Abstract
IMPORTANCE
Among high-risk patients with hypertension, targeting a systolic blood pressure of 120 mm Hg reduces cardiovascular morbidity and mortality compared with a higher target. However, intensive blood pressure management incurs additional costs from treatment and from adverse events.
OBJECTIVE
To evaluate the incremental cost-effectiveness of intensive blood pressure management compared with standard management.
DESIGN, SETTING, AND PARTICIPANTS
This cost-effectiveness analysis conducted from September 2015 to August 2016 used a Markov cohort model to estimate cost-effectiveness of intensive blood pressure management among 68-year-old high-risk adults with hypertension but not diabetes. We used the Systolic Blood Pressure Intervention Trial (SPRINT) to estimate treatment effects and adverse event rates. We used Centers for Disease Control and Prevention Life Tables to project age- and cause-specific mortality, calibrated to rates reported in SPRINT. We also used population-based observational data to model development of heart failure, myocardial infarction, stroke, and subsequent mortality. Costs were based on published sources, Medicare data, and the National Inpatient Sample.
INTERVENTIONS
Treatment of hypertension to a systolic blood pressure goal of 120 mm Hg (intensive management) or 140 mm Hg (standard management).
MAIN OUTCOMES AND MEASURES
Lifetime costs and quality-adjusted life-years (QALYs), discounted at 3% annually.
RESULTS
Standard management yielded 9.6 QALYs and accrued $155 261 in lifetime costs, while intensive management yielded 10.5 QALYs and accrued $176 584 in costs. Intensive blood pressure management cost $23 777 per QALY gained. In a sensitivity analysis, serious adverse events would need to occur at 3 times the rate observed in SPRINT and be 3 times more common in the intensive management arm to prefer standard management.
CONCLUSIONS AND RELEVANCE
Intensive blood pressure management is cost-effective at typical thresholds for value in health care and remains so even with substantially higher adverse event rates.
Hypertension is a common risk factor for cardiovascular disease, affecting nearly 2 in 3 older adults in the United States.1 Although treatment of hypertension has long been central to cardiovascular disease prevention, the optimal systolic blood pressure target has remained controversial.2,3 Recently, the Systolic Blood Pressure Intervention Trial (SPRINT) compared a target systolic blood pressure of 120 mm Hg with a target of 140 mm Hg among adults with hypertension but not diabetes who were also at elevated risk for cardiovascular disease. The trial reported that intensive blood pressure management reduced the rate of cardiovascular morbidity and mortality by 25%.4 A recent meta-analysis supported these findings and, together, these studies suggest that among higher-risk patients, achieving a lower blood pressure could have substantial health benefits.5
While the benefits of intensive blood pressure management make it appealing, such a strategy also has important tradeoffs. Participants in the intensive treatment arm of SPRINT required additional medications and physician visits to achieve a lower target blood pressure. They also experienced higher rates of some serious adverse events. Last, although the relative benefit reported in SPRINT for intensive blood pressure management was large, the absolute event rates were low, with a number needed to treat of about 198 to avert 1 cardiovascular event or death per year. By comparison, the number needed to harm was much smaller, about 56 per year. Thus, the benefits of intensive blood pressure management may be offset by the costs of treatment and by the costs and burden of adverse events and adverse effects.
Our goal in this study was to evaluate the incremental cost-effectiveness of intensive blood pressure management compared with standard management, weighing the lifetime benefits of treatment against the risks for adverse events and costs accrued. We also explored the value of intensive blood pressure management insituations that more closely resemble typical nontrial conditions, particularly addressing how serious adverse event rates, common adverse effects, and reduced effectiveness could alter the value of intensive blood pressure management.
Methods
Model Structure, Treatments, Health States, and Target Population
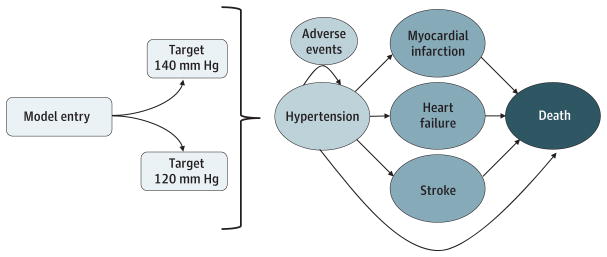
To estimate lifetime costs and benefits of intensive and standard blood pressure control, we developed a decision analytic Markov model that captures hypertension and cardiovascular disease under 2 alternative blood pressure management strategies (Figure 1). The Markov model tracks a simulated cohort of 68-year-old adults over their remaining lifetimes. The cohort begins at risk for cardiovascular events including myocardial infarction (MI), stroke, and congestive heart failure. Those who experience a cardiovascular event can die immediately or transition to a postevent state in which they are at higher risk for death and experience lower quality of life and higher costs.
