SUMMARY
Background.
The purpose of the study is to evaluate the effectiveness of Low-Level Laser Therapy in reducing joint and muscle pain in patients with acute and chronic temporomandibular dysfunction.
Materials and methods.
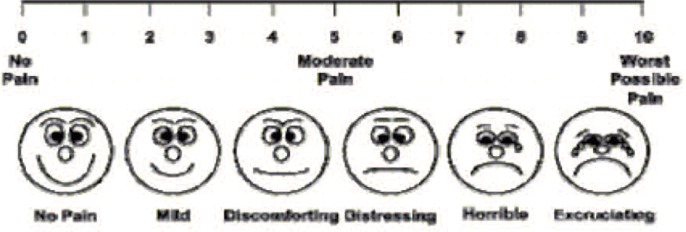
The study was conducted on a sample of 180 patients. The sample was divided into two groups according to the time of onset of the disease: acute TMD (<6 months) and chronic TMD (> 6 months). The treatment for all patients provided for the irradiation with Diode Laser Wiser Doctor Smile with tip plane wave at wavelength of 830 nm, continuous beam to 40nW diameter and radius of 6 mm. The irradiated areas were the joint area, temporal, masseter and pterygoid. The irradiation time for each zone was 60s.The protocol adopted consisted of two weekly treatment for six weeks. Pain assessment was performed using the Visual Analog Scale (VAS), in which different scores (s) depending accused of pain by the patient: s0 no pain, s1–3 mild pain, s4–6 moderate pain, s7–9 severe pain and s10 excessive pain. The pain monitoring was performed before treatment, after 15 days and after one month.
Results.
The sample included 80 patients with acute TMD and 100 with chronic TMD. The sample belonging to acute TMD group before treatment, was distributed as follows: 0% in s0; 12,5% in s1–3; 31.3% in s4–6; 53.6% in s7–9 and 2.5% in s10. After 15 days the distribution was was as follows: 6.25% in s0; 47.5% in s1–3; 20% in s4–6; 26.3% in s7–9 and 0% in s10. After 30 days the sample was well distributed: 35% in s0; 45% in 1–3; 10% in s4–6; 10% in s7–9 and 0% in s10. The sample belonging to the chronic TMD group, at time zero, was as follows: 0% at s0; 48% in S1–3; 35% in s4–6; 15% in s7–9 and 2% in s10. After 15 days the distribution was: 29% in s0; 28% in S1–3; 33% in s4–6; 10% in s7–9 and 0% in s10. After 30 days the sample was well distributed: 45% in s0; 36% in S1–3; 15% in s4–6; 4% in s7–9 and 0% in s10.
Conclusions.
The Low-Level-Laser-Therapy is a valuable tool that can significantly decrease the perception of pain in patients with temporomandibular joint dysfunction, acute and chronic.
Keywords: TMD, laser therapy, orofacial pain
Introduction
Temporo-mandibulardisorders (TMD) are defined, by the American Academy of Orofacial Pain, as a pathological condition affecting the TMJ, teeth and muscles associated with the stomatognathic system. The incidence in the population varies between 40 and 60%, with a woman/man ratio of 2.5:1. The age of onset of the symptomatology is observed in women between 40 and 50 years and in men between 30 and 40 years. The symptoms most frequently reported by affected individuals are noises or pains, affecting the TMJ, temporal area, masseterin and cervical, parafunctions and diffuse facial tension. In the physical examination there is often a marked achiness during the palpation of temporal, masseters and pterygoids muscles. As demonstrated by the International literature, the most frequent predisposing factor is an incorrect occlusal condition. The triggering of this pathology occurs when non-optimal occlusion is associated with cofactors such as traumas, parafunctions or emoziona stress escapable of destabilizing the pre-existing equilibrium of the stomatognathic system. The conventional therapeutic approach to the treatment of TMD involves a first phase of symptomatic resolution through occlusal devices able to rebalance the mandibular position in the glenoid pit and then a second phase of elimination of the etiological factors triggering the pathology (1). Laser therapy has been increasingly used in the treatment of musculoskeletal pains in the various branches of medicine (2, 3). In particular, it has been noticed that when laser light is used at low intensity with an emission of monochromatic infrared rays (Low-level laser Therapy - LLLT), the irradiated tissue undergoes a series of beneficial effects: increate pain tolerance by modifying the membrane potential of nociceptors (4); vasodilation with consequent reduction of local inflammatory edema (5); increase in cellular metabolism and acceleration of tissue healing speed (6). These effects lead to a reduction in the inflammatory state of the tissue with a reduction in perceived pain (7). The purpose of the article is to assess-whether the application of LLLT to the masticatory muscles is able to alleviate the pain perceived by those affected by TMD.
