Abstract
Background
The aim of this study was to examine how modifiable factors like satisfaction with cancer care and self-efficacy impact health-related quality of life (HRQoL) among Latino cancer survivors.
Methods
Latinos previously diagnosed with breast, prostate, or colorectal cancer (N = 288) completed questionnaires (Patient Satisfaction with Cancer Care Scale, Stanford Chronic Disease Self-Management Measures, Functional Assessment of Cancer Therapy-General) within two years following primary cancer treatment.
Results
Path model analyses demonstrated that satisfaction with cancer care was associated with greater HRQoL and that this relationship was explained by several facets of self-efficacy (i.e., confidence in managing: psychological distress, z = 3.81, p < .001; social support from close others, z = 2.46, p = .014; social/recreational activities, z = 3.30, p = .001; patient-provider communication, z = −3.72, p < .001). Importantly, foreign-born, less acculturated, and monolingual-Spanish speaking survivors reported lower self-efficacy in patient-provider communication; however, adjusting for acculturation, language, nativity, and other covariates did not alter these results.
Conclusions
Factors that contribute to HRQoL disparities in Latino cancer survivors relative to non-Latino whites, such as low income, less education, and lack of health insurance, can be difficult to address. The current findings underline the importance of self-efficacy in the context of patient-centered cancer care practices (e.g., patient inclusion in care decisions, sufficient time with provider, ready access to medical advice) and suggest that improving satisfaction with care may increase patients’ confidence in managing important aspects of their cancer experience and, in turn, improve HRQoL among Latino cancer survivors.
Keywords: satisfaction with care, self-efficacy, quality of life, patient-centered practices, patient-provider communication, Latino/Hispanic
Latino breast, prostate, and colorectal cancer survivors experience lower overall HRQoL than non-Latino white survivors.1–6 More specifically, Latina breast cancer survivors report worse treatment-related symptom bother (e.g., fatigue pain, nausea, and lymphedema) and greater distress and depressed mood than non-Latina white women.4 Similarly, Latino prostate cancer survivors report greater sexual and urinary dysfunction as well as worse physical and emotional wellbeing than non-Latino white survivors2,3 and Latino colorectal cancer survivors report greater social distress and worse emotional wellbeing than non-Latino white survivors.1,5 Yet, Latinos are highly underrepresented in cancer survivorship research and limited work has addressed these disparities.7 Furthermore, factors that contribute to health-related disparities in Latino cancer survivors, such as low income, less education, and lack of health insurance,8–10 can be difficult to address. Therefore, more research is needed to identify modifiable factors that can be targeted to improve HRQoL, particularly among Latino cancer survivors previously diagnosed with the three most common cancer types among Latinos: breast, prostate, and colorectal.11.
Greater satisfaction with cancer care predicts better HRQoL in Latino cancer survivors.12 However, Latino cancer survivors report lower overall satisfaction with cancer care and more difficulty accessing and coordinating cancer care.1,13 Spanish-speaking Latino cancer survivors, in particular, report lower satisfaction with cancer care14 and lower confidence and trust in their medical providers.1 Given these observed disparities in satisfaction with cancer care and evidence that cancer care satisfaction predicts HRQoL in Latino cancer survivors, we aimed to identify factors that may explain for the relationship between satisfaction with cancer care and HRQoL and provide possible targets for future intervention efforts. To this end, we selected a measure of satisfaction with cancer care (Patient Satisfaction with Cancer Care Scale15,16) that assesses modifiable patient-centered cancer care practices (e.g., patient inclusion in care decisions, sufficient time with provider, ready access to medical advice, timely appointments, courteous/respectful staff).
Greater self-efficacy, or perceived confidence in managing care and different life domains, may be a pathway by which satisfaction with cancer care influences HRQoL in Latino cancer survivors. Greater satisfaction with cancer care (including patient inclusion in care decisions, sufficient time and information for treatment decision-making, clear medical advice and recommendations) is associated with both greater self-efficacy in patient-provider communication among Latino cancer survivors12 and greater self-efficacy in managing healthcare among Latino medical patients.17 Furthermore, self-efficacy is a demonstrated mechanism by which psychosocial interventions improve wellbeing in cancer survivors18 and an important determinant of psychological adjustment in the context of coping with chronic stress.18–21 However, foreign-born, less acculturated, and primarily Spanish-speaking Latino patients report lower self-efficacy managing both their health and medical care.17 In the current study, we examined whether facets of self-efficacy (i.e., confidence in managing: patient-provider communication, psychological distress, physical symptoms, social support from close others, social/recreational activities, and chores) were associated with greater HRQoL in Latino cancer survivors, and explained the relationship between satisfaction with cancer care and greater HRQoL.
To our knowledge, this is the first study to examine whether multiple facets of self-efficacy explain the relationship between satisfaction with cancer care and HRQoL in a diverse, underrepresented sample of Latino breast, prostate, and colorectal cancer survivors. Consistent with previous research, it was hypothesized that satisfaction with cancer care would be associated with greater HRQoL. Furthermore, it was hypothesized that the relationship between satisfaction with cancer care and greater HRQoL would be explained by the relationship between satisfaction with cancer care and greater self-efficacy (i.e., perceived confidence in managing: patient-provider communication, psychological distress, physical symptoms, social support from close others, chores, and social/recreational activities). In light of previous research documenting the relationship of acculturation, language use, and nativity with both self-efficacy12,17 and satisfaction with care1,14 in Latino patients, we also examined relationship of these variables with satisfaction with cancer care, facets of self-efficacy, and HRQoL.
Method
Participants
The current sample (N = 288) was derived from baseline data of a National Cancer Institute (NCI) funded project that aimed to reduce symptom burden and improve adherence to treatment recommendations in Latino cancer survivors. Eligibility criteria included a diagnosis of breast, colorectal, or prostate cancer; completion of primary cancer treatment within the past 15 months; self-identified as Hispanic/Latino; and verbal fluency in Spanish or English. Potential participants with evidence of metastatic disease, current severe mental illness (e.g., psychosis), active suicidal ideation, and/or substance dependence within the past year were excluded.
