Abstract
Torsades de pointes with prolonged QTc interval is a form of ventricular tachycardia. Many predisposing factors have been identified and hypocalcemia is among the rare ones. Our case illustrates that though rare, hypocalcemia might manifest as torsades de pointes with prolongation of QTc interval. Early diagnosis and management of dyselectrolytemia can prevent these patients from catastrophic torsades de pointes.
Keywords: Hypocalcemia, QTc interval prolongation, Torsades de pointes
Introduction
Hypocalcemia is a common biochemical abnormality that can range in severity from asymptomatic in mild cases to life threatening crisis [1] in others. It is a very rare cause of torsades de pointes [2]. Carter and Andrus first reported QT prolongation in hypocalcemia in 1922 [3] and there have been very few cases reported since then. Herein we report a case in which patient had multiple runs of polymorphic ventricular tachycardia, which later turned out to be hypocalcemic torsades de pointes.
Case Report
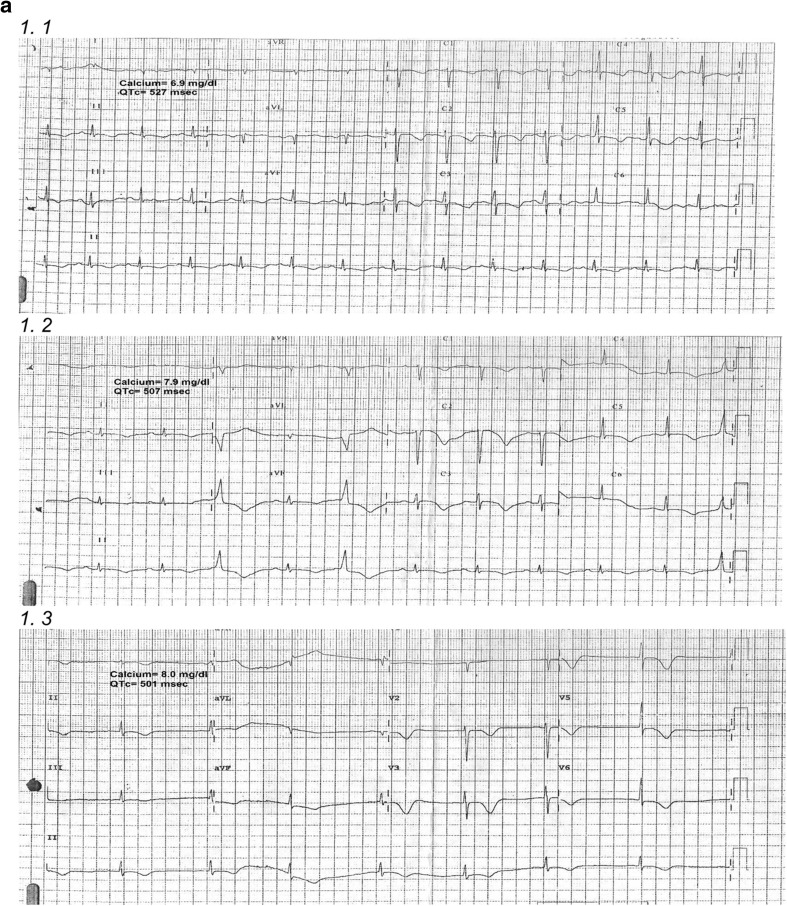
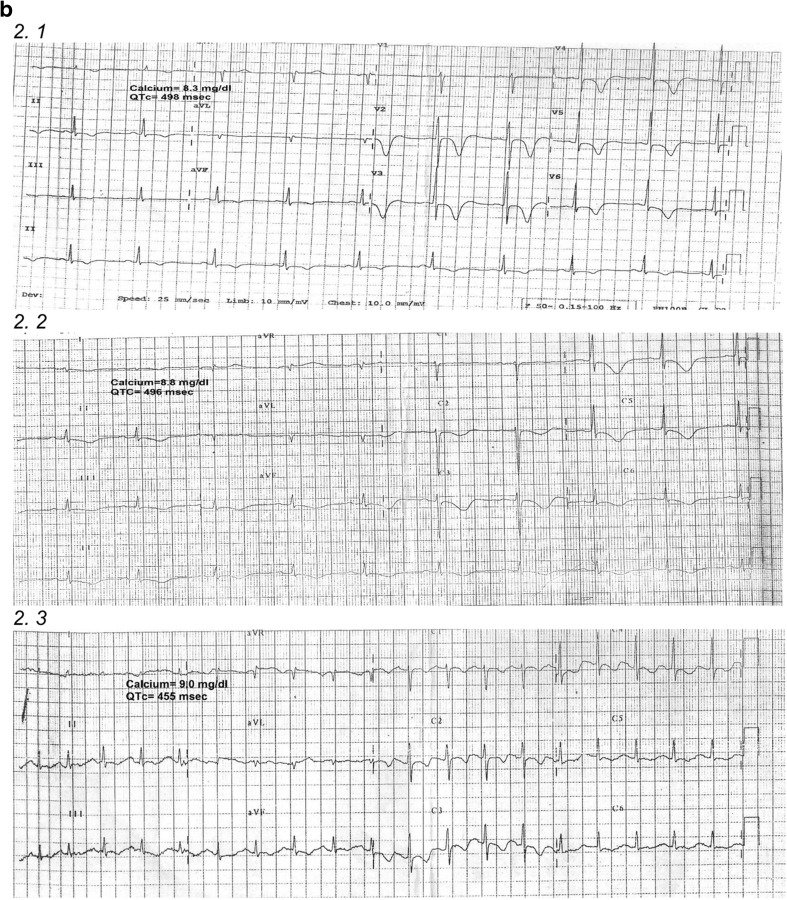
A 53-year-old female was admitted in shock to the emergency department. She had been suffering from fever, loose stools, and breathlessness for 3 days prior to the admission. There was no history of palpitations or syncope. She had a past medical history of hypothyroidism and rheumatoid arthritis for which she was taking some herbal medicine. Her blood pressure was unrecordable. Monitor revealed polymorphic ventricular tachycardia, so immediate DC cardioversion was done. The patient reverted back to sinus rhythm with BP of 100/60 mm of Hg. ECG post cardioversion showed normal sinus rhythm with HR of 82 beats/min, ST segment depression, T wave inversion and prolonged QTc interval (527 ms). Left ventricular ejection fraction, hematological investigations, and assessment of renal functions were normal. Blood sample analysis showed low levels of corrected calcium (6.9 mg/dl), deranged thyroid Function Indices (TSH-4.72 mIU/ml, free T3-1.61 