SUMMARY
Objectives.
This prospective cohort study aimed to investigate effectiveness of Computerized Local Anesthesia (CLA) on oral implantology through estimation of pain and discomfort and total quantity of injected anesthetic.
Methods.
Forty-five consecutive patients whose treatment plan included immediate or late dental implants were included in this study. The main inclusion criteria comprised: previous implant intervention under conventional anesthesia (CA) during the past 3 years and no previous treatment of pain relief. All patients reported on a 0–10 scale on previous experience with CA, and new experience with CLA. The same CLA system, namely Single Tooth Anesthesia (STA) was used for all patients with half of the quantity normally used for CA. Data on quantity of anesthetic and reported ratings were collected and described. Potential associations and determinant variables were analysed through correlation analysis and regression models.
Results.
Out of 45 patients, 27 received post-extractive implant surgery whereas the rest 18 implant surgery on healed sites. The reported pain from STA (mean 1.6, SD 0.7) showed important difference as compared to CA (7.9, SD 1.2; z=5.873; p<0.0001). The comfort perceived during the STA ranged from 7 to 10 (mean 9.5, SD 0.79). A second injection with half of the initial dose was necessary in three cases only.
Conclusions.
STA system proved to be effective during interventions of dental implantology, by markedly reducing patients’ pain and discomfort and the total quantity of necessary anesthetic.
Keywords: computerized local anesthesia, single tooth anesthesia, pain and discomfort, intraligamentary anesthesia, dental anxiety
Introduction
Dental anxiety and dental phobia are phenomena which exhibit high prevalence worldwide. Self-reported dental anxiety is directly influenced by dental procedures-related pain (1). The following avoidance of dental care results in poor oral health and compromised quality of life (2). Recent studies have reported how dental anxiety is an understudied problem and have underlined the importance of implementing strategies to overcome such a common problem for both children and adult patients (2–4). Attempts to control dental pain and discomfort include a wide variety of psychological therapies and mechanical strategies, depending mainly on the type of dental treatment and structure of dental anxiety (5, 6). Among the fear provoking objects, the sight and sensation of anesthetic needle remains one of the most relevant (7, 8). Considering the fact that local anesthesia is a necessary procedure for pain control during the majority of dental treatments, management of needle – related anxiety is of outmost importance for an atraumatic and efficient therapy. To this end, new technologies are focused on enhancing anesthetic agents and delivery devices. The most promising technique consists of computerized local anesthesia (CLA) that combines controlled flow rate with anesthetic delivery pathway. The device Single Tooth Anesthesia (STA - Milestone Scientific Inc., Livingston, NJ, USA) is a computer-controlled provider of local anesthetic for specific use in dentistry. The painless injection is primarily due to slow computer-driven supply of anesthetic which results in mechanical insult remaining below the pain threshold of the patient. The hand piece has a pen-like shape which allows for an easy grip proximal to the needle and accurate insertion into the target site. In this way the operator has more control of the needle during the injection. The interface of the device is constituted by a series of visual LED indicators that, along with the relevant acoustic signals, guides the clinician during anesthetic procedures providing information regarding the speed supply, the amount of dispersed anesthetic and the needle position compared the target site. Previous research has reported that the STA system offers several advantages over conventional needles and traditional local anesthesia, including reduced trauma for injected tissues, enhanced tactile sensation and higher precision. Moreover, it is purported that STA requires lower quantity of anesthetic for obtaining the same anesthetic effect as conventional anesthesia especially considering its rapid onset (9, 10). This aspect could be particularly beneficial for patients suffering from systemic diseases that require peculiar treatment during local anesthesia. The increased comfort and better patient’s acceptance during STA have been extensively documented on pediatric dentistry research (11–15). Several comparative studies between CLA and conventional injections have been conducted also in periodontology, endodontics, prosthetics, maxillofacial surgery and restorative dentistry (15–19). To the best of our knowledge, effectiveness and potential advantages of STA on dental implant surgery have not been investigated so far.
