Abstract
Objective
To assess associations between enactment of state medical marijuana laws (MMLs), MML restrictiveness, and past-30-day youth alcohol use overall, and in relation to marijuana use.
Method
This quasi-experimental difference-in-difference designed study used state-level Youth Risk Behavior Survey data of 9th–12th grade students in 45 states from 1991–2011 (N = 715,014). We conducted bivariate (unadjusted) and multivariable (adjusted for state, year, individual characteristics) logistic regression analyses to examine the effect of MML enactment (yes/no) and less restrictive vs. more restrictive MMLs on five varying measures of past 30-day alcohol use (i.e., any use or binge) and alcohol and marijuana use behaviors.
Results
In the final adjusted analyses, MML enactment was associated with lower odds of adolescent past 30-day (1) alcohol use (OR = 0.92, [0.87, 0.97], p < .01) and (2) use of both alcohol and marijuana (OR = 0.93, [0.87, 0.99], p < .05). States with less restrictive MMLs had lower odds of past 30-day (1) alcohol use (OR = 0.94, [0.92, 0.97], p < .001), (2) binge drinking (OR = 0.96, [0.93, 0.97], p < .05), (3) alcohol use without any marijuana use (OR = 0.96, [0.93, 0.99], p < .01), and (4) use of both alcohol and marijuana (OR = 0.96, [0.92, 0.99], p < .05).
Conclusions
This study found that enactment of any MML, and of less restrictive MMLs, was associated with lower odds of past 30-day adolescent alcohol use among adolescents. With continued change in state marijuana laws, it is important to monitor the effect of their enactment and implementation, as well as their specific provisions (e.g. dispensaries, home cultivation), which may differentially affect adolescent behaviors.
Keywords: Youth, marijuana use, alcohol use, medical marijuana laws, marijuana and alcohol co-use, substance use
Introduction
Adolescents in the United States have high levels of alcohol and marijuana use,1 which puts them at risk for a host of adverse outcomes in the short and long term.2–5 The past-30-day prevalence estimates for alcohol and marijuana use among US high school students are 32.8% and 21.7%, respectively.6 The reported lifetime use for both has declined since 1999, with steeper declines observed for alcohol use. These findings are particularly noteworthy given that the past 20 years have been marked by rapid changes in state-level marijuana policies. Because liberalized restrictions on marijuana could lead to increases in substance use and related problems among adolescents (e.g., increased alcohol use), ongoing public health monitoring is critically important. Therefore, we examine the association between medical marijuana laws (MMLs) and changes in past-30-day use of alcohol and marijuana.
Medical marijuana laws and adolescent marijuana and alcohol use
Since 1996, 29 states and the District of Columbia have enacted medical marijuana laws (MMLs), the most liberal category of marijuana reform previous to recreational marijuana laws (RMLs), which effectively allows patients to consume marijuana for varying medicinal purposes.7 Although MMLs tend to restrict access and use to those younger than 21, it had been hypothesized that they would lead to an increase in marijuana use among adolescents.8,9 To date, there is little support for this hypothesis.10,12–21 Thirteen national studies have examined the association between MMLs and changes in adolescent marijuana use.10–22 Although two of those found higher rates of adolescent marijuana use in MML compared with non-MML states,19,23 subsequent analyses with the same data demonstrated that there was no association.11,22 The remaining studies similarly found little support for increased marijuana use following MML enactment,10,12–21 although one study found an increase in marijuana use initiation in MML states among 12-to 20-year-olds.18
MMLs may also impact adolescent alcohol use, partially because youth engage in high levels of concurrent alcohol and marijuana use.24,25 Unfortunately, there is limited research on how MML studies are associated with changes in alcohol use. It is particularly important to examine whether MMLs are associated with decreases in alcohol use and increases in marijuana use, i.e., “the substitution hypothesis,” or with increases in both use, i.e., “the complement hypothesis.”26 In a recently published systematic review of studies that examined changes in alcohol use in relation to marijuana policies, Guttmannova et al. found evidence for both hypotheses.26 However, many of the studies included in that review were conducted with data from the 1990s and are now dated.
Current literature shows that MMLs have not increased adolescent marijuana use, but it is unclear whether MMLs increase adolescent alcohol use. Therefore, we examine past-30-day alcohol use in addition to marijuana use behaviors. Given the high levels of alcohol and marijuana co-use, we examined a broad set of substance use outcomes: any alcohol use, binge drinking, alcohol use without any marijuana use, marijuana use without any alcohol use, and both alcohol and marijuana use. This study was unable to assess alcohol and marijuana “co-use,” i.e., whether adolescents reported alcohol and marijuana use on the same occasion.
