Abstract
The patient was a 63-year-old man with drug-resistant atrial fibrillation who developed coronary spasm during cryoballoon ablation (CBA). CBA was started from the left inferior pulmonary vein. ST elevations in II, III, and aVf, with reciprocal ST depressions in V2-5, occurred in association with chest pain just after balloon rewarming and deflation, and the patient's blood pressure fell to 50 mmHg. Coronary angiography revealed 90% diffuse stenosis from the orifice of segment 1 to segment 4 in the right coronary artery. The stenosis and ST elevations improved after the intracoronary injection of nitroglycerine. Using continuous peripheral intravenous coronary vasodilation, we electrically isolated the other pulmonary veins with CBA without incident.
Keywords: coronary artery spasm, cryoballoon ablation, atrial fibrillation
Introduction
Radiofrequency (RF) ablation is commonly performed to treat atrial fibrillation (AF); however, cryoballoon ablation (CBA) for paroxysmal AF is expected to have a shorter operative time (1) and is associated with a lower incidence of recurrence after initial ablation (2). As Japanese have a higher prevalence of vasospastic angina (VSA) (3,4), we often encounter patients in whom chest pain is induced by exposure to cold (5). We herein report the case of a 63-year-old man with drug-resistant AF who developed coronary artery spasm (CAS) during CBA.
Case Report
A 63-year-old man was found to have AF during an examination 10 months before his first visit to our hospital. He had a history of appendicitis, pneumonia, hepatic disorder, and acute gastric bleeding with treatment for Helicobacter pylori infection. He had no known allergies or family history of sudden death or cardiac disease. The only coronary risk factor was a more than 40-year smoking history. He drank approximately 1,700 mL of beer every day. He had recently experienced exertional dyspnea. Bisoprolol fumarate (2.5 mg) and cibenzoline (100 mg), which had been prescribed by his family doctor, were initially effective for preventing AF. However, the patient developed atrial flutter, and was referred to our hospital for ablation. The electrocardiogram at his first visit to our hospital showed AF with no significant ST-T changes. Chest radiography revealed mild cardiomegaly with a cardiothoracic ratio of 57% and no pleural effusion. Transthoracic echocardiography revealed a slightly large left atrium (diameter: 39 mm) and left ventricular systolic dysfunction (left ventricular ejection fraction: 35%). The results of laboratory studies were as follows: brain natriuretic peptide, 90.6 g/dL; creatinine, 1.04 mg/dL; Hb, 14.5 g/dL; C-reactive protein, 0.07 mg/dL; and HbA1c, 5.7%. His thyroid function test results were unremarkable. The CHADS2 score was 1, due to the presence of heart failure. Coronary computed tomography angiography revealed no significant stenosis, with a single small calcification in both the left anterior descending coronary artery and the right coronary artery (RCA). Bisoprolol fumarate and cibenzoline were stopped, and edoxaban (a direct oral anticoagulant) was started. After 1 month of anticoagulant loading, CBA was performed under conscious sedation with dexmedetomidine hydrochloride and fentanyl. After obtaining transseptal access, the four pulmonary veins were identified and CBA was started from the left inferior pulmonary vein (LIPV). Fig. 1 shows the LIPV contrasting and the position of cryoballoon. Cooling for 3 minutes at the LIPV decreased the balloon and esophageal temperatures to -45℃ and 13.8℃, respectively. Then, the LIPV was electrically isolated. However, the heart rate decreased and ST elevations in II, III, and aVf accompanied by reciprocal ST depressions in V2-5, developed in association with chest pain just after balloon rewarming and deflation (Fig. 2). The patient's blood pressure fell to 50 mmHg and a vasopressor was administrated. There was no air embolus on coronary angiography (CAG); however, 90% diffuse coronary stenosis was observed from the orifice of segment 1 to segment 4 in the RCA (Fig. 3). The angiographic stenosis and electrocardiography (ECG) changes improved 2 minutes after an intracoronary injection of nitroglycerine (2.5 mg). No stenosis was apparent in the left coronary arteriography. We waited for 30 minutes, while maintaining peripheral intravenous infusion of a coronary vasodilator, nicorandil. Under continuous coronary vasodilation, we isolated the other 3 pulmonary veins with CBA; there were no ST changes and incidents (Fig. 2). Detailed history taking subsequently revealed that the patient usually felt chest pain when he entered the refrigeration room at work, and resolution when he left the refrigeration room. Although beta-blockers often worsen coronary spasm in VSA patients, bisoprolol fumarate, which was prescribed before the ablation, did not worsen his chest pain. A calcium channel blocker was prescribed, and the patient was given instruction on smoking cessation. He was discharged 4 days after the ablation.