Considering the increasing application of dental implants into everyday clinical practice, especially for post-extractive and immediate rehabilitation (20–22), estimation of anesthetic procedures that might reduce the total discomfort and anxiety related to the intervention is of particular interest.
The aim of the present study was to evaluate clinical benefits of STA system through patients’ self-reported pain and discomfort and measurement of required anesthetic quantity during dental implant surgery performed under STA.
Materials and methods
This clinical investigation was designed as a prospective cohort one-centre trial. Forty-five consecutive patients were enrolled based on the following inclusion criteria: older than 18 years, treatment planning involving dental implants, previous dental implant surgery with conventional anesthetic methods during the last 3 years, no previous pain relief therapy, no previous STA injections, no systemic or local conditions that might be a contraindication for dental implant therapy. Data on gender, age, number of extracted teeth (when performed), type of surgery (post-extraction or edentulous ridge, open flap or flapless, number of inserted implants), jaw (mandible or maxilla) and site of implant placement (sextant of the mouth, number of tooth) were collected and recorded.
Each patient filled two questionnaires, each one consisting of several questions to be answered on a 10-degree scale (1 not at all, 10 extremely). The first questionnaire was submitted during the appointment before the treatment and aimed at quantification of pain and discomfort during previous dental implant surgery performed under conventional local anesthesia and expectations from computerized anesthesia. It included the following questions: Q1. How much do you fear the traditional anesthesia?; Q2. How much pain did you feel with conventional anesthesia procedures performed during your previous dental implant treatment?; Q3. After receiving information on computerized anesthesia, how much do you fear this technique?
The second questionnaire was delivered at the end of the surgical intervention performed under STA and consisted of two questions: Q4. How much pain did you feel with STA?; Q5. How much comfortable is computerized anesthesia? (1 not at all, 10 extremely). Patients were also asked on their feeling of surrounding soft tissue anesthesia and perioral numbness feeling. They were informed that STA was being tested and written informed consent was obtained from all of them. The followed procedures were in accordance with the ethical standards of the responsible committee of human experimentation and with the Helsinki Declaration of 1975, as revised in 1983.
Surgical procedure
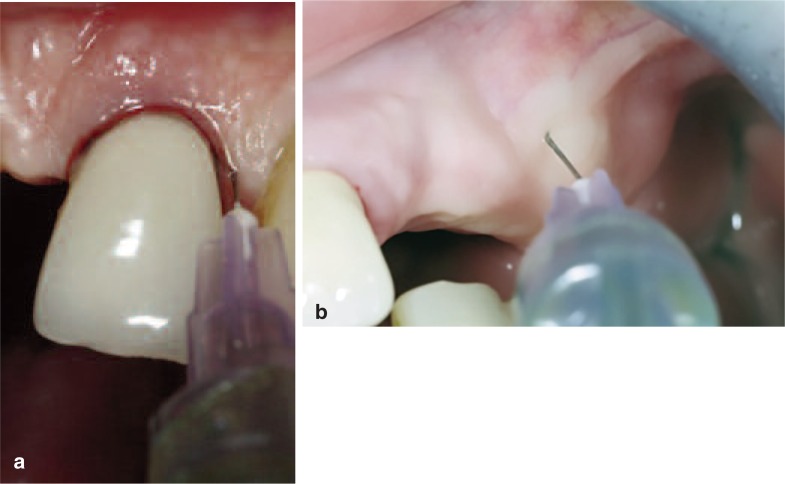
All patients underwent one or several sessions of oral hygiene debridement prior to surgery. The STA was used in normal mode flow and with Control Flow. The STA needle has a diameter of 30 gauge and length of 0.5 inches. No topical anesthetic was used. Articaine hydrochloride 4% combined with epinephrine 1: 100,000 (1.8 ml cartridges) was administered to all patients. In case of healed alveolar crests, two injections were performed, one on the vestibular side and the other on the oral side, both midway between the centre crest and the muco-gengival line (Figure 1a). For post-extractive sites, one single vestibular intraligamentary injection was performed for incisors and canines, whereas premo-lars and molars received one vestibular and one oral injection (Figure 1b). In order to test the hypothesis that STA requires a reduced quantity of anesthetic for providing the same effect as conventional anesthesia, patients were injected with half of the total quantity normally used during conventional technique. Namely, one cartridge was injected in both post-extractive or healed sites. In cases of two adjacent teeth, the total quantity of anesthetic was augmented by half cartridge. Additional anesthetic was administered in case of reported pain during the intervention. Data on quantity of delivered anesthetic during the first injection and second injection (when necessary) were recorded on customized data sheets.
