Abstract
Objective
The World Health Organization (WHO) recently proposed an Integrated Care for Older People approach to guide health systems and services in better supporting functional ability of older people. A knowledge gap remains in the key elements of integrated care approaches used in health and social care delivery systems for older populations. The objective of this review was to identify and describe the key elements of integrated care models for elderly people reported in the literature.
Design
Review of reviews using a systematic search method.
Methods
A systematic search was performed in MEDLINE and the Cochrane database in June 2017. Reviews of interventions aimed at care integration at the clinical (micro), organisational/service (meso) or health system (macro) levels for people aged ≥60 years were included. Non-Cochrane reviews published before 2015 were excluded. Reviews were assessed for quality using the Assessment of Multiple Systematic Reviews (AMSTAR) 1 tool.
Results
Fifteen reviews (11 systematic reviews, of which six were Cochrane reviews) were included, representing 219 primary studies. Three reviews (20%) included only randomised controlled trials (RCT), while 10 reviews (65%) included both RCTs and non-RCTs. The region where the largest number of primary studies originated was North America (n=89, 47.6%), followed by Europe (n=60, 32.1%) and Oceania (n=31, 16.6%). Eleven (73%) reviews focused on clinical ‘micro’ and organisational ‘meso’ care integration strategies. The most commonly reported elements of integrated care models were multidisciplinary teams, comprehensive assessment and case management. Nurses, physiotherapists, general practitioners and social workers were the most commonly reported service providers. Methodological quality was variable (AMSTAR scores: 1–11). Seven (47%) reviews were scored as high quality (AMSTAR score ≥8).
Conclusion
Evidence of elements of integrated care for older people focuses particularly on micro clinical care integration processes, while there is a relative lack of information regarding the meso organisational and macro system-level care integration strategies.
Keywords: geriatric medicine, rehabilitation medicine
Strengths and limitations of this study.
While existing reviews summarise evidence for effectiveness of integrated care approaches, this review of reviews summarised evidence on the elements (components) of integrated care interventions for older adults, providing important data to inform implementation activities.
This review used a systematic search method to identify reviews of integrated care interventions for older adults and represents a component of a broader programme of work being undertaken by the WHO to support implementation of the WHO Integrated Care for Older People approach.
A single author responsible for screening and quality appraisal may have introduced rater some bias.
Background
Health and demographic profiles of the global population are changing rapidly. In particular, life expectancy is increasing and fertility rates are decreasing.1 These changing health profiles are culminating in rapid population ageing—from 2015 to 2050, the proportion of the global population aged 60 years and over will nearly double.2 While increased life expectancy may be a worthy aspiration, older people are not necessarily experiencing functional ability with longevity; that is Healthy Ageing.2 An increasing proportion of the global burden of disease is now attributed to non-communicable physical, sensory and cognitive impairments; increasing the disability burden experienced by older people, particularly in low- and middle-income settings.1 Further, older people commonly experience multimorbidity, particularly those who are socioeconomically disadvantaged.3–5
Rapid population ageing coupled with an increasing proportion of older people with significant loses in intrinsic capacity and long-term complex conditions creates major challenges for health systems, which have been historically designed to provide episodic and curative healthcare.6 7 This historical approach to healthcare no longer aligns with the current and future needs of the population. The World Health Organization (WHO) World Report on Ageing and Health and subsequent Global Strategy and Action Plan on Ageing and Health advocate for major reforms to health and long-term care systems to support healthy ageing.2 8 Such reforms are critical and urgent in order to achieve the goals of the UN Sustainable Development Agenda, in particular the Sustainable Development Goal 3 for health and well-being, for which the foundation is universal health coverage. WHO recommends that health and social care services should be targeted towards preventing and managing declines in intrinsic capacity and improving functional ability in older people, rather than supporting a siloed and often disjointed approach to management of individual health conditions.6
