Abstract
Purpose:
Changing pattern of uveitis in a subset of a population is an important ocular health indicator.
Methods:
A comparative study was done between uveitis patients of 2013 and 1995 using two proportions Z-test.
Results:
In 2013, 352 new uveitis cases were examined. Males 56%, females 44%; unilateral 30.4%; bilateral in 69.6%. A specific diagnosis achieved in 66.2%. Anterior uveitis was seen in 35.22%, intermediate uveitis in 30.11%, posterior uveitis in 25%, and panuveitis in 9.65%. There was no significant difference in the incidence of new uveitic cases (1.04% vs. 1.8%). A decline in male preponderance from 64% to 56% (P = 0.0187) was observed. In both studies, anterior uveitis was the most common but human leukocyte antigen-B27 positivity uveitis had increased (29.83% vs. 14.5%; P < 0.05). Intermediate uveitis was the second-most common type instead of posterior uveitis (P = 0.0006). In posterior uveitis cases, etiology was established in 88.6% versus 56.06% cases (P < 0.05). The most common cause of posterior uveitis was tuberculosis (TB) (35.2%). Viral retinitis had increased to 6.81% from 0.76% (P < 0.05). However, a declining trend in cases of toxoplasmosis was observed (P = 0.0545). The cause of panuveitis was comparable in both studies. The prevalence of TB has significantly increased in the present era (22.5% vs. 0.64%; P < 0.0001) and was the proven etiological cause of uveitis in overall 22.5% of which 4.8% cases were of anterior uveitis cases, 7.1% cases of intermediate uveitis cases, 8.8% cases of posterior uveitis cases, and 1.8% of panuveitis cases.
Conclusion:
A shifting paradigm of uveitis over the past two decades was observed.
Keywords: Changing pattern, retinitis, toxoplasmosis, tuberculosis, uveitis, South India
With the commencement of the 21st century, major remarkable changes have taken place in the diagnosis and management of the uveitic practice. A change in the pattern of uveitis has also been observed with the emergence and identification of newer entities of uveitis.[1] The pattern of uveitis can be vivid and can vary from country to country and region to region. There are various reports available from different regions of India regarding the epidemiology of uveitis.[2,3] The changing pattern of uveitis is also influenced by several demographic and ethnic factors. Moreover, the latest advancement in diagnostic modalities of uveitis has greatly influenced the identification of etiology of uveitis. The study on changing pattern of uveitis is therefore important to know further newer occurrences of various disease prevalence.[4] Das et al.[4] also mentioned that awareness of regional variation in disease configuration is essential to develop a region-specific list of differential diagnoses and also for comparison with different sub-population of the country and the world. However, these data should be periodically collected so that comparison between past and present scenario can be done. Since then, there have been several advances in the diagnostic criteria, imaging, and other ancillary modalities to reach the specific diagnosis and “changing patterns of uveitis”[5] over the years. Hence, there is a need to determine the present trend of etiologies in uveitis patients in our population.[3]
The first reported article on the pattern of uveitis in India is from the same author in 1995[1] which determined the trend of etiologies of uveitis in the Southern population of India during the 1990s. After two decades, we present this study on the changing pattern of uveitis experienced by the same author in same the region of India which is a Tertiary Referral Eye Institute of India. The aim of this study is to document the shifting paradigm of uveitis in a subset of a population of ocular disease which can act as an important health indicator.
Methods
A retrospective review of records was done from institution database, which included all the new uveitis patients presented to uvea clinic of a tertiary ophthalmic care center in South India between January and December 2013. The results of this study were compared with the study performed by the same author, in the same clinical setup, in the same geographic location for the same duration (January to December 1992) and published in 1995.[1] Approval from the Institutional Review Board of Medical Research Foundation was taken and adherence to the tenets of Declaration of Helsinki maintained.