Figure 1. Conceptual Diagram of the Cost-effectiveness Model.
Patients enter the model and are assigned to 1 of 2 treatment strategies. Patients in each treatment strategy can remain hypertensive, develop cardiovascular disease, or die. While hypertensive, patients accrue the costs of treatment and adverse events associated with treatment. The probabilities of events in the model vary according to treatment group.
Based on treatment patterns described in SPRINT, we assumed that those who underwent intensive blood pressure management took 3 blood pressure medications and saw their physician 3 times a year. Those in the standard treatment arm took 2 medications and saw their physician twice yearly.
Once participants experienced cardiovascular events (MI, stroke, or heart failure), we assumed they returned to standard management and no longer accrued the additional costs, risks, or benefits of intensive blood pressure management. We chose this approach because SPRINT was designed to evaluate the effect of intensive blood pressure management on the first occurrence of cardiovascular disease or death among a group of high-risk patients with hypertension rather than on recurrent events. Further, because SPRINT excluded patients with heart failure and stroke, we have little insight into the effect of intensive blood pressure management in these populations. Last, once patients develop cardiovascular disease, particularly stroke or heart failure, other treatment considerations may prevail as there are separate, well-developed bodies of literature for blood pressure treatment in those populations.6,7
Base case parameters are listed in the Table. In our model, all costs and quality-of-life adjustments were discounted by 3% annually and all costs were inflated to 2016 prices using the Consumer Price Index.22 All analyses were performed in Tree Age Pro (Tree Age Software), Excel (Microsoft), or Stata (StataCorp). Institutional review board approval was not needed, as this study did not involve human participants.
Table.
Base Case Parameters and Sources
| Parameter | Intensive Management | Standard Management | Source |
|---|---|---|---|
| Age, y | 68 | 68 | Wright et al,4 2015 |
| Efficacy, HR | |||
| CV death | 0.57 | 1 | Wright et al,4 2015 |
| Non-CV death | 0.77 | 1 | Wright et al,4 2015 |
| MI | 0.83 | 1 | Wright et al,4 2015 |
| Stroke | 0.89 | 1 | Wright et al,4 2015 |
| HF | 0.62 | 1 | Wright et al,4 2015 |
| Events, probability of (per mo) | |||
| Death, hypertensive group | 0.000706 | 0.000767 | Centers for Disease Control and Prevention8 |
| Death after MI | 0.008355 | 0.008355 | Centers for Disease Control and Prevention8; Coles et al,9 2012 |
| Death after stroke | 0.022691 | 0.022691 | Centers for Disease Control and Prevention8; Fonarow et al,10 2011 |
| Death after HF | 0.009084 | 0.009084 | Centers for Disease Control and Prevention8; Mozaffarian et al,11 2015 |
| Nonfatal MI | 0.000497 | 0.000598 | National Heart, Lung, and Blood Institute12 |
| Nonfatal stroke | 0.000232 | 0.000260 | National Heart, Lung, and Blood Institute12 |
| HF | 0.000279 | 0.000449 | National Heart, Lung, and Blood Institute12 |
| Adverse events (per mo) | |||
| Probability of serious adverse events | 0.00419 | 0.00264 | Wright et al,4 2015 |
| HR for serious adverse events | 1.59 | 1 | Wright et al,4 2015 |
| Probability of minor adverse effects | 0.268 | 0.229 | Bardage and Isacson,13 2000 |
| HR for minor adverse effects | 1.20 | 1 | Bardage and Isacson,13 2000; Law et al,14 2003 |
| Costs (per mo), $ | |||
| Background cost | 543 | 543 | Neuman et al,15 2015 |
| Medication costs | 56 | 37 | Moran et al,16 2015 |
| Physician visits | 21 | 14 | Centers for Medicare and Medicaid Services17 |
| One-time cost of stroke | 6909 | 6909 | Duh et al,18 2009 |
| One-time cost of HF | 8671 | 8671 | Duh et al,18 2009 |
| One-time cost of MI | 28 983 | 28 983 | Duh et al,18 2009 |
| Long-term incremental cost of stroke | 365 | 365 | Duh et al,18 2009 |
| Long-term incremental cost of HF | 674 | 674 | Duh et al,18 2009 |
| Long-term incremental cost of MI | 612 | 612 | Duh et al,18 2009 |
| Cost of serious adverse event | 7151 | 7151 | Duh et al,18 2009 |
| Cost of minor adverse event | 0 | 0 | Expert judgment |
| Utilities at age 68 y (per y, unless noted) | |||
| Baseline utility at 68 | 0.83925 | 0.83925 | Sullivan and Ghushchyan,19 2006 |
| Marginal disutility for | |||
| Hypertension | −0.025 | −0.025 | Sullivan and Ghushchyan,19 2006 |
| Stroke | −0.0524 | −0.0524 | Sullivan and Ghushchyan,19 2006 |
