Abstract
INTRODUCTION:
Treatment-emergent central sleep apnea (TECSA) is observed in some patients when they are treated with positive airway pressure (PAP) after significant resolution of the preexisting obstructive events in patients with obstructive sleep apnea. The objective of this study was to systematically review the literature for studies describing the natural history of TECSA.
METHODS:
PubMed, Medline, Scopus, Web of Science, and Cochran Library databases were searched through June 29, 2017.
RESULTS:
Five studies were identified that discussed the natural history of TECSA. TECSA developed in 3.5%–19.8% of PAP-treated patients. Treatment-persistent central sleep apnea (TPCSA), representing protracted periods of PAP therapy-related central apneas, was noted in 14.3%–46.2% of patients with TECSA. Delayed-TECSA (D-TECSA) represents an anomalous TECSA entity appearing weeks to months after initial PAP therapy. D-TECSA was observed in 0.7%–4.2% of OSA patients undergoing PAP treatment (after at least 1 month). In patients with TECSA, a higher apnea–hypopnea index (AHI) and central apnea index at their baseline study or a higher residual AHI at their titration study may be associated with an increased likelihood of conversion to TPCSA.
CONCLUSIONS:
Overall, TECSA developed in 3.5%–19.8% of PAP-treated patients with OSA. The vast majority will experience complete resolution of central apneas over a few weeks to months. Unfortunately, about a third of patients with TECSA may continue to exhibit persistence of central sleep apnea on reevaluation. A small proportion may experience D-TECSA after few weeks to several months of initial exposure to PAP therapy.
Keywords: Apnea–hypopnea index, central sleep apnea, delayed-treatment-emergent central sleep apnea, obstructive sleep apnea, treatment-emergent central sleep apnea, treatment-persistent central sleep apnea
Treatment-emergent central sleep apnea (TECSA) is characterized by the emergence or persistence of central apneas while undergoing treatment for obstructive sleep apnea (OSA) such as while using positive airway pressure (PAP) therapy.[1] TECSA typically occurs following substantial resolution of previously witnessed obstructive respiratory events that were identified on a prior diagnostic sleep study or diagnostic portion of a split-night sleep study.[1] Previous studies have noted that the prevalence of TECSA varies between 3.5% and 20%.[2,3,4,5,6,7,8,9,10]
A recent systematic review on the prevalence of TECSA found that the aggregate point prevalence of TECSA is around 8% while the estimated range varies from 5% to 20% in patients with untreated OSA.[11] It has been postulated that in a patient with ventilatory instability, continuous positive airway pressure (CPAP) therapy can intermittently lower the partial pressure of arterial carbon dioxide (PaCO2) below the apneic threshold leading to the development of central apneas and this serves as a possible explanation for TECSA.[12] This happens more commonly during nonrapid eye movement sleep when the CO2 reserve (the difference between eupneic PaCO2 and the apneic threshold) is highly labile.[12]
Most of the patients with TECSA show gradual resolution of central apneas over weeks to months. However, some patients appear to experience central apneas for protracted periods of time. For these patients, CPAP use may be associated with dyspnea or air hunger as well as inadvertent CPAP mask removal during the night.[13] All this can lead to persistence or worsening of sleep-disordered breathing as well as poor sleep quality at night. To the best of our knowledge, the natural history of TECSA has not been evaluated with a systematic review. We would like to delineate any characteristics of a patient population exhibiting central sleep apnea over a protracted period after the initial PAP titration study (i.e., patients with treatment persistent central sleep apnea [TPCSA]). Therefore, the primary objective of this study was to identify patients with TECSA who continue to experience PAP treatment-related central apneas, weeks to months after initiating CPAP therapy (i.e., patients with persistent refractory central sleep apnea or TPCSA). Secondary objectives included (1) the prevalence of TPCSA if such patients do exist, (2) factors that determine the prevalence of TPCSA, and (3) patients who may exhibit delayed-TECSA (D-TECSA).
Methods
For purposes of clarification, we used the following terminologies:
PAP-1: First PAP treatment data (titration or titration portion of the split-night study or PAP device data for the first time period) that were used to determine the prevalence of TECSA.