International uveitis study group classification and descriptors were followed.[6] Detailed ocular findings were documented by external examination, slit lamp biomicroscopy, applanation tonometry, and indirect ophthalmoscopy with scleral depression after maximum pupillary dilatation. Ancillary ocular investigations such as ultrasonography, fundus fluorescein angiography, indocyanine green, ultrasound biomicroscope, and optical coherence tomography angiography (OCT) were performed as per need. All patients underwent careful history evaluation for specific ocular uveitis entities or association with systemic diseases. Laboratory investigations were carried out in each case in a tailored approach. The additional ancillary tests used for the present study was high resolution computed tomography of the chest to rule of tuberculosis (TB) and sarcoidosis; QuantiFERON-TB GOLD test to support TB and OCT for analysis of macular thickness. Polymerase chain reaction (PCR) analysis in suspected cases of infectious uveitis was performed for mycobacterium TB (nested and real-time), herpes simplex virus 1, 2, varicella zoster virus, and cytomegalovirus, and Toxoplasma gondii. Human leukocyte antigen (HLA) B typing were performed in nongranulomatous uveitis cases to rule out HLA-B27-related uveitis and Behcet's disease.
The term idiopathic was used for cases in which the intraocular inflammation was not characteristic of a recognized uveitic entity or could not be attributed to a specific underlying systemic disease. The patients with traumatic uveitis, lens-induced uveitis, endophthalmitis, and Eales' disease were not included as it was excluded in the previous study.
The aim of the study was to compare the changing patterns of uveitis over two decades in South India. Hence, the results of past and present studies were compared using two proportion Z-test. The P < 0.05 was taken statistical significant, 95% confidence interval and acceptable margin of error of 5% were considered. SPSS 14 software (SPSS Inc., Chicago, IL, USA) was used for analysis.
Results
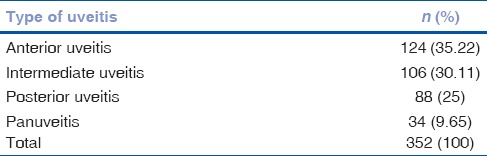
Total uveitis cases seen in this study were 352 amounting to 1.04% of all new ophthalmic patients examined in this period in this institute of which males were 56% and females were 44%. Unilateral involvement was in 107 cases and bilateral in 245 cases. Thus, 597 eyes of 352 uveitic patients were affected. Maximum patients (69.9% n = 246) were in the age group of 20–29 years. Anterior uveitis was the most common anatomical type of uveitis (35.22%) [Table 1].
Table 1.
The anatomical types of uveitis
The tailored laboratory investigations established the specific diagnosis in 233 cases (66.2%). The specific diagnosis was identified mainly in posterior uveitis (88.64%) than in other anatomic types of uveitis.
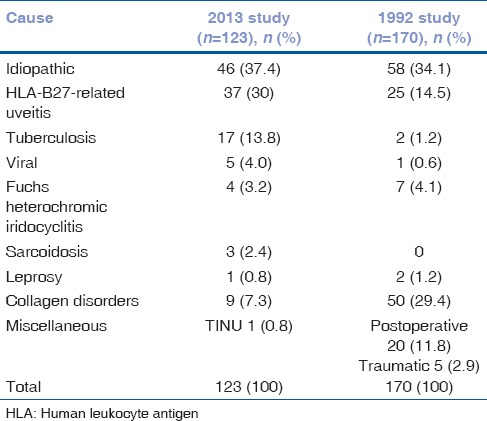
Among cases of anterior uveitis, 66.9% were idiopathic followed by HLA B27 associated acute anterior uveitis (30%) and TB (13.70%) [Table 2].
Table 2.
Etiological cause of different types of anterior uveitis
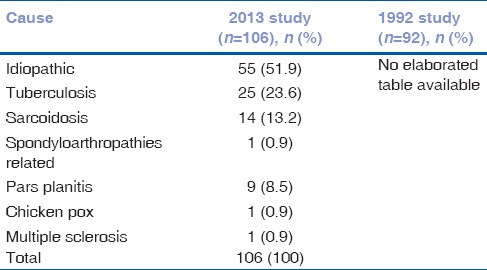
Intermediate uveitis was the second leading cause of uveitis. A total of 106 cases (30.1%) were suffering from intermediate uveitis among which 51.88% cases were of idiopathic origin. TB and sarcoidosis were identified in 23.58% and 13.21%, respectively [Table 3].
Table 3.