Materials and methods
A sample of 180 subjects with TMD who had not undergone any occlusal or pharmacological therapy was selected. The sample was divided into two groups: group A composed of individuals with acute dysfunction (onset<6 months), and group B composed of individuals with chronic TMD (onset> 6 months). Treatment for each patient involved the irradiation of 60s for each area (articular area, temporal, masseterin and pterygoid muscles) (Figures 1, 2, 3, 4, 5) twice a week for six weeks. The laser used was a WiserDoctor Smile diode (Figure 6) with an AB 2799 flat wave tip at a wavelength of 830 nm, a continuous beam of 40nW and a radius of 6 mm. Pain perception was observed using the VAS scale (Visual analog scale, Figure 7), attributing different scores (s) according to the pain reported by the subject: s0 absence of pain; s1–s3 mild pain; s4–s6 moderate pain; s7–s9 high pain; s10 unbearable pain.
Figure 1.
Irradiation of the right joint area.
Figure 2.
Irradiation of the right masseterin area.
Figure 3.
Irradiation of the right temporal area.
Figure 4.
Irradiation of the left temporal area.
Figure 5.
Irradiation of the left masseterin area.
Figure 6.
Diode laser Wiser Doctor Smile.
Figure 7.
VAS Scale.
The study protocol considered the application of the VAS scale to each patient following three phases: at zero time (before treatment), after 15 days and finally 30 days after the starting of laser therapy. Each patient was strongly advised not to take pain medication and anti-inflammatory drugs during the whole duration of the treatment. The results were elaborated through a statistical analysis evaluating the distribution of the patients in the different classes of pain in the three different classes of pain: time zero, after 15 days and after 30 days.
Results
The sample consisted of 80 patients with acute DTMs and 100 with chronic DTMs. At each recording of the perceived pain with the VAS scale, each group was subdivided into 5 subgroups according to the recorded score (s0; s1–3, s4–6, s7–9 and s10).
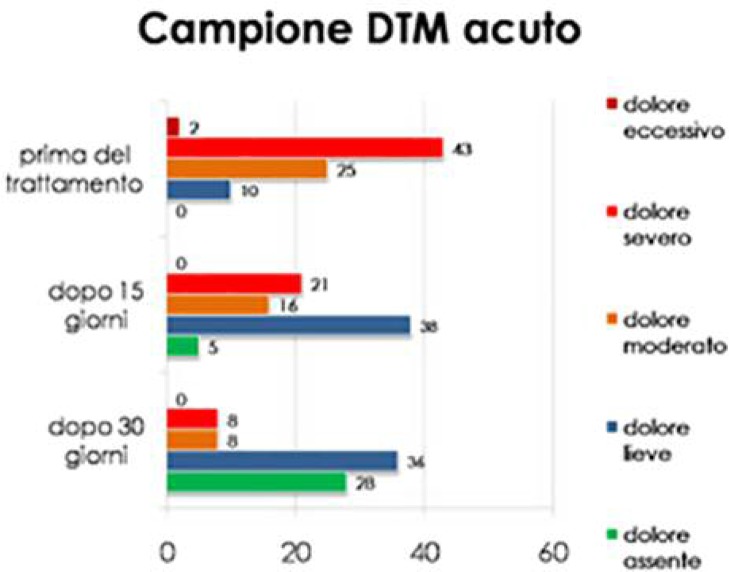
Group A at time zero was distributed as follows: 0% in s0; 12.5% in s1–3; 31.3% in s4–6; 53.6% in s7–9 and 2.5% in s10. After 15 days the distribution was: 6.25% in s0; 47.5% in s1–3; 20% in s4–6; 26.3% in s7–9 and 0% in s10. After 30 days the distribution was: 35% in s0; 45% in s1–3; 10% in s4–6; 10% in s7–9 and 0% in s10 (Table 1 and Chart 1).
