Abstract
Objective
Patients normotensive in the trauma bay despite documented prehospital hypotension may not be recognized as significantly injured. The purpose of this study was to determine whether isolated prehospital hypotension portends poor outcomes and correlates with injury severity.
Methods
Prospective cohort study conducted at a level 1 university trauma center. The lowest recorded prehospital systolic blood pressure (SBP) and the first recorded SBP on hospital arrival were used to divide patients into either the normotensive (NP) or hypotensive (HP) group. Patients who failed to achieve normotension on hospital arrival were excluded. Hypotension was defined as SBP≤110 mmHg.
Results
Compared to NP (n=206), HP (n=81) had lower Glasgow Coma Scores both prehospital (12.81±0.44 vs 14.38±0.13) and at hospital admission (12.78±0.47 vs 14.37±0.14). Injury Severity Score positively correlated with prehospital hypotension (HP 12.27±1.12 vs NP 9.22±0.49). Prehospital hypotension positively correlated with intensive care unit (ICU) admission (HP 56.79% vs NP 22.82%), ICU length of stay (LOS) (HP 3.23±0.71 vs NP 0.71±0.17), hospital LOS (HP 8.58±1.39 vs NP 4.86±0.33), ventilator days (HP 3.38±1.20 vs NP 0.27±0.08 days), and repeat hypotensive episodes during their hospital stay (HP 81.71% vs NP 38.16%). HP also required more packed red blood cells in the first 24 hours after admission (22% vs 6%). Significance was set at p<0.05.
Conclusions
Isolated prehospital hypotension in patients in the trauma and emergency department correlates with increased injury severity and portends worse outcomes despite a normal blood pressure reading at admission. Prehospital hypotension must be given heavy consideration in triage, as these patients may be transiently hypotensive and appear less critical than their true status.
Level of Evidence
Level II, Prognostic study.
Keywords: hypotension, triage, Emergency Medical Services, trauma/ critical care
Background
Among the principal vital signs, blood pressure offers medical providers valuable insight into certain aspects of their patients' clinical status, such as intravascular volume and degree of hemorrhagic shock. Hypotension has also been found to correlate with injury severity, morbidity, and mortality.1–3 Therefore, blood pressures recorded in the emergency department (ED) are given strong consideration in triage decision-making.4
Of the traumatically injured patients evaluated in the trauma bay or ED with normal blood pressure readings, there exists a subset of patients who have transient documented hypotension prior to arrival (eg, at the referring hospital or en route with emergency medical services (EMS)). Previous retrospective research has shown that this group of patients may be at risk for undertriage and delayed treatment.5 Other studies, however, have shown that EMS blood pressure recordings are not always accurate, pointing to factors such as environmental noise and distractions at the scene.6–8 As a result, the value of EMS blood pressure recordings remains controversial.
The purpose of our study is to evaluate the relationship of isolated prehospital hypotension to injury severity and ultimate outcome in patients with trauma who arrive normotensive. The use of a prospective cohort was implemented to minimize recall bias and confounders, as well as to offer a more accurate analysis compared to previous retrospective studies. In addition, our study takes place in a predominantly urban setting, which serves as a contrast to similar studies conducted in the rural population.5 We hypothesize that isolated prehospital hypotension portends negative outcomes and serves as an indicator of injury severity.
Methods
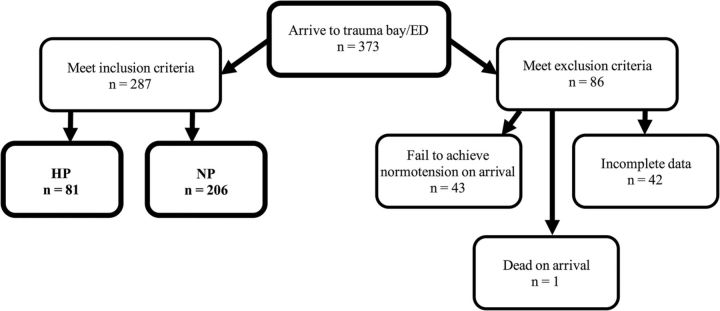
This prospective cohort study was conducted at The Nebraska Medical Center (TNMC), a 735-bed, level 1 trauma center averaging ∼1400 patients with trauma each year. Data were collected between May and August 2014 from the TNMC trauma registry, patient charts, the Electronic Nebraska Ambulance Rescue Service Information System, and referring hospitals. From these sources, we obtained patient demographics, prehospital and admission systolic blood pressure (SBP), prehospital and admission Glasgow Coma Scores (GCS), injury severity score (ISS), injury location and mechanism, hospital length of stay (LOS), intensive care unit (ICU) admission rate and ICU LOS, ventilator days, repeat hypotensive episodes, and administration of packed red blood cells (PRBC) during the hospital stay (tables 1–3). Unless otherwise stated, ‘admission’ refers to arrival at the trauma bay or ED. Patients were excluded if they remained hypotensive on admission, if they were transferred by a non-EMS service and thus had no prehospital SBP documentation, or if they had incomplete data (figure 1). Approval for this study was obtained from the University of Nebraska Medical Center Institutional Review Board.