pmol/l and T4-1.85 pmol/l), hypocortisolism (serum cortisol of 2.8 µg/dl which rose to 6.27 μg/dl after ACTH stimulation test) while other electrolytes (Na-140 mmol/dl, K-5 mmol/l, Mg-1.93 mg/dl), Vitamin D-T (33.64 ng/ml) and PTH (47.30 pg/ml) were within the reference range. The patient was given an infusion of 10% calcium gluconate slowly over an hour followed by oral administration of calcium 500 mg thrice daily. There was a progressive reduction in QTc interval with rising serum calcium levels as shown in Table 1. She was prescribed daily dose of levothyroxine 50 mcg to treat hypothyroidism and prednisolone 7.5 mg for hypocortisolism.
Table 1.
Progressive reduction in QTc interval with rising serum calcium levels
| Day | Serum calcium (mg/dl) | QTc interval (ms) |
|---|---|---|
| 1 | 6.9 | 527 |
| 2 | 7.9 | 507 |
| 3 | 8.0 | 501 |
| 4 | 8.3 | 498 |
| 5 | 8.8 | 496 |
| 6 | 9.0 | 455 |
A probable diagnosis of rheumatoid arthritis with hypothyroidism, hypocalcemia, hypocortisolism (secondary to exogenous steroids) and prolonged QTc interval with torsades de pointes (secondary to hypocalcemia) was made.
After recovery, the patient was put on beta-blockers, calcium supplementation, levothyroxine and tapering dose of corticosteroids. There was no recurrence of symptoms in subsequent follow up visits.
Discussion
Polymorphic ventricular tachycardia secondary to prolonged QTc interval can be congenital or acquired. Acquired causes, especially drug induced are far more common than congenital. Other predisposing factors are female gender, hypokalemia, hypomagnesemia, severe heart blocks and rarely hypocalcemia and hypothyroidism.
The exact incidence of torsades de pointes remains speculative, but the condition is thought to be more unrecognized than rare. Some patients appear to have a benign course with one or two episodes in their entire life while others tend to have recurrent symptomatic episodes [4]. The overall mortality rate for patients with prolonged QT syndromes has been estimated to be 1–2% per year [5].