| HF | −0.0635 | −0.0635 | Sullivan and Ghushchyan,19 2006 |
| MI | −0.0409 | −0.0409 | Sullivan and Ghushchyan,19 2006 |
| Serious adverse events | −0.5/wk | −0.5/wk | Sullivan and Ghushchyan,19 2006 |
| Minor adverse events | −0.01 | −0.01 | Timbie et al,20 2010 |
| Taking a pill (2 vs 3 pills) | −0.003 | −0.002 | Timbie et al,20 2010; Hutchins et al,21 2015 |
Abbreviations: CV, cardiovascular; HF, heart failure; HR, hazard ratio; MI, myocardial infarction.
Mortality and Cardiovascular Disease Events
We based age-specific risk for death among at-risk patients with hypertension on data from Centers for Disease Control and Prevention Life Tables.8,23 All-cause mortality among patients with a prior MI, stroke, or heart failure was based on survival data from observational studies (eAppendix, section 1A, in the Supplement).9–11 We used the Cardiovascular Health Study cohort as the basis for age-specific estimates of non-fatal MI, nonfatal stroke, and heart failure incidence.12
Treatment Effects
For those receiving intensive blood pressure management, we reduced cardiovascular and noncardiovascular mortality to reflect the benefit reported in SPRINT (eAppendix, section 1A, in the Supplement). We also reduced the risk for developing cardiovascular disease (MI, heart failure, or stroke) according to the hazard ratios reported in SPRINT.
Adverse Events
We included a category of combined serious adverse events that captured typical costs and harms associated with adverse events requiring hospitalization or an emergency department visit (eAppendix, section 1B, in the Supplement). In a sensitivity analysis, we modeled the specific adverse events that differed between arms as reported in SPRINT (ie, hypotension, syncope, electrolyte abnormalities, and acute kidney injury).
SPRINT did not report minor adverse events or adverse effects, so we used adverse effect rates from the published literature in those taking 2 or 3 antihypertensive medications.13,14 Our goal was to capture medication adverse effects, such as fatigue, cough, and dizziness, that are common and uncomfortable but do not have severe or irreversible health consequences.
Costs
We calculated background monthly medical costs using age-specific Medicare estimates.15 For cardiovascular disease states (MI, stroke, and heart failure), we incorporated a cost associated with an acute event as well as a monthly additional cost that captured long-term costs (eAppendix, section 1C, in the Supplement).18 For costs of generic blood pressure medications, we used previously published costs for standard doses.16 We based the cost of a physician visit on Medicare outpatient visit reimbursement rates.17
We calculated costs of serious adverse events based on typical costs for a hospitalization for that event and physician fees for a 4-day hospitalization (eAppendix, section 1C, in the Supplement).17,24 For minor adverse events and adverse effects, we assumed no health care cost in our base case, as many patients may not report adverse effects or may address them only in the context of an already-scheduled visit. We varied this assumption in sensitivity analyses.
Health-Related Quality of Life
We calculated age-specific utilities for patients with hypertension and prior MI, stroke, and heart failure based on the EuroQol EQ-5D scores from a nationally representative sample (eAppendix, section 1D, in the Supplement).19 Similar to other published work, we applied a utility decrement of −0.5 for 1 week in case of a serious adverse event, assuming serious but time-limited decrement in quality of life.16 In our base case, we used a small monthly decrement for minor adverse events and medication adverse effects based on prior literature.20 We included a small disutility for the inconvenience of taking pills, consistent with prior literature.20,21
Model Calibration
We calibrated event rates in our modeled cohort to multiple targets from SPRINT. This approach allowed us to capture the experience of the SPRINT population and, implicitly, the population’s characteristics. To achieve this, we simultaneously calibrated event-free survival at 3.26 years to within 0.5 percentage points of that observed in SPRINT and all-cause mortality to fall within the 95% confidence limit for the Kaplan-Meier curves reported in SPRINT. We also ensured that event rates (MI, stroke, and heart failure) did not exceed event rates reported in SPRINT, as our model captured nonfatal first events only and SPRINT reported all events.