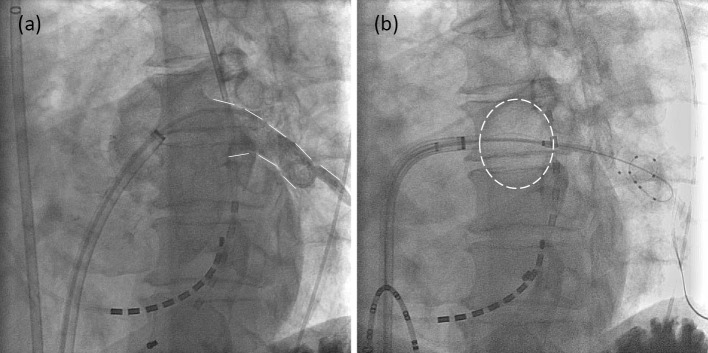
Figure 1.
Cryoballoon ablation was initiated from the left inferior pulmonary vein (LIPV). Left anterior oblique views are shown. (a) LIPV contrast is shown with a dotted line. (b) The cryoballoon during ablation is depicted with a dotted line.
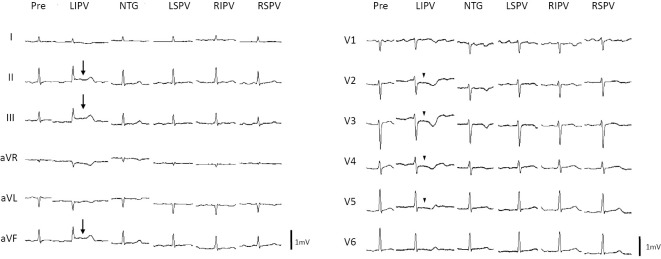
Figure 2.
Electrocardiography tracings obtained during cryoballoon ablation (CBA) are shown in chronological order. ST elevations in II, III, and aVf (arrows) accompanied by reciprocal ST segment depressions in V2-5 (arrowheads) were seen in association with chest pain just after balloon rewarming and deflation. The electrocardiography changes improved within 2 min after the intracoronary injection of nitroglycerine (2.5 mg). The other 3 pulmonary veins were isolated by CBA with no ST changes. LIPV: left inferior pulmonary vein, NTG: nitroglycerine, LSPV: left superior pulmonary vein, RIPV: right inferior pulmonary vein, RSPV: right superior pulmonary vein
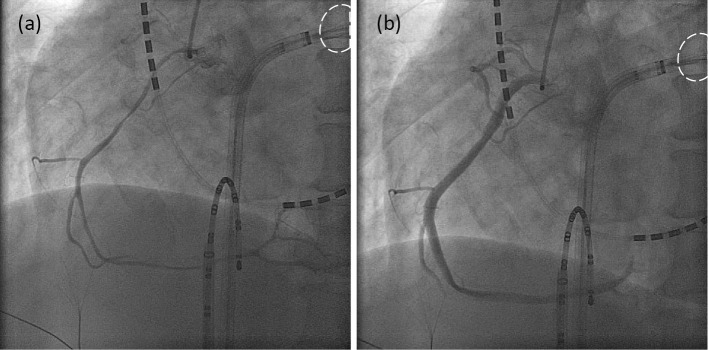
Figure 3.