Etiological cause of different types of intermediate uveitis
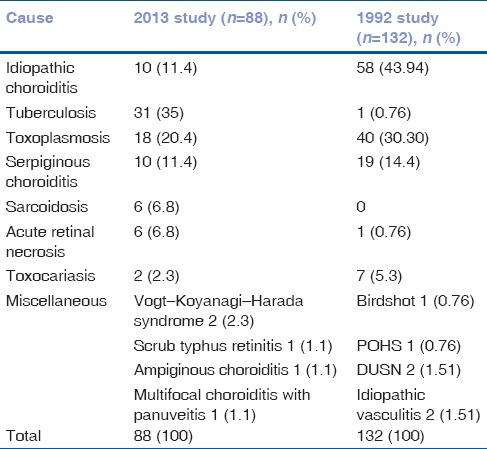
Posterior uveitis cases comprised of 25% of the study in population. The etiology could be established in 88.6% cases, and the most common cause was TB-related posterior uveitis in 35.2% (n = 31) cases. The manifestation of proven tubercular posterior uveitis was in the form of multifocal serpiginous choroiditis (17 cases), tuberculoma (7 cases), tubercular subretinal abscess (4 cases), and vasculitis (3 cases). Other common causes of posterior uveitis are depicted in Table 4. A case of scrub typhus associated retinitis was identified in a 2-year-old child.
Table 4.
Etiological cause of different types of posterior uveitis
Panuveitis was present in 9.6% (n = 34). The most common cause of panuveitis was Vogt–Koyanagi–Harada (VKH) syndrome [Table 5].
Table 5.
Etiological causes of different types of panuveitis
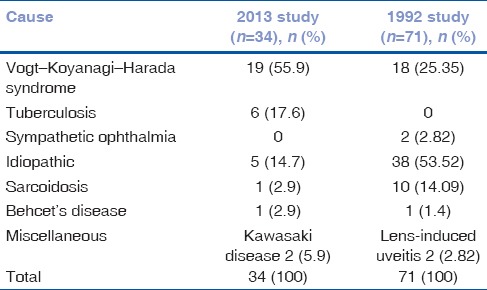
Lesser idiopathic cases were seen in the present study as compared to previously study. TB was an important cause of panuveitis in contrast to sarcoidosis seen previously. A case of panuveitis with HLA-B27 positivity was seen. Cases of Behcet's disease and sympathetic ophthalmia were comparable with the past result.
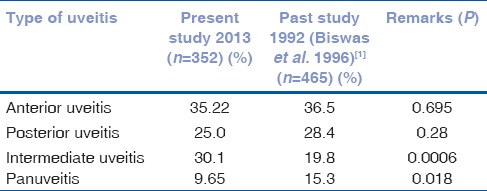
The comparative findings between the present study (352 uveitic cases) and past study (465 uveitic cases) are shown in [Table 6]. A significant difference was noted in the occurrence of intermediate uveitis (P = 0.0006) and panuveitis (P = 0.018)compared to the past study.
Table 6.
Comparison of present study in 2013 with similar past study in 1992
Among cases of idiopathic anterior uveitis, HLA-B27 positivity was identified more frequently (30%) than in the past (14.5%) (P< 0.05). Percentage of proven tubercular anterior uveitis has risen in the present study (P< 0.05).
The past study did not provide any details of intermediate uveitis, so the comparison of the intermediate uveitis pattern of the present study with the past study was not possible. Among posterior uveitis, the specific diagnosis could be reached in a larger number of cases than seen previously (idiopathic 11.36% at present vs. 43.94% seen previously P < 0.05). The cases of viral retinitis have significantly increased to 6.81% from 0.76%; P < 0.05.
The most common cause of panuveitis was VKH syndrome in both studies. At present, TB was identified an important cause of panuveitis in contrast to sarcoidosis in the past previously. However, the cases of Behcet's disease and sympathetic ophthalmia were comparable.
The global pattern of uveitis varies according to the demography and ethnicity. Anterior uveitis is the most common type of uveitis in any part of Asia. However, for the second-most common type, there is variation between intermediate uveitis, posterior uveitis, or panuveitis according to the different region studied.[5] The gender-wise difference in prevalence of uveitis was also noted in some part of Asia.
Discussion
With the advent of newer diagnostic tools, change in lifestyle, change in the pattern of infectious diseases, the pattern of uveitis is changing. The periodic analysis of these variations in the epidemiology of uveitis patterns is essential for comparison of treatment practices, management, prognosis, and complications of uveitis. With time and generation, the causes can also change, so we aimed to compare the scenario of uveitis over the past two decades.
Epidemiologic knowledge is important to guide clinicians in their consideration of differential diagnoses and clinical investigations.[7] Changing pattern of any disease in a subset of the population is an important health indicator.[8] There are lots of similar reports from different parts of India and world.[1,3,4,5,8,9,10] The necessities of these reports are to increase the awareness of regional variation in disease configuration which is an important health predictor in the epidemiological study.
