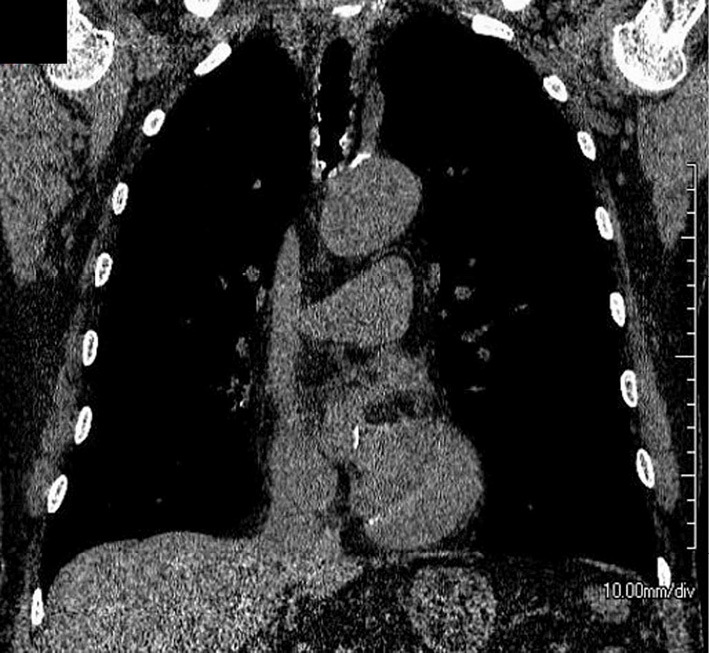
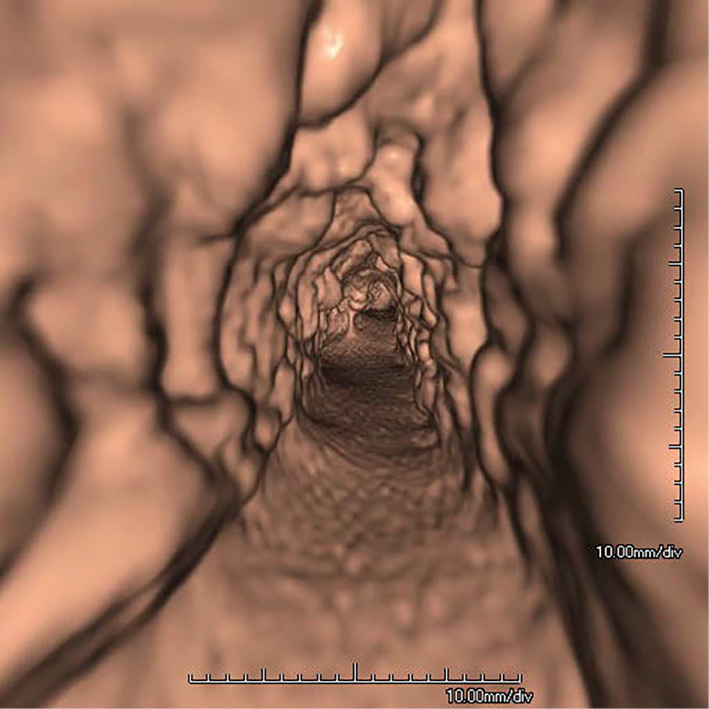
Tracheal intubation repeatedly failed in an 80-year-old man. Although chest X-ray showed no obvious abnormalities, computed tomography (CT) revealed raised lesions accompanied by calcification at the tracheal wall (Picture 1). Furthermore, virtual bronchoscopy using three-dimensional CT demonstrated many protruding lesions in the tracheal lumen (Picture 2).
Picture 1.
Picture 2.
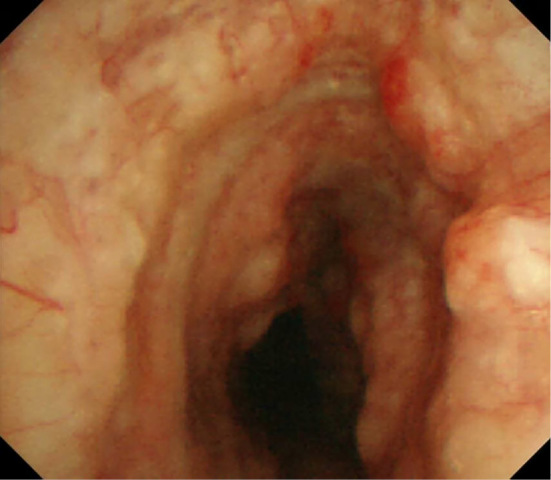
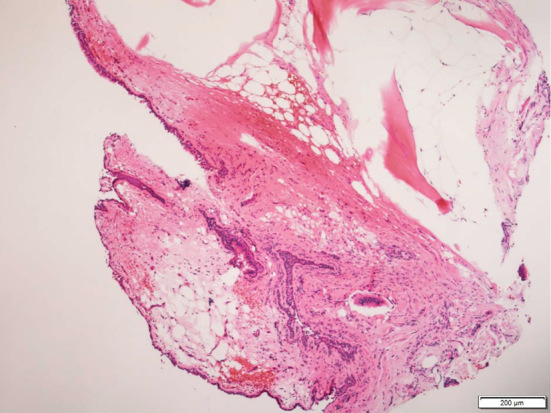
Bronchoscopy revealed numerous protruding white lesions from the trachea to both main bronchi, excluding membranous areas (Picture 3). In addition, a tissue biopsy of the diseased lesion showed bone tissue and mild infiltration of inflammatory cells (Picture 4). Based on these findings, the patient was diagnosed with tracheobronchopathia osteochondroplastica (TO).
Picture 3.
Picture 4.
The etiology of this condition is considered to be chronic irritation and metaplasia of elastic connective tissue (1). While many patients with TO show chronic coughing and some respiratory symptoms, others are incidentally noted at autopsy or on bronchoscopy (2). If tracheal intubation is difficult, it is important to consider TO in the differential diagnosis.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Muhanned AH, Daivid L, Aidney SB. Tracheobronchopathia osteochondroplastica: a rare large airway disorder. Lung 186: 353-359, 2008. [DOI] [PubMed] [Google Scholar]
- 2.Wang N, Long F, Jiang S. Tracheobronchopathia osteochondroplastica: two cases reports and review of literature. Medicine (Baltimore) 95: e3396, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]


