age and gender across all time points. The interpretation of statistically significant change over time as clinically meaningful is potentially misleading. By focusing on an individual’ s clinical course over time (i.e., those who maintain their preoperative status, those who improve or decline over time), a different outcome story emerged with greater clinical relevance.
Conclusion
RYGB for adolescent severe obesity leads to substantial improvement in weight and WRQOL in young adulthood, even as many remain obese. Mental health outcomes were variable, with profiles of positive change and alternately, persistent vulnerability. These preliminary data illustrate important caveats to consider clinically and in study design with larger contemporary samples as there is likely considerable depth in these data to inform patient care. Prospective examination of links among WRQOL, mental health, and primary outcomes (weight loss, morbidity, mortality) as well as whether mental health serves as a signal for other emerging risks are important next steps. This research will serve as a foundation to identify critical targets and time frames for prevention and intervention efforts to both promote positive physical and mental health and reduce the potential for long-term negative consequences in this younger patient population.
Acknowledgments
We gratefully acknowledge the dedication and expertise of research coordinators over the course of these studies: Christina Ramey, B.A., Lindsay Wilson, B.A., Faye Doland, B.S., Jennifer Black, M.S.S.A., L.S.W., Lindsey Shaw, M.S., Tawny W. Boyce, M.S., M.P.H., April Carr, B.S., Nina Cunning, Andrea Ferris, B.S., Allison Greenberg, B.A., Patricia Hirsch, R.N., Renee Jeffreys, Ph.D., Linda Kollar, R.N., Rosie Miller, R.N., C.C.R.C., Dana Raab, R.N., Cynthia Spikes, C.R.C., Jessica Woo, Ph.D., and data processing and data management staff in the Division of Biostatistics and Epidemiology at Cincinnati Children’ s Medical Center.
Supported by: Study 1 was supported by a CReFF award (PI: Zeller) Cincinnati Children’s Hospital Medical Center-General Clinical Research Center (USPHS grant M01 RR 08084 from the General Clinical Research Centers Program, National Center for Research Resources/National Institutes of Health), and the National Institutes of Health (R03 DK0788901; PI: Zeller). FABS5+ was supported by investigator initiated grants from Ethicon Endo-Surgery (grants 15161 and 15151.3) (PI: Inge). Dr. Hunsaker’s effort was supported by an NIH postdoctoral training grant (T32 DK063929).
Footnotes
Disclosures
Thomas H. Inge has received bariatric research grant funding from Ethicon Endo-Surgery. The other authors have no commercial associations that might be a conflict of interest in relation to this article.
References
- 1.Inge TH, Zeller MH, Jenkins TM, et al. Perioperative outcomes of adolescents undergoing bariatric surgery: the Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS) study. JAMA Pediatr. 2014;168(1):47–53. doi: 10.1001/jamapediatrics.2013.4296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Inge TH, Courcoulas AP, Jenkins TM, et al. Weight Loss and health status 3 years after bariatric surgery in adolescents. N Engl J Med. 2016;374(2):113–23. doi: 10.1056/NEJMoa1506699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Brien PE, Sawyer SM, Laurie C, et al. Laparoscopic adjustable gastric banding in severely obese adolescents: a randomized trial. JAMA. 2010;303(6):519–36. doi: 10.1001/jama.2010.81. [DOI] [PubMed] [Google Scholar]
- 4.Zitsman JL, DiGiorgi MF, Fennoy I, Kopchinski JS, Sysko R, Devlin MJ. Adolescent laparoscopic adjustable gastric banding (LAGB): prospective results in 137 patients followed for 3 years. Surg Obes Relat Dis. 2015;11(1):101–9. doi: 10.1016/j.soard.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Schmitt F, Riquin E, Beaumesnil M, et al. Laparoscopic adjustable gastric banding in adolescents: results at two years including psychosocial aspects. J Pediatr Surg. 2016;51(3):403–8. doi: 10.1016/j.jpedsurg.2015.08.057. [DOI] [PubMed] [Google Scholar]
- 6.Olbers T, Beamish AJ, Gronowitz E, et al. Laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity (AMOS): a prospective, 5-year, Swedish nationwide study. Lancet Diabetes Endocrinol. 2017;5(3):174–83. doi: 10.1016/S2213-8587(16)30424-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Inge TH, Jenkins TM, Xanthakos SA, et al. Long-term outcomes of bariatric surgery in adolescents with severe obesity (FABS-5+): a prospective follow-up analysis. Lancet Diabetes Endocrinol. 2017;5(3):165–73. doi: 10.1016/S2213-8587(16)30315-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. The CBHSQ Report: Serious Mental Health Challenges Among Older Adolescents and Young Adults. Rockville, MD: May 6, 2014. [monograph on the Internet] Available from: https://www.samhsa.gov/data/sites/default/files/sr173-mh-challenges-young-adults-2014/sr173-mh-challenges-young-adults-2014/sr173-mh-challenges-young-adults-2014.htm. Accessed March 1, 2017. [PubMed] [Google Scholar]