WHO defines integrated care as ‘services that are managed and delivered so that people receive a continuum of health promotion, disease prevention, diagnosis, treatment, disease-management, rehabilitation and palliative care services, coordinated across the different levels and sites of care within and beyond the health sector, and according to their needs throughout the life course.9 Accordingly, integrated care strategies can target different levels of service provision: clinical (micro) level, service/organisational (meso) level or system (macro) level.6 10 Integration of health and social care is widely advocated as a way to improve person-centred and system-centred outcomes for the increasing numbers of older people with varying and sometimes complex health needs.11–18 However, the evidence for strategies to achieve care integration across micro, meso and macro levels remains limited.10 19–22 The WHO Framework on Integrated People-Centred Health Services provides a whole-of-system roadmap for policymakers to drive health system and service reform to better support integrated care and health across the life course by optimising the way services are designed, funded, managed and delivered.9 17 In the context of providing integrated care for older people specifically, WHO has proposed the Integrated Care for Older People (ICOPE) approach to inform the application of the Framework on Integrated People-Centred Health Services in the context of older people and bridge the gap between what is presumed to be best practice care for older people and emerging evidence.2 The ICOPE approach supports providing health and social care services by promoting governance and integrated service models that maintain or prevent avoidable declines in older people’s intrinsic capacity and functional ability. To achieve this, WHO suggests that systems and services need to be organised, coordinated and delivered around the preferences, needs and goals of older people, rather than the structural needs of services themselves.6 Specifically, the WHO ICOPE approach recommends comprehensive assessments and integrated care plans; shared decision-making and goal setting; support for self-management; multidisciplinary teams; unified information or data-sharing systems; community linkages or integration; and supportive leadership, governance and financing mechanisms.
While there has been an increasing focus on developing and evaluating integrated care models across the life course at different levels of the health system23 and the establishment of a taxonomy of elements for implementing integrated care,24 there is currently a knowledge gap regarding the requisite elements of integrated care approaches that address the needs of older people. This knowledge gap hinders the implementation of the WHO ICOPE approach and the evaluation of its effectiveness, particularly the transferability of any recommendations concerning how to improve outcomes for older people across care settings and geographies. Recognising the heterogeneity in integrated care interventions, there is a need to better understand the components of contemporary integrated care approaches.25–27
WHO has approached this knowledge gap over the last 4 years through a phased programme of work to define and refine the ICOPE approach as a means to ultimately support its implementation in health and social care systems across Member States. An initial phase of evidence synthesis was undertaken by WHO in 2014 where a detailed review of the literature (from 2000 to 2014) on health and social care needs of older people and responsiveness of health and long-term care systems was undertaken and summarised in the World Report on Ageing and Health.2 Subsequently, a steering group, with international experts on integrated care, was established to produce background papers on essential micro and meso level elements of integrated health and social care services.6 In 2016, a face-to-face meeting with experts was organised in Japan as preparatory work for the G7 summit. In this meeting, experts reviewed the evidence synthesised in the background papers and recommended three core micro level elements for implementing the WHO ICOPE approach: (1) one assessment—every older people should undergo comprehensive assessments; (2) one goal—optimising functional ability; and (3) one care plan—care plans should be shared among all providers.6 The experts also recommended that the implementation of these core micro level elements required support from meso and macro level factors. Therefore, a second wave of evidence review (the current review) was performed to identify essential elements of integrated care models that would enable implementation of the WHO ICOPE approach.
The aim of this review was to conduct a review of reviews evaluating integrated care interventions for older people. The review did not seek to synthesise outcomes of integrated care approaches, but rather to identify and appraise the types of integrated care approaches reported in the literature and their intrinsic elements, in people aged ≥60 years in any setting or level of the health and long-term care system. Here, we refer to an ‘element’ as a discrete component of an integrated care intervention. The evidence review formed part of a larger programme of work to identify elements and reach global consensus on key elements for implementation of the ICOPE approach (see: http://www.who.int/ageing/health-systems/icope/icope-consultation/en/).
Methods
Design
A review of reviews using systematic search methods was conducted under predefined criteria established by the authors and reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.28 A PRISMA checklist has been included (refer to online supplementary file 1). No protocol paper was developed.
bmjopen-2017-021194supp001.pdf (116.3KB, pdf)
Patient and public involvement
While this review focuses on patient-centred care, patients were not involved in planning or conduct of the review.