PAP-2: Second PAP treatment data (titration or the in-lab CPAP study at patient's “home” CPAP setting or PAP device data for the second time period) done weeks to months after PAP-1 on patients with TECSA that were used to determine the prevalence of TPCSA. Alternatively, PAP-2 treatment data could also be used to evaluate for D-TECSA.
Treatment-emergent central sleep apnea
TECSA refers to the patients with OSA (with or without concomitant central sleep apnea) that on initial PAP treatment demonstrated central apnea index (CAI) of 5 or higher and/or demonstrated Cheyne–Stokes breathing that became prominent and disruptive.
Treatment-persistent central sleep apnea
TPCSA refers to patients with OSA (with or without concomitant central sleep apnea) that demonstrated TECSA on initial PAP treatment and then redemonstrated central sleep apnea when evaluating the second PAP treatment data.
Delayed-treatment-emergent central sleep apnea
These are patients with OSA (with or without concomitant central sleep apnea) that did not demonstrate TECSA on initial PAP treatment but then insidiously demonstrated central sleep apnea when evaluating the second PAP treatment data.
Two authors (GN and MR) conducted a systematic search of electronic databases that included PubMed, Medline, Scopus, Web of Science, and Cochrane Library from inception through June 29, 2017. The search included MeSH terms, keywords, and phrases in various combinations. The reference lists of relevant articles were further reviewed to identify other pertinent articles. Extensive grey literature and Google Scholar searches were completed to identify relevant publications that may have been missed during the electronic database search. No language limits were imposed at the time of screening of relevant articles. Randomized controlled trials, case–control studies, cohort studies, and case series were included. The investigators independently performed data extraction using a standard data extraction form to determine the eligibility for inclusion.
The following is an example of a PubMed/MEDLINE search strategy: ([“Sleep Apnea, Central” (Mesh)] AND [(treatment-emergent) OR (“treatment emergent”) OR (complex)]). All articles which discussed findings for initial and persistent central sleep apnea in patients with PAP treatment data were reviewed. Articles meeting the inclusion criteria were included in the systematic review.
Inclusion criteria were (1) all studies that included subjects with a new or established diagnosis of TECSA and (2) studies in which patients with TECSA were discretely evaluated at least at two distinct points in time and the data collected were made available. Exclusion criteria were (1) studies that did not define what constituted central sleep apnea, (2) studies that did not utilize PAP therapy to arrive at their determined rates of TECSA, and (3) studies that did not have at least two points in time with data available for evaluation.
Results
Based on the methodology, established inclusion, and exclusion criteria, five studies met criteria for detailed evaluation [Figure 1].[6,7,8,9,10] The demographic data and the PAP treatment data for these five studies are presented in Tables 1 and 2, respectively. The five studies included one prospective observational, one cross-sectional, and three retrospective observational studies. Four studies conducted titration studies and one study queried a telemonitoring database to establish the prevalence and persistence of TECSA. All studies except the one done by Dernaika et al. allowed inclusion of patients demonstrating central sleep apnea (i.e., CAI >5 events/h) at baseline for the PAP-1 study. Once the prevalence of TECSA was established, all five studies followed the patients with TECSA through a repeat PAP study to evaluate for the existence of TPCSA and to establish its prevalence. The average age for the patients with TECSA varied between 53 and 65 years and most patients were obese with a body mass index (BMI) ranging between 32 and 37 kg/m2. Overall, there were 135,283 OSA patients who were sampled, and 4823 patients had some sort of treatment-related central sleep apnea (either transient, delayed emergent, or persistent central sleep). The studies reported the prevalence of TECSA to be between 3.5% and 19.8% of PAP-treated patients. Of 3832 patients with TECSA on PAP-1 that returned for PAP-2, 1193 continued to exhibit the presence of central sleep apnea giving a cumulative aggregate TPCSA point prevalence of 31.1% among patients with TECSA; the TPCSA range varied between 14.3% and 46.2% among TECSA patients. Even when the study by Liu et al. is excluded, given this study did not conduct in-lab sleep studies to calculate TECSA and TPCSA estimates, the cumulative aggregate TPCSA point prevalence remains 25.1% in patients with TECSA. The review also found that between 0.7-4.2% patients with OSA do not develop TECSA spontaneously on their initial PAP study, but demonstrate a somewhat delayed emergence of central sleep apnea (called D-TECSA) at their subsequent PAP study.