Sensitivity Analyses
The primary goal of our sensitivity analyses was to evaluate how the value of intensive blood pressure management might change in response to typical nontrial conditions. In particular, we evaluated whether increased frequency, severity, and cost of both serious and minor adverse events influenced the preferred blood pressure management strategy. We assessed whether a combination of attenuated benefits and concurrent increased risks for adverse events, as might be seen outside of a clinical trial, substantially altered our findings (eAppendix, section 3, in the Supplement). We also evaluated how a reduction in baseline cardiovascular risk and a decrease in the benefits of treatment affected the cost-effectiveness of intensive blood pressure management.
In addition to our main analysis, which models cost-effectiveness at age 68 years, the mean age of participants in SPRINT, we also evaluated the cost-effectiveness of intensive blood pressure management among 80-year-old and among 50-year-old patients, the youngest age included in SPRINT (eAppendix, section 3, in the Supplement).
Last, we recalibrated our model to represent a more typical, nontrial population. Here, we calibrated all-cause mortality in our model to that observed among a cohort of participants from the National Health and Nutrition Examination Survey who met SPRINT inclusion criteria.25 We used population-based incidence rates of cardiovascular disease from the Cardiovascular Health Study as the basis of our cardiovascular disease risk estimates in this model (eAppendix, section 2, in the Supplement).12
We performed additional sensitivity analyses designed to test the robustness of our findings to its assumptions and uncertainty of its inputs. First, we altered the duration of benefits, costs, and risks of intensive blood pressure management from lifetime to 3.26 years, the median duration of follow-up in SPRINT. We also conducted a probabilistic sensitivity analysis of all parameters (eAppendix, section 4, and eTable in the Supplement).
Results
Model Calibration
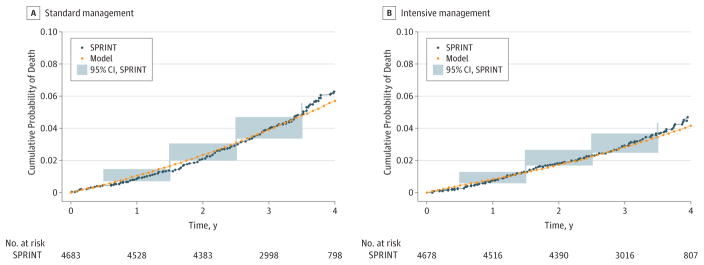
We calibrated our model to align with cumulative all-cause mortality as reported in SPRINT (Figure 2). After 3.26 years, the median trial follow-up, event-free survival was similar in our model and SPRINT. In the intensive management arm, event-free survival was 93.2% in the model and 92.9% in SPRINT. In the standard treatment arm, event-free survival was 90.9% in the model and 91.0% in SPRINT. Likewise, for sensitivity analyses, model calibration to data representing the hypertensive population in the United States from the National Health and Nutrition Examination Survey also achieved good concordance (eFigure 1 in the Supplement).
Figure 2. Cumulative All-Cause Mortality.
A, Figure depicts cumulative all-cause mortality in the standard management arm of the Systolic Blood Pressure Intervention Trial (SPRINT) compared with the model. The blue shaded areas are the approximate 95% CIs from SPRINT. B, Figure depicts cumulative all-cause mortality in the intensive management arm of SPRINT compared with the model. The blue shaded areas are the approximate 95% CIs from SPRINT.
Base Case Analysis
At 5 years, patients in the standard treatment arm had higher event rates than patients in the intensive treatment arm for nonfatal MI (3.8% vs 3.2%), nonfatal stroke (2.3% vs 2.1%), heart failure (3.2% vs 2.0%), and death (7.8% vs 5.7%). We estimated a life expectancy of 12.97 years in the standard arm and 14.25 years in the intensive management arm. After accounting for quality-of-life reductions associated with cardiovascular disease, aging, treatment, and adverse events, we estimated a quality-adjusted life expectancy of 9.6 years in the standard management arm and 10.5 years in the intensive management arm. Lifetime health care costs were $155 261 in the standard treatment arm and $176 584 in the intensive management group. Taken together, intensive blood pressure management cost $23 777 per quality-adjusted life-year (QALY) gained relative to standard management.