Restrictiveness and heterogeneity in MMLs
Although provisions of MMLs vary widely across states (e.g., rules about dispensaries, home cultivation, user registration etc.), MMLs have been historically specified as a binary variable in policy evaluation studies. This strategy does not account for heterogeneity and precludes examination of how specific provisions relate to changes in substance use. More recently, studies have started to address heterogeneity by examining specific MML provisions separately. Findings suggest that different MML provisions have differential effects on substance use outcomes, highlighting the importance of incorporating measures of heterogeneity in research examining the impact of MMLs.15,18,27–31 Additionally, a recent study developed an MML restrictiveness taxonomy by categorizing MML provisions and scoring MML states along 3 key dimensions: (1) Initiation (i.e., level of difficulty to become an approved medical marijuana user), (2) Quantity (i.e., quantity of marijuana product allowed for each user), and (3) Distribution (i.e., tightness of state regulation/monitoring of the medical marijuana supply and distribution system). The sum of these domain scores produced an “Overall Restrictiveness” score29 (possible range: 3 [most restrictive] to 15 [least restrictive]), which was found to vary widely across the MML states (range: 4–14). Validity of this taxonomy was supported by analysis results showing significant associations between these scores and adjusted rates of past-year marijuana use among adult residents in state-level analysis.29 The authors did not examine these scores in relation to adolescent outcomes, however.
Current study
This study builds on prior literature by examining the relationship between MMLs and rates of adolescent past-30-day use of alcohol and marijuana using data collected from 45 states between 1991 and 2011, during which time 12 states enacted MMLs and no states had RMLs. To explore the relationship between alcohol and marijuana use, we examine alcohol use in relation to marijuana use (i.e., alcohol only, use of both alcohol and marijuana, marijuana only, etc.). A unique feature of this study is our analysis of not only the effect of having any MML on these outcomes, but also the effect of state MML restrictiveness, using policy taxonomy scores.29
Methods
This study used a quasi-experimental difference-in-difference design to assess changes in rates of adolescent past-30-day alcohol and marijuana use behaviors using a series of repeated cross-sectional Youth Risk Behavior Surveillance (YRBS) System data from 45 states merged with state-level MML data, 1991–2011.
Data source: State-level youth risk behavior surveys (1991–2011)
Individual-level data (N = 735,352) from 45 US states were derived from the school-based state-level Youth Risk Behavior Surveillance (YRBS) surveys collected biennially between 1991 and 2011. The YRBS is a cross-sectional survey monitoring health-risk behaviors that contribute to the leading causes of morbidity and mortality among youth. The YRBS survey and methodology has been described in detail at: http://www.cdc.gov/healthyyouth/data/yrbs/index.htm. Briefly, the state-level YRBS data are collected by various state education and health agencies and can vary year to year in the number of participating states, and years of available weighted data for participating states. Each state and year YRBS sample used a 2-stage, cluster sample design to produce a representative sample of students in grades 9 to 12 in its jurisdiction for each year. The primary sampling units are all public schools within the state, except a few states that additionally included private schools. This sample consisted of 10 cross-sectional adolescent cohort panels, each representing the year of data collection, 1991–2011 (see Table 1 for pre-post years of YRBS data collection for MML states). Surveys from states with a scientifically selected sample, appropriate documentation, and at least a 60% response rate were weighted to adjust for student nonresponse, grade, sex, and race/ethnicity and included in these analyses.
Table 1.
Youth Risk Behavior Surveillance (YRBS) data for states that enacted medical marijuana laws (MMLs), pre/post–MML enactment YRBS weighted data availability, and MML “restrictiveness” taxonomy scores.
| State* | Year MML Enacted | Years of data pre-MML | Years of data post-MML | Initiationa | Quantityb | Distributionc | “Least Restrictive” scored |
|---|---|---|---|---|---|---|---|
| Alaska | 1998 | 1 | 4 | 1 | 3 | 5 | 9− |
| Arizona | 2010 | 4 | 1 | 3 | 3 | 3 | 8− |
| Colorado | 2000 | 0 | 3 | 4 | 3 | 3 | 10+ |
| Delaware | 2011 | 5 | 1 | 3 | 2 | 1 | 6− |
| Maine | 1999 | 2 | 6 | 5 | 3 | 4 | 12+ |
| Michigan | 2008 | 6 | 2 | 4 | 3 | 5 | 12+ |
| Montana | 2004 | 6 | 4 | 4 | 4 | 5 | 13+ |
| Nevada | 2000 | 4 | 5 | 3 | 2 | 3 | 8− |
| New Jersey | 2010 | 3 | 1 | 2 | 1 | 1 | 4− |
| New Mexico | 2007 | 2 | 3 | 4 | 4 | 2 | 10+ |
| Rhode Island | 2006 | 4 | 3 | 4 | 4 | 3 | 11+ |
| Vermont | 2004 | 0 | 1 | 3 | 2 | 2 | 7− |
States that enacted MMLs between 1991 and 2011 (study years).
a,b,c,dTaxonomy scores developed by Chapman et al.29
Initiation: Range: 1–5 (“1” indicating that it was difficult to become an approved medical marijuana user, and “5” indicated that it was relatively easy to initiate use).
Quantity: Range: 1–5 (“1” defined as not permitting a large quantity of product for each user, and “5” indicating that a relatively large quantity was permitted).
Distribution: Range: 1–5 (“1” indicated that distribution was tightly controlled, and “5” indicated little state control for distribution).
“Least Restrictive” MML score adapted from Chapman et al.29 study: Range: 4–13: A sum of the scores 1–3, with higher scores indicating less restrictive MMLs in regards to ability of (1) initiating medical marijuana use, the (2) quantity of medical marijuana product per marijuana user, and state system ability to control the (3) distribution of medical marijuana. For analyses in this study and interpretability, these scores were renamed “Least Restrictiveness” score (vs. the “Overall Restrictiveness” used in Chap-man et al.29 study) to distinguish “more restrictive” versus “less restrictive” MML states (“Least Restrictive” MML score range: 4–13 (coded “1” or “more restrictive” [scores 4–9−]; coded “2” or “less restrictive” [scores 10–14+]).