- 9.Zeller MH, Reiter-Purtill J. Psychosocial issues in adolescent bariatric surgery. In: Still C, Sarwer D, Blankenship J, editors. The ASMBS Textbook of Bariatric Surgery. Vol. 2. New York, NY: Springer; 2014. pp. 65–73. [Google Scholar]
- 10.Zeller MH, Modi AC, Noll JG, Long JD, Inge TH. Psychosocial functioning improves following adolescent bariatric surgery. Obesity (Silver Spring) 2009;17(5):885–90. doi: 10.1038/oby.2008.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zeller MH, Reiter-Purtill J, Ratcliff MB, Inge TH, Noll JG. Two-year trends in psychosocial functioning after adolescent Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2011;7(6):727–32. doi: 10.1016/j.soard.2011.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Järvholm K, Karlsson J, Olbers T, et al. Two-year trends in psychological outcomes after gastric bypass in adolescents with severe obesity. Obesity (Silver Spring) 2015;23(10):1966–72. doi: 10.1002/oby.21188. [DOI] [PubMed] [Google Scholar]
- 13.Järvholm K, Karlsson J, Olbers T, et al. Characteristics of adolescents with poor mental health after bariatric surgery. Surg Obes Relat Dis. 2016;12(4):882–90. doi: 10.1016/j.soard.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 14.de Zwaan M, Enderle J, Wagner S, et al. Anxiety and depression in bariatric surgery patients: A prospective, follow-up study using structured clinical interviews. J Affect Disord. 2011;133(1–2):61–8. doi: 10.1016/j.jad.2011.03.025. [DOI] [PubMed] [Google Scholar]
- 15.Kalarchian MA, King WC, Devlin MJ, et al. Psychiatric disorders and weight change in a prospective study of bariatric surgery patients: a 3-year follow-up. Psychosom Med. 2016;78(3):373–81. doi: 10.1097/PSY.0000000000000277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kolotkin RL, Zeller MH, Modi AC, et al. Assessing weight-related quality of life in adolescents. Obesity (Silver Spring) 2006;14(3):448–57. doi: 10.1038/oby.2006.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kolotkin RL, Crosby RD, Kosloski KD, Williams GR. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9(2):102–11. doi: 10.1038/oby.2001.13. [DOI] [PubMed] [Google Scholar]
- 18.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- 19.Achenbach TM, Rescorla LA. Manual for the ASEBA Adult Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2003. [Google Scholar]
- 20.Perrin EC, Stein RE, Drotar D. Cautions in using the Child Behavior Checklist: observations based on research about children with a chronic illness. J Pediatr Psychol. 1991;16(4):411–21. doi: 10.1093/jpepsy/16.4.411. [DOI] [PubMed] [Google Scholar]
- 21.Kolotkin RL, Davidson LE, Crosby RD, Hunt SC, Adams TD. Six-year changes in health-related quality of life in gastric bypass patients versus obese comparison groups. Surg Obes Relat Dis. 2012;8(5):625–33. doi: 10.1016/j.soard.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zabelina DL, Erickson AL, Kolotkin RL, Crosby RD. The effect of age on weight-related quality of life in overweight and obese individuals. Obesity (Silver Spring) 2009;17(7):1410–3. doi: 10.1038/oby.2009.43. [DOI] [PubMed] [Google Scholar]
- 23.Callahan ST, Cooper WO. Changes in ambulatory health care use during the transition to young adulthood. J Adolesc Health. 2010;46(5):407–13. doi: 10.1016/j.jadohealth.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 24.Fortuna RJ, Robbins BW, Halterman JS. Ambulatory care among young adults in the United States. Ann Intern Med. 2009;151(6):379–85. doi: 10.7326/0003-4819-151-6-200909150-00002. [DOI] [PubMed] [Google Scholar]
- 25.Nock MK, Green JG, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry. 2013;70(3):300–10. doi: 10.1001/2013.jamapsychiatry.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zeller MH, Washington GA, Mitchell JE, et al. Alcohol use risk in adolescents 2 years after bariatric surgery. Surg Obes Relat Dis. 2017;13(1):85–94. doi: 10.1016/j.soard.2016.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitchell JE, Crosby R, de Zwaan M, et al. Possible risk factors for increased suicide following bariatric surgery. Obesity (Silver Spring) 2013;21(4):665–72. doi: 10.1002/oby.20066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.King WC, Chen J, Mitchell JE, et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012;307(23):2516–25. doi: 10.1001/jama.2012.6147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Backman O, Stockeld D, Rasmussen F, Näslund E, Marsk R. Alcohol and substance abuse, depression and suicide attempts after Roux-en-Y gastric bypass surgery. Br J Surg. 2016;103(10):1336–42. doi: 10.1002/bjs.10258. [DOI] [PubMed] [Google Scholar]
- 30.Rofey DL, Zeller MH, Brode C, et al. TeenView Writing Group in cooperation with the Teen-LABS Consortium A multisite view of psychosocial risks in patients presenting for bariatric surgery. Obesity (Silver Spring) 2015;23(6):1218–25. doi: 10.1002/oby.21065. [DOI] [PubMed] [Google Scholar]
- 31.Sysko R, Devlin MJ, Hildebrandt TB, Brewer SK, Zitsman JL, Walsh BT. Psychological outcomes and predictors of initial weight loss outcomes among severely obese adolescents receiving laparoscopic adjustable gastric banding. J Clin Psychiatry. 2012;73(10):1351–7. doi: 10.4088/JCP.12m07690. [DOI] [PMC free article] [PubMed] [Google Scholar]