This study compared the demographic profile and pattern between the new uveitis patients of 1992 and 2013 examined by a single uveitis specialist. No significant difference was observed in the incidence of new uveitic cases (1.04% vs. 1.8% of the past study). However, gender wise, there was a significant decline in male preponderance from 64% to 56% (P = 0.0187). The most common anatomical type is still anterior uveitis in both studies, but the second-most common type of uveitis was intermediate uveitis (P = 0.0006) instead of posterior uveitis in the past scenario.
For a sizable proportion of patients, the cause of uveitis remains unknown despite the appropriate investigation, regardless of age, gender, or anatomical location.[5] In general, anterior and intermediate uveitis is more often idiopathic than are posterior and diffuse forms of inflammation, and uveitis tends more often to be idiopathic in women as compared to men.[5] This holds true in our present study too. However, a sharp and significant decline in the idiopathic cause of uveitis from 58.7% in the past to 33.8% present study (P ≤ 0.0001) was observed. The identification of the cause of uveitis at present is contributed by the better diagnostic imaging technique and improved laboratory facilities such as polymerase chain reaction (PCR). There is an overall trend towards recognition of uveitis etiologies and a decrease in the incidence of idiopathic cases. Other factors that have led to improved diagnostic abilities include increased availability of nucleic acid amplification techniques, and better radiologic imaging modalities, such as high-resolution computerized tomography.[3] Also attributed to better classification of the disease (such as ocular TB, sarcoidosis, Behcet's disease, juvenile idiopathic arthritis, and among others)[11,12,13,14] and improvement in the diagnostic modalities.[3]
A significant change in the HLA-B27-associated idiopathic acute anterior uveitis was seen in the present study and past study (30% vs. 14.5%; P < 0.05). TB is an endemic disease of India. TB was the proven etiological cause of uveitis was identified in overall 22.5% of which 17 cases were of anterior uveitis cases (4.8%), 25 intermediate uveitis cases (7.1%), 31 posterior uveitis cases (8.8%), and 6 panuveitis cases (1.8%). The prevalence of TB in the present era is significantly increased (22.5% vs. 0.64%, P ≤ 0.0001). This may be due to the ability to detect the mycobacterium from the ocular fluid using real-time and nested PCR analysis in the present context. In contrast to toxoplasmosis uveitis seen earlier (8.6%), a declining trend in cases of toxoplasmosis (5.11%) was seen which was statistically significant (P = 0.0545). The decline in incidence may reflect the improvement in the food habit, sanitation and awareness of the disease.
As mentioned by BenEzra et al.[15] “pattern changes in uveitis diagnosis” in different uveitis is due to the cause for the variable incidence of specific uveitic etiologies reported in different studies. These pattern changes are because of a multitude of factors, including genetic, ethnic, geographic, and environmental factors in addition to “changing pattern of uveitis” over the years.[5,15]
Overall, the results of our study are comparable to the other studies.[8,16,17] However, Perkins and Folk[18] have correctly mentioned that there is the limitation of making valid comparisons between uveitis statistics of different countries, due to different diagnostic criterion and concept of etiopathogenesis. In such studies, limitations are bound to exist. Our study institute being a tertiary referral center, more patients with posterior uveitis and panuveitis could have been referred, and hence the total incidence quoted may not truly reflect the actual incidence in the population. Despite these limitations, our results still have the strength of being able to study the shifting paradigm of uveitis over the past two decades observed by the same uveitis specialist in the same set up in the same region. Hence, the results are consistent and reliable with no interpersonal variation.
Conclusion
We presume that the updates on the changing pattern of uveitis are of utmost importance for us to resume with the time because we must keep on moving to remain in the same position.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We extend our sincere gratitude to Dr. Deepak Edward from John Hopkins Institute for taking his efforts in editing this manuscript.