Twelve states in this 45-state sample enacted MMLs within study years, 1991–2011, excluding 4 early adopter MML states: California, Washington, Oregon, and Hawaii. State MML year of enactment information was derived from national government and proponent databases.7,32,33
This study was approved by the Brandeis University Institutional Review Board in September 2013. We obtained the data securely from the Centers for Disease Control and Prevention (CDC) and varying state YRBS coordinators. The CDC had pre-authorized permission to distribute 1991–2011 data from 30 states upon request. Eleven states gave the CDC permission to distribute data after an individual direct request or application was made to the state coordinators. Four states granted permission after a formal data use agreement was signed, and 1 state after an informal data use agreement was agreed upon. Although all data used in analyses were de-identified, and thus exempt, the YRBS did receive parental consent for student participation. Prior to a school’s participation in the YRBS, local procedures for obtaining parental permission included either (1) active permission (i.e., parents must send a signed form permitting student participation) or (2) passive permission (parents only send back signed form if student not permitted to participate).34
Measures
Dependent variables: Substance use outcomes
The following 5 dichotomous outcome variables were constructed from YRBS variables consistently worded across all states and years: report of any past-30-day (1) alcohol use (“at least 1 drink of alcohol”), (2) binge drinking (5 or more drinks in a row), (3) alcohol use without any past-30-day marijuana use, (4) marijuana use without any past-30-day alcohol use, and (5) both alcohol and marijuana use (reported use of both alcohol and marijuana use in the past 30 days).
Independent variables: MML and restrictiveness
The main independent variable, “any MML,” indicated whether an observation is from a state which had enacted an MML in any prior year (Table 1). Twelve states with available YRBS data enacted MMLs between 1991 and 2011 (total N for these states = 102,124). Since states varied in the years of MML enactment and years of YRBS participation, there was variation in available pre-post data for states (Table 1). A second MML variable (“restrictiveness”) was constructed to differentiate less restrictive versus more restrictive MMLs based on the taxonomy scores developed by Chapman and colleagues.29 In the Chapman et al. study, the domains of Initiation, Quantity, and Distribution were scored 1 to 5, with “1” being the most restrictive and “5” the least restrictive. The sum of these domain scores, called the “Overall Restrictiveness,” ranged from 4 to 13 across the states (Table 1), with higher scores indicating less restrictive MMLs. To reduce confusion, we have renamed this overall restrictiveness sum score to the “Least Restrictiveness” score to indicate that a higher score means less restrictiveness. To enhance ease of interpretation of analyses results, we further collapsed this overall score into an ordinal variable, coded: “0” for no MML, “1” for more restrictive MML states (scores 4–9), and “2” for less restrictive MML states (scores 10–14). In addition to the overall restrictiveness score, we ran all models with each individual domain of the taxonomy scoring (Initiation, Quantity, and Distribution; data not shown); however, there was not enough difference between the individual taxonomy scores and the overall restrictiveness scores to qualify for the need to further separate out in Table 2.
Table 2.
Past-30-day adolescent alcohol and covarying marijuana use behaviors by state medical marijuana law (MML) enactment status and restrictiveness, 1991–2011 (N = 715,014).
| Any MMLa/MML restrictiveness taxonomy scoreb | Adjusted ORc (95% CI) |
|---|---|
| Any MML; 12 states (n = 102,124) “Least Restrictiveness” scoreb | Past-30-day alcohol use 0.92** (0.87–0.97) 0.94*** (0.92–0.97) |
| Any MML; 12 states (n = 102,124) “Least Restrictiveness” scoreb | Past-30-dayb binge drinking 0.95 (0.89–1.00) 0.96* (0.934–0.997) |
| Any MML; 12 states (n = 102,124) “Least Restrictiveness” scoreb | Past-30-day alcohol use without any marijuana use 0.96 (0.91–1.02) 0.96** (0.93–0.99) |
| Any MML; 12 states (n = 102,124) “Least Restrictiveness” scoreb | Past-30-day marijuana use without any alcohol use 0.99 (0.86–1.14) 0.99 (0.92–1.07) |
| Any MML; 12 states (n = 102,124) “Least Restrictiveness” scoreb | Past-30-day alcohol and marijuana use 0.93* (0.87–0 .99) 0.96* (0.92–0.99) |
Note. Each row shows the unadjusted (bivariate) and adjusted model results for each independent variable with the dependent variables in the columns. Stata 13 MP “svyset” survey data settings were used to assign YRBS design variables: (sampling units: “psu” and strata “stratum”) as provided by all state YRBS data sets to account for their sampling procedures.
Each cell shows the result of a separate logistic regression analysis. Control group: States that either did not enact MMLs during any of the survey years or did not enact an MML in the varying survey years before they eventually enacted MMLs. Estimates are weighted using YRBS weights.
