Abstract
Background
The aims of this study were to investigate the relationship between optimal anthropometric indices and their cut-off values and the incidence of hypertension in a cohort of middle-aged women in China.
Material/Methods
A cohort of 812 women, aged between 40–70 years were recruited between May 2011 and June 2013. An ideal baseline blood pressure was defined as <120/80 mmHg; pre-hypertension was 120–139/80–89 mmHg; hypertension was ≥140/≥90 mmHg. Anthropometric measurements included waist circumference (WC), body mass index (BMI), waist-hip ratio (WHR), and waist-height ratio (WHtR). The cohort was divided into an ideal blood pressure group (Group 1) and a pre-hypertensive group (Group 2). Two-year follow-up blood pressure measurements were performed. Receiver-operating characteristic (ROC) curve analysis determined the optimal anthropometric indices and cut-off values for developing hypertension.
Results
At two-year follow-up, hypertension developed in 9.0% (n=31) in Group 1 and 32.3% (n=121) in Group 2. Logistic regression analysis showed that in both groups, women in the highest quartile for WC, BMI, WHR, and WHtR had a significantly increased risk of developing hypertension compared with the lowest quartile (P<0.05). ROC curve area under the curve (AUC) for these anthropometric indices were greater in Group 1, and for WC in Groups 1 and 2, with the optimal cut-off values greater in Group 1.
Conclusions
In a cohort of middle-aged women in China, anthropometric indices of obesity were predictive of the development of hypertension during a two-year follow-up period.
MeSH Keywords: Hypertension, Metabolism, Obesity, Prehypertension
Background
Worldwide, including in China, the increasing prevalence of hypertension is becoming a significant public health problem, resulting in high morbidity and mortality [1]. Therefore, primary prevention of hypertension is important. The concept of pre-hypertension was first proposed in 2003, in the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (the JNC 7 report) [2]. Although the 2017 American College of Cardiology and American Heart Association (ACC/AHA) guidelines on the prevention, diagnosis, and management of hypertension in adults has proposed new definition of high blood pressure, there is still some controversy regarding the applicability of the recent ACC/AHA clinical criteria for the Chinese population [3]. Of relevance to the present study, mildly elevated blood pressure or Stage 1 hypertension in the 2017 ACC/AHA guidelines, which recommend non-pharmacological therapy, was chosen as a group in the present study, termed the ‘pre-hypertensive group’ (Group 2) [3].
Among the independent risk factors for progression from normal or ideal blood pressure to hypertension, obesity is an important factor that is increasing globally, especially in China [4–9]. Anthropometric indices of obesity are recognized to be associated the development of hypertension, and various anthropometric measurements that reflect overweight and obesity include waist circumference (WC), body mass index (BMI), waist-hip ratio (WHR), and waist–height ratio (WHtR), although which of these indices best predicts the development of hypertension remains controversial [10–13]. Recent studies have shown that anthropometric indices of increased weight and obesity are associated with the incidence of hypertension in pre-hypertensive populations [14–16]. However, few studies have focused on whether these indices have different effects in pre-hypertensive populations, compared with those an ideal or normal blood pressure.
The aims of this prospective cohort study were to investigate the relationship between anthropometric indices and their optimal cut-off values and the incidence of hypertension in a cohort of middle-aged (between 40–70 years) Chinese women. The anthropometric indices chosen included WC, BMI, WHR, and WHtR and the use of receiver-operating characteristic (ROC) curve analysis to demonstrate the optimal cut-off value and reveal the best indices for predicting the development of hypertension during a two-year follow-up period. To the best of our knowledge, this was the first prospective cohort study to use ROC curve analysis to determine optimal cut-off values of anthropometric indices in middle-aged pre-hypertensive Chinese women.
Material and Methods
Study cohort and groups
This study was a population-based prospective cohort study that recruited 812 urban female residents in Tianjin, China, aged between 40–70 years who were not hypertensive. Cluster stratification sampling was used to recruit subjects in six districts of Tianjin between May 2011 and June 2013. The study exclusion criteria included high blood pressure (systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg), women who were being treated with anti-hypertensive drugs, who were in renal failure, or who had severe hepatic insufficiency, cancer, cerebrovascular disease, tuberculosis, autoimmune disease, systemic infections, any woman who was unable to cooperate in the study, or any woman with heart failure according to the New York Heart Association (NYHA) Class III–IV.
The study cohort was divided into two groups. Group 1 had a baseline ideal, or normal, blood pressure. Group 2, or the ‘pre-hypertensive group’ were equivalent to the mildly elevated blood pressure or Stage 1 hypertension classification used in the 2017 American College of Cardiology and American Heart Association (ACC/AHA) guidelines, which recommend non-pharmacological therapy in these cases [3].
After receiving complete information about the aims and methods of the study, all participants gave written informed consent for the examinations and follow-up. The demographic and medical history of the women in the study cohort were obtained using a structured questionnaire, which included sex, age, smoking history, and family history of hypertension. Between May 2013 and June 2015, the data of all the subjects were measured again, excluding those who were lost during the two-year follow-up. The final sample size of the study cohort comprised 719 women for analysis.