Figure 1.
(a) Intraligamentary injection performed on existing teeth; (b) Crestal injection performed on edentulous sites.
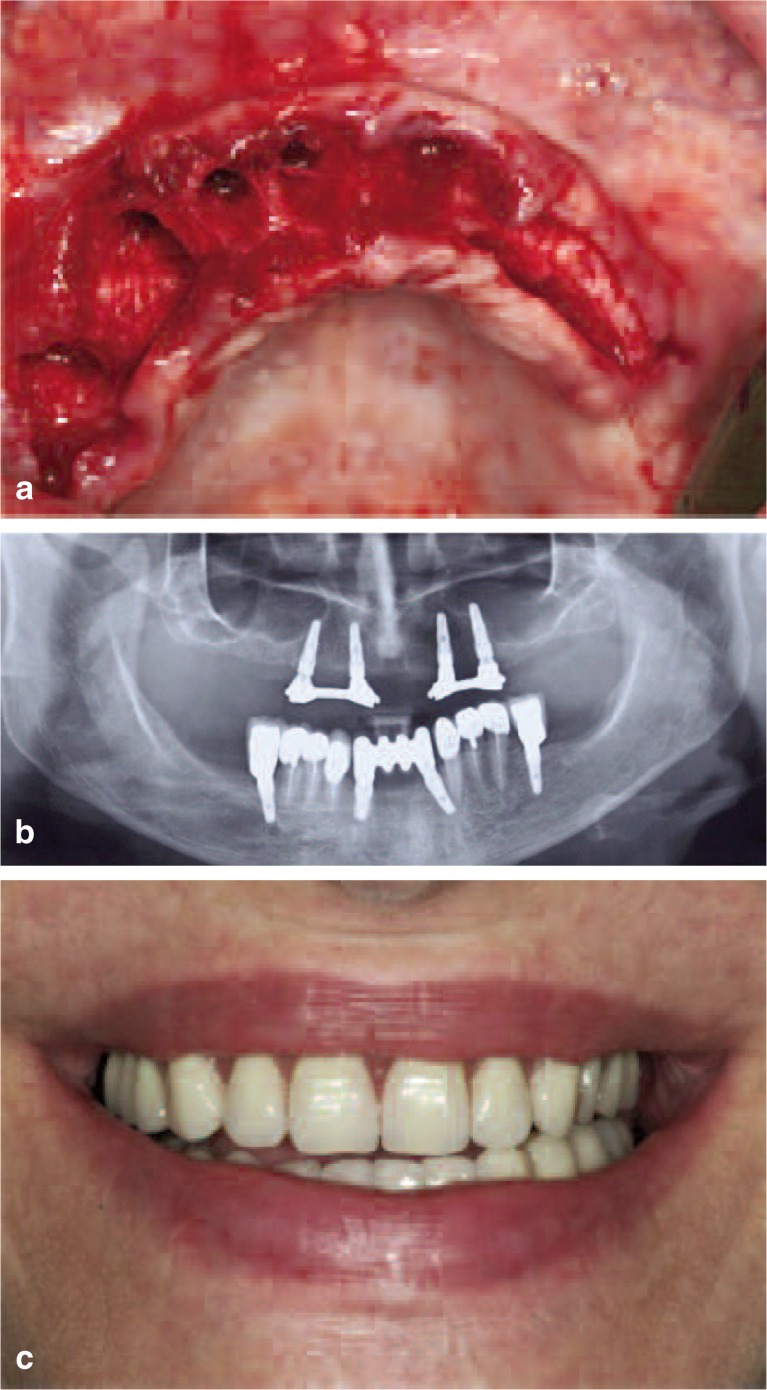
All post-extractive implants were placed through a flapless technique, while a full thickness flap with no lateral incisions was elevated for implants inserted in healed edentulous sites (Figure 2a). Patients received dental implants with length varying from 8 mm to 11.5 mm and diameters from 3.75 mm to 5 mm (Figure 2b). Each implant was inserted following the manufacturer’s instructions and the dedicated kit of surgical instruments. All implants were covered by healing screw. Open flap sites were sutured, whereas flapless sites were healed by secondary intention. All interventions were performed by the same senior surgeon (G.FR) having an extensive experience with STA system. Prosthetic rehabilitation was achieved through removable and/or fixed prosthesis (Figure 2c).