Procedures
Potential participants were identified via medical chart review and recruited from major tertiary medical centers in Chicago and San Antonio. Upon recruitment, participants provided informed consent and completed a comprehensive psychosocial baseline in-person assessment (approximately 90 minutes) with trained bilingual interviewers. Participants had the option of completing the baseline assessment in English or Spanish based on their language preferences and were compensated $25 for participation, as well as parking and other transportation reimbursements. All measures have been translated and validated in both English and Spanish speaking samples with good to excellent psychometric properties. All procedures were approved by the Institutional Review Board (IRB) of each institution and were compliant with the Health Insurance Portability and Accountability Act (HIPPA). Data were collected between February 2012 and January 2015.
Measures
Sociodemographic and Cancer-Related Characteristics
A sociodemographics questionnaire was administered to assess age, marital status, parental status, race, ethnicity, nativity, immigration generation, language use, years living in the US, formal education, and combined household income. Electronic health records were reviewed to capture: diagnosis, stage, treatment type, months since diagnosis, and months since treatment completion.
Satisfaction with Cancer Care
The 18-item Patient Satisfaction with Cancer Care Scale15,16 assessed satisfaction with cancer care on a Likert-type scale from 1 (strongly disagree) to 4 (strongly agree). Sample items include: “I felt included in decisions about my health,” “I had enough time with my doctor,” “I was treated with courtesy and respect,” “My doctors seemed to communicate well about my care,” “Making an appointment was easy,” “I knew who to contact when I had a question.” This scale demonstrated excellent internal consistency in this sample (overall α = .94; English version α = .94; Spanish version α = .95).
Self-Efficacy
The 24-item self-efficacy scale of the Stanford Chronic Disease Self-Management Measures22,23 assessed perceived confidence in managing patient-provider communication, psychological distress, physical symptoms, social support from close others, social/recreational activities, and chores on a Likert-type scale from 1 (not at all confident) to 5 (totally confident). Sample items include: “How confident are you that you can discuss openly with your doctor any personal problems that may be related to your illness?” (patient-provider communication), “How confident are you that you can do something to make yourself feel better when you feel sad or down in the dumps?” (psychological distress), “How confident are you that you can reduce your physical discomfort or pain?” (physical symptoms), “How confident are you that you can get emotional support from friends and family?” (social support), “How confident are you that you can continue to do your hobbies and recreation?” (social/recreational activities), and “How confident are you that you can get your errands done despite your health problems?” (chores). These scales demonstrated good to excellent internal consistency in this sample (overall α = .78 – .95; English version α = .78 – .95; Spanish version α = .78 – .95).
Health Related Quality of Life (HRQoL)
The 27-item Functional Assessment of Cancer Therapy-General (FACT-G) scale24,25 assessed HRQoL, including facets of physical, functional, social, and emotional well-being on a Likert-type scale from 0 (not at all) to 4 (very much). Sample items include: “I am bothered by side effects of treatment” (physical, reverse-coded), “I am able to work” (functional), “I am satisfied with family communication about my illness” (social), and “I worry about dying” (emotional, reverse-coded). This scale demonstrated excellent internal consistency in this sample (overall α = .91; English version α = .92; Spanish version α = .90).
Acculturation
The 12-item Short Acculturation Scale for Hispanics26 assessed US acculturation, including English language use, English language media, and social relations with non-Latino US Americans on Likert-type scales. Sample language items include (1 [only Spanish] to 5 [only English]): “In general, what language(s) do you read and speak?” (English language use) and “In what language(s) are the T.V. programs you usually watch?” (English language media). Sample social relations items include (1 [all Latinos/Hispanics] to 5 [all US Americans]): “Your close friends are ____.” and “The persons you visit or who visit you are ____.” This scale demonstrated excellent internal consistency in this sample (overall α = .93; English version α = .83; Spanish version α = .85).
Statistical Analyses
Relations between measures of interest and acculturation, sociodemographic characteristics (i.e., age, gender, primary language, nativity, income, educational history, and marital status) and cancer-related variables (i.e., cancer stage, cancer type, months since diagnosis, and months since treatment completion) were assessed using zero-order bivariate correlations, independent t-tests, and one-way analyses of variance (ANOVAs).
Path Model Analyses
Path model analyses were conducted in order to simultaneously examine the direct and indirect effects of satisfaction with cancer care and multiple facets of self-efficacy on HRQoL. These analyses also allowed us to examine which self-efficacy subscales emerged as significant predictors of HRQoL when the effects of all six self-efficacy subscales are modeled simultaneously. Path model analyses were estimated using maximum likelihood with missing values (MLMV) in STATA 14.0 (StataCorp). This estimation method allows data from all participants to be included in path model analyses (i.e., each participant’s available data is included in the model to estimate all other parameters). Models included paths from satisfaction with cancer care to facets of self-efficacy as well as paths from each facet of self-efficacy to HRQoL. Given that facets of self-efficacy are positively correlated (i.e., covary), the self-efficacy subscales were allowed to covary within path models in order to account for their significant correlations. The ability to covary variables that are significantly correlated and account for their shared variance is a unique strength of path model analysis.27,28 A direct path from satisfaction with cancer care to HRQoL was also included in order to examine whether facets of self-efficacy accounted for the direct effect between satisfaction with cancer care and HRQoL. Indirect effects of satisfaction with cancer care on HRQoL through each facet of self-efficacy were calculated. Facets of self-efficacy that did not demonstrate a significant direct effect on HRQoL were pruned from the model. Analyses controlling for covariates (i.e., relationships between measures of interest with acculturation, relevant sociodemographic/cancer characteristics) were also conducted. In order to examine an alternative model, we also conducted path model analyses in which the predictor and mediators were reversed (i.e., satisfaction with cancer care was modeled as the mediator of the effects of facets of self-efficacy on HRQoL). Model fit was evaluated according to criteria proposed by Hu and Bentler.29 The Tucker-Lewis Index (TLI) and Comparative Fit Index (CFI) are scaled as goodness-of-fit indices that range from 0 to 1 with higher values indicating better model fit. In accordance with the Hu and Bentler criteria, a value greater than or equal to .95 was used as a cutoff score to indicate good model fit. The Root Mean Square Error of Approximation (RMSEA) is scaled as a badness-of-fit index that ranges from 0 to 1 with lower values indicating better model fit. In accordance with the Hu and Bentler criteria, a RMSEA value less than or equal to .06 was used as a cutoff score to indicate good model fit.
