Abstract
A 36-year-old immunocompetent man developed endogenous endophthalmitis 1 week after intravenous fluid infusion in a rural setting. Large submacular abscess with posterior hypopyon warranted urgent vitrectomy which revealed Aspergillus terreus on fungal culture. Intravitreal and oral antifungals lead to resolution of inflammation with satisfactory anatomic outcome but poor visual outcome due to submacular scar.
Keywords: Aspergillus terreus, endogenous endophthalmitis, posterior hypopyon
Endophthalmitis is defined as intraocular infection affecting the inner coats of the eye with inflammation of the vitreous.[1] The spread of infection may be from an external source, such as after trauma or surgery. These cases fall under the category of exogenous endophthalmitis. Hematogenous spread of infection from a distant foci is categorized as endogenous endophthalmitis (EE).[2] Aspergillus terreus fungal EE has been reported in immunodeficient individuals but has never been reported after presumably contaminated intravenous fluid infusion in an immunocompetent individual.[3]
Case Report
A 36-year-old nondiabetic, immunocompetent male presented to us with a history of sudden onset, progressive, and painful diminution of vision in the right eye (RE) associated with redness for 4 days. He gave a history of fever with vomiting 1 week prior, for which he was hospitalized and received intravenous maintenance fluids along with antibiotics at a rural primary health-care facility.
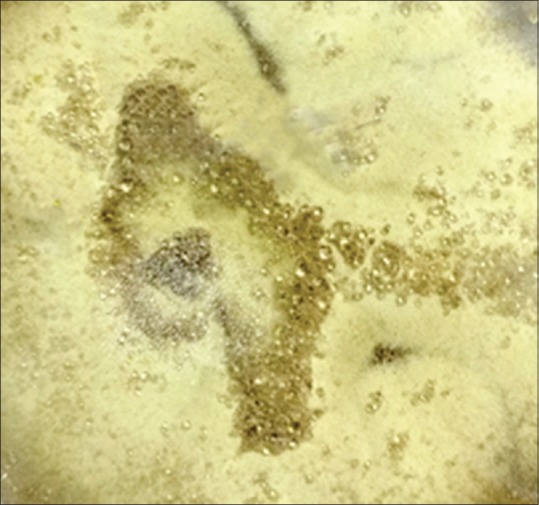
On examination, the best corrected visual acuity (BCVA) in his RE was light perception with accurate projection of rays and 6/6 in his left eye (LE). Anterior Segment examination of the RE revealed circumcorneal congestion, clear cornea, a 3 mm yellowish white hypopyon with fibrin in the pupillary area and a clear crystalline lens. Fundus examination of RE revealed a Media clarity of Grade 2, 3+ vitreous cells and crescentic creamy yellow exudates inferior to the inferior arcade, suggestive of posterior hypopyon. A 4 disc diameter (DD), yellowish subretinal lesion in the macula with plastered creamy yellow exudates all over the posterior pole was seen [Fig. 1], suggestive of submacular abscess with intense overlying vitreous inflammation. Examination of the LE was essentially normal.
Figure 1.

Wide field Optomap fundus image of right eye at presentation showing Media clarity Grade 2, yellowish crescentic preretinal exudates below the inferior arcade suggestive of posterior hypopyon and a 3–4 DD submacular abscess in the posterior pole
A clinical diagnosis of RE contaminated infusion fluid induced EE was made. The patient was admitted, and he underwent 23 G pars plana vitrectomy (PPV) the same day. Systemic investigations including hemogram, liver function tests, renal function tests, and blood and urine cultures were unremarkable. Enzyme-linked immunosorbent assay (ELISA) for HIV was nonreactive. Undiluted vitreous samples were sent for Gram stain, potassium hydroxide (KOH) mount, bacterial and fungal cultures. Intraoperatively, vitreous exudates were fluffy and dry looking. Once posterior hyaloid was detached during PPV, exudates plastered all over the posterior pole and those trapped in the subhyaloid space were freed into the vitreous cavity. A submacular abscess of 4 DD with surrounding retinal whitening was noted. Suspecting fungal endophthalmitis, at the end of PPV intravitreal vancomycin (1 mg/0.1 ml), ceftazidime (2.25 mg/0.1 ml), Amphotericin B (5 mcg/0.1 ml), and dexamethasone (0.4 mg/0.1 ml) were injected.