Figure 1.
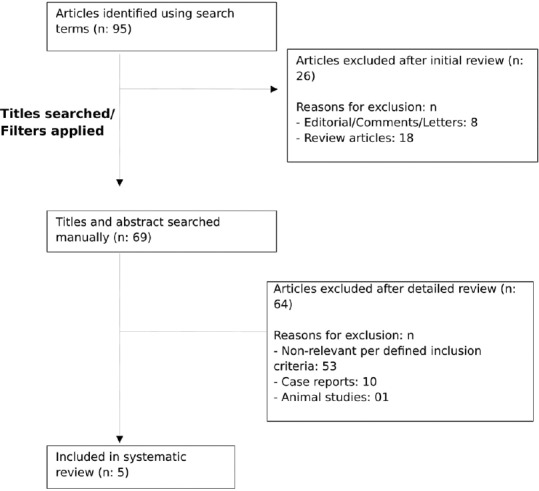
Literature search methodology for studying natural history of treatment-emergent central sleep apnea
Table 1.
Demographic characteristics for patients with treatment-emergent central sleep apnea and delayed-treatment emergent central sleep apnea
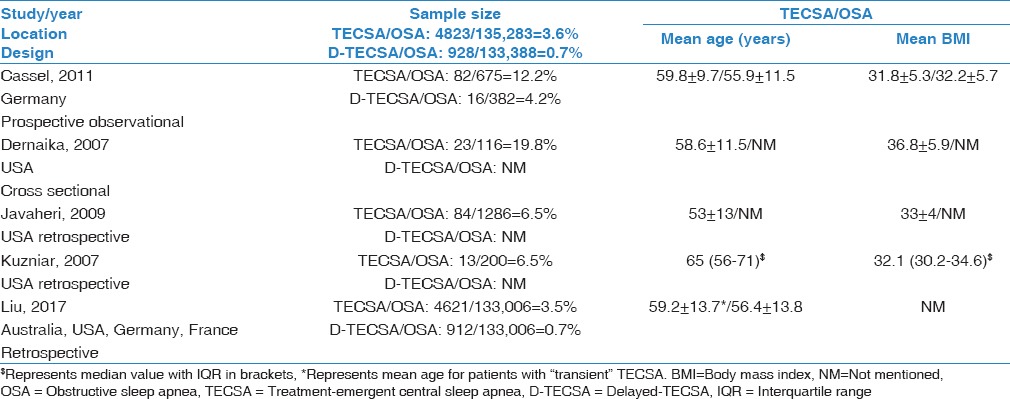
Table 2.
Polysomnographic characteristics for patients with treatment-emergent central sleep apnea and treatment-persistent central sleep apnea
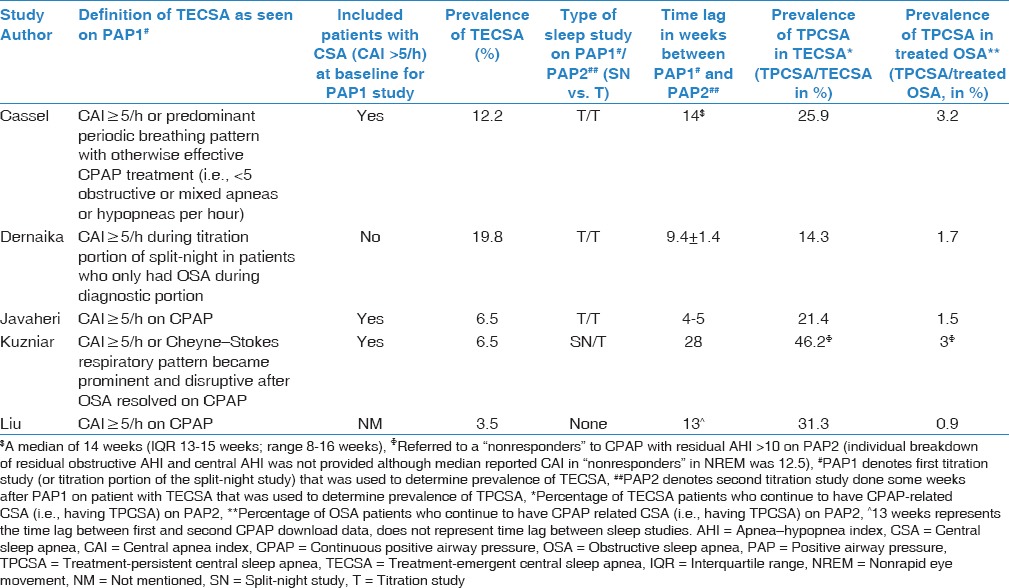
All the studies used in-lab full-night titration to establish prevalence of TECSA, except Kuzniar et al., who used the titration portion of a split-night study, and Liu et al., who used a telemonitoring database (AirView; ResMed). The prevalence of TECSA in these five studies ranged from 3.5% (Liu et al.) to 19.8% (Dernaika et al.). The study with the largest sample size (in terms of the number of patients with OSA) was the study by Liu et al. with 133,006 patients and the one with the smallest sample size was done by Dernaika et al. with 116 patients. The time period between PAP-1 and PAP-2 varied between 4 and 5 weeks in the study by Javaheri et al. to approximately 28 weeks in the study by Kuzniar et al.