Results
Table 1 displays the sociodemographic characteristics of the sample. Participants were on average 56 years old (M = 56.05, SD = 10.20), married or cohabitating (61.5%), and had children (87.8%). Most participants reported a high school education or less (65.6%) and a combined household income less than $50,000 (68.4%) with approximately half of the sample reporting a combined household income less than $25,000 (48.9%). Participants represented a variety of countries/regions of origin, including Mexico (80.6%), South America (6.2%), and Puerto Rico (5.2%). Most participants were foreign born (59.4%) and were either monolingual Spanish-speaking (54.2%) or English-Spanish bilingual (26.0%). Table 2 displays the medical characteristics. Participants were on average diagnosed 17 months previously (M = 17.14, SD = 19.33) with breast (44.4%), colorectal (24.3%), and prostate (31.3%) cancer. The majority of participants were diagnosed with Stage 0 (2.1%), I (20.1%), and II (35.4%) cancers and one-quarter of participants were diagnosed with Stage III (25.0%). Few participants received neoadjuvant chemotherapy (16.0%), however approximately one-third received adjuvant chemotherapy (31.3%). Approximately half of participants received radiation (56.6%) and hormone therapy (46.9%). As demonstrated in Tables 1 and 2, there were significant differences by cancer type in some sociodemographic and cancer covariates (i.e., age, years living in the US, gender, months since cancer diagnosis and treatment completion, cancer stage, and treatment type).
Table 1.
Sociodemographic Characteristics
| Combined | Breast Cancer | Prostate Cancer | Colorectal Cancer | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| (N = 288) | (n = 128) | (n = 90) | (n = 70) | ||||||
| Age, mean (SD) | 56.05 | (10.20) | 51.44 | (9.13) | 63.07 | (8.23) | 55.03 | (9.30) | F(2,279) = 44.83, p< .001, η2= .25 |
| Years living in US, mean (SD) | 28.65 | (14.48) | 24.64 | (14.21) | 32.89 | (14.52) | 29.68 | (12.97) | F(2, 175) = 6.13, p = .003, η2 = .07 |
| Gender, % (n) | χ2(2) = 221.27, p< .001, Cramer’s V = .88 | ||||||||
| Female | 53.8 | (155) | 100 | (128) | 0 | (0) | 38.6 | (27) | |
| Male | 46.2 | (133) | 0 | (0) | 100 | (90) | 61.4 | (43) | |
| Race, % (n) | χ2(8) = 9.45, n.s., Cramer’s V = .13 | ||||||||
| White | 88.2 | (254) | 86.7 | (111) | 86.7 | (78) | 92.9 | (65) | |
| Black | .3 | (1) | 0 | (0) | 1.1 | (1) | 0 | (0) | |
| Native American | .3 | (1) | 0 | (0) | 1.1 | (1) | 0 | (0) | |
| Other | 8.7 | (25) | 10.2 | (13) | 9.0 | (9) | 4.3 | (3) | |
| Unknown | 2.1 | (6) | 3.1 | (4) | 0 | (0) | 2.8 | (2) | |
| Missing | .3 | 1 | 0 | (0) | 1.1 | (1) | 0 | (0) | |
| Ethnicity, % (n) | |||||||||
| Hispanic/Latino | 100 | (288) | 100 | (128) | 100 | (90) | 100 | (70) | |
| Country/Territory of Origin, % (n) | χ2(24) = 21.88, n.s., Cramer’s V = .20 | ||||||||
| Mexico | 80.6 | (232) | 78.1 | (100) | 84.4 | (76) | 80.0 | (56) | |
| Puerto Rico | 5.2 | (15) | 4.7 | (6) | 6.7 | (6) | 4.3 | (3) | |
| Central America | 1.7 | (5) | 3.1 | (4) | 1.1 | (1) | 0 | (0) | |
| South America | 6.2 | (18) | 6.3 | (8) | 6.7 | (6) | 5.7 | (4) | |
| Caribbean | 1.0 | (3) | 1.5 | (2) | 0 | (0) | 1.4 | (1) | |
| Other | 1.0 | (3) | 1.5 | (2) | 1.1 | (1) | 0 | (0) | |
| Unknown | .7 | (2) | 0 | (0) | 0 | (0) | 2.9 | (2) | |
| Missing | 3.5 | (10) | 4.7 | (6) | 0 | (0) | 5.7 | (4) | |
| Language, % (n) | χ2(4) = 8.14, n.s., Cramer’s V = .12 | ||||||||
| English monolingual | 17.0 | (49) | 15.6 | (20) | 15.6 | (14) | 21.4 | (15) | |
| Spanish monolingual | 54.2 | (156) | 49.2 | (63) | 66.7 | (60) | 47.1 | (33) | |
| English-Spanish bilingual | 26.0 | (75) | 30.5 | (39) | 17.8 | (16) | 28.6 | (20) | |
| Missing | 2.8 | (8) | 4.7 | (6) | 0 | (0) | 2.9 | (2) | |
| Nativity, % (n) | χ2(2) = 3.08, n.s., Cramer’s V = .11 | ||||||||
| US Born | 37.8 | (109) | 36.7 | (47) | 33.3 | (30) | 45.7 | (32) | |
| Foreign Born | 59.4 | (171) | 58.6 | (75) | 66.7 | (60) | 51.4 | (36) | |
| Missing | 2.8 | (8) | 4.7 | (6) | 0 | (0) | 2.9 | (2) | |
| Immigrant Generation, % (n) | χ2(14) = 14.94, n.s., Cramer’s V = .16 | ||||||||
| 1st generation | 56.6 | (163) | 52.3 | (67) | 67.8 | (61) | 50.0 | (35) | |
| 2nd generation | 12.8 | (37) | 12.5 | (16) | 12.2 | (11) | 14.2 | (10) | |
| 3rd generation | 10.8 | (31) | 14.0 | (18) | 5.5 | (5) | 11.4 | (8) | |
| 4th generation | 6.6 | (19) | 4.6 | (6) | 7.7 | (7) | 8.5 | (6) | |