Figure 2.
(a) Clinical view prior to implant insertion. Crestal incision was performed on the healed site of the alveolar crest, whereas no other flap was elevated; (b) Radiographic image after implant placement; (c) Clinical view after prosthetic rehabilitation.
Statistical analysis
Sample size calculation was performed by conducting a preliminary investigation on 20 patients who reported on a zero-to-ten scale the fear from conventional anesthesia, which was considered the primary outcome. Results indicated a mean of 6.8 (SD=3.9). Sample size was calculated through the command “power one-mean” on Stata, aiming to improve the score on STA system by 5 as compared to conventional anesthesia. A total of 45 patients were included, accounting for 6 (10%) potential dropouts. Demographic data of patients and intervention characteristics were described calculating means, medians and standard deviations for continuous variables and proportion for categorical variables. Difference on pain rates between conventional anesthesia and STA was tested through Wilcoxon signed-rank test. Single and multiple linear regression models, accounting also for potential interaction, were fitted in order to assess any influence on perceived pain and fear of variables such as age, sex, second time injection, quantity of anesthetic, post-extraction intervention and pain from traditional anesthesia. Regression model coefficients and 95% confidence intervals were calculated for different potential predictive variables. Potential correlations were investigated also through Pearson’s correlation coefficient. All tests were two-tailed and all statistical comparisons were conducted at .05 level of significance. Analyses were performed by an independent operator using Stata version 13 (Stata Statistical Software, release 13.0, StataCorp).
Results
The study population of 45 patients included 22 males (49%) and 23 females (51%) aged 32 to 70 years (overall mean age 54.8 years, SD 9.2 years). Twenty-seven patients (60%) received post-extractive implant surgery whereas the rest 18 (40%) implant surgery on healed sites. Out of all post-extractive interventions, 16 were single teeth, 8 included 2 adjacent teeth, 1 included 3 adjacent teeth and 2 included 6 teeth. Interventions on healed sites comprised 16 single-tooth areas which were restored by single implants, one case of two adjacent missing teeth and one of three adjacent missing teeth areas. For 42 patients interventions and STA were performed on one sextant only, whereas for the remaining three, on two adjacent sextants. A second injection during the intervention was deemed necessary and performed in three cases, one being post-extractive. For each of these patients, the additional injected quantity was half cartridge (0.9 ml). Data on sites of anesthesia and quantity of injected anesthetic are presented in Table 1. Fear from conventional anesthesia resulted in quite high levels ranging from a minimum of 5 to a maximum of 10 (mean 8.4, SD 1.5). Immediately after having information on STA, patients reflected a markedly reduced fear on anesthesia (Q3 mean 3, SD 1.65). The mean pain level experienced during STA technique (mean 1.6, SD 0.7) showed highly significant difference as compared to pain reported on conventional technique (7.9, SD 1.2; z=5.873; p<0.0001). The comfort perceived during the STA ranged from 7 to 10 with a mean of 9.5 (SD 0.79). Pain and fear from conventional anesthesia exhibited important positive correlation (Pearson’s coefficient 0.64), whereas pain from STA and pain from conventional anesthesia did not show interaction (Pearson’s coefficient −0.07).
Table 1.