Table 1.
Patient demographics
| Hypotensive patients (n=81) | Normotensive patients (n=206) | p Value | |
|---|---|---|---|
| Sex | Female: 33 Male: 48 |
Female: 82 Male: 124 |
0.77 |
| Age | 38.8±2.7 | 51.1±1.6 | <0.0001 |
| Method of transport | Ambulance: 62 Helicopter: 19 Police: 0 |
Ambulance: 184 Helicopter: 20 Police: 2 |
0.0078 |
| Injury mechanism | Blunt: 73 Burn: 1 Penetrating: 7 |
Blunt: 190 Burn: 2 Penetrating: 14 |
0.7593 |
| Injury location | Head: 27 Head, thorax: 2 Head, appendage: 10 Thorax: 4 Back: 4 Other: 34 |
Head: 65 Head, thorax: 11 Head, appendage: 19 Thorax: 10 Back: 11 Other: 90 |
0.8649 |
Data are presented as mean±SE.
Table 2.
Injury severity data
| Hypotensive patients | Normotensive patients | p Value | |
|---|---|---|---|
| Average prehospital SBP | 99.11±1.75 mm Hg | 143.44±1.59 mm Hg | <0.0001 |
| Average ED SBP | 132.65±1.39 mm Hg | 148.47±1.69 mm Hg | <0.0001 |
| Average prehospital GCS | 12.81±0.44 | 14.38±0.13 | <0.0001 |
| Average ED GCS | 12.78±0.47 | 14.37±0.14 | <0.0001 |
| ISS | 12.27±1.12 | 9.22±0.49 | <0.0001 |
Data are presented as mean±SE.
ED, emergency department; GCS, Glasgow Coma Score; SBP, systolic blood pressure.
Table 3.
Outcomes data, hypotension defined as SBP ≤110 mm Hg
| Hypotensive patients | Normotensive patients | p Value | |
|---|---|---|---|
| ICU admissions | 56.79% | 22.82% | <0.0001 |
| ICU LOS (days) | 3.23±0.71 | 0.71±0.17 | <0.0001 |
| Hospital LOS | 8.58±1.39 | 4.86±0.33 | 0.0105 |
| Ventilator days | 3.38±1.20 | 0.27±0.08 | 0.0001 |
| Repeat hypotensive episodes | 81.48% | 38.35% | <0.0001 |
| PRBC in first 24 hours | 22%±8% | 6%±2% | 0.0114 |
Data are presented as mean±SE or percent (patients).
ICU, intensive care unit; LOS, length of stay; PRBC, packed red blood cells; SBP, systolic blood pressure.
Figure 1.
Flow diagram illustrating breakdown of exclusion and inclusion criteria. ED, emergency department; HP, hypotensive; NP, normotensive.
While hypotension has traditionally been defined as an SBP ≤90 mm Hg, recent studies suggest that higher values are more accurate. Therefore, we defined hypotension as an SBP ≤110 mm Hg, consistent with current evidence.9–11 For comparison, we also analyzed outcomes using the traditional hypotension definition of SBP ≤90 mm Hg. For each patient, the lowest recorded prehospital SBP (either from EMS or the referring hospital) and the first recorded SBP on arrival at the trauma bay or ED were used. Statistical methods for linear models were used for continuous variables.12 χ2 or Fisher exact tests were used for categorical variables depending on whether or not the observed number in each cell was >5.13 t-Test was used for the comparisons of two continuous samples, but if data were skewed and sample sizes small, then the Mann-Whitney-Wilcoxon test was used. This is a non-parametric method, which was used for testing if two samples were from the same distribution.14 Statistical significance was defined as p<0.05. All the analyses were performed using SAS 9.4.
Results
Two hundred eighty-seven patients met the inclusion criteria. Patients normotensive in the trauma bay or ED were divided into either the normotensive group (NP) or hypotensive group (HP) based on prehospital SBP. Patient sex, injury mechanism, and injury location did not significantly differ between the NP and HP groups. Patients in the HP cohort tended to be younger and were more likely to be transported via helicopter compared to the NP group (table 1).