Any MML: State had enacted medical marijuana in year of data collection (yes/no)
“Least Restrictive” MML score adapted from Chapman et al.29 study: Range: 4–13, with higher scores indicating less restrictive MMLs in regards to ability of (1) initiating medical marijuana use, the (2) quantity of medical marijuana product per marijuana user, and state system ability to control the (3) distribution of medical marijuana. For analyses in this study and interpretability, these scores were renamed “Least Restrictiveness” score” (vs. the “Overall Restrictiveness” used in Chapman et al.29 study) to distinguish “more restrictive” vs. “less restrictive” MML states (“Least Restrictive” MML score range: 4–13 (coded “1” or “more restrictive” [scores 4–9−]; coded “2” or “less restrictive” [scores 10–14+]). 0 = no MML; 1 = “more restrictive”; 2 = “less restrictive.
Adjusted odds ratios (multivariable models), adjusted for year fixed effects, state fixed effects, and individual demographics: age, sex, white, black, Hispanic, and other.
Binge drinking: report of drinking ≥5 alcoholic beverages on 1 occasion in the past 30 days.
P ≤ .05;
P ≤ .01;
P ≤.001.
Data analysis
Fixed-effects logistic regression modeling was used to assess the associations between state-level variables and adolescent reports of past-30-day alcohol and marijuana use from 1991 to 2011. All final adjusted multivariable logistic regression models adjusted for (1) state (45 dichotomous variables indicating individual states; n = 45), (2) year of data collection (11 dichotomous variables indicating each biennial year of data collection; range: 1991–2011), (3) age (ordinal variable indicating age; range: 12–18), (4) sex (male vs. female), and race/ethnicity (black non-Hispanic, white non-Hispanic, Hispanic, and other).
Results
Prevalence estimates
Figures 1 and 2 graphically display unadjusted prevalence estimates of the rates of all 5 adolescent substance use outcome variables across years (N = 735,352). Figure 1 shows the rates for the overall sample across the entire study period (1991–2011), and Figure 2 shows the rates of these same variables separately for MML states and non-MML states from 2001, the first year of data collection subsequent to the first 2 states in sample enacting MMLs, which enabled an “MML” comparison group, to 2011, the last year of data collection, by which time 12 of the 45 states had enacted MMLs.
Figure 1.
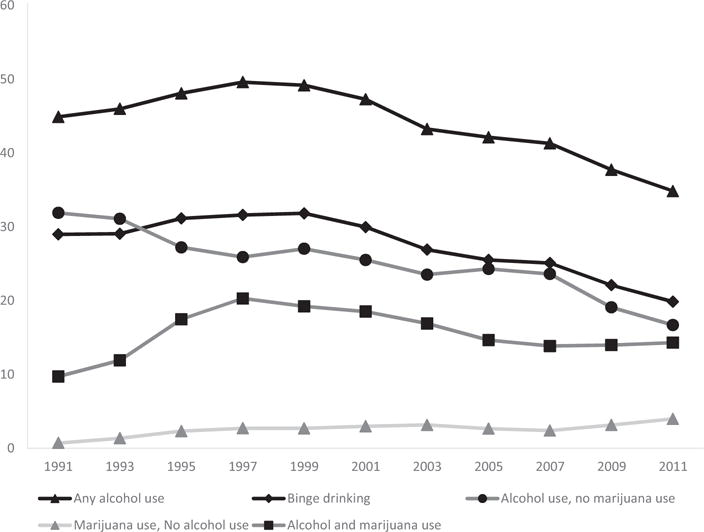
Unadjusted prevalence estimates (means) of adolescent past-30-day alcohol and marijuana use behaviors, all 45 states from 1991 to 2011 (N = 715,014).
Figure 2.
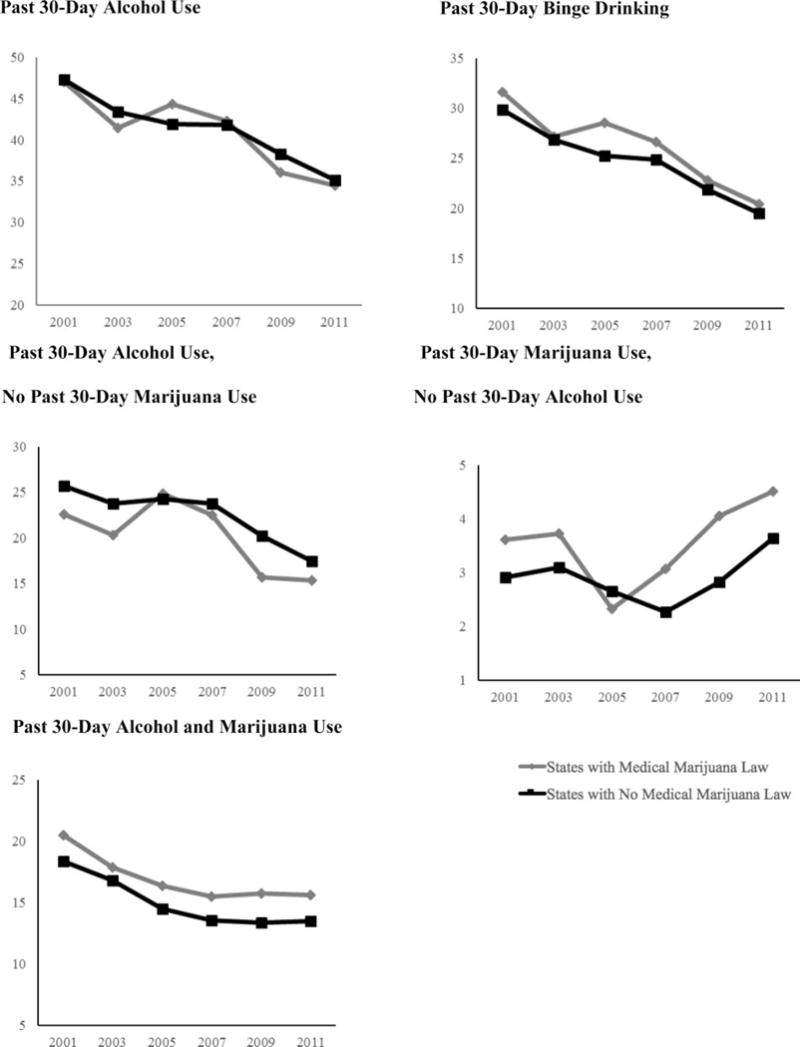
Unadjusted prevalence estimates (means) of adolescent past-30-day alcohol and marijuana use behaviors in medical marijuana law (MML) states and non-MML states, 45 states from 2001 to 2011.