Data on type, site and quantity of administered STA.
| Number of patients (percentage) | ||
|---|---|---|
| Type of injection | ||
| Intraligamentary | 27 (60%) | |
| Crestal | 18 (40%) | |
|
| ||
| Site of injection* | ||
| Maxillary anterior | 11 (23%) | |
| Maxillary posterior | 19 (40%) | |
| Mandibular anterior | 5 (10%) | |
| Mandibular posterior | 13 (27%) | |
|
| ||
| Quantity of injected anesthetic (ml) | ||
| 0.9 | 19 (42%) | |
| 1.8 | 13 (29%) | |
| 2.5 | 9 (20%) | |
| 3.6 | 4 (89%) | |
Three patients received anesthesia on two adjacent sextants.
Relationship between potential determinant variables such as age, gender, jaw, type of injection, quantity of anesthetic and pain during STA did not result in any significant association in both univariate and adjusted multivariate models. Comfort experienced with STA seemed to be influenced by age, younger patients reporting higher levels of comfort (coeff=−0.04; 95%CI=−0.06 to −0.01; p=0.004). Similarly, it was slightly influenced by pain reported during conventional anesthesia, those experiencing more pain during conventional injection tempted to consider more comfortable STA (coeff=0.19; 95%CI=−0.05 to 0.38; p=0.05). Independently of the injection site, number of injections and total quantity of injected anesthetic, no numbness of lips or face were reported by patients.
Discussion
The natural progress of medical care through a century where the single individual is the centre of society has moved the priorities of dental care providers towards the accomplishment of patient’s requirements and satisfaction. Apart from implementation of effective and scientifically-based therapies, dentists should assure that their interventions are well accepted by patients and do not compromise their quality of life. Despite the high frequency and routinely performance for many decades the injection remains one of the most important sources of anxiety. Similarly, dental treatments still rank almost on top of the big fears perceived by patients (23, 24). Oral surgery is a particularly stressful condition that causes relevant increase in pain perception, anxiety and expected suffering (25). Such a situation can also impair patient’s capacity of understanding provided important information (26). Moreover, considering that pain experienced by patients in oral surgery is influenced by the presurgical anxiety (27), control of stress and anxiety are essential steps toward appropriate patient management and high-quality care. CLA has already proved to be efficient in pediatric dentistry, whereas its use on adult patients and specifically in dental implantology has been partially investigated.
The present study estimated pain and anxiety on patients undergoing dental implant therapy with STA system and investigated also the potential benefit of this system in terms of reducing quantity of anesthetic. Although the study was not of cross-over design, it included patients who had previously undergone similar surgery under CA and reported on their experience in terms of pain and anxiety during CA and STA injection, serving as their own controls. With the aim of reducing bias, patients were asked to report on CA before they had information on STA and not on the same day of surgery (27). The time lap between the previous CA intervention and their rating might have modified the memory of their experience, therefore the reporting on differences between the two anesthetic systems was not considered similar to the comparative result of a randomized study. This difference served to roughly quantify the experience with STA with reference to CA. Considering these aspects, calculation of sample size was also settled seeking a big difference between the two mean ratings. Nevertheless, the observed advantage of STA against CA tempts to be fairly realistic, considering also that in the majority of cases, with time, pain experiences are remembered less intensive than immediately after the intervention. Testing the hypothesis of reduced quantity of anesthetic provided interesting results, accounting for the fact that the half of the normal quantity had to be potentiated with an additional injection only in 3 patients out of 45. This effect might be attributed to the high precision of STA which detects the injection site, providing visual orientation for the operator. It is well known that local anesthetic dosage varies between operators and patients, and depends on several factors. However, scientific evidence reports that dental practitioners appear to have an inadequate knowledge about local anesthetics maximum-dose and dose calculations (28). Appropriate dosage of local anesthetic is very often neglected and derives from a poor knowledge of anatomy and pharmacology of anesthetic (29, 30).