Blood pressure measurement
The blood pressure measurements were taken on the right arm after a 15-minute rest and between the hours of 8 a.m. to 9 a.m., using a calibrated mercury sphygmomanometer by trained health workers. The appearance of Korotkoff sounds (phase 1) was the criterion for measurement of the systolic blood pressure (SBP), and the disappearance of the Korotkoff sounds (phase 5) was the criterion for the measurement of diastolic blood pressure (DBP). Blood pressure measurements were taken in triplicate at two-minute intervals, and the average value was used to record the SBP and DBP. None of the subjects had tea, coffee, alcohol, or smoked cigarettes during the 30 minutes before the blood pressure measurements.
An ideal, or normal, blood pressure was defined as a baseline SBP <120 mmHg and DBP <80 mmHg; pre-hypertension was defined as a baseline SBP of 120–139 mmHg, or a DBP of 80–89 mmHg, or both; hypertension at follow-up was defined as a SBP ≥140 mmHg or a DBP ≥90 mmHg, or both, or as hypertension diagnosed at other hospitals during the two-year follow-up [2].
Anthropometric indices
Trained health workers took anthropometric measurements. Height was measured to the nearest cm without the woman wearing shoes. Weight was measured to the nearest kg without heavy clothes. Each woman’s waist circumference (WC) was defined as the midpoint between the lower rib and upper margin of the iliac crest and measured using a tape measure with an insertion buckle at one end. Hip circumstance (HC) was measured at the level of the maximal gluteal protrusion. The WC and HC were measured to the nearest cm. The body mass index (BMI) was calculated by dividing weight in kg by the height in meters2 (kg/m2). The waist-hip ratio (WHR) was calculated as the WC/HC. The waist-height ratio (WHtR) was calculated as the WC/height [17]. Measurements of BMI, WC, WHR, and WHtR were divided into quartiles to determine whether these indices were associated with the incidence of hypertension.
Biochemical indices
Fasting blood glucose (FBG), total cholesterol (TC), triglyceride (TG), high-density lipoprotein-cholesterol (HDL-C), low-density lipoprotein-cholesterol (LDL-C), serum creatinine (Cr), uric acid (UA), and high sensitivity C-reactive protein (hs-CRP) were measured after 12 hours of overnight fasting. Postprandial blood glucose (PBG) was measured after drinking 250 mL of water mixed with 75 g dextrose anhydrate. All the biochemical indices were measured from venous blood samples using a Roche C8000 Automated Analyzer at the Laboratory Center of the General Hospital of Tianjin Medical University. All quality control indices of the laboratory analysis met the requirements of the professional laboratories of the Tianjin Medical University General Hospital in strict accordance with laboratory protocols.
Statistical analysis
All statistical analyses were performed using SPSS version 21 (SPSS Inc., Chicago, IL, USA). Continuous variables were presented as the mean ± standard deviation (SD), and categorical variables were presented as percentages. A t-test was used to compare continuous variables between subjects with ideal, or normal, blood pressure and pre-hypertension subjects, and the chi-squared (χ2) test was used for categorical data. The contribution of anthropometric indices to the development of hypertension was evaluated using binary logistic analysis. Receiver-operating characteristic (ROC) curve analysis and the area under the curve (AUC) determined the optimal anthropometric indices and cut-off values for developing hypertension. Optimal cut-off values for the anthropometric measurements were determined using Youden’s index. P<0.05 was considered as statistically significant.
Results
Of the 719 women in the study cohort, 47.8% (n=344) were in Group 1, with an ideal, or normal, blood pressure, and 52.2% (n=375) were in Group 2, the pre-hypertension group. Table 1 shows the clinical and anthropometric characteristics of the study population.
Table 1.
Characteristics in both groups.
| Variables | Group 1 (n=344) | Group 2 (n=375) | P value |
|---|---|---|---|
| Age (years) | 54.83±6.30 | 57.22±6.52 | <0.001 |
| Anthropometric indices | |||
| WC (cm) | 80.77±7.94 | 86.23±8.84 | <0.001 |
| BMI (kg/m2) | 23.23±2.82 | 25.20±3.37 | <0.001 |
| WHR | 0.833±0.054 | 0.852±0.053 | <0.001 |
| WHtR | 0.501±0.049 | 0.537±0.055 | <0.001 |
| Biochemistry test | |||
| FBG (mmol/L) | 5.23±1.43 | 5.57±1.43 | <0.001 |
| PBG (mmol/L) | 6.68±2.80 | 7.50±3.50 | 0.001 |
| TC (mmol/L) | 5.46±1.06 | 5.70±1.03 | 0.002 |
| TG (mmol/L) | 1.46±1.21 | 1.78±1.23 | <0.001 |
| HDL-C (mmol/L) | 1.54±0.37 | 1.48±0.39 | 0.039 |
| LDL-C (mmol/L) | 3.33±0.94 | 3.47±0.92 | 0.047 |
| Scr (mmol/L) | 58.88±8.94 | 59.35±8.99 | 0.479 |
| UA (mmol/L) | 263.16±63.07 | 280.93±61.11 | <0.001 |
| hs-CRP (mg/L) | 2.56±3.60 | 2.86±6.68 | 0.452 |
| Other hypertension risk factors | |||
| Smoking (%) | 15 (4.4) | 11 (2.9) | >0.05 |
| Family history (%) | 180 (52.3) | 212 (56.5) | >0.05 |
| Blood pressure | |||
| Baseline SBP (mmHg) | 110.59±6.50 | 128.06±5.88 | <0.001 |
| Baseline DBP (mmHg) | 70.51±4.92 | 79.06±5.49 | <0.001 |
| Follow-up SBP (mmHg) | 117.28±21.71 | 128.53±12.52 | <0.001 |
| Follow-up DBP (mmHg) | 74.57±7.63 | 81.36±8.14 | <0.001 |
Group 1, ideal blood pressure group; Group 2, pre-hypertensive group. WC – waist circumference; BMI – body mass index; WHR – waist-hip ratio; WHtR – waist-height ratio; FBG – fasting blood glucose; PBG – postprandial blood glucose; TC – total cholesterol; TG – triglyceride; HDL-C – high-density lipoprotein cholesterol; LDL – low-density lipoprotein cholesterol; Scr – serum creatinine; UA – uric acid; hs-CRP – high sensitivity C-reactive protein.