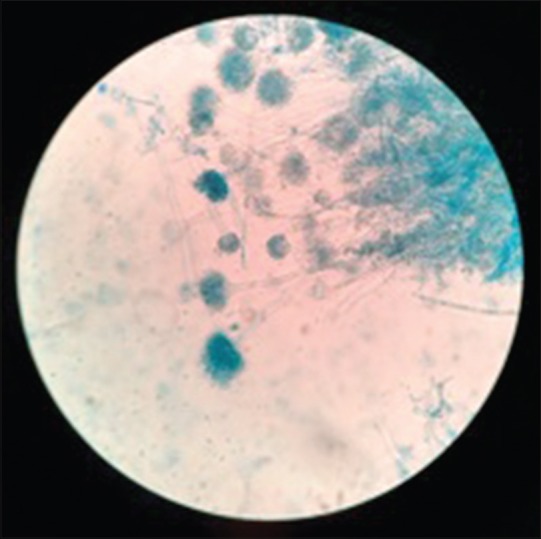
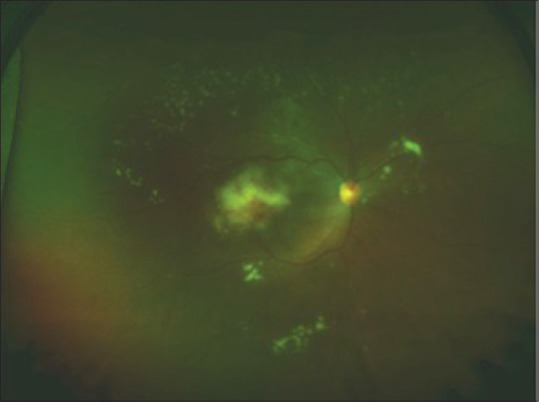
Wet mount microscopy with 10% KOH showed filamentous, septate, and acute-angled branching hyphae. Fungal culture on Sabouraud's Dextrose Agar revealed velvety cinnamon brown colonies [Fig. 2] and wet mount preparation from the culture plate showed compact, biseriate, smooth walled conidiophores consistent with the morphology of Aspergillus terreus [Fig. 3]. Aspergillus terreus was reported to be sensitive to both Amphotericin B and voriconazole. Oral Voriconazole 200 mg twice a day was started along with topical moxifloxacin (0.5%), prednisolone (1%), and atropine (1%).
Figure 2.
Sabouraud's Dextrose agar culture plate showing characteristic cinnamon brown colored colonies, suggestive of Aspergillus terreus
Figure 3.
Wet mount preparation from growth on culture plate showing septate hyphae with characteristic conidiophores consistent with Aspergillus terreus morphology
The patient received an additional injection of Intravitreal Amphotericin B (5 mcg/0.1 ml) and Dexamethasone (0.4 mg/0.1 ml) on postoperative day 3, for persistent vitreous exudates. As the media clarity improved and vitreous inflammation decreased following the second intravitreal injection, repeat intravitreal injection of Amphotericin B and Dexamethasone was injected, 6 days later. 3 weeks after PPV, media clarity improved to Grade 1 along with decrease in vitreous inflammation and disappearance of posterior hypopyon. At final follow-up visit at 3 months, the BCVA in the RE was counting fingers at 1feet with a clear cornea, quiet anterior chamber, and media clarity Grade 1. Oral voriconazole was stopped after 3 months. A vascularized, well-defined 3–4 DD submacular scar was visible in the posterior pole [Fig. 4].
Figure 4.