| 5th generation | 6.9 | (20) | 7.8 | (10) | 5.5 | (5) | 7.1 | (5) | |
| Not Applicable | 2.1 | (6) | 2.3 | (3) | 0 | (0) | 4.2 | (3) | |
| Unknown | .7 | (2) | 0.8 | (1) | 0 | (0) | 1.4 | (1) | |
| Missing | 3.4 | (10) | 5.4 | (7) | 1.1 | (1) | 2.9 | (2) | |
| Household Income, % (n) | χ2(20) = 23.11, n.s., Cramer’s V = .20 | ||||||||
| Less than $11,9999 | 22.2 | (64) | 21.8 | (28) | 18.8 | (17) | 27.1 | (19) | |
| Between $12,000 and $24,999 | 26.7 | (77) | 26.5 | (34) | 30.0 | (27) | 22.8 | (16) | |
| Between $25,000 and $49,999 | 19.5 | (56) | 20.3 | (26) | 18.8 | (17) | 18.5 | (13) | |
| Between $50,000 and $99,999 | 9.8 | (28) | 6.2 | (8) | 13.3 | (12) | 11.4 | (8) | |
| More than $100,000 | 5.6 | (16) | 7.8 | (10) | 4.4 | (4) | 2.9 | (2) | |
| Unknown | 12.5 | (36) | 10.1 | (13) | 14.4 | (13) | 14.2 | (10) | |
| Missing | 3.8 | (11) | 7.0 | (9) | 0 | (0) | 2.9 | (2) | |
| Educational History, % (n) | χ2(18) = 18.19, n.s., Cramer’s V = .18 | ||||||||
| Less than high school | (113) | 30.4 | (39) | 44.4 | (40) | 48.5 | (34) | ||
| High school or equivalency (GED) | (76) | 25.7 | (33) | 25.5 | (23) | 28.5 | (20) | ||
| Associate’s degree | (18) | 7.0 | (9) | 4.4 | (4) | 7.1 | (5) | ||
| Bachelor’s degree | (23) | 8.6 | (11) | 11.1 | (10) | 2.9 | (2) | ||
| Master’s degree | (6) | 3.1 | (4) | 2.2 | (2) | 0 | (0) | ||
| Doctoral degree (PhD, DPhil) | (3) | .8 | (1) | 1.1 | (1) | 1.4 | (1) | ||
| Professional degree (MD, JD, DDS) | (2) | .8 | (1) | 0 | (0) | 1.4 | (1) | ||
| Other | (9) | 4.6 | (6) | 2.2 | (2) | 1.4 | (1) | ||
| Missing | (38) | 18.7 | (24) | 8.8 | (8) | 8.5 | (6) | ||
| Relationship Status, % (n) | χ2(10) = 16.08, n.s., Cramer’s V = .17 | ||||||||
| Single | 11.5 | (33) | 10.9 | (14) | 8.8 | (8) | 15.7 | (11) | |
| Married or Living with Partner | 61.5 | (177) | 56.2 | (72) | 76.6 | (69) | 51.4 | (36) | |
| Dating | .3 | (1) | 0 | (0) | 0 | (0) | 1.4 | (1) | |
| Separated | 5.6 | (16) | 7.8 | (10) | 3.3 | (3) | 4.2 | (3) | |
| Divorced | 13.5 | (39) | 14.8 | (19) | 7.7 | (7) | 18.5 | (13) | |
| Widowed | 4.9 | (14) | 5.4 | (7) | 3.3 | (3) | 5.7 | (4) | |
| Missing | 2.8 | (8) | 4.6 | (6) | 0 | (0) | 2.9 | (2) | |
| Parental Status, % (n) | χ2(2) = 1.42, n.s., Cramer’s V = .07 | ||||||||
| Yes | 87.8 | (253) | 8.6 | (11) | 7.7 | (7) | 12.8 | (9) | |
| No | 9.4 | (27) | 86.7 | (111) | 92.2 | (83) | 84.2 | (59) | |
| Missing | 2.8 | (8) | 4.6 | (6) | 0 | (0) | 2.9 | (2) | |
Table 2.
Medical & Cancer Characteristics
| Combined | Breast Cancer | Prostate Cancer | Colorectal Cancer | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| (N = 288) | (n = 128) | (n = 90) | (n = 70) | ||||||
| Months since Diagnosis, mean (SD) | 11.98 | (5.53) | 11.16 | (5.04) | 11.78 | (5.45) | 13.76 | (6.17) | F(2, 245) = 4.81, p = .009, η2 = .04 |
| Months since Treatment, mean (SD) | 5.00 | (4.38) | 3.92 | (3.68) | 5.17 | (4.57) | 6.64 | (4.78) | F(2, 234) = 8.05, p< .001, η2 = .06 |
| Cancer Type, % (n) | |||||||||
| Prostate | 31.3 | (90) | 0 | (0) | 100 | (90) | 0 | (0) | |
| Breast | 44.4 | (128) | 100 | (128) | 0 | (0) | 0 | (0) | |
| Colorectal | 24.3 | (70) | 0 | (0) | 0 | (0) | 100 | (70) | |
| Cancer Stage, % (n) | χ2(8) = 53.61, p< .001, Cramer’s V = .34 | ||||||||
| 0 | 2.1 | (6) | 4.7 | (6) | 0 | (0) | 0 | (0) | |
| I | 20.1 | (58) | 33.5 | (43) | 10.0 | (9) | 8.5 | (6) | |
| II | 35.4 | (102) | 35.1 | (45) | 42.2 | (38) | 27.1 | (19) | |
| III | 25.0 | (72) | 14.0 | (18) | 22.2 | (20) | 48.5 | (34) | |
| Missing | 17.3 | (50) | 12.5 | (16) | 25.5 | (23) | 15.7 | (11) | |
| Treatment Type, % (n) | |||||||||
| Neoadjuvant Chemotherapy | 16.0 | (46) | 16.4 | (21) | 0 | (0) | 35.7 | (25) | χ2(4) = 43.94, p< .001, Cramer’s V = .29 |
| Adjuvant Chemotherapy | 31.3 | (90) | 39.8 | (51) | 1.1 | (1) | 54.3 | (38) | χ2(4) = 74.93, p< .001, Cramer’s V = .38 |
| Radiation Therapy | 56.6 | (163) | 63.3 | (81) | 62.2 | (56) | 37.1 | (26) | χ2(4) = 19.59, p = .001, Cramer’s V = .19 |
| Hormone Therapy | 46.9 | (135) | 75.8 | (97) | 29.7 | (38) | 0 | (0) | χ2(4) = 122.77, p< .001, Cramer’s V = .47 |
| Immunotherapy | 7.6 | (22) | 16.4 | (21) | 1.1 | (1) | 0 | (0) | χ2(4) = 52.80, p< .001, Cramer’s V = .31 |
| Study Site, % (n) | |||||||||
| San Antonio | 59.4 | (171) | 57.8 | (74) | 55.6 | (50) | 67.1 | (47) | χ2(2) = 2.43, n.s., Cramer’s V = .09 |
| Chicago | 40.6 | (117) | 42.2 | (54) | 44.4 | (40) | 32.9 | (23) | |
Note. Patients with stage IV cancer were not eligible.