At baseline, when the women were initially recruited into the study cohort, the mean age, waist circumference (WC), body mass index (BMI), waist-hip ratio (WHR), and waist-height ratio (WHtR), fasting blood glucose (FBG), postprandial blood glucose (PBG), total cholesterol (TC), triglyceride (TG), low-density lipoprotein-cholesterol (LDL-C), and uric acid (UA) were significantly greater in Group 2 compared with Group 1, while high-density lipoprotein-cholesterol (HDL-C) was significantly greater in Group 1 (P<0.05). The smoking history and family history of hypertension showed no significant differences between the two groups.
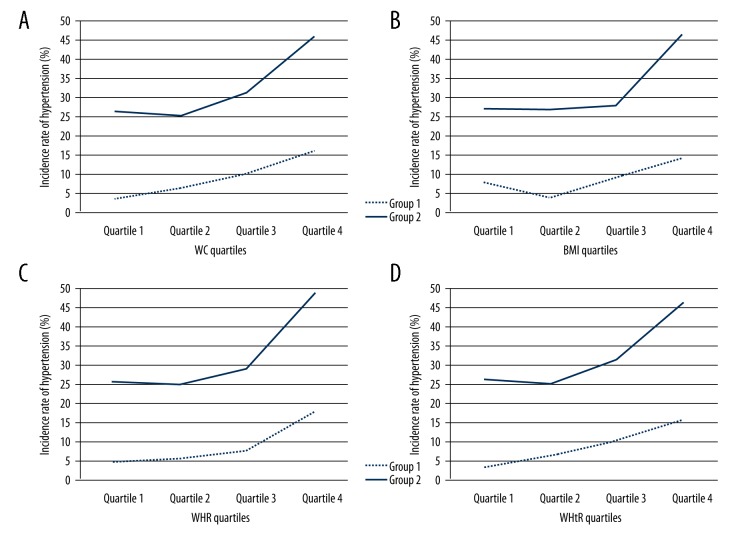
During the two-year follow-up period, 9.0% (n=31) in Group 1, and 32.3% (n=121) in Group 2 developed hypertension. The incidence of hypertension in Group 2 was significantly greater compared with Group 1 (χ2=58.2; P<0.001). Also, there was a significant trend of an increased incidence of hypertension with an increase in WC, BMI, WHR, and WHtR (P<0.05) in both Group 1 and Group 2 (Figure 1).
Figure 1.
The relationship between anthropometric indices quartiles and incidence of hypertension during the 2-year follow-up in both groups. Group 1, ideal blood pressure group; Group 2, pre-hypertensive group. WC – waist circumference; BMI – body mass index; WHR – waist-hip ratio; WHtR – waist-height ratio.
Table 2 shows the association between the anthropometric indices and the incidence of hypertension. Univariate logistic regression analysis indicated that women in both groups in the highest quartile of WC, BMI, WHR, and WHtR had the greatest risk of developing hypertension compared with women in the lowest quartile. Even after adjusting for age, UA, FBG, PBG, LDL-C family history, and smoking history, these anthropometric indices remained statistically significant. However, there was no statistically significant difference in anthropometric indices between quartiles 2 and 3, compared with quartile 1.
Table 2.
Odd ratio and 95% confidence interval for progression to hypertension in both groups.