Logistic regression analyses
Table 2 displays the adjusted logistic regression models assessing associations between adolescent alcohol and marijuana use behaviors and whether a state enacted any MML and MML restrictiveness. In the analyses, living in an MML state predicted significantly lower odds of past-30-day adolescent (1) alcohol use and (2) both alcohol and marijuana use. Less MML restrictiveness was associated with significantly lower odds of adolescents reporting past-30-day (1) alcohol use, (2) binge drinking, and (3) alcohol use without any past-30-day marijuana use. Past-30-day marijuana use without any past-30-day alcohol use was the only dependent variable that did not show any significant effect.
Discussion
To examine whether MMLs affect varying past-30-day adolescent alcohol and marijuana use behaviors, this study examined data for 45 states between 1991 and 2011, including 12 of the 16 states that enacted MMLs on or previous to 2011, representing the most liberalized categorization of marijuana laws prior to the wave of recreational marijuana legalization laws that began in 2012, and found that states that enacted a MML, and having a less restrictive policy, were associated with lowered odds of adolescent past-30-day alcohol use. Although MML states had higher odds of adolescents reporting past-30-day marijuana use without alcohol use in unadjusted bivariate analysis (data not shown), this effect dissipated after adjustment for state, year, and individual demographics (final adjusted model, Table 2). This finding is consistent with the bulk of prior research based on large national data sets, which found no increase in adolescent past-30-day marijuana use rates pre- to post-MML enactment after adjusting for state effects. It is important to note that the last year of data collection was 2011, and since this time 9 states in this data set enacted MMLs (Arkansas, Connecticut, Florida, Illinois, Maryland, Massachusetts, New Hampshire, New York, West Virginia) and another 6 states additionally enacted RMLs (Alaska, Colorado, Florida, Maine, Massachusetts, and Nevada). It is possible that these results do not represent more recent adolescent alcohol and marijuana use rates in states with MMLs given these more recent changes.
A distinguishing feature of this study is its analysis of state MMLs along a gradient of restrictiveness using a validated taxonomy scoring system recently published by Chapman and colleagues.29 We found that less MML restrictiveness was associated with lower odds of adolescent past-30-day alcohol use, binge drinking, alcohol use without any marijuana use, and use of both alcohol and marijuana. Few prior studies have accounted for the variability in MML design (i.e., the provisions included or level of restrictiveness). The current literature assessing adolescent marijuana and/or alcohol use adjusting for the heterogeneity of MML design is mixed, which may be a result of limitations in available data’s ability to isolate effects of MMLs and their provisions, as well as the newness and evolving nature of these laws.
This study’s finding that MML enactment was associated with significantly lower odds of adolescent alcohol use differs from one previous analysis by Pacula and colleagues using an aggregated YRBS sample from 1993 to 2009, which found no overall association between MML enactment and adolescent alcohol use.15 However, that study found significant negative associations when examining specific MML provisions (i.e., allowing dispensaries and home cultivation were associated with lower odds of alcohol use), which is more comparable to our results based on analysis of MML “Least Restrictiveness” taxonomy scores.
Other studies examining MMLs and alcohol use trends have used a variety of other national data sets and have shown mixed findings. A study analyzing the Treatment Episode Data from 1992 to 2008 found no association between MML enactment and alcohol use treatment admissions but did find that states allowing MML dispensaries had higher rates of alcohol treatment admissions in the <21 age cohort.15 Our study examined any alcohol use and any binge drinking in the past 30 days, not severity of involvement, such as that which might warrant treatment. It is possible that the effects of MMLs, and different MML provisions, may vary by level of substance use involvement, with a potentially stronger effect on those already substantially involved in substance use. Another analysis using National Longitudinal Survey of Youth 1997–2008 found no association among individuals <21 years old between MML and alcohol use, a positive association between alcohol use and home cultivation, and a negative association between alcohol use and MML patient registration.15 Another analysis using a restricted access data set from the National Survey on Drug Use and Health from 2004 to 2012 found no evidence of an effect of an MML or any MML provisions on any measure of alcohol use among 12- to 20-year-olds. However, this study reported higher likelihood of past-month marijuana use and binge drinking and simultaneous use of marijuana and alcohol for people aged 21 and older.18 It is possible that any effects on adolescent alcohol use associated with MMLs lag behind changes in adults ≥21, who can use alcohol legally.