Hypocalcemia is relatively a common metabolic abnormality that presents as paraesthesia, muscle spasms, tetany, seizures, cognitive impairment, prolonged QT intervals, electrocardiographic changes mimicking myocardial infarction, or heart failure.
Hypocalcemia manifesting as Torsades de pointes with prolongation of QTc interval is a rare presentation. It causes prolongation of the plateau phase of the cardiac action potential [6, 7].
Our patient had gastroenteritis and presented with torsades de pointes with prolonged QTc interval. Intake of QTc prolonging drugs, hypokalemia and hypomagnesemia were ruled out. Hypocalcemia was evaluated and, serum PTH and vitamin D were found to be normal. Our patient had been taking some herbal medicine for rheumatoid arthritis and hypothyroidism for a long time. Studies have shown that most of these medicines are contaminated with steroids [8]. They increase renal calcium excretion and decrease gastrointestinal calcium absorption, resulting in reduced serum calcium [9].
The Prolongation of QTc interval was proportional to the degree of hypocalcemia. We have presented a series of electrocardiograms of the patient in Fig. 1a, b, showing a progressive reduction in QTc interval with rising corrected serum calcium levels.
Fig. 1.
12 Lead ECG: 12 lead ECGs displaying gradual decrease in QTc interval with relation to rising serum calcium levels
Torsades de pointes is a catastrophic event that may degenerate to ventricular fibrillation and then to sudden cardiac death. Thorough drug history of the patients should be taken along with a complete evaluation of serum electrolytes including serum potassium, magnesium and corrected calcium levels. Prompt diagnosis and management of dyselectrolytemia can be life-saving for these patients.
Conclusion
QTc interval prolongation is in direct proportion to degree of reduction in corrected serum calcium levels. Hence, measurement of corrected serum calcium levels should be a part of evaluation protocol for these patients presenting with Torsades de pointes, besides serum potassium and magnesium.
Abbreviations
- DC
Direct current
- BP
Blood pressure
- ECG
Electrocardiogram
- HR
Heart rate
Compliance with Ethical Standards
Conflict of interest
None.
References
- 1.Cooper MS, Gittoes NJ. Diagnosis and management of hypocalcemia. BMJ. 2008;336:1298–1302. doi: 10.1136/bmj.39582.589433.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roden DM. A practical approach to torsade de pointes. Clin Cardiol. 1997;20:285–290. doi: 10.1002/clc.4960200318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carter EP, Andrus EC. QT interval in human electrocardiogram in absence of cardiac disease. JAMA. 1922;78:19–22. [Google Scholar]
- 4.Schwartz PJ, Periti M, Malliani A. The long QT syndrome. Am Heart J. 1975;89:378–390. doi: 10.1016/0002-8703(75)90089-7. [DOI] [PubMed] [Google Scholar]
- 5.Moss AJ. Prolonged QT-interval syndromes. JAMA. 1986;256:2985–2987. doi: 10.1001/jama.1986.03380210081029. [DOI] [PubMed] [Google Scholar]
- 6.Eryol NK, Colak R, Ozdogru I, Tanriverdi F, Unal S, Topsakal R, et al. Effects of calcium treatment on QT interval and QT dispersion in hypocalcemia. Am J Cardiol. 2003;91:750–752. doi: 10.1016/S0002-9149(02)03423-9. [DOI] [PubMed] [Google Scholar]
- 7.Bronsky D, Dubin A, Waldstein SS, Kushner DS. Calcium and the electrocardiogram. I. The electrocardiographic manifestations of hypoparathyroidism. Am J Cardiol. 1961;7:823–832. doi: 10.1016/0002-9149(61)90401-5. [DOI] [Google Scholar]
- 8.Ismail Z, Mohamed R, Hassan MHM, Wan SuK. Usage of traditional medicines among elderly and prednisolone contamination. MJMS. 2005;12:50–55. [PMC free article] [PubMed] [Google Scholar]
- 9.Patschan D, Loddenkemper K, Buttgereit F. Molecular mechanisms of glucocorticoid-induced osteoporosis. Bone. 2001;29:498–505. doi: 10.1016/S8756-3282(01)00610-X. [DOI] [PubMed] [Google Scholar]