| Anthropometric indices | Quartile | Range (min, max) | No. of subjects | Without adjusting | Adjusting for age, UA, FBG, PBG, LDL-C family history and smoking | ||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | P value | ||||
| Group 1 | |||||||||
| WC (cm) | 1 | 60, 74 | 76 | 1.000 | – | – | 1.000 | – | – |
| 2 | 75, 81 | 94 | 2.079 | 0.392–11.026 | 0.390 | 1.606 | 0.280–9.221 | 0.595 | |
| 3 | 82, 85 | 82 | 3.453 | 0.694–17.172 | 0.130 | 2.544 | 0.472–13.714 | 0.278 | |
| 4 | 86, 106 | 92 | 8.387 | 1.871–37.584 | 0.005 | 6.363 | 1.287–31.454 | 0.023 | |
| BMI (kg/m2) | 1 | 16.42, 21.47 | 91 | 1.000 | – | – | 1.000 | – | – |
| 2 | 21.48, 23.03 | 81 | 0.623 | 0.176–2.213 | 0.465 | 0.648 | 0.182–2.312 | 0.504 | |
| 3 | 23.05, 24.98 | 86 | 1.231 | 0.426–3.553 | 0.701 | 1.250 | 0.432–3.616 | 0.680 | |
| 4 | 24.99, 42.29 | 86 | 1.946 | 0.728–5.201 | 0.018 | 1.956 | 0.731–5.232 | 0.019 | |
| WHR | 1 | 0.706, 0.790 | 86 | 1.000 | – | – | 1.000 | – | – |
| 2 | 0.791, 0.827 | 87 | 1.250 | 0.324–4.822 | 0.746 | 1.264 | 0.327–4.888 | 0.734 | |
| 3 | 0.828, 0.862 | 87 | 1.794 | 0.506–6.365 | 0.366 | 1.773 | 0.499–6.307 | 0.376 | |
| 4 | 0.863, 1.215 | 84 | 4.457 | 1.413–14.053 | 0.011 | 4.369 | 1.376–13.873 | 0.012 | |
| WHtR | 1 | 0.394, 0.467 | 88 | 1.000 | – | – | 1.000 | – | – |
| 2 | 0.469, 0.497 | 80 | 1.889 | 0.437–8.171 | 0.395 | 2.790 | 0.509–15.274 | 0.237 | |
| 3 | 0.500, 0.532 | 88 | 3.228 | 0.437–8.171 | 0.087 | 3.799 | 0.729–19.786 | 0.113 | |
| 4 | 0.533, 0.665 | 88 | 5.360 | 1.483–19.382 | 0.010 | 6.249 | 1.231–31.718 | 0.027 | |
| Group 2 | |||||||||
| WC (cm) | 1 | 64, 79 | 77 | 1.000 | – | – | 1.000 | – | – |
| 2 | 80, 84 | 93 | 1.728 | 1.431–19.126 | 0.128 | 1.747 | 0.842–3.624 | 0.134 | |
| 3 | 85, 91 | 107 | 1.287 | 0.637–2.597 | 0.482 | 1.102 | 0.526–2.309 | 0.798 | |
| 4 | 92, 125 | 98 | 3.812 | 1.935–7.511 | <0.001 | 3.460 | 1.673–7.156 | 0.001 | |
| BMI (kg/m2) | 1 | 16.82, 22.86 | 92 | 1.000 | – | – | 1.000 | – | – |
| 2 | 22.89, 24.92 | 97 | 0.981 | 1.935–7.511 | 0.954 | 0.895 | 0.460–1.742 | 0.744 | |
| 3 | 24.97, 27.18 | 89 | 1.047 | 0.546–2.009 | 0.890 | 0.949 | 0.473–1.906 | 0.884 | |
| 4 | 27.24, 46.61 | 97 | 2.319 | 1.262–4.262 | 0.007 | 2.253 | 1.174–4.325 | 0.015 | |
| WHR | 1 | 0.691, 0.818 | 93 | 1.000 | – | – | 1.000 | – | – |
| 2 | 0.819, 0.852 | 92 | 0.958 | 0.494–1.858 | 0.900 | 0.974 | 0.486–1.955 | 0.942 | |
| 3 | 0.853, 0.879 | 96 | 1.184 | 0.494–1.858 | 0.605 | 1.104 | 0.556–2.194 | 0.777 | |
| 4 | 0.880, 1.141 | 94 | 2.755 | 0.494–1.858 | 0.001 | 2.599 | 1.320–5.116 | 0.006 | |
| WHtR | 1 | 0.386, 0.494 | 95 | 1.000 | – | – | 1.000 | – | – |
| 2 | 0.497, 0.530 | 95 | 0.946 | 0.494–1.813 | 0.868 | 0.875 | 0.447–1.714 | 0.698 | |
| 3 | 0.531, 0.568 | 92 | 1.289 | 0.684–2.43 | 0.433 | 1.048 | 0.534–2.057 | 0.892 | |
| 4 | 0.569, 0.791 | 93 | 2.408 | 1.306–4.441 | 0.005 | 1.948 | 1.010–3.759 | 0.047 | |
Group 1, ideal blood pressure group; Group 2, pre-hypertensive group. WC – waist circumference; BMI – body mass index; WHR – waist–hip ratio; WHtR – waist–height ratio; CI – confidence interval; UA – uric acid; FBG – fasting blood glucose; PBG – postprandial blood glucose; LDL-C – low-density lipoprotein cholesterol.