Lastly, this study sought to assess if there were any “complementary” or “substitutive” effects between alcohol and marijuana, specifically if MMLs were associated with higher marijuana use odds and lower alcohol use odds. Interestingly, this study did not find evidence of either. In this sample, MMLs were associated with lower odds of past-30-day (1) alcohol use and (2) alcohol and marijuana use (any reported use of both substances in past 30 days), and no effect on past-30-day marijuana use without any alcohol use. The alcohol finding is not as surprising given that Monitoring in the Future, a national surveillance of youth substance use, reports steadily annual declining alcohol use rates among youth from 1991 when 39.8% of youth reported past-30-day alcohol use to 2011 when only 25.5% of youth reported use (cohort includes average of grades 8, 10, and 12). By contrast, prevalence of marijuana use has remained steady from 1994 (13.9%) to 2014 (15.2%), despite a changing marijuana reform landscape.35 This could be a result of preventative methods targeting youth simultaneously enacted in states enacting MMLs, states’ control of the quantity of marijuana and youth access to marijuana in the state, and lagged time from policy enactment to implementation of policy provisions (e.g., dispensary, commercialization, etc.) that theoretically may decrease fiscal and social costs and thus increase youth access and marijuana use.
Strengths and limitations
This study included 45 states spanning the years 1991–2011 and therefore captured more states and years of data collection in the analyses than most previous studies assessing MMLs and adolescent alcohol or marijuana use. It also moves the field forward by accounting for MML heterogeneity (“Least Restrictiveness”) in the analysis of MML effects, and it examined adolescent alcohol use in relation to marijuana use. The study had a number of limitations. This study relied on state YRBS data, which are cross-sectional; thus, results are unable to establish cause-effect relationships. It is possible that changes in the composition of the study population over time could have contributed to differences in use over time. Analyses address this potential confounding by weighting procedures to address non-response bias, and multivariable models further adjusted for individual demographic characteristics, state, and year effects. Our substance use data relied on the particular wording of the YRBS survey questions, and on self-report, which may be subject to recall error and social desirability bias. YRBS survey question design prevented analyses from discerning more precise estimates on alcohol and marijuana co-use, since these data don’t distinguish whether adolescents used marijuana and alcohol on the same occasion, only whether they used each substance used in the past 30 days. Additionally, the YRBS sample was limited to adolescents attending high school, mostly public schools, and may not be generalizable to the entire state adolescent populations. State YRBS samples varied across participating states and years of participation. This study excluded California, Oregon, Washington, and Hawaii and only had post-enactment data for Colorado and Vermont. This is an important limitation, since all the above states with the exception of Vermont passed MMLs on or before 2000 and are generally considered “early adopter states,” thus limiting our ability to discern full effects of all early MMLs. Maine, Nevada, and Alaska are the 3 remaining states that enacted MMLs on or before 2000 that are included in our sample. Eleven states used as control states in this study were on the brink of enacting similar MMLs, with (1) Connecticut and Massachusetts in 2012; (2) Illinois and New Hampshire in 2013; (3) New York and Maryland in 2014; and (4) Maryland, Pennsylvania, Ohio, North Dakota, Arkansas, and Florida in 2016. It is possible that these control states’ substance use and social norms were more like the intervention states, resulting in their eventually enacting MMLs. Current literature suggests that states that enacted MMLs had higher rates of marijuana use before MML enactment.17 The MML variables were constructed based on MML enactment in order to have enough pre-post MML state/years for comparison, rather than on implementation. Full policy implementation takes time, and this study may not have included a sufficient number of years to capture implementation effects in all MML states. Analyses did not adjust for any alcohol diversion policies, which may have moderated MML effects on alcohol use.
Future research
Medical marijuana laws were the most liberalized marijuana laws until 2012, when 2 of the current 8 states and Washington, DC, enacted varying laws permitting adults to use small quantities of marijuana for recreational use. Further assessment of the effects of all state marijuana laws on adolescent marijuana and alcohol use are important as more states move to legalize marijuana for medicinal or recreational use. It is important for future research to assess alcohol and marijuana co-use behaviors on the same occasion of use versus use of both substances within the past month. Preventing and/or reducing the potential harms of marijuana liberalization laws on adolescents should take a multifaceted approach, including the public health and policy sectors. A more comprehensive understanding of how varying marijuana laws and provisions influence adolescent substance use behavior can contribute to more efficacious alcohol and marijuana prevention and intervention policies in the future.