The problem becomes even more important in patients with cardiovascular diseases. Considering that unintended intravascular injections might occur and central plasma epinephrine levels are influenced by local anesthesia, applying local anesthetic injections that reduce anxiety and total quantity of anesthetic is of particular benefit (31, 32). Due to the reduced total quantity of anesthetic, STA injection is followed by a shorter latency and sufficient duration of the anesthesia for performing the surgical intervention. As reported also in other studies (10), after CLA the post-surgical feeling of numbness and soft tissue anesthesia is importantly reduced and this is particularly appreciated by patients who tempt more and more to consider dental appointment as part of their busy day schedule.
Conclusions
STA used for surgical dental implant placement in both post-extractive alveolus and healed alveolar crest resulted in very low levels of pain and discomfort for the patients. From a point of view of clinical comfort, STA seems to be highly beneficial and very well accepted by the patients who can go through the surgical intervention with less fear, anxiety and disruptive behaviour. Furthermore, the total quantity of required anesthetic is markedly reduced, due to a very precise injection and consequent rapid onset. As a result, the numbness feeling of surrounding soft tissues is reduced and the patient can recover faster after the intervention. As patient’s safety, comfort and satisfaction are of outmost importance for all medical interventions, further studies that investigate potentials of STA on dental treatments are encouraged.
Footnotes
Conflicts of interest
The Authors declare that no conflicts of interest exist.
References
- 1.Heaton LJ. Self-reported Dental Anxiety is Associated With Both State Anxiety and Dental Procedure-Related Pain. J Evid Based Dent Pract [Internet]. 2017 Mar;17(1):45–7. doi: 10.1016/j.jebdp.2017.01.007. [cited 2017 Oct 8]; [DOI] [PubMed] [Google Scholar]
- 2.Seligman LD, Hovey JD, Chacon K, Ollendick TH. Dental anxiety: An understudied problem in youth. Clin Psychol Rev [Internet]. 2017 Jul;55:25–40. doi: 10.1016/j.cpr.2017.04.004. [cited 2017 Oct 8]; [DOI] [PubMed] [Google Scholar]
- 3.Cianetti S, Lombardo G, Lupatelli E, Pagano S, Abraha I, Montedori A, et al. Dental fear/anxiety among children and adolescents. A systematic review. 2017 Jun;18(2):121–30. doi: 10.23804/ejpd.2017.18.02.07. doi.org [Internet]. ARIESDUE SRL; [cited 2017 Oct 8]; [DOI] [PubMed] [Google Scholar]
- 4.Gordon D, Heimberg RG, Tellez M, Ismail AI. A critical review of approaches to the treatment of dental anxiety in adults. J Anxiety Disord [Internet]. 2013 May;27(4):365–78. doi: 10.1016/j.janxdis.2013.04.002. [cited 2017 Oct 8]; [DOI] [PubMed] [Google Scholar]
- 5.Kalemaj Z, Buti J, Deregibus A, Canuto RM, Maggiora M, Debernardi CL. Aligning Effectiveness, Secretion of Interleukin 1β and Pain Control During Fixed Orthodontic Treatment with Self-Ligating Appliances and Supplemental Vibrational Appliances. A Randomized Controlled Clinical Trial. J Biomed [Internet]. 2017;2(1):25–33. [cited 2017 May 20]; [Google Scholar]
- 6.van Houtem CMHH, van Wijk AJ, Boomsma DI, Ligthart L, Visscher CM, De Jongh A. The factor structure of dental fear. Eur J Oral Sci [Internet]. 2017 Jun;125(3):195–201. doi: 10.1111/eos.12343. [cited 2017 Oct 8]; [DOI] [PubMed] [Google Scholar]