Wide field Optomap fundus image of the right eye 3 months after pars plana vitrectomy showing Media clarity of Grade 1 with submacular scar in the posterior pole
Discussion
Endophthalmitis due to Aspergillus species has been reported in immunocompromised individuals, intravenous drug abusers, posttrauma and postsurgery.[1,2,4] EE due to Aspergillus is commonly caused by Aspergillus flavus and Aspergillus niger and is the second most common cause of fungal EE after Candida endophthalmitis.[2] Aspergillus terreus is considered to be a laboratory contaminant owing to its ubiquitous presence in soil.[3] A total of eight culture positive cases of EE due to Aspergillus terreus have been reported till date, six of them in immunocompromised individuals.[3,5] Two case reports of Aspergillus terreus EE in immunocompetent patients by Ng et al.[5] and Panigrahi et al.[3] exist in literature. Both these cases developed EE secondary to bronchiectasis and gastroenteritis, respectively. Development of fungal EE due to Aspergillus flavus, Aspergillus niger, and Candida species has been reported after administration of a single contaminated infusion fluid bottle.[6] However, to the best of our knowledge, Aspergillus terreus EE has not been reported after administration of presumably contaminated intravenous infusion in an immunocompetent patient.
Systemic and intravitreal antifungal agents with urgent vitrectomy are the mainstays of treatment.[1,2] Amphotericin B and voriconazole are antifungals of choice for treating infections caused by filamentous fungi, with voriconazole having superior outcomes in Aspergillus terreus endophthalmitis.[7] In our patient, satisfactory anatomic outcome was achieved with urgent PPV, intravitreal Amphotericin B, and oral voriconazole. However, the functional outcome remained poor due to macular scarring. This is in conjunction with previously reported cases of Aspergillus EE.[3,8]
Conclusion
Aspergillus terreus EE can develop in immunocompetent individuals following contaminated intravenous fluid infusion. Pars plana vitrectomy with intravitreal Amphotericin B and oral voriconazole are effective in management.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sadiq MA, Hassan M, Agarwal A, Sarwar S, Toufeeq S, Soliman MK, et al. Endogenous endophthalmitis: Diagnosis, management, and prognosis. J Ophthalmic Inflamm Infect. 2015;5:32. doi: 10.1186/s12348-015-0063-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lingappan A, Wykoff CC, Albini TA, Miller D, Pathengay A, Davis JL, et al. Endogenous fungal endophthalmitis: Causative organisms, management strategies, and visual acuity outcomes. Am J Ophthalmol. 2012;153:162–60. doi: 10.1016/j.ajo.2011.06.020. [DOI] [PubMed] [Google Scholar]
- 3.Panigrahi PK, Roy R, Pal SS, Mukherjee A, Lobo A. Aspergillus terreus endogenous endophthalmitis: Report of a case and review of literature. Indian J Ophthalmol. 2014;62:887–9. doi: 10.4103/0301-4738.141065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Das T, Vyas P, Sharma S. Aspergillus terreus postoperative endophthalmitis. Br J Ophthalmol. 1993;77:386–7. doi: 10.1136/bjo.77.6.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ng J, Ho S, Krishnan P, Teoh SC. Aspergillus terreus endogenous endophthalmitis in a nonimmunocompromised patient with a history of bronchiectasis. Ocul Immunol Inflamm. 2013;21:231–3. doi: 10.3109/09273948.2012.754907. [DOI] [PubMed] [Google Scholar]
- 6.Gupta A, Gupta V, Dogra MR, Chakrabarti A, Ray P, Ram J, et al. Fungal endophthalmitis after a single intravenous administration of presumably contaminated dextrose infusion fluid. Retina. 2000;20:262–8. [PubMed] [Google Scholar]
- 7.Kramer M, Kramer MR, Blau H, Bishara J, Axer-Siegel R, Weinberger D, et al. Intravitreal voriconazole for the treatment of endogenous Aspergillus endophthalmitis. Ophthalmology. 2006;113:1184–6. doi: 10.1016/j.ophtha.2006.01.059. [DOI] [PubMed] [Google Scholar]
- 8.Riddell Iv J, McNeil SA, Johnson TM, Bradley SF, Kazanjian PH, Kauffman CA, et al. Endogenous Aspergillus endophthalmitis: Report of 3 cases and review of the literature. Medicine (Baltimore) 2002;81:311–20. doi: 10.1097/00005792-200207000-00007. [DOI] [PubMed] [Google Scholar]