Discussion
The typical course of TECSA appears variable [Figure 2]. The majority of patients with TECSA show resolution of central apneas over a few weeks to months. Although most cases of TECSA resolve over time, about one-third of such patients convert to TPCSA related to PAP therapy. Our systematic review noted that 0.9%–3.2% of all patients treated with PAP therapy for OSA will exhibit TPCSA on a long-term basis [Table 2]. They represent 14.3%–46.2% of TECSA patients, who continue to experience PAP therapy-related central sleep apnea over a protracted period after they were first diagnosed with TECSA. Javaheri et al. noted that the daily CPAP adherence tends to be lower in patients who eventually declare themselves as TPCSA on PAP-2 compared to patients who experience resolution of their TECSA.
Figure 2.
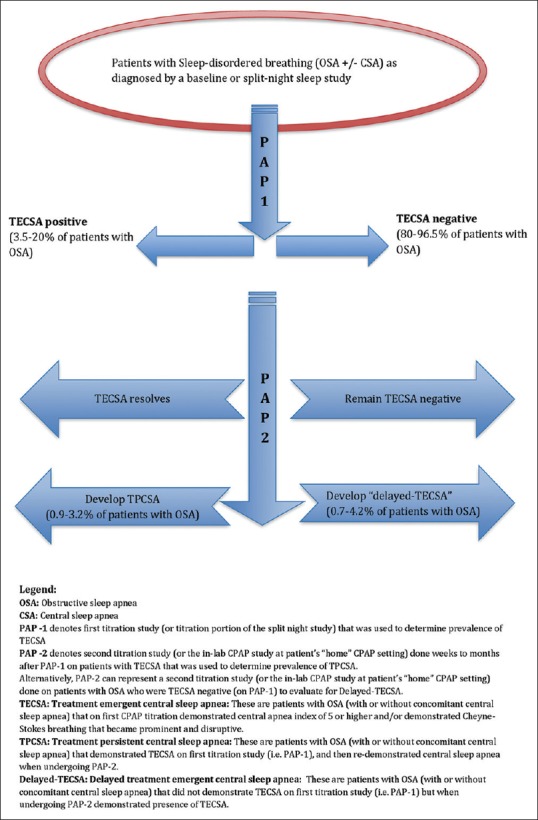
Schematic diagram showing natural history of treatment-emergent central sleep apnea
The prevalence of TPCSA at 0.9%–3% in all patients with treated OSA may be an underrepresentation given some patients in the discussed studies were lost to follow-up after the first titration study. Cassel et al. reported a TPCSA prevalence of 3.2%, which was the highest of the five studies evaluating this phenomenon. Even this TPCSA prevalence figure could be an underestimation, as 28 out of the 82 patients with TECSA at PAP-1 were lost to follow-up and hence unavailable to undergo a PAP-2 study. Similarly, in the study by Dernaika et al. which reported the TPCSA prevalence at 1.7%, it was noted that seven out of 21 patients with TECSA at PAP-1 were lost to follow-up and also unavailable for a PAP-2 study. Selective exclusion of patients with preexisting central sleep apnea from the titration study (as performed by Dernaika et al.) can also lead to underestimation of overall prevalence.