- 7.Hakim H, Razak IA. ScientificWorldJournal [Internet]. Vol. 2014. Hindawi; 2014. Oct 16, Dental fear among medical and dental undergraduates; p. 747508. [cited 2017 Oct 8]; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.J Am Dent Assoc [Internet] 6. Vol. 128. Elsevier; 1997. Jun 1, Four dimensions of fear of dental injections; pp. 756–62. [cited 2017 Oct 23]; [DOI] [PubMed] [Google Scholar]
- 9.Friedman MJ, Hochman MN. A 21st century computerized injection system for local pain control. Compend Contin Educ Dent [Internet]. 1997 Oct;18(10):995–1000. 1002–3. [cited 2017 Oct 23]; quiz 1004. [PubMed] [Google Scholar]
- 10.Beneito-Brotons R, Peñarrocha-Oltra D, Ata-Ali J, Peñarrocha M. Med Oral Patol Oral Cir Bucal [Internet]. 3. Vol. 17. Medicina Oral S.L; 2012. May 1, Intraosseous anesthesia with solution injection controlled by a computerized system versus conventional oral anesthesia: a preliminary study; pp. e426–9. [cited 2017 Oct 24]; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Allen KD, Kotil D, Larzelere RE, Hutfless S, Beiraghi S. Comparison of a computerized anesthesia device with a traditional syringe in preschool children. [cited 2017 Oct 23]. [PubMed]
- 12.Gibson RS, Allen K, Hutfless S, Beiraghi S. The Wand vs. traditional injection: a comparison of pain related behaviors. Pediatr Dent [Internet]. 2000;22(6):458–62. [cited 2017 Oct 23]; [PubMed] [Google Scholar]
- 13.Tahmassebi JF, Nikolaou M, Duggal MS. A comparison of pain and anxiety associated with the administration of maxillary local analgesia with Wand and conventional technique. Eur Arch Paediatr Dent [Internet]. 2009 Jun;10(2):77–82. doi: 10.1007/BF03321604. [cited 2017 Oct 23]; [DOI] [PubMed] [Google Scholar]
- 14.Kandiah P, Tahmassebi JF. Comparing the onset of maxillary infiltration local anaesthesia and pain experience using the conventional technique vs. the Wand in children. BDJ [Internet]. 2012 Nov 9;213(9):E15–E15. doi: 10.1038/sj.bdj.2012.988. [cited 2017 Oct 23]; [DOI] [PubMed] [Google Scholar]
- 15.Kwak E-J, Pang N-S, Cho J-H, Jung B-Y, Kim K-D, Park W. Computer-controlled local anesthetic delivery for painless anesthesia: a literature review. J Dent Anesth Pain Med [Internet]. 2016 Jun;16(2):81. doi: 10.17245/jdapm.2016.16.2.81. [cited 2017 Oct 24]; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yenisey M. J Appl Oral Sci [Internet]. 5. Vol. 17. Faculdade De Odontologia De Bauru - USP; 2009. Oct, Comparison of the pain levels of computer-controlled and conventional anesthesia techniques in prosthodontic treatment; pp. 414–20. [cited 2017 Oct 23]; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nicholson JW, Berry TG, Summitt JB, Yuan CH, Witten TM. Pain perception and utility: a comparison of the syringe and computerized local injection techniques. Gen Dent [Internet]. 2001;49(2):167–73. [cited 2017 Oct 23]; [PubMed] [Google Scholar]
- 18.Loomer PM, Perry DA. J Am Dent Assoc [Internet] 3. Vol. 135. Elsevier; 2004. Mar 1, Computer-controlled delivery versus syringe delivery of local anesthetic injections for therapeutic scaling and root planing; pp. 358–65. [cited 2017 Oct 23]; [DOI] [PubMed] [Google Scholar]
- 19.Özer S, Yaltirik M, Kirli I, Yargic I. A comparative evaluation of pain and anxiety levels in 2 different anesthesia techniques: locoregional anesthesia using conventional syringe versus intraosseous anesthesia using a computer-controlled system (Quicksleeper) Oral Surg Oral Med Oral Pathol Oral Radiol [Internet]. 2012 Nov;114(5):S132–9. doi: 10.1016/j.oooo.2011.09.021. [cited 2017 Oct 24]; [DOI] [PubMed] [Google Scholar]