Search strategy
A systematic search was performed in MEDLINE via Ovid and the Cochrane database in June 2017. MEDLINE was searched from 1 January 2015 to 1 June 2017 and Cochrane was searched from inception by PPV. Non-Cochrane reviews published before 2015 were excluded to identify only recent reviews (and therefore contemporary evidence) and maximise the likely quality of the included reviews.29 Searches were limited to reviews only and used Medical Subject Headings terms and specific keywords relevant to integrated care (eg, care coordination, collaborative care, transmural care, multidisciplinary care)30 and older populations (eg, ageing, elderly, frail elderly).24 Full search strategies are included in online supplementary file 2. Grey literature sources were not included in the search strategy.
bmjopen-2017-021194supp002.pdf (76.1KB, pdf)
Eligibility
Reviews were selected if they included studies that: (1) evaluated integrated care strategies at the micro, meso or macro levels; (2) targeted older people (≥60 years); (3) were published in a peer-reviewed journal in English; and (4) used one of the review designs (eg, systematic, meta-analysis, rapid, qualitative) as described by Grant and Booth.31 Reviews were excluded if they focused on an intervention, for example, self-management support, but without any coordinated care activity among care providers. Here, we refer to ‘care-providers’ as any paid or unpaid (eg, family) person who provides health or social care to an older person.
Selection and data extraction
Review selection, assessment against eligibility criteria and quality assessment were performed by one reviewer (PPV) using Covidence systematic review software. Data extraction was performed initially by one author (PPV). Titles and abstracts of the search yield were screened and full texts of potentially relevant papers were reviewed against eligibility criteria. Data were extracted using a standardised data extraction form. The following information was collected from eligible reviews: year of publication, review methodology (aim, review design and design of its included studies, number of primary studies included, number of databases searched, method of quality appraisal and analysis), characteristics of included reviews (number of included participants, type of participants and countries/regions), intervention characteristics (study population, type of provider(s) included, type of integrated care intervention(s) and elements of the interventions) and type of outcome measures reported. Thereafter, a second author (AMB) screened the extracted information for accuracy.
Quality assessment
Methodological quality of included reviews was appraised using the Assessment of Multiple Systematic Reviews (AMSTAR 1) tool.32 One researcher (PPV) assessed the quality of the included reviews.
Data synthesis and analysis
A narrative synthesis was used for reporting, owing to the heterogeneity of study designs, interventions and outcome measures reported across the primary studies. For each included review, details about the type of integrated care intervention, specific elements of the intervention and outcome measures were reported by PPV and verified by AMB. The Rainbow Model of Integrated Care and associated taxonomy of key elements for implementation of integrated care approaches were used as the coding frame for the type of interventions and their elements.10 24 After completing the primary data analysis, reviewers (AMB, JAT, IAC) then considered alignment of the coded elements within the strategies of the WHO Framework on Integrated People-Centred Health Services.9 17 All other review-related characteristics were narratively synthesised for comparison across reviews to highlight common findings.
Results
Review selection
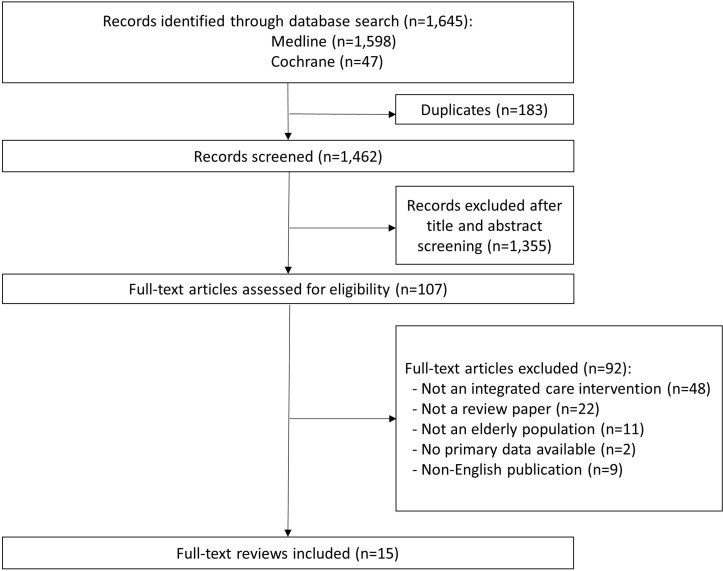
Overall, the search yielded 1645 citations, of which 1462 were screened at the title and abstract level with 107 considered as potentially relevant and underwent full-text screening for inclusion. Ninety-two articles were subsequently excluded, resulting in a total of 15 reviews to be included (figure 1).
