Sir,
We read with great interest the review by Abdelfattah Ahmed Touman et al.,[1] recently published in your journal, focused on the correct management of gaining access to the periphery of the lung. Their statements are sound and easily transferable to clinical practice.
However, according to us, the authors should have better highlighted the complementary roles of bronchoscopic, computed tomography, and ultrasound guidance for lung biopsies.
The authors only mentioned the opportunity to perform transthoracic US (TUS)-guided biopsies. It is mandatory to underline that TUS has to be considered a valuable tool in detecting even small lesions adherent to the pleural surface.[2]
The low complications rate is not only due to the correct patients' selection, as highlighted in the paper,[1] but also to the correct technique, the use of an atraumatic semi-automatic needle (20-gauge) and a dedicated probe.[2]
The procedure-related complications with TUS guidance are less frequent than reported in the review.[1] It has been already published that in 856 fine-needle aspiration biopsy (FNAB) performed, only four patients had a self-limiting pneumothorax (0.4%), and no major complications have been reported.[3]
In another case series,[4] in 95 TUS-guided FNAB, there was no pneumothorax or hemorrhagic pleural effusion.
It is advisable the use of a dedicated probe, that is, with a central hole through which the needle set is introduced.[4] This is still the most suitable and reliable approach for these purposes because the needle is visible in real time during the biopsy. Transducers with “parallel” needle guidance allow only oblique access, with the needle angulated versus the US beam, causing some uncertainty of localization.
Under TUS guidance, it is also possible to choose the right needle size, generally an atraumatic 20-gauge. The technique used is called “modified Menghini.” It consists of a needle with stylet connected to a syringe plunger; the needle tip is Menghini type, whereas the stylet tip is pyramidal. This provides specimens suitable for histologic diagnosis and minimizes the occurrence of complications, which appear to be more frequent with 18-gauge needles[1] [Figure 1].
Figure 1.
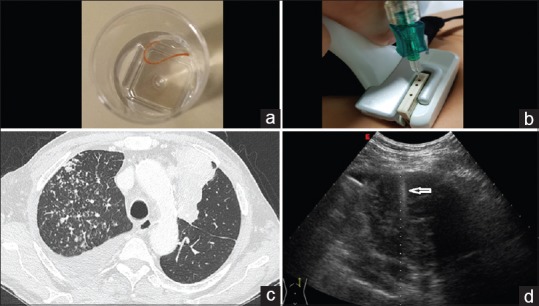
A sufficient sample (a) for histological and molecular analysis is obtained using a dedicated probe (b) with a semi-automated modified Menghini type needle from an anterior subpleural lesion (c) this method allows real-time visualization of the needle (d)
Moreover, TUS guidance allows to perform biopsies even at the bedside; this could be useful in patients with low-performance status.
In conclusion, TUS-guided FNAB should be the “ first choice” as a diagnostic procedure in pleural and adherent to pleura pulmonary lesions.[5]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Touman AA, Vitsas VV, Koulouris NG, Stratakos GK. Gaining access to the periphery of the lung: Bronchoscopic and transthoracic approaches. Ann Thorac Med. 2017;12:162–70. doi: 10.4103/atm.ATM_416_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sperandeo M, Rotondo A, Guglielmi G, Catalano D, Feragalli B, Trovato GM, et al. Transthoracic ultrasound in the assessment of pleural and pulmonary diseases: Use and limitations. Radiol Med. 2014;119:729–40. doi: 10.1007/s11547-014-0385-0. [DOI] [PubMed] [Google Scholar]
- 3.Sperandeo M, Dimitri L, Pirri C, Trovato FM, Catalano D, Trovato GM, et al. Advantages of thoracic ultrasound-guided fine-needle aspiration biopsy in lung cancer and mesothelioma. Chest. 2014;146:e178–9. doi: 10.1378/chest.14-1557. [DOI] [PubMed] [Google Scholar]
- 4.Sperandeo M, Trovato FM, Dimitri L, Catalano D, Simeone A, Martines GF, et al. Lung transthoracic ultrasound elastography imaging and guided biopsies of subpleural cancer: A preliminary report. Acta Radiol. 2015;56:798–805. doi: 10.1177/0284185114538424. [DOI] [PubMed] [Google Scholar]
- 5.Tinti MG, Frongillo E, Sperandeo M. Role of pleural transthoracic ultrasound guidance. Ann Thorac Med. 2017;12:216–7. doi: 10.4103/atm.ATM_77_17. [DOI] [PMC free article] [PubMed] [Google Scholar]