(a) A coronary angiogram revealed no air embolus; however, 90% diffuse coronary stenosis was present from the orifice of segment 1 to segment 4 in the right coronary artery, just after balloon rewarming and deflation. The cryoballoon during ablation is depicted with a dotted line. (b) Angiographic stenosis improved within 2 min after the intracoronary injection of nitroglycerine (2.5 mg).
Discussion
In this case, diffuse coronary artery stenosis in the RCA developed during CBA. No findings of coronary air embolus on CAG and the immediate improvement following the administration of nitroglycerine indicated that the cause of coronary artery stenosis was CAS. CAS is an abnormal contraction of the epicardial coronary arteries, which results in myocardial ischemia (6). Although the underlying mechanism responsible for CAS remains unclear, reduced endothelial nitric oxide activity, hypercontraction of the coronary smooth muscle, and inflammation have been implicated (7,8). Smoking is the only predisposing factor for CAS, which is widely recognized in many studies, in contrast to the multiple risk factors for structural atherosclerotic coronary artery disease, such as hypertension, diabetes mellitus, and dyslipidemia (9-11). Oxidative particles that are present in cigarette smoke may contribute to vascular damage (12). In Japanese patients with VSA, regular alcohol consumption may also be involved. Alcohol consumption promotes the urinary excretion of magnesium (13). Magnesium deficiency may be related to the genesis of CAS in some patients with VSA. The patient in this case was a heavy smoker and drinker. Smoking and drinking cessation can help prevent CAS. Instructions for smoking cessation are indispensable to the treatment of VSA, and alcohol intake should be limited. The patient usually experienced chest pain with cold stimulation. A cool pressor test, which provokes CAS, is performed by submersing the patient's hand in ice water (5). Cold pressor stimulation induces reflex vasoconstriction in multiple vascular beds, with a consequent increase in the peripheral vascular resistance and systemic arterial blood pressure (14). Cold pressor stimulation has been shown to reduce coronary blood flow in some patients with coronary artery disease (15). Although beta-blockers often worsen CAS in VSA (16), our patient did not have increased chest pain.
Coronary artery complications have been reported after RF ablation; these include direct thermal injury by RF energy (17), embolus (18), and CAS (19-22). Although the relationship between the RF energy delivery or embolus site and the coronary artery lesion is clear (damage via direct thermal injury or embolus may occur), CAS does not necessarily occur near the point at which the RF energy is applied. The incidence of CAS due to RF ablation is extremely rare; it occurs more frequently in the RCA than in the left coronary artery (21). Most cases of CAS caused by RF ablation have no history of CAS (19-21). The detailed mechanism through which RF ablation causes CAS remains to be elucidated. However, human histological studies show that the atrium contains epicardial ganglionated plexuses, which consist of different patterns of sympathetic and vagal nerves (23). Thus, endocardial RF ablation may affect the epicardial ganglionated plexus through a thermal injury, which may cause an imbalance in autonomic nervous activity. Furthermore, a sudden increase in sympathetic or vagal tone might trigger CAS (24).
CAS has been reported to occur near the cooling site after the application of a cryoablation catheter (25,26). Conversely, the cryoballoon was located far from the RCA in our case (Fig. 3). Although the underlying mechanism is not clear, an imbalance in the autonomic nerve activity, which was possibly caused by RF ablation, might have contributed to CAS. Cooling in the left atrium during CBA is different from the cooling of the hand during a cold pressor test. It has been reported that CAS is induced during hypothermia therapy with ice packs and by chilled intravenous infusion after successful cardiopulmonary resuscitation (27). It is possible that blood cooled by the cryoballoon in the left atrium flows through the coronary arteries and induces CAS.