Sensitivity Analyses
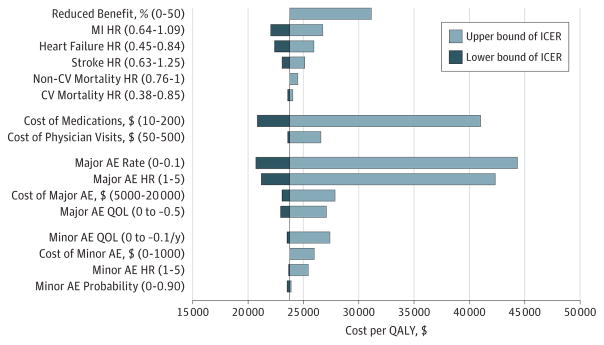
In 1-way sensitivity analyses, altering the costs, probabilities, hazard ratios, and disutility associated with serious adverse events and minor adverse events did not materially affect the preferred treatment strategy at a willingness to pay threshold of $50000perQALY gained (Figure 3). Similarly, reducing the anticipated benefits of intensive blood pressure management by half did not alter our preferred strategy (Figure 3). A version of our model with serious adverse events individually enumerated estimated a cost of $22 780 per QALY gained. Among a cohort of 80-year-old patients, we found that intensive blood pressure management cost $24 810 per QALY. We found similar results among a cohort of 50-year-old patients, where intensive blood pressure management cost $23 081 per QALY.
Figure 3. One-Way Sensitivity Analysis of Benefits and Risks of Intensive Blood Pressure Management.
Model parameters were varied between the ranges, which are shown in parentheses. The length of the bar indicates the incremental cost-effectiveness ratio associated with the range. Reduced benefit indicates that all of the hazard ratios (HRs) for benefit are simultaneously attenuated toward the null from a zero percentage reduction (ie, hazard ratios are as reported in the Systolic Blood Pressure Intervention Trial) to 50% (ie, a 50% reduction in the benefit). AE indicates adverse event; CV, cardiovascular; ICER, incremental cost-effectiveness ratio; MI, myocardial infarction; QALY, quality-adjusted life-year; and QOL, quality of life.
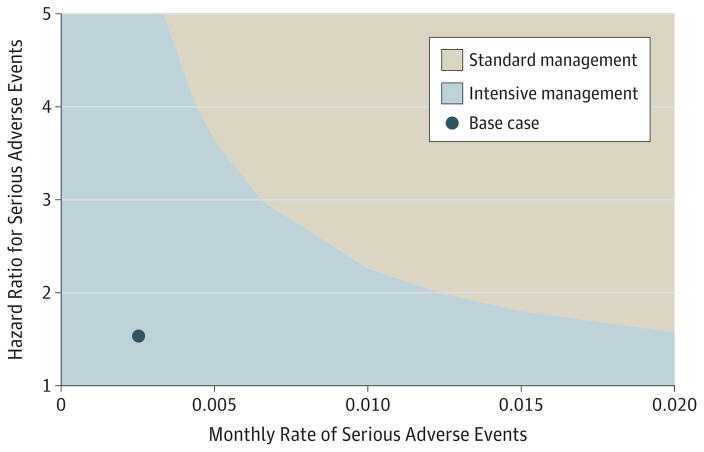
Given concerns that serious adverse event rates are higher in clinical practice settings than in trial populations, we used 2-way sensitivity analyses to examine the effect of both the underlying rates of such events and the differential risk from intensive management. To prefer standard management, serious adverse events would need to be substantially more common than observed in SPRINT overall and more likely to occur with intensive blood pressure management relative to standard management than observed in SPRINT (Figure 4). For example, to prefer standard management at a willingness to pay threshold of $50 000 per QALY gained, serious adverse event rates would need to be 3 times that observed in the standard management arm of SPRINT and also be 3 times more likely in the intensive group than the standard group.
Figure 4. Two-Way Sensitivity Analysis of Serious Adverse Events.
The y-axis depicts an increasing hazard ratio for serious adverse events in the intensive management arm compared with the standard management arm. The x-axis depicts an increasing monthly rate of serious adverse events in the standard management arm. The figure assumes a willingness to pay threshold of $50 000.