Compared to NP (n=206 patients), hypotensive patients (HP) (n=81 patients) had lower GCS both prehospital (12.81±0.44 vs 14.38±0.13, p<0.05) and at hospital admission (12.78±0.47 vs 14.37±0.14, p<0.05). ISS positively correlated with prehospital hypotension (HP 12.27±1.12 vs NP 9.22±0.49, p<0.05) (table 2).
With regard to medical outcomes, prehospital hypotension had a positive correlation with ICU admission (HP 56.79% vs NP 22.82%, p<0.05), ICU LOS (HP 3.23±0.71 vs NP 0.71±0.17, p<0.05), hospital LOS (HP 8.58±1.39 vs NP 4.86±0.33), ventilator days (HP 3.38±1.20 vs NP 0.27±0.08 days, p<0.05), and repeat hypotensive episodes during hospital stay (HP 81.71% vs NP 38.16%, p<0.05). HP also required more packed red blood cells in the first 24 hours after admission (22% vs 6%) (table 3).
The outcome variables for HP compared to NP were also investigated using the traditional hypotension definition of SBP ≤90 mm Hg, and similar results were observed (table 4).
Table 4.
Outcomes data, hypotension defined as SBP ≤90 mm Hg
| Hypotensive patients (n=20) | Normotensive patients (n=272) | p Value | |
|---|---|---|---|
| ICU admissions | 70% | 30.51% | 0.0008 |
| ICU LOS (days) | 1 | 0 | 0.0002 |
| Hospital LOS | 6.5 | 4 | 0.0011 |
| Ventilator days | 0 | 0 | 0.0024* |
| Repeat hypotensive episodes | 85% | 48.53% | 0.0019 |
| PRBC in first 24 hours | 20% | 3.69% | 0.0105 |
Data are presented as median or percent (patients).
*HP were found to have significantly higher ventilator days compared to NP based on the Mann-Whitney-Wilcoxon test despite equivalent medians. Detailed explanation is provided in the Methods section.
ICU, intensive care unit; LOS, length of stay; PRBC, packed red blood cells; SBP, systolic blood pressure.
Discussion
The most important findings of this prospective cohort study is that isolated prehospital hypotension is an indicator of injury severity in patients who arrive normotensive at the ED or trauma bay and also portends worse outcomes in these patients. These conclusions are supported by previously published retrospective reviews.3 5 Our study also supports the use of SBP ≤110 mm Hg as the definition for hypotension in patients with trauma.
HP patients were found to have significantly lower EMS and ED GCS and had higher ISS, all indicating that the HP group suffered more critical injuries than did the NP group. Neither the ISS nor GCS is calculated using SBP; therefore, the correlation between the three may be considered independent yet accurate measures of injury severity. ISS and GCS also have been shown to be valuable predictors of ICU LOS;15 therefore, our study supports that ISS may be considered both a marker of injury severity and a predictor of patient outcomes.
HP were shown to have worse outcomes after admission than NP, as HP were more likely to be admitted to the ICU and had a higher LOS in the ICU and in the hospital, spent over nine times more days on the ventilator, experienced more episodes of repeat hypotension during their hospital stay, and required more PRBC than did the NP group. Not only are these negative outcomes in themselves, but they also each pose further potential complications. For example, ICU LOS has been found to positively correlate with increased risk of iatrogenic infections, hospital mortality, and costs.16 17 Repeat hypotension during the hospital stay itself has been found to be a reliable predictor of adverse hospital outcomes and mortality, especially if prolonged.18 19
As expected, sex, injury mechanism, and injury location did not significantly differ between our group of HP and NP. HP, however, were younger compared to NP. This is perhaps a function of age, as SBP is known to increase with age.20 However, given that younger age historically portends improved outcomes for any given ISS,21 this finding relative to transient prehospital hypotension is significant.
Until now, similar studies have used the traditional definition of hypotension as SBP ≤90 mm Hg; however, the current literature suggests that this definition may be too low. For this reason, we used the hypotension threshold of SBP ≤110 mm Hg and compared those outcomes using the traditional SBP ≤90 mm Hg definition. It is highly significant that we observe similar results using a greater hypotension threshold, even though this expansion increased the likelihood of including more ‘healthy’ patients in the hypotensive group. Therefore, emergency and trauma physicians should take prehospital hypotension seriously and also not be quick to judge a patient with an admission SBP between 90 and 110 mm Hg as being simply ‘normotensive.’