Although a near-fatal case involving CAS induced by CBA has been reported (28), the patient in the present case was diagnosed in the early phase, which enabled us to proceed with CBA after CAS. It is important for cryoballoon operators to understand that cold stimulation by CBA might induce CAS and to be prepared for this possibility. A thorough preoperative history should be taken to determine whether a patient has a history of chest pain and whether it is induced by exposure to cold. The administration of a calcium channel blocker and education on smoking cessation before ablation are also important. When vagal suppression is predicted, atropine (a vagal nerve blocker) may be useful. Given that the ST changes on ECG during CBA may reflect CAS, it is necessary to carefully monitor the ECG during CBA. Additionally, we should perform CAG when ST changes are observed during CBA and promptly administrate a coronary vasodilator.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Kuck K, Brugada J, Albenque J. Cryoballoon or radiofrequency ablation for atrial fibrillation. N Engl J Med 375: 1100-1101, 2016. [DOI] [PubMed] [Google Scholar]
- 2.Okumura K, Matsumoto K, Kobayashi Y, et al. . Safety and efficacy of cryoballoon ablation for paroxysmal atrial fibrillation in Japan-results from the Japanese prospective post-market surveillance study. Circ J 80: 1744-1749, 2016. [DOI] [PubMed] [Google Scholar]
- 3.Beltrame JF, Sasayama S, Maseri A. Racial heterogeneity in coronary artery vasomotor reactivity: differences between Japanese and Caucasian patients. J Am Coll Cardiol 33: 1442-1452, 1999. [DOI] [PubMed] [Google Scholar]
- 4.Pristipino C, Beltrame JF, Finocchiaro ML, et al. . Major racial differences in coronary constrictor response between Japanese and Caucasians with recent myocardial infarction. Circulation 101: 1102-1108, 2000. [DOI] [PubMed] [Google Scholar]
- 5.Raizner AE, Chahine RA, Ishimori T, et al. . Provocation of coronary artery spasm by the cold pressor test. Hemodynamic, arteriographic and quantitative angiographic observations. Circulation 62: 925-932, 1980. [DOI] [PubMed] [Google Scholar]
- 6.Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J Cardiol 51: 2-17, 2008. [DOI] [PubMed] [Google Scholar]
- 7.Kugiyama K, Yasue H, Okumura K, et al. . Nitric oxide activity is deficient in spasm arteries of patients with coronary spastic angina. Circulation 94: 266-271, 1996. [DOI] [PubMed] [Google Scholar]
- 8.Lanza GA, Careri G, Crea F. Mechanisms of coronary artery spasm. Circulation 124: 1774-1782, 2011. [DOI] [PubMed] [Google Scholar]
- 9.Scholl JM, Benacerraf A, Ducimetiere P, et al. . Comparison of risk factors in vasospastic angina without significant fixed coronary narrowing to significant fixed coronary narrowing and no vasospastic angina. Am J Cardiol 57: 199-202, 1986. [DOI] [PubMed] [Google Scholar]
- 10.Nobuyoshi M, Abe M, Nosaka H, et al. . Statistical analysis of clinical risk factors for coronary artery spasm: identification of the most important determinant. Am Heart J 124: 32-38, 1992. [DOI] [PubMed] [Google Scholar]
- 11.Sugiishi M, Takatsu F. Cigarette smoking is a major risk factor for coronary spasm. Circulation 87: 76-79, 1993. [DOI] [PubMed] [Google Scholar]
- 12.Morrow JD, Frei B, Longmire AW, et al. . Increase in circulating products of lipid peroxidation (F2-isoprostanes) in smokers. Smoking as a cause of oxidative damage. N Engl J Med 332: 1198-1203, 1995. [DOI] [PubMed] [Google Scholar]