Studies are needed that analyze more recent years of YRBS data (2013 to present), as there may be lagged effects of previously enacted MMLs, and additional states have passed MMLs since 2011. It is important to additionally assess the 4 states that this study was unable to include, using other weighted state-level data, such as Monitoring the Future survey data.17 Future studies should also examine whether marijuana laws effects are moderated by adolescent age group, sex, and race, as well as examine other risk behaviors associated with adolescent alcohol and marijuana use, such as driving after using, unprotected sexual activity, tobacco use, and use of other drugs.27
Conclusion
Past-30-day adolescent alcohol and marijuana use behaviors are still concerningly high. However, using repeated cross-sectional YRBS data collected from 45 states between 1991 and 2011, this study found little evidence of increases in adolescent past-30-day alcohol use behaviors attributable to MML enactment or to less restrictive MMLs. Instead, this study suggests that policies that liberalize marijuana access are associated with lower rates of adolescent alcohol use; more studies are needed to confirm and elucidate this finding. Given the rapidly evolving marijuana law landscape, evaluating the impact of marijuana law enactment/implementation on adolescent behaviors is an important research priority moving forward and is necessary for informing public health and policy efforts to prevent the possible adverse consequences of marijuana legalization.
Acknowledgments
The authors would like to thank the Centers for Disease Control and Prevention for use of the Youth Risk Behavior Surveillance System data and the many state health and education departments for their assistance in providing access to their state’s data. The lead author would like to acknowledge Peter Kreiner, PhD, Rosalie Pacula, PhD, John Knight, MD, Constance Horgan, ScD, and Sharon Reif, PhD, for their mentorship at different phases of this study.
Funding
This research was primarily supported by the National Institute on Drug Abuse (NIDA) grants 5F31DA036923-02 (Principal Investigator [PI]: Julie K. Johnson) and 4T32DA007292-24 (Julie K. Johnson, Abenaa A. Jones, PI: Renee M. Johnson). The primary funder, NIDA, was involved in the review and approval of study design and conduct, but not involved in data collection, management, analysis, data interpretation, or manuscript preparation. Secondary support was provided by NIDA grant K01DA031738-06 (PI: Renee M. Johnson); National Institute on Alcohol Abuse and Alcoholism (NIAAA) grants T32AA00567 (Julie K. Johnson, Ann Marie Matteucci, PI: Constance Horgan), 1R01AA021904 (Sion K. Harris, PI: John R. Knight), 1R34AA023026 (Sion K. Harris, PI: John R. Knight), 1R01AA02243 (Sion K. Harris, PI: John R. Knight); and the Leadership Education in Adolescent Health Training Program Health Resources and Service Administration Maternal and Child Health (MCH/HRSA) grant T71 MC00009 (Sion K. Harris). The secondary funders were not involved in involved in data collection, management, analysis, data interpretation, or manuscript preparation. This article is the sole responsibility of the authors and does not reflect the view of NIDA, NIAAA, or MCH/HRSA.
Footnotes
Author contributions
Julie Johnson is responsible for the study conception, design, analysis, and manuscript writing. Julie Johnson had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors assisted with writing and interpretation of findings. Sion Harris, Dominic Hodgkin, and Ann Marie Matteucci also assisted with study conception, design, and analysis.
References
- 1.Hedden SL, Kennet J, Lipari R, Medley G, Tice P. Results from the 2014 National Survey on Drug Use and Health. Rockville, MD: Substance Abuse and Mental Health Services Administration [SA and MHSA]; 2014. [Google Scholar]
- 2.Johnston LD, O’Malley MP, Miech RA, Bachman JG, Schulenberg JE. 2015 Overview: Key Findings on Adolescent Drug Use. Ann Arbor, MI: The University of Michigan Institute for Social Research; 2015. http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2015.pdf. Accessed xxx. [Google Scholar]
- 3.Harding FM, Hingson RW, Klitzner M, et al. Underage drinking: a review of trends and prevention strategies. Am J Prev Med. 2016;51(4 Suppl 2):S148–S157. doi: 10.1016/j.amepre.2016.05.020. [DOI] [PubMed] [Google Scholar]
- 4.Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012;109:E2657–E2664. doi: 10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Castellanos-Ryan N, Pingault J-B, Parent S, Vitaro F, Tremblay RE, Seguin JR. Adolescent cannabis use, change in neurocognitive function, and high-school graduation: a longitudinal study from early adolescence to young adulthood. Dev Psychopathol. 2016 doi: 10.1017/S0954579416001280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance—United States, 2015. Atlanta, GA: Centers for Disease Control and Prevention; 2016. https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2015/ss6506_updated.pdf. [Google Scholar]
- 7.National Conference of State Legislatures. State Medical Marijuana Laws. http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx. Accessed January 4, 2017.