Minor adverse events and adverse effects from antihypertensive medications are common and more likely to occur as antihypertensive treatment intensifies.13 While adverse effects may not contribute to significant disability, they can be troubling. Minor adverse effects, though, would have to be about 10-fold more severe than anticipated, and thus would no longer truly be minor, in order to prefer standard management at a willingness to pay threshold of $50000 per QALY.
In addition to increased adverse event rates, the benefits observed in a trial may also be attenuated when evidence is translated into practice. eFigure 2 in the Supplement represents a range of scenarios in which the benefits associated with intensive blood pressure management are reduced and the risks of adverse events are increased. If the benefits of intensive blood pressure management were all reduced by half and the risks for adverse events increased 2-fold, standard management would be preferred at a willingness to pay threshold of $50000 per QALY.
The results of the Heart Outcomes Prevention Evaluation–3 Study, which indicated a nonsignificant 7% reduction in the primary end point of major cardiovascular events and death raise the question of whether intensive blood pressure management would be cost-effective in lower-risk patients.26 In a 2-way sensitivity analysis, we varied both cardiovascular risk and the benefit of intensive blood pressure management (eFigure 3 in the Supplement). These analyses indicate that the cost-effectiveness of intensive blood pressure management becomes less favorable as either cardiovascular risk or the benefit from intensive blood pressure management decreases. For example, at the full benefit observed in SPRINT, intensive blood pressure management would still be cost-effective in a population with approximately 50% of the cardiovascular risk of the SPRINT population, but not as cardiovascular risk drops below approximately 25% of that seen in SPRINT. However, the magnitude of benefit that could be obtained in lower-risk populations is not known; therefore, an assessment of the cost-effectiveness in such populations must await further trial based estimates of effectiveness.
We also asked whether intensive blood pressure management would remain cost-effective in a representative population of patients with hypertension in the United States. We repeated our base case analysis in a model calibrated to the National Health and Nutrition Examination Survey population. Here, we found that intensive management cost $21 592 per QALY gained under the assumptions in our main analysis.
While it is plausible that the benefits observed in SPRINT would persist as long as a patient is treated, the trial formally only demonstrated benefit for the duration of the trial. In an analysis where the duration of benefits, costs, and risks associated with intensive management was limited to the median trial follow-up, intensive management cost $35 343 per QALY gained relative to standard management.
In a probabilistic sensitivity analysis, intensive blood pressure management was preferred in 84% of simulations at a willingness to pay threshold of $50 000 per QALY gained (eFigure 4 in the Supplement).
Discussion
In a population of patients with hypertension and an elevated risk for cardiovascular events, we estimated the lifetime benefits and costs of standard and intensive blood pressure management. Our analysis implies that intensive blood pressure management costs $23 777 per QALY gained. This cost-effectiveness ratio is comparable with that of other interventions that are considered to be cost-effective in the United States and suggests that intensive blood pressure management in this population provides excellent value.
As adverse event rates and benefits in clinical practice can differ substantially from trial populations, we explored multiple scenarios that evaluated the cost-effectiveness of intensive blood pressure management in such settings. Even with increased adverse event rates and reduced efficacy, intensive blood pressure management remained cost-effective, suggesting that this approach would be preferred even outside the tightly controlled context of a clinical trial.
Our results are consistent with previous cost-effectiveness analyses of blood pressure management, which have generally found that treating hypertension is cost-effective or even cost-saving. For example, a recent cost-effectiveness analysis examined implementation of the 2014 Eighth Joint National Committee hypertension guidelines and found that in many cases, treating hypertension according to the guidelines was cost-saving or extremely cost-effective.16 A second recent cost-effectiveness analysis evaluated the cost-effectiveness of intensive blood pressure management in addition to current hypertension guidelines and concluded that intensive blood pressure management is cost-effective or cost-saving.27 Our analysis adds to this body of literature by specifically incorporating the estimates of benefit and risk described in SPRINT and exploring the cost-effectiveness of intensive blood pressure management in older populations.
How might our findings influence practice? Increasingly, clinicians are held accountable both for the health of their patients and also the costs of caring for them. Concerns about costs of treatment and adverse events might temper enthusiasm for intensive blood pressure management, especially given the number needed to treat described in SPRINT. Our analysis indicates that unless adverse events are markedly higher or benefits are substantially lower than observed in SPRINT, intensive blood pressure management is both effective and cost-effective in patients at high cardiovascular risk. These analyses can inform clinicians, provider organizations, and guideline developers as they translate the results of SPRINT into practice.