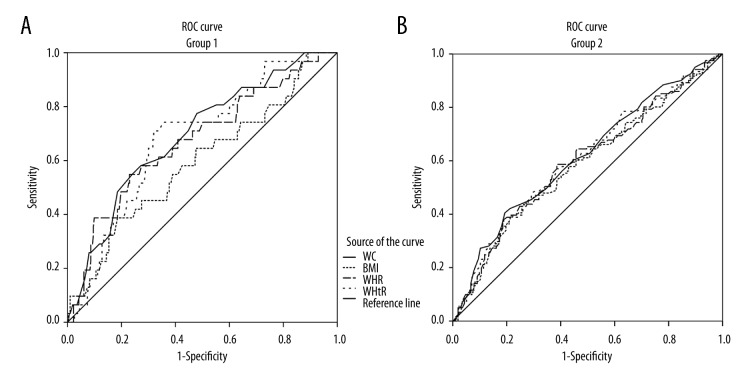
To determine the most effective anthropometric indices in predicting the incidence of developing hypertension, analysis of the receiver-operating characteristic (ROC) curve and the area under the curve (AUC) for these anthropometric indices in relation to the incidence of hypertension were calculated (Figure 2). As shown in Table 3, WC has the highest AUC among the four indices (WC, BMI, WHR, and WHtR) in both groups. Compared with Group 2, the AUC of all the four indices were higher in Group 1. Also, the optimal cut-off points of the anthropometric indices for predicting hypertension were calculated using Youden’s index (Table 3), which showed that the cut-off points for WC, BMI, WHR, and WHtR were higher in Group 2 than in Group 1. Youden’s index for WHtR appeared to be the highest in Group 1 and WC in Group 2 among the measured obesity anthropometric indices.
Figure 2.
ROC curves for anthropometric indices in relation to incidence of hypertension. Group 1, ideal blood pressure group; Group 2, pre-hypertensive group. ROC – receiver operating characteristic; WC – waist circumference; BMI – body mass index; WHR – waist-hip ratio; WHtR – waist-height ratio.
Table 3.
AUC and optimal cut-off points of anthropometric indices in relation to incidence of hypertension in both groups.
| Anthropometric indices | AUC | 95% CI | P value | Cut-off point | Sensitivity (%) | Specificity (%) | Youden Index |
|---|---|---|---|---|---|---|---|
| Group 1 | |||||||
| WC (cm) | 0.692 | 0.598–0.787 | <0.001 | 84.5 | 0.581 | 0.272 | 0.309 |
| BMI (kg/m2) | 0.593 | 0.484–0.702 | 0.087 | 25.4 | 0.387 | 0.185 | 0.202 |
| WHR | 0.671 | 0.568–0.775 | 0.002 | 0.859 | 0.548 | 0.230 | 0.318 |
| WHtR | 0.682 | 0.591–0.772 | 0.001 | 0.516 | 0.710 | 0.319 | 0.390 |
| Group 2 | |||||||
| WC (cm) | 0.615 | 0.553–0.677 | <0.001 | 91.5 | 0.405 | 0.193 | 0.212 |
| BMI (kg/m2) | 0.587 | 0.525–0.650 | 0.006 | 26.2 | 0.446 | 0.272 | 0.175 |
| WHR | 0.597 | 0.534–0.660 | 0.002 | 0.862 | 0.587 | 0.386 | 0.201 |
| WHtR | 0.604 | 0.542–0.667 | 0.001 | 0.550 | 0.479 | 0.291 | 0.188 |
Group 1, ideal blood pressure group; Group 2, pre-hypertensive group. WC – waist circumference; BMI – body mass index; WHR – waist-hip ratio; WHtR – waist-height ratio; AUC – area under the receiver operating characteristic curve; CI – confidence interval.
Discussion
In this cohort study of 812 middle-aged women in China, aged between 40–70 years, women were divided into an ideal, or normal, blood pressure group (Group 1) and a pre-hypertensive group (Group 2) on recruitment. The aims of the study were to determine whether anthropometric measurements, including waist circumference (WC), body mass index (BMI), waist–hip ratio (WHR), and waist-height ratio (WHtR) were predictive for the development of hypertension. The findings were that after two-year follow-up, the receiver-operating characteristic (ROC) curve and the area under the curve (AUC) analysis showed that WC had the highest AUC among the four indices (WC, BMI, WHR, and WHtR), in both groups, but compared with Group 2, the AUC of all the four indices were higher in Group 1, and the optimal cut-off points of the anthropometric indices for predicting hypertension were all higher in Group 2 than in Group 1, and that WHtR had the highest index in Group 1 and WC had the highest index Group 2. The findings of this study showed that, in a cohort of middle-aged Chinese women, anthropometric indices were different in their ability to predicting hypertension in pre-hypertensive women compared with women with an ideal, or normal, initial blood pressure. These findings may have implications for the prevention of hypertension in this population.
Obesity is a major risk factor for hypertension that can be effectively controlled through exercise and diet, and control of obesity is recognized to have an important role in primary prevention of hypertension. The mechanism of the association between obesity and hypertension might be explained by the increase in leptin in obesity, the decrease in adiponectin, and in the development of insulin resistance [18–21]. This study used some of the main anthropometric assessment methods for obesity, including WC, BMI, WHR, and WHtR. However, there remains some controversy as to which is the best of the anthropometric and other indices for predicting the development of hypertension.
Several previously published studies have supported the finding that WC is the best predictor for the development of hypertension [12–14,22]. However, other studies have suggested that WHR or WHtR are the best predictors [23–26]. In the present study, WC appeared to be a better predictor than BMI, WHR, or WHtR in women who began the study with an ideal or normal blood pressure (wider AUC), a finding that is supported by the previously published study by Panagiotakos et al. [14]. Although WC is not an index adjusted by hip size or height, it does reflect the condition of visceral obesity, which is closely related to the incidence of hypertension [27]. Also, because of the simplicity in obtaining this measurement directly, without any calculations, WC can be widely used to predict the development of hypertension.