Cassel et al. noted a distinct group of patients with OSA that did not demonstrate a CAI >5 on their first full-night PAP titration (i.e., initially TECSA negative) but when retested 3 months later developed CAI >5 (i.e., subsequently TECSA positive). Similarly, Liu et al. found that 912 patients who did not have TECSA on initial PAP treatment data demonstrated treatment-related central sleep apnea on the second PAP treatment data and this represented 0.7% of the total PAP treatment data sample. This entity can be best described as experiencing “D-TECSA” and has prevalence between 0.7% and 4.2% in patients undergoing PAP treatment after at least 1 month. It appears that TECSA lies within a dynamic spectrum between sleep apnea without TECSA at one end to TPCSA at the other end with multiple intermediate polysomnographic variations in between (transient-TECSA, D-TECSA, and resolved-TECSA) [Figure 2].
One plausible explanation for the dynamic nature of TECSA could be that the CO2 reservoir and the apnea threshold for the same patient are labile as a direct consequence of preexisting comorbidities, emergence of additional new comorbidities, changes in BMI and as a response to continued/intermittent PAP usage. This view is supported by experiments that have demonstrated that the magnitude of reduction in PaCO2 below eupneic PaCO2 and the transient increase in alveolar ventilation required to attain the apneic threshold is not a constant value.[14] This variability in the apneic threshold could lead to emergence, persistence, or resolution of central apneas on PAP therapy depending on the degree of adaptation of chemoreceptors to the fluctuating CO2 reservoir and the apneic threshold.
It appears that certain polysomnographic features specific to the individual patient with TECSA could be associated with higher chances of developing TPCSA independent of a time variable. Javaheri et al. noted that TECSA patients, who demonstrated TPCSA on subsequent PAP-2 titration when compared to those who showed resolution of TECSA, were more likely to have CAI of 5 or greater on their baseline study. The patients in the TPCSA group had higher baseline apnea–hypopnea index (AHI) and higher residual AHI at PAP-1 and PAP-2 when compared to those who showed resolution of TECSA (Javaheri et al.). It is possible that TECSA patients with higher AHI and CAI at their baseline study as well as higher residual AHI, higher arousal index, lower total sleep time, and lower sleep efficiency at their titration studies predict higher chances of converting to TPCSA in the long run, but more robust data are required before such claims can be made conclusively.
Limitations
Our review has certain limitations. Only five studies were available for review limiting heterogeneity, sample size, and statistical power of the study. Three of the five studies were retrospective observational studies and had the same limitations as that of any retrospective study. The sample sizes for patients with TECSA undergoing PAP-2 study were generally smaller than those undergoing the PAP-1 study. The study by Liu et al. enrolling the largest number of OSA patients derived TECSA, D-TECSA, and TPCSA data based on CPAP machine download algorithms. Such data might not be consistent with central sleep apnea index determined by in-lab CPAP studies. Given the overwhelmingly large sample size of their study, their results to some extent might have skewed the final conclusions drawn from this systematic review. All studies reported a substantial number of patients with TECSA that were lost to follow-up between PAP-1 and PAP-2 which further limits the accuracy of estimation of TPCSA prevalence. Further, it is unknown if patients developed any new risk factors (heart failure, stroke, or use of opiate medications) between PAP-1 and PAP-2 studies that could have increased the estimated prevalence of TPCSA. Large-scale, prospective, well-designed studies will be required in the future to better understand the prevalence of TPCSA in patients diagnosed with TECSA during their first PAP titration study.
Conclusions
Overall, TECSA developed in 3.5%–19.8% of PAP-treated patients. About two-thirds of patients with TECSA on initial PAP exposure go on to experience complete resolution of central apneas over a period of few weeks to several months. However, a significant proportion demonstrating TECSA on initial PAP exposure may continue to exhibit TPCSA or persistence of central apneas on reevaluation. D-TECSA was observed in between 0.7% and 4.2% of patients undergoing PAP treatment after at least 1 month. In patients with TECSA, a higher AHI and CAI at their baseline study as well as a higher residual AHI at their titration study may be associated with increased likelihood of conversion to TPCSA in the long run. Given their unfavorable polysomnographic profile, patients with TPCSA may have poor adherence to PAP therapy and may need to be monitored closely. Future studies should consider enrolling higher number of patients with TECSA to better delineate the prevalence and risk factors associated with conversion to TPCSA.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.ICSD-3 Online Version – American Academy of Sleep Medicine (AASM) [Last accessed on 2015 Mar 30]. Available from: http://www.aasmnet.org/store/product.aspx?pid=849 .