Our approach had some important limitations. Our model addressed a specific question within hypertension management and drew largely on findings from SPRINT. Although relying on estimates from a single study may limit generalizability and recapitulate any biases in that study, we believe this approach is warranted because SPRINT answers a key clinical question and because the approach described in SPRINT is likely to be incorporated into practice.
Although we have tried to anticipate a range of scenarios associated with intensive blood pressure management, we did not include every possible consequence of hypertension in our model. In particular, we did not incorporate long-term renal complications of hypertension or hypertension treatment. SPRINT found that patients in the intensive management arm were more likely to develop acute kidney injury and persistent reductions in glomerular filtration rate. However, the clinical significance of these findings is uncertain, particularly because SPRINT reported no difference in progression to end-stage renal disease even among patients with chronic kidney disease at baseline. While further follow-up may clarify the effect of intensive blood pressure management on renal disease, given the findings reported in SPRINT, we did not include differential long-term renal outcomes in our model.
Likewise, we did not represent repeated cardiovascular events in our model. While this is a simplification of reality, we chose this approach so that we could most closely model the findings from SPRINT without excessive extrapolation. Further, this approach is likely conservative. Repeated cardiovascular events would likely create greater cost and lower quality of life in the standard treatment arm compared with the intensive treatment arm if intensive blood pressure management had a favorable effect on repeated events. If so, intensive blood pressure management would be even more cost-effective than we estimated.
Conclusions
Treatment of systolic blood pressure to a target of 120 mm Hg for patients with hypertension and not diabetes at high risk for cardiovascular disease provides excellent value relative to standard management with a target systolic blood pressure of 140 mm Hg. This finding was consistent over a wide range of clinical scenarios and populations where benefits may be smaller, adverse event rates may be higher, and the duration of benefit may be shorter.
Supplementary Material
Key Points.
Question
Is intensive blood pressure management cost-effective?
Findings
We conducted a cost-effectiveness analysis comparing intensive blood pressure management with standard management among patients with hypertension at high risk for cardiovascular disease. We found that intensive blood pressure management costs $23 777 per quality-adjusted life-year gained.
Meaning
Intensive blood pressure management is cost-effective among patients with hypertension at high risk for cardiovascular disease.
Acknowledgments
Dr Richman is supported by a VA Office of Academic Affairs Advanced Fellowship in Health Services Research and Development. Mr Jørgensen is supported by the Lundbeck Foundation Clinical Research Fellowship Program. Dr Owens is supported by the Department of Veterans Affairs. Dr Goldhaber-Fiebert is supported by grant 1K01AG037593-01A1 from the National Institute on Aging. No other disclosures were reported.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position nor the policy of the Department of Veterans Affairs of the US government.
Additional Contributions: We thank Emma Rastatter, BA, for her help with earlier versions of this work. She did not receive compensation for her contributions.
Author Contributions: Dr Richman had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: All Authors.
Acquisition, analysis, or interpretation of data: All Authors.
Drafting of the manuscript: Richman, Jørgensen.
Critical revision of the manuscript for important intellectual content: All Authors.
Statistical analysis: Richman, Fairley, Owens, Goldhaber-Fiebert.
Administrative, technical, or material support: Schuler.
Study supervision: Richman, Jørgensen, Owens.
References
- 1. [Accessed April 16, 2016];FastStats: hypertension. http://www.cdc.gov/nchs/fastats/hypertension.htm.
- 2.James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 3.Wright JT, Jr, Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014;160(7):499–503. doi: 10.7326/M13-2981. [DOI] [PubMed] [Google Scholar]
- 4.Wright JT, Jr, Williamson JD, Whelton PK, et al. SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387(10017):435–443. doi: 10.1016/S0140-6736(15)00805-3. [DOI] [PubMed] [Google Scholar]
- 6.Yancy CW, Jessup M, Bozkurt B, et al. American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J AmColl Cardiol. 2013;62(16):e147–e239. doi: 10.1016/j.jacc.2013.05.019. [DOI] [PubMed] [Google Scholar]
- 7.Kernan WN, Ovbiagele B, Black HR, et al. American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(7):2160–2236. doi: 10.1161/STR.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. [Accessed April 16, 2016];Life tables. http://www.cdc.gov/nchs/products/life_tables.htm.