Table 3 displays descriptive statistics for primary variables. Compared to norms derived from primarily non-Hispanic/Latino white survivors, the current sample of Latino cancer survivors reported lower overall HRQoL (FACT-G).25 Across the subscales of self-efficacy, participants on average endorsed feeling ‘somewhat confident’ to ‘quite a bit confident’ in their ability to manage: patient-provider communication, psychological distress, physical symptoms, support from close others, social/recreational activities, and chores (with a standard deviation of approximately one point on a 5-point Likert-type scale). The six facets of self-efficacy were positively correlated (r’s = .48 – .81, p’s < .001). Breast cancer survivors reported worse HRQoL (F(2, 275) = 5.31, p = .005) and lower confidence managing chores (F(2, 271) = 4.64, p = .010) than prostate cancer survivors (no difference between colorectal cancer survivors and either group). Furthermore, breast cancer survivors report lower confidence managing: psychological distress (F(2, 273) = 4.68, p = .010) and physical symptoms (F(2, 271) = 6.12, p = .003) than both prostate and colorectal survivors (no difference between colorectal and prostate cancer survivors). Similarly, women reported lower HRQoL (t(276) = −2.31, p = .022) and confidence in managing: psychological distress (t(274) = −2.73, p = .007), physical symptoms (t(272) = −2.92, p = .004), and chores (t(272) = −3.15, p = .002) than men.
Table 3.
Descriptive Statistics for Primary Variables
| Measure | Mean | (SD) |
|---|---|---|
| Satisfaction with Cancer Care | ||
| Patient Satisfaction with Cancer Care | 80.64 | (9.25) |
| Health Related Quality of Life (HRQoL) | ||
| FACT – General | 80.36 | (16.27) |
| Facets of Self-Efficacy | ||
| Stanford Chronic Disease Self-Management Measures | ||
| Patient-Provider Communication | 4.29 | (.88) |
| Psychological Distress | 3.82 | (.93) |
| Physical Symptoms | 3.77 | (.97) |
| Social Support from Close Others | 3.85 | (.96) |
| Chores | 3.92 | (1.05) |
| Social/Recreational Activities | 3.83 | (1.14) |
Sociodemographic & Cancer Covariates
Acculturation, language use, and nativity were uniquely associated with self-efficacy in patient-provider communication. Acculturation to the US was positively correlated with self-efficacy in patient-provider communication (r = .13, p = .030) and foreign-born participants reported lower self-efficacy in patient-provider communication than US-born participants (t(274) = −2.90, p = .004). Bilingual English-Spanish speakers also reported greater self-efficacy in patient-provider communication than monolingual Spanish speakers (F(2, 273) = 4.41, p = .013; English monolingual speakers did not differ). Age was positively correlated with HRQoL (r = .13, p = .028) and confidence managing: patient-provider communication (r = .13, p = .036), psychological distress (r = .14, p = .024), and physical symptoms (r = .15, p = .011). Combined household income was also positively correlated with HRQoL (rs = .16, p = .007) and confidence managing: psychological distress (rs = .14, p = .023) and chores (rs = .12, p = .043). Married participants reported greater HRQoL (t(276) = 3.09, p = .002) and confidence managing social support from close others (t(273) = 2.53, p = .012) than those not married. More advanced cancer stage was positively correlated with confidence managing patient-provider communication (rs = .17, p =.012), psychological distress (rs = .15, p = .022), physical symptoms (rs = .17, p = .011), and chores (rs = .18, p = .006). (We note the importance of interpreting associations between sociodemographic/cancer covariates and primary variables of interest with caution given that these correlations are significant, but modest in magnitude.) All other associations between acculturation and sociodemographic/cancer characteristics, including both time since diagnosis and treatment completion, with primary measures (i.e., satisfaction with cancer care, facets of self-efficacy, and HRQoL) were non-significant.