The cut-off points for obesity indices are also controversial. The BMI cut-off points as recommended by the World Health Organization (WHO) are 25.0–29.9 kg/m2 as being overweight, and ≥30 kg/m2 for obesity [28]. While in China, the Working Group on Obesity in China (WGOC) recommends >24.0 kg/m2 as being overweight [29]. The WGOC has also developed WC cut-off points for the general Chinese population, which are 85.0 cm for men and 80.0 cm for women [29]. According to WHO, a WHR >0.9 for men and >0.85 for women is defined as abdominal obesity [30]. The study by Shao et al. [31], in a Chinese population, applied an optimal WHtR cut-off point of 0.5 for both sexes. Other studies have reported other values for anthropometric cut-off points [11,32,33].
In the present study, the optimal cut-off points for anthropometric indices in women with an ideal, or normal, blood pressure were 84.5 cm for WC, 25.4 kg/m2 for BMI, 0.859 for WHR, and 0.516 for WHtR, respectively. These findings are slightly higher than those reported by previously published studies. This difference could be related to the fact that the present study specifically recruited middle-aged women, between 40–70 years, and age group that was higher than in previous studies, which mainly included participants ≥18 years. Furthermore, the cut-off point for WHtR appeared to have the highest Youden’s index among the four indices in the present study (0.390), which indicated that the optimal cut-off point for WHtR had a better sensitivity and specificity for predicting the development of hypertension in women who initially has an ideal, or normal, blood pressure.
A previously published study by Hu et al. showed that the incidence of hypertension during a six-year follow-up in patients with normal blood pressure (<120/80 mmHg) and pre-hypertension (120–139/80–89 mmHg) was 9.8% and 32.7%, respectively [34]. Similarly, the findings of the present study showed that during the two-year follow-up period, the incidence of hypertension in the ideal blood pressure group (Group 1) and the pre-hypertensive group (Group 2) were 9.0% and 32.3%, respectively. Therefore, these findings have implications for the primary prevention of the development of hypertension in a pre-hypertensive population and with reduction of the incidence of hypertension in this population of middle-aged women. However, to the best of our knowledge, few studies have investigated the anthropometric indices and the optimal cut-off values in predicting hypertension in pre-hypertensive populations.
Some previously published studies have shown that WC, BMI, WHR, and WHtR were associated with the incidence of hypertension in pre-hypertensive populations [14,15]. In the present study, logistic regression analysis showed that all the four anthropometric indices studied were associated with the future development of hypertension in pre-hypertensive women during a two-year follow-up period. The findings of the study showed that the AUC for WC, BMI, WHR, and WHtR in pre-hypertensive women (which were 0.615, 0.587, 0.597, and 0.604, respectively) were lower than the AUC in women with a baseline ideal, or normal, blood pressure (which were 0.692, 0.593, 0.671, and 0.682, respectively. These findings indicate that anthropometric indices appear to be better in predicting the development and future incidence of hypertension in subjects with a baseline ideal, or normal, blood pressure. Furthermore, the WC in both the ideal blood pressure group (Group 1) and the pre-hypertensive group (Group 2) was still the better anthropometric indicator for the prediction of the development of hypertension (with a wider AUC). However, comparing the four obesity indices (WC, BMI, WHR, and WHtR) in relation to the population with an initial ideal, or normal, blood pressure, WC performed less well the pre-hypertensive population (Group 2).
Also, the findings of the present study showed that the optimal cut-off values for WC (91.5 cm), BMI (26.2 kg/m2), WHR (0.862), and WHtR (0.550) in pre-hypertensive women (Group 2) were higher than those in women with a baseline ideal, or normal, blood pressure (Group 1) with values of WC (84.5 cm), BMI (25.4 kg/m2), WHR (0.859), and WHtR (0.516), and were even higher than in the populations with an initial normal blood pressure in previously published studies. Because of these varied findings, it is likely that different standards might have been used for the definitions or measurements of anthropometric indices, classification of pre-hypertensive individuals, and different age groups, and ethnicities in different studies. However, in the present study, the cut-off values for all four of the anthropometric indices (WC, BMI, WHR, and WHtR) had a lower Youden’s index in the pre-hypertensive group (Group 2), which may indicate that the value of cut-off points for the anthropometric obesity indices were likely to be lower in pre-hypertensive women.
This study had several limitations. A cohort study was undertaken in an urban Chinese ethnic population of middle-aged women, aged between 40–70 years, which was a very specific study population. Whether the same conclusions can be applied to other ages, sex, or ethnic groups is unknown. Also, because of financial limitations, the size of the research sample was small, and for future studies, a larger participant sample size would be recommended. This study only used the baseline anthropometric data and did not consider variations in the anthropometric obesity parameters during the two-year follow-up, as recommended in the JNC 7 report [2]. The definition of ‘pre-hypertension’ in this study was equivalent to that of mildly elevated blood pressure or Stage 1 hypertension in the 2017 American College of Cardiology and American Heart Association (ACC/AHA) guidelines, which recommend non-pharmacological therapy in these cases [3]. Despite these limitations, the findings of this study are meaningful regarding their implications for the prevention of hypertension and the reduction in the incidence of hypertension in women in the age group and population studied.