Table 1.
Group A results.
| TMD acute | Absence of pain | Mild pain | Moderate pain | High pain | Excessive pain |
|---|---|---|---|---|---|
| after 30 days | 28 | 36 | 8 | 8 | 0 |
| after 15 days | 5 | 38 | 16 | 21 | 0 |
| Time 0 | 0 | 10 | 25 | 43 | 2 |
Chart 1.
Group A results.
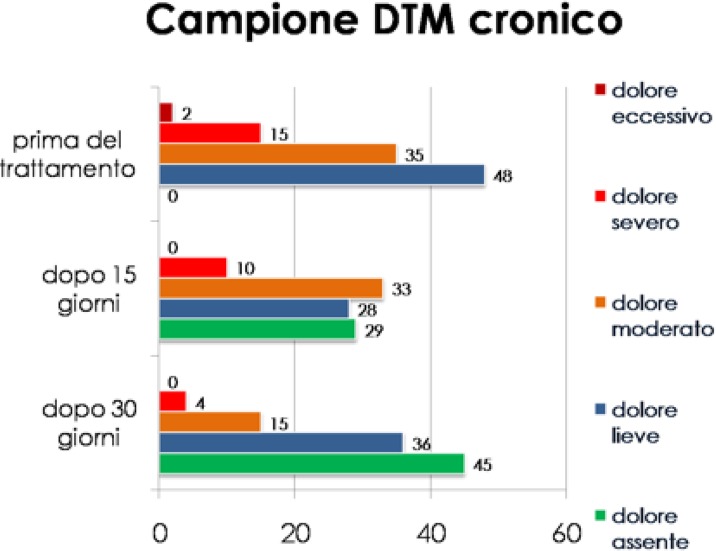
Regarding group B, the distribution at time zero was: 0% in s0; 48% in s1–3; 35% in s4–6; 15% in s7–9 and 2% in s10. After 15 days the distribution was: 29% in s0; 28% in s1–3; 33% in s4–6; 10% in s7–9; 0% in s10. After 30 days: 45% in s0; 36% in s1–3; 15% in s4–6; 4% in s7–9 and 0% in s10 (Table 2 and Chart 2).
Table 2.
Group B results.
| TMD Chronic | Absence of pain | Mild pain | Moderate pain | High pain | Excessive pain |
|---|---|---|---|---|---|
| after 30 days | 45 | 36 | 15 | 4 | 0 |
| after 15 days | 29 | 28 | 33 | 10 | 0 |
| Pre-treatment | 0 | 48 | 35 | 15 | 2 |
Chart 2.
Group B results.
Discussion and conclusions
The results obtained reveal a significant improvement in the pain symptoms reported by patients with both acute and chronic DTM. Observing the progress of the subgroups expressed in the graphs with different colors, it can be observed that the excessive and severe pain end to decrease considerably, going from zero to 15 days, drastically decreasing after 30 days. Likewise, it can be noticed that the cases of complete absence of pain increase significantly, ranging from time zero to time 1 and 2. Another very interesting result is that in the group with acute pain the symptomatology is much more evident than in the group with chronic pathology.