References
- 1.Biswas J, Narain S, Das D, Ganesh SK. Pattern of uveitis in a referral uveitis clinic in India. Int Ophthalmol. 1996;20:223–8. doi: 10.1007/BF00175264. [DOI] [PubMed] [Google Scholar]
- 2.Singh R, Gupta V, Gupta A. Pattern of uveitis in a referral eye clinic in North India. Indian J Ophthalmol. 2004;52:121–5. [PubMed] [Google Scholar]
- 3.Dogra M, Singh R, Agarwal A, Sharma A, Singh SR, Gautam N, et al. Epidemiology of uveitis in a tertiary-care referral institute in North India. Ocul Immunol Inflamm. 2017;25:S46–53. doi: 10.1080/09273948.2016.1255761. [DOI] [PubMed] [Google Scholar]
- 4.Das D, Bhattacharjee H, Bhattacharyya PK, Jain L, Panicker MJ, Das K, et al. Pattern of uveitis in North East India: A tertiary eye care center study. Indian J Ophthalmol. 2009;57:144–6. doi: 10.4103/0301-4738.45506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rathinam SR, Namperumalsamy P. Global variation and pattern changes in epidemiology of uveitis. Indian J Ophthalmol. 2007;55:173–83. doi: 10.4103/0301-4738.31936. [DOI] [PubMed] [Google Scholar]
- 6.Jabs DA, Nussenblatt RB, Rosenbaum JT Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol. 2005;140:509–16. doi: 10.1016/j.ajo.2005.03.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mi H, Ho SL, Lim WK, Wong EP, Teoh SC. Trends in patterns of intermediate uveitis in a tertiary institution in Singapore. PLoS One. 2014;9:e91533. doi: 10.1371/journal.pone.0091533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Das D, Bhattacharjee H, Das K, Tahiliani PS, Bhattacharyya P, Bharali G, et al. The changing patterns of uveitis in a tertiary institute of Northeast India. Indian J Ophthalmol. 2015;63:735–7. doi: 10.4103/0301-4738.170973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Venkatesh P, Gogia V, Shah B, Gupta S, Sagar P, Garg S, et al. Patterns of uveitis at the apex institute for eye care in India: Results from a prospectively enrolled patient data base (2011-2013) Int Ophthalmol. 2016;36:365–72. doi: 10.1007/s10792-015-0128-9. [DOI] [PubMed] [Google Scholar]
- 10.Henderly DE, Genstler AJ, Smith RE, Rao NA. Changing patterns of uveitis. Am J Ophthalmol. 1987;103:131–6. doi: 10.1016/s0002-9394(14)74217-5. [DOI] [PubMed] [Google Scholar]
- 11.Read RW, Holland GN, Rao NA, Tabbara KF, Ohno S, Arellanes-Garcia L, et al. Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: Report of an international committee on nomenclature. Am J Ophthalmol. 2001;131:647–52. doi: 10.1016/s0002-9394(01)00925-4. [DOI] [PubMed] [Google Scholar]
- 12.Herbort CP, Rao NA, Mochizuki M Members of Scientific Committee of First International Workshop on Ocular Sarcoidosis. International criteria for the diagnosis of ocular sarcoidosis: Results of the first international workshop on ocular sarcoidosis (IWOS) Ocul Immunol Inflamm. 2009;17:160–9. doi: 10.1080/09273940902818861. [DOI] [PubMed] [Google Scholar]
- 13.Criteria for diagnosis of Behçet's disease. International Study Group for Behçet's Disease. Lancet. 1990;335:1078–80. [PubMed] [Google Scholar]
- 14.Gupta V, Gupta A, Rao NA. Intraocular tuberculosis – an update. Surv Ophthalmol. 2007;52:561–87. doi: 10.1016/j.survophthal.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 15.BenEzra D, Cohen E, Maftzir G. Uveitis in children and adolescents. Br J Ophthalmol. 2005;89:444–8. doi: 10.1136/bjo.2004.050609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kianersi F, Mohammadi Z, Ghanbari H, Ghoreyshi SM, Karimzadeh H, Soheilian M, et al. Clinical patterns of uveitis in an Iranian tertiary eye-care center. Ocul Immunol Inflamm. 2015;23:278–82. doi: 10.3109/09273948.2014.902474. [DOI] [PubMed] [Google Scholar]
- 17.Siak J, Jansen A, Waduthantri S, Teoh CS, Jap A, Chee SP, et al. The pattern of uveitis among Chinese, Malays, and Indians in Singapore. Ocul Immunol Inflamm. 2017;25:S81–93. doi: 10.1080/09273948.2016.1188968. [DOI] [PubMed] [Google Scholar]
- 18.Perkins ES, Folk J. Uveitis in London and Iowa. Ophthalmologica. 1984;189:36–40. doi: 10.1159/000309382. [DOI] [PubMed] [Google Scholar]