Conclusions
In a cohort of middle-aged women in China, anthropometric indices of obesity, particularly the measurement of waist circumference (WC), were predictive of the development of hypertension during a two-year follow-up period, and therefore of the incidence of hypertension developing in this population. Although this study specifically included middle-aged Chinese women and had some limitations, the study findings demonstrated the value of anthropometric obesity indices as predictors of the development of hypertension. Also, the optimal cut-off values of anthropometric obesity indices in pre-hypertensive (ACC/AHA Stage 1 hypertensive) women were much higher compared with women who had a normal baseline blood pressure. The findings of the study also highlight the importance of controlling obesity in pre-hypertensive middle-aged women in the primary prevention of hypertension.
Acknowledgments
The authors gratefully acknowledge the numerous study investigators, fellows, and research coordinators who participated in the study.
Footnotes
Source of support: This study was funded by Tianjin City Health Bureau (Grant Number: 11KG133)
References
- 1.Liu LS. Writing Group of 2010 Chinese Guidelines for the Management of Hypertension [2010 Chinese guidelines for the management of hypertension] Zhonghua Xin Xue Guan Bing Za Zhi. 2010;8:701–43. [in Chinese] [PubMed] [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, et al. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee: The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 3.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2017 doi: 10.1161/HYP.0000000000000066. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 4.Luo W, Guo Z, Hu X, et al. A prospective study on association between 2 years change of waist circumference and incident hypertension in Han Chinese. Int J Cardiol. 2013;167(6):2781–85. doi: 10.1016/j.ijcard.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Decoda Study Group. Nyamdorj R, Qiao Q, Lam TH, et al. BMI compared with central obesity indicators in relation to diabetes and hypertension in Asians. Obesity. 2008;16(7):1622–35. doi: 10.1038/oby.2008.73. [DOI] [PubMed] [Google Scholar]
- 6.Huang X, Zhou Z, Liu J, et al. Prevalence, awareness, treatment, and control of hypertension among China’s Sichuan Tibetan population: A cross-sectional study. Clin Exp Hyperten. 2016;38(5):457–63. doi: 10.3109/10641963.2016.1163369. [DOI] [PubMed] [Google Scholar]
- 7.Martin-Rodriguez E, Guillen-Grima F, Martí A, Brugos-Larumbe A. Comorbidity associated with obesity in a large population: The APNA study. Obes Res Clin Pract. 2015;9(5):435–47. doi: 10.1016/j.orcp.2015.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Droyvold WB, Midthjell K, Nilsen TI, Holmen J. Change in body mass index and its impact on blood pressure: A prospective population study. Int J Obes. 2005;29(6):650–55. doi: 10.1038/sj.ijo.0802944. [DOI] [PubMed] [Google Scholar]
- 9.Paynter L, Koehler E, Howard AG, et al. Characterizing long-term patterns of weight change in China using latent class trajectory modeling. PLoS One. 2015;10(2):e0116190. doi: 10.1371/journal.pone.0116190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tuan NT, Adair LS, Stevens J, Popkin BM. Prediction of hypertension by different anthropometric indices in adults: the change in estimate approach. Public Health Nutr. 2010;13(5):639–46. doi: 10.1017/S1368980009991479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Castanheira M, Chor D, Braga JU, et al. Predicting cardiometabolic disturbances from waist-to-height ratio: Findings from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) baseline. Public Health Nutr. 2018;9:1–8. doi: 10.1017/S136898001700338X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Oliveira CM, Ulbrich AZ, Neves FS, et al. Association between anthropometric indicators of adiposity and hypertension in a Brazilian population: Baependi Heart Study. PLoS One. 2017;12(10):e0185225. doi: 10.1371/journal.pone.0185225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abshire DA, Mudd-Martin G, Moser DK, et al. Comparing measures of general and abdominal adiposity as predictors of blood pressure in college students. J Am Coll Health. 2018;66(1):51–60. doi: 10.1080/07448481.2017.1369092. [DOI] [PubMed] [Google Scholar]
- 14.Panagiotakos DB, Chrysohoou C, Pitsavos C, et al. Hierarchical analysis of anthropometric indices in the prediction of 5-year incidence of hypertension in apparently healthy adults: The ATTICA study. Atherosclerosis. 2009;206:314–20. doi: 10.1016/j.atherosclerosis.2009.02.030. [DOI] [PubMed] [Google Scholar]
- 15.Chiu YH, Wu SC, Tseng CD, et al. Progression of pre-hypertension, stage 1 and 2 hypertension (JNC 7): A population-based study in Keelung, Taiwan (Keelung Community-based Integrated Screening No. 9) J Hypertens. 2006;24(5):821–28. doi: 10.1097/01.hjh.0000222750.82820.19. [DOI] [PubMed] [Google Scholar]