- 9.Coles AH, Fisher KA, Darling C, et al. Recent trends in post-discharge mortality among patients with an initial acute myocardial infarction. Am J Cardiol. 2012;110(8):1073–1077. doi: 10.1016/j.amjcard.2012.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fonarow GC, Smith EE, Reeves MJ, et al. Get With The Guidelines Steering Committee and Hospitals. Hospital-level variation in mortality and rehospitalization for Medicare beneficiaries with acute ischemic stroke. Stroke. 2011;42(1):159–166. doi: 10.1161/STROKEAHA.110.601831. [DOI] [PubMed] [Google Scholar]
- 11.Mozaffarian D, Benjamin EJ, Go AS, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics: 2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–e322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 12.National Heart, Lung, and Blood Institute. [Accessed November 25, 2015];NHLBI incidence and prevalence chart book. 2006 http://www.nhlbi.nih.gov/research/reports/2006-incidence-chart-book.
- 13.Bardage C, Isacson DG. Self-reported side-effects of antihypertensive drugs: an epidemiological study on prevalence and impact on health-state utility. Blood Press. 2000;9(6):328–334. doi: 10.1080/080370500300000905. [DOI] [PubMed] [Google Scholar]
- 14.Law MR, Wald NJ, Morris JK, Jordan RE. Value of low dose combination treatment with blood pressure lowering drugs: analysis of 354 randomised trials. BMJ. 2003;326(7404):1427. doi: 10.1136/bmj.326.7404.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neuman P, Cubanski J, Damico A. Medicare per capita spending by age and service: new data highlights oldest beneficiaries. Health Aff (Millwood) 2015;34(2):335–339. doi: 10.1377/hlthaff.2014.1371. [DOI] [PubMed] [Google Scholar]
- 16.Moran AE, Odden MC, Thanataveerat A, et al. Cost-effectiveness of hypertension therapy according to 2014 guidelines. N Engl J Med. 2015;372(5):447–455. doi: 10.1056/NEJMsa1406751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Medicare and Medicaid Services. [Accessed April 16, 2016];Physician fee schedule. https://www.cms.gov/Medicare/Medicare-Fee-For-Service-Payment/PhysicianFeeSched/Index.html. Published April 7, 2016.
- 18.Duh MS, Fulcher NM, White LA, et al. Costs associated with cardiovascular events in patients with hypertension in US managed care settings. J Am Soc Hypertens. 2009;3(6):403–415. doi: 10.1016/j.jash.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Sullivan PW, Ghushchyan V. Preference-based EQ-5D index scores for chronic conditions in the United States. Med Decis Making. 2006;26(4):410–420. doi: 10.1177/0272989X06290495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Timbie JW, Hayward RA, Vijan S. Variation in the net benefit of aggressive cardiovascular risk factor control across the US population of patients with diabetes mellitus. Arch Intern Med. 2010;170(12):1037–1044. doi: 10.1001/archinternmed.2010.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hutchins R, Viera AJ, Sheridan SL, Pignone MP. Quantifying the utility of taking pills for cardiovascular prevention. Circ Cardiovasc Qual Outcomes. 2015;8(2):155–163. doi: 10.1161/CIRCOUTCOMES.114.001240. [DOI] [PubMed] [Google Scholar]
- 22.Bureau of Labor Statistics. [Accessed April 16, 2016];CPI inflation calculator. http://www.bls.gov/data/inflation_calculator.htm.
- 23.Heron M US Department of Health and Human Services. National Vital Statistics Reports. [Accessed April 16, 2016];Deaths: leading causes for 2010. 62(6) http://www.cdc.gov/nchs/data/nvsr/nvsr62/nvsr62_06.pdf. Published December 20, 2013. [Google Scholar]
- 24.Agency for Healthcare Research and Quality. [Accessed April 16, 2016];HCUPnet. http://hcupnet.ahrq.gov/
- 25.Centers for Disease Control and Prevention. [Accessed April 17, 2016];National Health and Nutrition Examination Survey. http://www.cdc.gov/nchs/nhanes.htm.
- 26.Lonn EM, Bosch J, López-Jaramillo P, et al. HOPE-3 Investigators. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2009–2020. doi: 10.1056/NEJMoa1600175. [DOI] [PubMed] [Google Scholar]
- 27.Moise N, Huang C, Rodgers A, et al. Comparative cost-effectiveness of conservative or intensive blood pressure treatment guidelines in adults aged 35–74 years: the cardiovascular disease policy model. Hypertension. 2016;68(1):88–96. doi: 10.1161/HYPERTENSIONAHA.115.06814. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.