- 8.Joffe A, Yancy WS, American Academy of Pediatrics Committee on Substance Abuse, American Academy of Pediatrics Committee on Adolescence Legalization of marijuana: potential impact on youth. Pediatrics. 2004;113:e632–e638. [PubMed] [Google Scholar]
- 9.Wang GS. Pediatric concerns due to expanded cannabis use: unintended consequences of legalization. J Med Toxicol. 2016 doi: 10.1007/s13181-016-0552-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wall MM, Poh E, Cerd a M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21:714–716. doi: 10.1016/j.annepidem.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harper S, Strumpf EC, Kaufman JS. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann Epidemiol. 2012;22:207–212. doi: 10.1016/j.annepidem.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 12.Anderson MD, Hansen B, Rees DI. Anderson Medical Marijuana Laws and Teen Marijuana Use. Cambridge, MA: NBER; 2014. (NBER Working Papers No. 20332). http://econpapers.repec.org/paper/nbrnberwo/20332.htm. [Google Scholar]
- 13.Anderson DM, Hansen B, Rees DI. Medical marijuana laws and teen marijuana use. Am Law Econ Rev. 2015;17:495–528. doi: 10.1093/aler/ahv002. [DOI] [Google Scholar]
- 14.Lynne-Landsman SD, Livingston MD, Wagenaar CA. Effects of state medical marijuana laws on adolescent marijuana use. Am J Public Health. 2013;103:1500–1506. doi: 10.2105/AJPH.2012.301117. http://ajph.aphapublications.org/doi/abs/10.2105/ajph.2012.301117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the Effects of Medical Marijuana Laws on Marijuana and Alcohol Use: The Devil Is in the Details. Cambridge, MA: NBER; 2013. (NBER Working Papers No. 19302). http://www.nber.org/papers/w19302. [Google Scholar]
- 16.Choo EK, Benz M, Zaller N, Warren O, Rising KL, McConnell KJ. The impact of state medical marijuana legislation on adolescent marijuana use. J Adolesc Health. 2014;55:160–166. doi: 10.1016/j.jadohealth.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 17.Hasin DS, Wall M, Keyes KM, et al. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual. repeated cross-sectional surveys. Lancet Psychiatry. 2015;2:601–608. doi: 10.1016/S2215-0366(15)00217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wen H, Hockenberry JM, Cummings JR. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J Health Econ. 2015;42:64–80. doi: 10.1016/j.jhealeco.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 19.Stolzenberg L, D’Alessio SJ, Dariano D. The effect of medical marijuana laws on juvenile marijuana use. Int J Drug Policy. 2016;27:82–88. doi: 10.1016/j.drugpo.2015.05.018. [DOI] [PubMed] [Google Scholar]
- 20.Shi Y. The availability of medical marijuana dispensary and adolescent marijuana use. Prev Med. 2016;91:1–7. doi: 10.1016/j.ypmed.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 21.Johnson J, Hodgkin D, Kim S. The design of medical marijuana laws and adolescent use and heavy use of marijuana: analysis of 45 states from 1991 to 2011. Drug Alcohol Depend. 2017;170:1–8. doi: 10.1016/j.drugalcdep.2016.10.028. http://www.sciencedirect.com/science/article/pii/S0376871616309796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wall MM, Mauro C, Hasin DS, et al. Prevalence of marijuana use does not differentially increase among youth after states pass medical marijuana laws: commentary on and reanalysis of US National Survey on Drug Use in Households data 2002–2011. Int J Drug Policy. 2016;29:9–13. doi: 10.1016/j.drugpo.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wall MM, Poh E, Cerd a M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann Epidemiol. 2011;21:714–716. doi: 10.1016/j.pestbp.2011.02.012.Investigations. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chun TH, Spirito A, Herñandez L, et al. The significance of marijuana use among alcohol-using adolescent emergency department patients. Acad Emerg Med. 2010;17:63–71. doi: 10.1111/j.1553-2712.2009.00615.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Subbaraman MS, Kerr WC. Simultaneous versus concurrent use of alcohol and cannabis in the National Alcohol Survey. Alcohol Clin Exp Res. 2015;39:872–879. doi: 10.1111/acer.12698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guttmannova K, Lee CM, Kilmer JR, et al. Impacts of changing marijuana policies on alcohol use in the United States. Alcohol Clin Exp Res. 2016;40:33–46. doi: 10.1111/acer.12942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Friese B, Grube JW. Legalization of medical marijuana and marijuana use among youths. Drugs (Abingdon Engl) 2013;20:33–39. doi: 10.3109/09687637.2012.713408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J Policy Anal Manage. 2015;34:7–31. doi: 10.1002/pam.21804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chapman SA, Spetz J, Lin J, Chan K, Schmidt LA. Capturing heterogeneity in medical marijuana policies: a taxonomy of regulatory regimes across the United States. Subst Use Misuse. 2016;51:1174–1184. doi: 10.3109/10826084.2016.1160932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shi Y. The availability of medical marijuana dispensary and adolescent marijuana use. Prev Med. 2016;91:1–7. doi: 10.1016/j.ypmed.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 31.Johnson J, Hodgkin D, Harris SK. The design of medical marijuana laws and adolescent use and heavy use of marijuana: analysis of 45 states from 1991 to 2011. Drug Alcohol Depend. 2017;170:1–8. doi: 10.1016/j.drugalcdep.2016.10.028. http://www.sciencedirect.com/science/article/pii/S0376871616309796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.ProCon.org. 28 Legal medical marijuana states and DC: laws, fees, and possession limits. http://medicalmarijuana.procon.org/view.resource.php?resourceID=000881. Published 2017. Accessed February 22, 2017.
- 33.Marijuana Policy Project. State Policy. https://www.mpp.org/states/. Published 2017. Accessed February 22, 2017.
- 34.Kann K, Kinchen S, Shanklin SL, et al. Youth Risk Behavior Surveillance—United States, 2013. Atlanta, GA: Centers for Disease Control and Prevention; 2014. [PubMed] [Google Scholar]
- 35.Johnston LD, Malley PMO, Miech RA, Bachman JG, Schulenberg JE. 2014 Overview Key Findings on Adolescent Drug Use. Ann Arbor, MI: The University of Michigan Institute for Social Research; 2015. [Google Scholar]