Path Model Analyses
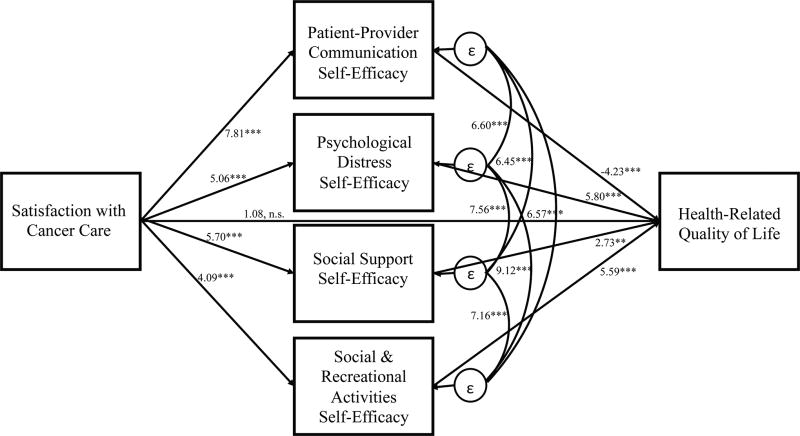
Path analyses simultaneously examining the direct and indirect effects of satisfaction with cancer care and facets of self-efficacy on HRQoL demonstrated that two facets of self-efficacy, confidence managing physical symptoms (z = .63, p = .529) and chores (z = 1.05, p = .296), were not significantly associated with HRQoL. The modified path analysis pruning these two facets of self-efficacy (Figure 1) demonstrated excellent overall fit (CFI = 1.00, TLI = 1.00, RMSEA < .001) and explained a proportion of variance in HRQoL (R2 = .46). Satisfaction with cancer care was significantly associated with greater confidence in managing: patient-provider communication (z = 7.81, p < .001), psychological distress (z = 5.06, p < .001), social support from close others (z = 5.70, p < .001), and social/recreational activities (z = 4.09, p < .001), which in turn were significantly associated with greater HRQoL (confidence in managing: psychological distress, z = 5.80, p < .001; social support from close others, z = 2.73, p = .006; social/recreational activities, z = 5.59, p < .001; patient-provider communication, z = −4.23, p < .001).1 All four facets of self-efficacy were significantly positively associated with one another (z’s = 6.45 – 9.12, p < .001). Indirect effect analyses demonstrated significant indirect effects of satisfaction with cancer care on HRQoL through its association with these four facets of self-efficacy (confidence in managing: psychological distress, z = 3.81, p < .001; social support from close others, z = 2.46, p = .014; social/recreational activities, z = 3.30, p = .001; patient-provider communication, z = −3.72, p < .001), which accounted for its direct association with HRQoL and rendered this effect non-significant (z = 1.08, p = .282). Importantly, this pattern of results was not altered in path analyses controlling for relationships between covariates (i.e., acculturation, language use, nativity, cancer type and stage, age, gender, income, marital status) with satisfaction with cancer care, facets of self-efficacy, and HRQoL. Results from the alternative model, in which satisfaction with cancer care was modeled as the mediator of the effects of facets of self-efficacy on HRQoL, demonstrated that satisfaction with cancer care did not explain the relationship between facets of self-efficacy and HRQoL (i.e., facets of self-efficacy continued to demonstrate significant direct effects on HRQoL [p <.001 – .006] while the direct effect of satisfaction with cancer care on HRQoL was non-significant [p = .282]).
Figure 1.
Path model (N = 288) of the direct and indirect effects of satisfaction with cancer care, facets of self-efficacy, and health-related quality of life (HRQoL). Standardized path coefficients are shown. *p < .05. **p < .01. ***p < .001. n.s. = non-significant.
Conclusions
Despite evidence that Latinos experience significantly greater decrements in health-related quality of life (HRQoL) relative to non-Latino whites following the diagnosis and treatment of cancer,6 including the three most common cancers among Latinos: breast,4 prostate,2,3 and colorectal,1,5 Latinos are underrepresented in cancer survivorship research.7 Furthermore, factors that contribute to health-related disparities in Latino cancer survivors, such as low income, less education, and lack of health insurance,8–10 can be difficult to address. Therefore, the aim of the current study was to examine how modifiable factors such as satisfaction with cancer care and self-efficacy impact HRQoL in Latino breast, prostate, and colorectal cancer survivors. More specifically, we examined whether facets of self-efficacy (confidence in managing: patient-provider communication, psychological distress, physical symptoms, social support from close others, social/recreational activities, and chores) explained the relationship between satisfaction with cancer care and greater HRQoL. Furthermore, our unique sample of primarily immigrant, Spanish-speaking, socioeconomically-disadvantaged Latino cancer survivors also allowed us to examine the influence of language use, acculturation, and nativity on these factors.
Results demonstrated that both satisfaction with cancer care and facets of self-efficacy were associated with greater HRQoL in Latino cancer survivors. Furthermore, path model analyses demonstrated that four facets of self-efficacy (i.e., patients’ perceived confidence in managing: patient-provider communication, psychological distress, social support, and social/recreational activities) explained the relationship between satisfaction with cancer care and greater HRQoL. Importantly, the satisfaction with cancer care measure used in this study (Patient Satisfaction with Cancer Care Scale15,16) assessed modifiable patient-centered cancer care practices (e.g., patient inclusion in care decisions, sufficient time with provider, ready access to medical advice, timely appointments, courteous/respectful staff) that can be targeted to improve patient satisfaction. Thus, findings underline the importance of implementing patient-centered cancer care practices and suggest that improving satisfaction with cancer care may increase patients’ confidence in managing important aspects of their cancer experience and, in turn, improve HRQoL and wellbeing among Latino cancer survivors. Interventions that include coping skills training19,21 or facilitate communication and social support30 may also be effective in improving self-efficacy among Latino cancer survivors as self-efficacy has been shown to mediate the effects of these interventions on improved quality of life in patients with chronic illness, including cancer.18 More research is needed to determine the viability of improving HRQoL by targeting satisfaction with cancer care and self-efficacy in Latino cancer survivors.
Previous research demonstrates that foreign-born, less acculturated, and Spanish-speaking Latino cancer survivors demonstrate lower satisfaction with cancer care1,14 and self-efficacy in managing patient-provider communication.12,17 We similarly found that foreign-born, less acculturated, and monolingual-Spanish speaking survivors reported lower self-efficacy in patient-provider communication. Furthermore, higher income was also associated with greater HRQoL and self-efficacy, including confidence managing psychological distress and chores. Of note, across the subscales of self-efficacy, participants on average endorsed feeling ‘somewhat confident’ to ‘quite a bit confident’ in their ability to manage to manage: patient-provider communication, psychological distress, physical symptoms, support from close others, social/recreational activities, and chores. Despite a somewhat high average endorsement, there was variance in responses, underlining the importance of identifying factors that are associated with lower self-efficacy. These findings highlight the importance of considering acculturation, language use, nativity, and income when working with Latino survivors in cancer care settings, as these factors may identify survivors that are more likely to experience decrements in HRQoL and self-efficacy and need additional support. Nevertheless, results should be interpreted in the context of the higher overall endorsement of self-efficacy in this sample as this may have biased results. Future studies should examine the effects of satisfaction with cancer care and self-efficacy in Latino cancer survivor samples with lower overall endorsements of self-efficacy in order to assess whether the associations observed in this study hold across a range of responses, including very low levels of self-efficacy.