Though they may appear euvolemic based on admission SBP, patients with isolated prehospital hypotension are at risk for undertriage. Conceivably, this may lead to improper level of care assignment, inadequate treatment, and ultimately poorer outcomes. Better recognition and appropriate triage of patients with trauma with documented prehospital hypotension, therefore, may help minimize poor outcomes in patients with trauma.
Our study provides further evidence for the value of assessing prehospital hypotension in patients with trauma and does so in different ways than previous similar studies. As a prospective cohort, we were able to minimize recall bias and other confounders. Our research adds further support to the conclusions of previous retrospective reviews such as the study by Schenarts et al.5 Additionally, it provides a nice comparison between the urban and rural population and their associated differences in transport times. Potential limitations to our study include lack of discharge disposition data in evaluating outcomes, that is, discharge to home, rehabilitation center, nursing home, etc. We also did not evaluate mortality rate between HP and NP groups, which would certainly be of value in future studies. In addition, the exclusion of patients with incomplete data may have led to a selection bias in our sample population.
Prehospital SBP should be highly considered in trauma center and emergency department triage decisions. Compared to the historic ISS and GCS, prehospital SBP proves to also offer a valuable assessment of injury severity and a patient's status without the need of a formula or calculation. For patients transferred in from referring hospitals or by EMS, it is not uncommon for the trauma physician to receive incomplete information regarding the patient. EMS crews should be encouraged to make their best efforts in recording accurate SBPs, and all episodes of prehospital hypotension need to be relayed to the receiving trauma team. For patients who are transferred from other hospitals, records should be sent promptly and in their entirety, especially records of vital signs. In the process of our research, we found that documentation from transferring hospitals was often incomplete. With the continued implementation of electronic medical charting systems, it is tenable that this information will be more easily accessible.
Conclusions
This study demonstrates that isolated prehospital hypotension in patients at the trauma and emergency department, defined by an SBP ≤110 mm Hg, correlates with increased injury severity and also portends poor outcomes for patients despite normal blood pressure readings on admission. These outcomes include increased hospital LOS, increased admissions to the ICU and increased LOS in the ICU, increased risk of future hypotensive episodes during the hospital admission, increased ventilator days, and increased frequency of blood transfusions. Prehospital hypotension must be given heavy consideration in triage, as these patients may be transiently hypotensive and appear less critical than their true status.
Acknowledgments
The authors thank Kimberly McWilliams for technical and data support. They also thank the UNMC Department of General Surgery for sponsoring the Department of Surgery Summer Student Research Program of Excellence.
Footnotes
This work was performed at the University of Nebraska Medical Center, Omaha, Nebraska.
Portions of this research have been presented in both abstract and poster form at the 2015 National Congress for the Society of Critical Care Medicine in Phoenix, Arizona (abstract award recipient), and at the 2015 Midwest Biomedical Conference in Omaha, Nebraska.
Contributors: CD served as the primary investigator for this research by performing the majority of the literature search, data collection and interpretation, and manuscript creation. Data analysis and further interpretation was performed by JL, a biostatistician. KLB developed the study design, oversaw the research in its entirety, and provided critical revisions of the manuscript.
Competing interests: None declared.