- 20.Grassi FR, Capogreco M, Consonni D, Bilardi G, Buti J, Kalemaj Z. Immediate occlusal loading of one-piece zirconia implants: five-year radiographic and clinical evaluation. Int J Oral Maxillofac Implants [Internet]. 30(3):671–80. doi: 10.11607/jomi.3831. [cited 2017 Jan 10]; [DOI] [PubMed] [Google Scholar]
- 21.Villa F, Grassi FR, Popovic M, Sordillo R, Kalemaj Z. Immediately Loaded, Implant-Supported Overdentures Retained by a Milled Bar: An Up-to-5-Year Retrospective Clinical Study. Int J Periodontics Restorative Dent [Internet]. 37(5):e261–9. doi: 10.11607/prd.3344. [cited 2017 Oct 24]; [DOI] [PubMed] [Google Scholar]
- 22.Kalemaj Z, Scarano A, Valbonetti L, Rapone B, Grassi FR. Bone response to four dental implants with different surface topography: a histologic and histometric study in minipigs. Int J Periodontics Restorative Dent. 2016 Sep-Oct;36(5):745–54. doi: 10.11607/prd.2719. [DOI] [PubMed] [Google Scholar]
- 23.Manani G, Alberton L, Bazzato MF, Berengo M, Da Corte Zandatina S, Di Pisa A, et al. Analysis of an anxiolytic technique applied in 1179 patients undergoing oral surgery. Minerva Stomatol [Internet]. 2005 Oct;54(10):551–68. [cited 2017 Oct 24]; [PubMed] [Google Scholar]
- 24.de St Georges J. How dentists are judged by patients. Dent Today [Internet]. 2004 Aug;23(8):96, 98–9. [cited 2017 Oct 24]; [PubMed] [Google Scholar]
- 25.Facco E, Zanette G, Favero L, Bacci C, Sivolella S, Cavallin F, et al. Anesth Prog [Internet]. 1. Vol. 58. American Dental Society of Anesthesiology; 2011. Toward the validation of visual analogue scale for anxiety; pp. 8–13. [cited 2017 Oct 24]; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eli I, Schwartz-Arad D, Bartal Y. Anxiety and Ability to Recognize Clinical Information in Dentistry. J Dent Res [Internet]. 2008 Jan;87(1):65–8. doi: 10.1177/154405910808700111. [cited 2017 Oct 24]; [DOI] [PubMed] [Google Scholar]
- 27.Eli I, Schwartz-Arad D, Baht R, Ben-Tuvim H. Effect of anxiety on the experience of pain in implant insertion. Clin Oral Implants Res [Internet]. 2003 Feb;14(1):115–8. doi: 10.1034/j.1600-0501.2003.140115.x. [cited 2017 Oct 24]; [DOI] [PubMed] [Google Scholar]
- 28.Saudi J Dent Res [Internet] 1. Vol. 5. Elsevier; 2014. Jan 1, Local anesthetics dosage still a problem for most dentists: A survey of current knowledge and awareness; pp. 49–53. [cited 2017 Oct 24]; [Google Scholar]
- 29.Blanton PL, Jeske AH. Misconceptions involving dental local anesthesia. Part 1: Anatomy. Tex Dent J [Internet]. 2002 Apr;119(4):296–300. 302–4, 306–7. [cited 2017 Oct 24]; [PubMed] [Google Scholar]
- 30.Jeske AH, Blanton PL. Misconceptions involving dental local anesthesia. Part 2: Pharmacology. Tex Dent J [Internet]. 2002 Apr;119(4):310–4. [cited 2017 Oct 24]; [PubMed] [Google Scholar]
- 31.Lipp M, Dick W, Daubländer M, Fuder H, Stanton-Hicks M. Exogenous and endogenous plasma levels of epinephrine during dental treatment under local anesthesia. Reg Anesth [Internet]. 18(1):6–12. [cited 2017 Oct 24]; [PubMed] [Google Scholar]
- 32.Liau FL, Kok S-H, Lee J-J, Kuo R-C, Hwang C-R, Yang P-J, et al. Cardiovascular influence of dental anxiety during local anesthesia for tooth extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod [Internet]. 2008 Jan;105(1):16–26. doi: 10.1016/j.tripleo.2007.03.015. [cited 2017 Oct 24]; [DOI] [PubMed] [Google Scholar]