Breast cancer survivors reported worse HRQoL and lower self-efficacy, including lower confidence in managing: psychological distress, physical symptoms, and chores, than prostate and colorectal cancer survivors. Given that gender was highly collinear with cancer type in this sample, it is not surprising that analyses examining gender differences replicated this pattern of results and demonstrated that Latina women experienced lower HRQoL and self-efficacy than men. Importantly, these findings suggest that Latina breast cancer survivors not only experience greater decrements in HRQoL when compared to non-Latino white women (for review see4, but also when compared to Latino survivors diagnosed with the two other most common cancers in this population, prostate and colorectal. Therefore, the viability of improving HRQoL in Latina breast cancer survivors by targeting patient-centered cancer care practices, satisfaction with cancer care, and facets of self-efficacy is an important future direction. Although more advanced cancer stage was associated with greater self-efficacy (including confidence managing: patient-provider communication, psychological distress, physical symptoms, and chores), this finding should be interpreted with caution since our study highly oversampled participants with early-stage disease (i.e., stages 0 to II) and excluded those with stage IV, resulting in truncated variance in this variable. Nevertheless, it is possible that in the very specific context of primarily early-stage, non-metastatic Latino cancer survivors higher stage disease provides more experience navigating clinical care and managing cancer-related symptoms and distress, thus resulting in higher levels of perceived confidence to manage these aspects of the cancer experience.
Strengths & Limitations
This study has several strengths, including its unique sample of underrepresented Latino cancer survivors and the use of path model analyses to examine the direct and indirect pathways through which satisfaction with cancer care experiences and facets of self-efficacy contribute to HRQoL. An additional strength of the current study is its focus on modifiable factors that may reduce disparities in HRQoL in Latino cancer survivors, as these factors can inform future intervention research. The primary limitation of this study is its cross-sectional design. Causal inference cannot be concluded given the cross-sectional design, however, we conducted analyses testing an alternative model reversing the direction of effects (i.e., whether satisfaction with cancer care explained the relationship between facets of self-efficacy and HRQoL), which was not supported. Future research should employ longitudinal designs in order to examine how these relationships unfold across time. In particular, a prospective design that establishes temporal precedence between satisfaction with cancer care, self-efficacy, and changes across time in HRQoL is recommended. Future research should also examine the influence of providers’ cultural competency and empathy31 on satisfaction with cancer care, self-efficacy, and HRQoL among Latino cancer survivors, particularly those who are foreign-born, less acculturated, and monolingual-Spanish speaking.
Acknowledgments
Findings underline the importance of implementing patient-centered practices in cancer care and suggest that improving satisfaction with cancer care may increase Latino cancer survivors’ confidence in managing important aspects of their cancer experience and, in turn, improve their quality of life. Importantly, foreign-born, less acculturated, and monolingual-Spanish speaking Latino cancer survivors report lower confidence managing patient-provider communication.
Source of Funding: Research supported by a National Cancer Institute grant (U54CA153511) awarded to A.G.R and F.J.P and a Susan G. Komen for the Cure grant (SAB-08-00005) awarded to A.G.R. P.I.M and R.S.F. were supported through a National Cancer Institute Training Grant (5T32CA193193).
Footnotes
All the authors contributed to this research and article. Conceptualization: Patricia I. Moreno, Frank J. Penedo, Amelie G. Ramirez: Data Curation: Ryne Estabrook, Edgar Munoz, Arely, Perez, Leopoldo Castillo; Formal Analysis: Patricia I. Moreno, Ryne Estabrook, Edgar Munoz; Funding Acquisition: Amelie G. Ramirez, Frank J. Penedo; Investigation: Amelie G. Ramirez, Sandra L. San Miguel-Majors, Leopoldo Castillo, Kipling J. Gallion, Edgar Munoz, Ryne Estabrook, Arely Perez, MS2, Thomas Lad, Courtney Hollowell, Frank J. Penedo; Methodology: Frank J. Penedo, Amelie G. Ramirez; Project, Patricia I. Moreno; Project Administration: Amelie G. Ramirez, Frank J. Penedo, Arely Perez, Leopoldo Castillo; Resources: Amelie G. Ramirez, Frank J. Penedo; Software: Ryne Estabrook, Edgar Munoz, Patricia I. Moreno; Supervision: Amelie G. Ramirez, Frank J. Penedo; Validation: Patricia I. Moreno, Edgar Munoz, Frank J. Penedo, Amelie G. Ramirez; Visualization: Patricia I. Moreno; Writing - Original Draft: Patricia I. Moreno, Amelie G. Ramirez, Sandra L. San Miguel-Majors, Rina S. Fox, Leopoldo Castillo, Kipling J. Gallion, Edgar Munoz, Ryne Estabrook, Arely Perez, Thomas Lad, Courtney Hollowell, Frank J. Penedo; Writing - Review and Editing: Patricia I. Moreno, Amelie G. Ramirez, Sandra L. San Miguel-Majors, Rina S. Fox, Leopoldo Castillo, Kipling J. Gallion, Edgar Munoz, Ryne Estabrook, Arely Perez, Thomas Lad, Courtney Hollowell, Frank J. Penedo.
None of the authors have any conflicts of interest to declare.
The total effect of patient-provider communication on HRQoL was positive, as expected; however there was a suppression effect when simultaneously modeling the four facets of self-efficacy.