- 13.Miwa K, Igawa A, Miyagi Y, Fujita M. Importance of magnesium deficiency in alcohol-induced variant angina. Am J Cardiol 73: 813-816, 1994. [DOI] [PubMed] [Google Scholar]
- 14.Greene MA, Boltax AJ, Lustig GA, Rogow E. Circulatory dynamics during the cold pressor test. Am J Cardiol 16: 54-60, 1965. [DOI] [PubMed] [Google Scholar]
- 15.Mudge GH Jr, Grossman W, Mills RM Jr, Lesch M, Braunwald E. Reflex increase in coronary vascular resistance in patients with ischemic heart disease. N Engl J Med 295: 1333-1337, 1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kern MJ, Ganz P, Horowitz JD, et al. . Potentiation of coronary vasoconstriction by beta-adrenergic blockade in patients with coronary artery disease. Circulation 67: 1178-1185, 1983. [DOI] [PubMed] [Google Scholar]
- 17.Wong KC, Lim C, Sadarmin PP, et al. . High incidence of acute sub-clinical circumflex artery ‘injury' following mitral isthmus ablation. Eur Heart J 32: 1881-1890, 2011. [DOI] [PubMed] [Google Scholar]
- 18.Kuwahara T, Takahashi A, Takahashi Y, et al. . Clinical characteristics of massive air embolism complicating left atrial ablation of atrial fibrillation: lessons from five cases. Europace 14: 204-208, 2012. [DOI] [PubMed] [Google Scholar]
- 19.Schwab JO, Burkhardt D, Yang A, Schrickel J, Luderitz B, Lewalter T. ECG signs mimicking acute inferior wall myocardial infarction are associated with elevated myocardial enzymes during isolation of pulmonary vein for focal atrial fibrillation. Europace 6: 111-115, 2004. [DOI] [PubMed] [Google Scholar]
- 20.Tada H, Naito S, Oshima S, Taniguchi K. Vasospastic angina shortly after left atrial catheter ablation for atrial fibrillation. Heart Rhythm 2: 867-870, 2005. [DOI] [PubMed] [Google Scholar]
- 21.Hishikari K, Kuwahara T, Takahashi A, Isobe M. Severe coronary artery spasm during radiofrequency ablation for atrial fibrillation. Int J Cardiol 172: e513-e515, 2014. [DOI] [PubMed] [Google Scholar]
- 22.Fujiwara R, Yoshida A, Hirata K. Ventricular fibrillation associated with multi-vessel coronary spasms following radiofrequency ablation of atrial fibrillation and atrial flutter. Europace 16: 1060, 2014. [DOI] [PubMed] [Google Scholar]
- 23.Kawano H, Okada R, Yano K. Histological study on the distribution of autonomic nerves in the human heart. Heart Vessels 18: 32-39, 2003. [DOI] [PubMed] [Google Scholar]
- 24.Lanza GA, Pedrotti P, Pasceri V, Lucente M, Crea F, Maseri A. Autonomic changes associated with spontaneous coronary spasm in patients with variant angina. J Am Coll Cardiol 28: 1249-1256, 1996. [DOI] [PubMed] [Google Scholar]
- 25.Rajbanshi BG, Rodrigues E, Lynch JJ, Gulati R, Sundt TM 3rd. Coronary artery spasm after Cryo Maze III procedure. Ann Thorac Surg 92: 1884-1887, 2011. [DOI] [PubMed] [Google Scholar]
- 26.Miyazaki S, Ichihara N, Takagi T, Iesaka Y. Coronary artery spasm during cryothermal cavotricuspid isthmus ablation. J Cardiovasc Electrophysiol 2015. [DOI] [PubMed] [Google Scholar]
- 27.Akin I, Rehders TC, Kische S, et al. . Diffuse coronary spasm during therapeutic hypothermia. Int J Cardiol 148: 373-375, 2011. [DOI] [PubMed] [Google Scholar]
- 28.Lehrmann H, Potocnik C, Comberg T, et al. . Near-fatal coronary artery spasm during cryoballoon pulmonary vein isolation: an unreported complication. Circ Arrhythm Electrophysiol 7: 1273-1274, 2014. [DOI] [PubMed] [Google Scholar]