According to the obtained results, it can be asserted that the LLLT is a valid therapeutic helping to olduring the early stages of temporomandibular disorders treatment as it allows to alleviate the musculoskeletal pain felt by affected patients. However, it should be stressed that laser therapy can not replace the gnathological treatment through occlusal devices, since the two therapeutic approaches have very different purpose (8). On one hand the laser reduces the perception of pain (9) as it raises the stimulation threshold of nociceptors, facilitates the elimination of inflammatory toxins, ensures a better blood flow and a rapid cellular turnover useful for the resolution of the inflammatory state (10); on the other, the occlusal therapy mechanically reconditions the position of the mandibular condyles within the glenoid pits. The use of both these therapeutic solutions at the same time, turns out to be a valid aid in the treatment of TMDs.
References
- 1.Da Cunha LA, Firoozmand LM, da Silva AP, Camargo SE, Oliveira W. Efficacy of low-level laser therapy in the treatment of temporomandibular disorder. Int Dent J. 2008;58(4):213–217. doi: 10.1111/j.1875-595x.2008.tb00351.x. [DOI] [PubMed] [Google Scholar]
- 2.Conti PC. Low level laser therapy in the treatment of temporomandibular disorders (TMD): a double-blind pilot study. Cranio. 1997;15(2):144–149. doi: 10.1080/08869634.1997.11746005. [DOI] [PubMed] [Google Scholar]
- 3.Mazzetto MO, Carrasco TG, Bidinelo EF, de Andrade Pizzo RC, Mazzetto RG. Low intensity laser application in temporomandibular disorders: a phase I double-blind study. Cranio. 2007;25(3):186–192. doi: 10.1179/crn.2007.029. [DOI] [PubMed] [Google Scholar]
- 4.Goldman JA, Chiapella J, Casey H, Bass N, Graham J, McClatchey W, Dronavalli RV, Brown R, Bennett WJ, Miller SB, Wilson CH, Pearson B, Haun C, Persinski L, Huey H, Muckerheide M. Laser therapy of rheumatoid arthritis. Lasers Surg Med. 1980;1(1):93–101. doi: 10.1002/lsm.1900010110. [DOI] [PubMed] [Google Scholar]
- 5.Sandoval MC, Mattiello-Rosa SM, Soares EG, Parizotto NA. Effects of laser on the synovial fluid in the inflammatory process of the knee joint of the rabbit. Photomed Laser Surg. 2009;27(1):63–69. doi: 10.1089/pho.2007.2216. [DOI] [PubMed] [Google Scholar]
- 6.Kulekcioglu S, Sivrioglu K, Ozcan O, Parlak M. Effectiveness of low-level laser therapy in temporomandibular disorder. Scand J Rheumatol. 2003;32(2):114–118. doi: 10.1080/03009740310000139. [DOI] [PubMed] [Google Scholar]
- 7.Shirani AM, Gutknecht N, Taghizadeh M, Mir M. Lowlevel laser therapy and myofacial pain dysfunction syndrome: a randomized controlled clinical trial. Lasers Med Sci. 2009;24(5):715–720. doi: 10.1007/s10103-008-0624-5. [DOI] [PubMed] [Google Scholar]
- 8.Dworkin SF, Sherman J, Mancl L, Ohrbach R, LeResche L, Truelove E. Reliability, validity, and clinical utility of the research diagnostic criteria for Temporomandibular Disorders Axis II Scales: depression, non-specific physical symptoms, and graded chronic pain. J Orofac Pain. 2002;16(3):207–220. [PubMed] [Google Scholar]
- 9.Kogawa EM, Kato MT, Santos CN, Conti PC. Evaluation of the efficacy of low-level laser therapy (LLLT) and the microelectric neurostimulation (MENS) in the treatment of myogenic temporomandibular disorders: a randomized clinical trial. J Appl Oral Sci. 2005;13(3):280–285. doi: 10.1590/s1678-77572005000300015. [DOI] [PubMed] [Google Scholar]
- 10.Gur A, Sarac AJ, Cevik R, Altindag O, Sarac S. Efficacy of 904 nm gallium arsenide low level laser therapy in the management of chronic myofascial pain in the neck: a double-blind and randomize-controlled trial. Lasers Surg Med. 2004;35(3):229–235. doi: 10.1002/lsm.20082. [DOI] [PubMed] [Google Scholar]