References
- 1.Ayanian JZ, Zaslavsky AM, Guadagnoli E, et al. Patients’ perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol. 2005;23(27):6576–6586. doi: 10.1200/JCO.2005.06.102. [DOI] [PubMed] [Google Scholar]
- 2.Penedo FJ, Dahn JR, Shen B-J, Schneiderman N, Antoni MH. Ethnicity and determinants of quality of life after prostate cancer treatment. Urology. 2006;67(5):1022–1027. doi: 10.1016/j.urology.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 3.Rosser CJ, Kuban DA, Levy LB, et al. Clinical features and treatment outcome of Hispanic men with prostate cancer following external beam radiotherapy. J Urol. 2003;170(5):1856–1859. doi: 10.1097/01.ju.0000092880.23660.de. [DOI] [PubMed] [Google Scholar]
- 4.Yanez B, Thompson EH, Stanton AL. Quality of life among Latina breast cancer patients: A systematic review of the literature. J Cancer Surviv. 2011;5(2):191–201. doi: 10.1007/s11764-011-0171-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yost KJ, Hahn EA, Zaslavsky AM, Ayanian JZ, West DW. Predictors of health-related quality of life in patients with colorectal cancer. Health Qual Life Outcomes. 2008;6:66. doi: 10.1186/1477-7525-6-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luckett T, Goldstein D, Butow PN, et al. Psychological morbidity and quality of life of ethnic minority patients with cancer: A systematic review and meta-analysis. Lancet Oncol. 2011;12(13):1240–1248. doi: 10.1016/S1470-2045(11)70212-1. [DOI] [PubMed] [Google Scholar]
- 7.Ramirez AG, Gallion KJ, Suarez L, et al. A national agenda for Latino cancer prevention and control. Cancer. 2005;103(11):2209–2215. doi: 10.1002/cncr.21053. [DOI] [PubMed] [Google Scholar]
- 8.Flores G. Language barriers to health care in the United States. N Engl J Med. 2006;355(3):229–231. doi: 10.1056/NEJMp058316. [DOI] [PubMed] [Google Scholar]
- 9.Freeman G, Lethbridge-Cejku M. Access to health care among Hispanic or Latino women: United States, 2000–2002. Adv Data. 2006;(368):1–25. [PubMed] [Google Scholar]
- 10.Kirby JB, Taliaferro G, Zuvekas SH. Explaining racial and ethnic disparities in health care. Med Care. 2006;44(5):I–64. doi: 10.1097/01.mlr.0000208195.83749.c3. [DOI] [PubMed] [Google Scholar]
- 11.American Cancer Society. Cancer Facts & Figures for Hispanics/Latinos 2015–2017. Atlanta, GA: American Cancer Society; 2015. [Google Scholar]
- 12.Yanez B, Stanton AL, Maly RC. Breast cancer treatment decision making among Latinas and non-Latina whites: A communication model predicting decisional outcomes and quality of life. Health Psychol. 2012;31(5):552–561. doi: 10.1037/a0028629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hoffman RM, Hunt WC, Gilliland FD, Stephenson RA, Potosky AL. Patient satisfaction with treatment decisions for clinically localized prostate carcinoma. Results from the Prostate Cancer Outcomes Study. Cancer. 2003;97(7):1653–1662. doi: 10.1002/cncr.11233. [DOI] [PubMed] [Google Scholar]
- 14.Hawley ST, Janz NK, Hamilton A, et al. Latina patient perspectives about informed treatment decision making for breast cancer. Patient Educ Couns. 2008;73(2):363–370. doi: 10.1016/j.pec.2008.07.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jean-Pierre P, Fiscella K, Freund KM, et al. Structural and reliability analysis of a patient satisfaction with cancer-related care measure. Cancer. 2011;117(4):854–861. doi: 10.1002/cncr.25501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jean-Pierre P, Fiscella K, Winters PC, et al. Psychometric validation and reliability analysis of a Spanish version of the patient satisfaction with cancer-related care measure: A patient navigation research program study. Support Care Cancer. 2012;20(9):1949–1956. doi: 10.1007/s00520-011-1297-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alegría M, Sribney W, Perez D, Laderman M, Keefe K. The role of patient activation on patient–provider communication and quality of care for US and foreign born Latino patients. J Gen Intern Med. 2009;24(3):534–541. doi: 10.1007/s11606-009-1074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stanton AL, Luecken LJ, MacKinnon DP, Thompson EH. Mechanisms in psychosocial interventions for adults living with cancer: Opportunity for integration of theory, research, and practice. J Consult Clin Psychol. 2013;81(2):318–335. doi: 10.1037/a0028833. [DOI] [PubMed] [Google Scholar]
- 19.Chesney MA, Chambers DB, Taylor JM, Johnson LM, Folkman S. Coping effectiveness training for men living with HIV: Results from a randomized clinical trial testing a group-based intervention. Psychosom Med. 2003;65(6):1038–1046. doi: 10.1097/01.psy.0000097344.78697.ed. [DOI] [PubMed] [Google Scholar]
- 20.Chesney MA, Neilands TB, Chambers DB, Taylor JM, Folkman S. A validity and reliability study of the coping self-efficacy scale. Br J Health Psychol. 2006;11(3):421–437. doi: 10.1348/135910705X53155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keefe FJ, Blumenthal J, Baucom D, et al. Effects of spouse-assisted coping skills training and exercise training in patients with osteoarthritic knee pain: A randomized controlled study. Pain. 2004;110(3):539–549. doi: 10.1016/j.pain.2004.03.022. [DOI] [PubMed] [Google Scholar]
- 22.Lorig K, Stewart A, Ritter P, Gonzalez V, Laurent D, Lynch J. Outcome Measures for Health Education and Other Health Care Interventions. Thousand Oaks, CA: SAGE Publications; 1996. [Google Scholar]
- 23.Lorig K, Ritter PL, González VM. Hispanic chronic disease self-management: A randomized community-based outcome trial. Nurs Res. 2003;52(6):361–369. doi: 10.1097/00006199-200311000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Cella D, Hernandez L, Bonomi AE, et al. Spanish language translation and initial validation of the Functional Assessment of Cancer Therapy Quality-of-Life Instrument. Med Care. 1998;36(9):1407–1418. doi: 10.1097/00005650-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Cella D, Tulsky D, Gray G, et al. The Functional Assessment of Cancer Therapy scale: Development and validation of the general measure. J Clin Oncol. 1993;11(3):570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 26.Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a Short Acculturation Scale for Hispanics. Hisp J Behav Sci. 1987;9(2):183–205. [Google Scholar]
- 27.Ullman JB. Structural equation modeling: Reviewing the basics and moving forward. J Pers Assess. 2006;87(1):35–50. doi: 10.1207/s15327752jpa8701_03. [DOI] [PubMed] [Google Scholar]
- 28.Kline RB. Principles and Practice of Structural Equation Modeling. 3. New York, NY: Guilford Publications; 2011. [Google Scholar]
- 29.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6(1):1–55. [Google Scholar]
- 30.Cleary EH, Stanton AL. Mediators of an Internet-based psychosocial intervention for women with breast cancer. Health Psychol. 2015;34(5):477–485. doi: 10.1037/hea0000170. [DOI] [PubMed] [Google Scholar]
- 31.Ashing KT, Chávez NR, George M. A health equity care model for improving communication and patient-centered care: A focus on oncology care and diversity. In: Kissane DW, Bultz BD, Butow PN, Bylund CL, Noble S, Wilkinson S, editors. Oxford Textbook of Communication in Oncology and Palliative Care. 2. Oxford: Oxford University Press; 2017. pp. 257–264. [Google Scholar]