- 16.Pitsavos C, Chrysohoou C, Panagiotakos DB, et al. Abdominal obesity and inflammation predicts hypertension among prehypertensive men and women: The ATTICA Study. Heart Vessels. 2008;23(2):96–103. doi: 10.1007/s00380-007-1018-5. [DOI] [PubMed] [Google Scholar]
- 17.Wang S, Liu Y, Li F, et al. A novel quantitative body shape score for detecting association between obesity and hypertension in China. BMC Public Health. 2015;15:7. doi: 10.1186/s12889-014-1334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galletti F, D’Elia L, Barba G, et al. High-circulating leptin levels are associated with greater risk of hypertension in men independently of body mass and insulin resistance: Results of an eight-year follow-up study. J Clin Endocrinol Metab. 2008;93(10):3922–26. doi: 10.1210/jc.2008-1280. [DOI] [PubMed] [Google Scholar]
- 19.Sung SH, Chuang SY, Sheu WH, et al. Adiponectin, but not leptin or high-sensitivity C-reactive protein, is associated with blood pressure independently of general and abdominal adiposity. Hypertens Res. 2008;31(4):633–40. doi: 10.1291/hypres.31.633. [DOI] [PubMed] [Google Scholar]
- 20.Kawamoto R, Kohara K, Tabara Y, et al. Insulin resistance and prevalence of prehypertension and hypertension among community-dwelling persons. J Atheroscler Thromb. 2010;17(2):148–55. doi: 10.5551/jat.2584. [DOI] [PubMed] [Google Scholar]
- 21.Tian H, Ma A, Li C, et al. Correlative factors of insulin resistance in essential hypertension. Hypertens Res. 2000;23(3):265–70. doi: 10.1291/hypres.23.265. [DOI] [PubMed] [Google Scholar]
- 22.Al-Sharbatti S, Shaikh R, Mathew E, et al. The use of obesity indicators for the prediction of hypertension risk among youth in the United Arab Emirates. Iran J Public Health. 2011;40(3):33–40. [PMC free article] [PubMed] [Google Scholar]
- 23.Lee CM, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: A meta-analysis. J Clin Epidemiol. 2008;61(7):646–53. doi: 10.1016/j.jclinepi.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 24.Can AS, Bersot TP, Gönen M, et al. Anthropometric indices and their relationship with cardiometabolic risk factors in a sample of Turkish adults. Public Health Nutr. 2009;12(4):538–46. doi: 10.1017/S1368980008002474. [DOI] [PubMed] [Google Scholar]
- 25.Anyanwu GE, Ekezie J, Danborno B, Ugochukwu AI. Body size and adiposity indicators and their relationship with blood pressure levels in Ibos of Nigeria. Niger J Med. 2011;20(1):44–51. [PubMed] [Google Scholar]
- 26.Rodrigues SL, Baldo MP, Mill JG. Association of waist-stature ratio with hypertension and metabolic syndrome: Population-based study. Arq Bras Cardiol. 2010;95(2):186–91. doi: 10.1590/s0066-782x2010005000073. [DOI] [PubMed] [Google Scholar]
- 27.Shimajiri T, Imagawa M, Kokawa M, et al. Revised optimal cut-of point of waist circumference for the diagnosis of metabolic syndrome in Japanese women and the influence of height. J Atheroscler Thromb. 2008;15(2):94–99. doi: 10.5551/jat.e540. [DOI] [PubMed] [Google Scholar]
- 28.Nguyen TT, Adair LS, He K, Popkin BM. Optimal cutoff values for overweight: Using body mass index to predict incidence of hypertension in 18- to 65-year-old Chinese adults. J Nutr. 2008;138(7):1377–82. doi: 10.1093/jn/138.7.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou BF Cooperative Meta-Analysis Group of the Working Group on Obesity in China. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults – study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci. 2002;15(1):83–96. [PubMed] [Google Scholar]
- 30.von Eyben FE, Mouritsen E, Holm J, et al. Intra-abdominal obesity and metabolic risk factors: A study of young adults. Int J Obes Relat Metab Disord. 2003;27(8):941–49. doi: 10.1038/sj.ijo.0802309. [DOI] [PubMed] [Google Scholar]
- 31.Shao J, Yu L, Shen X, et al. Waist-to-height ratio, an optimal predictor for obesity and metabolic syndrome in Chinese adults. J Nutr Health Aging. 2010;14(9):782–85. doi: 10.1007/s12603-010-0106-x. [DOI] [PubMed] [Google Scholar]
- 32.Midha T, Krishna V, Nath B, et al. Cut-off of body mass index and waist circumference to predict hypertension in Indian adults. World J Clin Cases. 2014;2(7):272–78. doi: 10.12998/wjcc.v2.i7.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shabnam AA, Homa K, Reza MT, et al. Cut-off points of waist circumference and body mass index for detecting diabetes, hypercholesterolemia and hypertension according to National Non-Communicable Disease Risk Factors Surveillance in Iran. Arch Med Sci. 2012;8(4):614–21. doi: 10.5114/aoms.2012.30284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hu J, Wu Y, Zhao L, et al. Natural variances in blood pressure category among Chinese adults. Hypertens Res. 2008;31(5):905–11. doi: 10.1291/hypres.31.905. [DOI] [PubMed] [Google Scholar]