- 2.Endo Y, Suzuki M, Inoue Y, Sato M, Namba K, Hasegawa M, et al. Prevalence of complex sleep apnea among Japanese patients with sleep apnea syndrome. Tohoku J Exp Med. 2008;215:349–54. doi: 10.1620/tjem.215.349. [DOI] [PubMed] [Google Scholar]
- 3.Lehman S, Antic NA, Thompson C, Catcheside PG, Mercer J, McEvoy RD, et al. Central sleep apnea on commencement of continuous positive airway pressure in patients with a primary diagnosis of obstructive sleep apnea-hypopnea. J Clin Sleep Med. 2007;3:462–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Morgenthaler TI, Kagramanov V, Hanak V, Decker PA. Complex sleep apnea syndrome: Is it a unique clinical syndrome? Sleep. 2006;29:1203–9. doi: 10.1093/sleep/29.9.1203. [DOI] [PubMed] [Google Scholar]
- 5.Yaegashi H, Fujimoto K, Abe H, Orii K, Eda S, Kubo K, et al. Characteristics of Japanese patients with complex sleep apnea syndrome: A retrospective comparison with obstructive sleep apnea syndrome. Intern Med. 2009;48:427–32. doi: 10.2169/internalmedicine.48.1459. [DOI] [PubMed] [Google Scholar]
- 6.Cassel W, Canisius S, Becker HF, Leistner S, Ploch T, Jerrentrup A, et al. A prospective polysomnographic study on the evolution of complex sleep apnoea. Eur Respir J. 2011;38:329–37. doi: 10.1183/09031936.00162009. [DOI] [PubMed] [Google Scholar]
- 7.Dernaika T, Tawk M, Nazir S, Younis W, Kinasewitz GT. The significance and outcome of continuous positive airway pressure-related central sleep apnea during split-night sleep studies. Chest. 2007;132:81–7. doi: 10.1378/chest.06-2562. [DOI] [PubMed] [Google Scholar]
- 8.Javaheri S, Smith J, Chung E. The prevalence and natural history of complex sleep apnea. J Clin Sleep Med. 2009;5:205–11. [PMC free article] [PubMed] [Google Scholar]
- 9.Kuzniar TJ, Pusalavidyasagar S, Gay PC, Morgenthaler TI. Natural course of complex sleep apnea – A retrospective study. Sleep Breath. 2008;12:135–9. doi: 10.1007/s11325-007-0140-z. [DOI] [PubMed] [Google Scholar]
- 10.Liu D, Armitstead J, Benjafield A, Shao S, Malhotra A, Cistulli PA, et al. Trajectories of emergent central sleep apnea during CPAP therapy. Chest. 2017;152:751–60. doi: 10.1016/j.chest.2017.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nigam G, Pathak C, Riaz M. A systematic review on prevalence and risk factors associated with treatment-emergent central sleep apnea. Ann Thorac Med. 2016;11:202–10. doi: 10.4103/1817-1737.185761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilmartin GS, Daly RW, Thomas RJ. Recognition and management of complex sleep-disordered breathing. Curr Opin Pulm Med. 2005;11:485–93. doi: 10.1097/01.mcp.0000183061.98665.b0. [DOI] [PubMed] [Google Scholar]
- 13.Pusalavidyasagar SS, Olson EJ, Gay PC, Morgenthaler TI. Treatment of complex sleep apnea syndrome: A retrospective comparative review. Sleep Med. 2006;7:474–9. doi: 10.1016/j.sleep.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Dempsey JA. Crossing the apnoeic threshold: Causes and consequences. Exp Physiol. 2005;90:13–24. doi: 10.1113/expphysiol.2004.028985. [DOI] [PubMed] [Google Scholar]