Ethics approval: University of Nebraska Medical Center IRB.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Shapiro NI, Kociszewski C, Harrison T, Chang Y, Wedel SK, Thomas SH. Isolated prehospital hypotension after traumatic injuries: a predictor of mortality? J Emerg Med 2003;25:175–9. doi:10.1016/S0736-4679(03)00167-7 [DOI] [PubMed] [Google Scholar]
- 2.Lipsky AM, Gausche-Hill M, Henneman PL, Loffredo AJ, Eckhardt PB, Cryer HG, de Virgilio C, Klein SL, Bongard FS, Lewis RJ. Prehospital hypotension is a predictor of the need for an emergent, therapeutic operation in trauma patients with normal systolic blood pressure in the emergency department. J Trauma 2006;61:1228–33. doi:10.1097/01.ta.0000196694.52615.84 [DOI] [PubMed] [Google Scholar]
- 3.Codner P, Obaid A, Porral D, Lush S, Cinat M. Is field hypotension a reliable indicator of significant injury in trauma patients who are normotensive on arrival to the emergency department? Am Surg 2005;71:768–71. [PubMed] [Google Scholar]
- 4.Lehmann R, Brounts L, Lesperance K, Eckert M, Casey L, Beekley A, Martin MA. A simplified set of trauma triage criteria to safely reduce overtriage: a prospective study. Arch Surg 2009;144:853–8. doi:10.1001/archsurg.2009.153 [DOI] [PubMed] [Google Scholar]
- 5.Schenarts PJ, Phade SV, Agle SC, Goettler CE, Sagraves SG, Newell MA, Rotondo MF. Field hypotension in patients who arrive at the hospital normotensive: a marker of severe injury or crying wolf? N C Med J 2008;69:265–9. [PubMed] [Google Scholar]
- 6.Prasad NH, Brown LH, Ausband SC, Cooper-Spruill O, Carroll RG, Whitley TW. Prehospital blood pressures: inaccuracies caused by ambulance noise? Am J Emergency Med 1994;12:617–20. doi:10.1016/0735-6757(94)90025-6 [DOI] [PubMed] [Google Scholar]
- 7.Low RB, Martin D. Accuracy of blood pressure measurements made aboard helicopters. Ann Emerg Med 1988;17:604–12. doi:10.1016/S0196-0644(88)80401-3 [DOI] [PubMed] [Google Scholar]
- 8.Hunt RC, Allison EJ Jr, Whitley TW, Robinson MJ, Smart TL. Comparison of EMT blood pressure measurements with an automated blood pressure monitor: on scene, during transport, and in the emergency department. Ann Emerg Med 1985;14:871–5. doi:10.1016/S0196-0644(85)80636-3 [DOI] [PubMed] [Google Scholar]
- 9.Bruns B, Gentilello L, Elliott A, Shafi S. Prehospital hypotension redefined. J Trauma 2008;65:1217–21. doi:10.1097/TA.0b013e318184ee63 [DOI] [PubMed] [Google Scholar]
- 10.Eastridge BJ, Salinas J, McManus JG, Blackburn L, Bugler E, Cooke W, Concertino V, Wade C, Holcomb J. Hypotension begins at 110 mm Hg: redefining “hypotension” with data. J Trauma 2007;63:291–9. doi:10.1097/TA.0b013e31809ed924 [DOI] [PubMed] [Google Scholar]
- 11.Berry C, Ley EJ, Bukur M, Malinoski D, Margulies D, Mirocha J, Salim A. Redefining hypotension in traumatic brain injury. Injury 2012;43:1833–7. doi:10.1016/j.injury.2011.08.014 [DOI] [PubMed] [Google Scholar]
- 12.Little R, Stroup W, Freund R. SAS for Linear Models. 4th Ed Cary, NC: SAS Institute, 2002. [Google Scholar]
- 13.Agresti A. Categorical data analysis. 3rd edn Hoboken, New Jersey: John Willey & Sons, 2013. [Google Scholar]
- 14.Randels RH, Wolfe DA. Introduction to the theory of nonparametric statistics. New York: John Willey & Sons, 1979. [Google Scholar]
- 15.Böhmer AB, Just KS, Lefering R. Factors influencing lengths of stay in the intensive care unit for surviving trauma patients: a retrospective analysis of 30,157 cases. Crit Care 2014;18:R143 doi:10.1186/cc13976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y. International study of the prevalence and outcomes of infection in intensive care units. JAMA 2009;302:2323–9. doi:10.1001/jama.2009.1754 [DOI] [PubMed] [Google Scholar]
- 17.Wunsch H, Gershengorn H, Scales DC. Economics of ICU organization and management. Crit Care Clinics 2012;28:25–37. doi:10.1016/j.ccc.2011.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones AE, Aborn LS, Kline JA. Severity of emergency department hypotension predicts adverse hospital outcome. Shock 2004;22:410–14. doi:10.1097/01.shk.0000142186.95718.82 [DOI] [PubMed] [Google Scholar]
- 19.Bilello JF, Davis JW, Lemaster D, Townsend RN, Parks SN, Sue LP, Kaups KL, Groom T, Egbalieh B. Prehospital hypotension in blunt trauma: identifying the “Crump Factor”. J Trauma Acute Care Surg 2011;70:1038–42. doi:10.1097/TA.0b013e31819638d0 [DOI] [PubMed] [Google Scholar]
- 20.Pinto E. Blood pressure and ageing. Postgrad Med J 2007;83:109–14. doi:10.1136/pgmj.2006.048371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Perdue PW, Watts DD, Kaufmann CR, Trask AL. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. J Trauma 1998;45:805–10. doi:10.1097/00005373-199810000-00034 [DOI] [PubMed] [Google Scholar]