Figure 1.
Flow chart of search outcomes and study selection.
Characteristics of the included reviews
Types of reviews
The characteristics of the 15 included reviews are shown in table 1. Reviews were published between 2005 and 2016, and included 11 (73%) systematic reviews,33–43 of which six incorporated meta-analyses or metasynthesis,35–38 40 41 and six were Cochrane reviews and four non-systematic reviews.44–47 Three reviews (20%) included only randomised controlled trials (RCT),33 37 39 while 10 reviews (65%) included both RCTs and non-RCTs.34–36 41–43 45–48
Table 1.
Characteristics of included reviews (n=15)
| Review (year) | Aim | Review design (design of included studies) | Number of primary studies included | Time frame of primary studies | Countries where primary studies were undertaken (n*) | Regions where primary studies were undertaken (n*) | Total number of participants in primary studies | Number of databases searched | Search terms provided | Language restrictions | Quality or bias assessment | Evidence synthesis |
| Alldred et al33 (2016) | To assess the effect of interventions to optimise medicines prescribing for older people living in care homes | Systematic review (RCTs) |
12 | 1994–2015 | Australia (1); Canada (4); Germany (1); Norway (1); Sweden (1); and USA (13) | Europe (3); North America (17); Oceania (1) | 10 953 | 6 | Yes | No | Cochrane collaboration’s risk of bias tool; GRADE | Narrative and tabular |
| Berthelsen and Kristensson34 (2015) | To describe the content and effects of case management interventions for informal caregivers of older adults | Systematic review (RCTs and non-RCTs) |
7 | 1997–2011 | Finland (2); The Netherlands (1); and USA (4) | Europe (3); North America (4) | 6956 | 3 | Yes | NS | GRADE | Narrative and tabular |
| Brown et al35 (2015) | To assess the effectiveness of day hospitals for older people in preventing death, disability, institutionalisation and improving subjective health status | Systematic review and meta-analysis (RCTs and non-RCTs) |
16 | 1962–2008 | Australia (1); Canada (1); Finland (1); Hong Kong (1); New Zealand (1); UK (8) and USA (3) | Asia (1); Europe (9); North America (4); Oceania (2) | 3689 | 23 | Yes | No | Cochrane collaboration’s risk of bias tool; GRADE | Narrative and tabular |
| Cochrane et al36 (2016) | To assess the effects of home care rehabilitation services for maintaining and improving the functional independence of older adults | Systematic review and meta-analysis (RCTs and non-RCTs) |
2 | 2013–2015 | Australia (1); Norway (1) | Europe (1); Oceania (1) | 811 | 9 | Yes | No | Cochrane collaboration’s risk of bias tool; GRADE | Narrative and tabular |
| Costa-de Lima et al44 (2015) | To search the literature for multiprofessional, cost-effective intervention programmes for elderly people in primary care settings | Literature review (NS) |
32 | 1993–2012 | NS | NS | NS | 10 | Yes | Yes | None | Narrative and tabular |
| Deschodt et al45 (2016) | To explore the structure and processes of interdisciplinary geriatric consultation teams | Scoping review (RCTs and non-RCTs) |
25 | 1983–2013 | Belgium (1); Canada (2); France (3); Germany (1); The Netherlands (1); Taiwan (1); UK (2); and USA (14) | Asia (1); Europe (8); North America (16) | NS | 3 | Yes | Yes | None | Narrative and tabular |
| Ellis et al37 (2011) | To assess the effectiveness of comprehensive geriatric assessment in hospital for older adults admitted as an emergency | Systematic review and meta-analysis (RCTs) |
22 | 1984–2007 | Australia (1); Canada (4); Germany (1); Norway (1); Sweden (1); and USA (13) | Europe (3); North America (17); Oceania (1) | 10 315 | 6 | Yes | NS | Cochrane collaboration’s risk of bias tool | Narrative and tabular |
| Fan et al46 (2015) | To review the effectiveness of interventions targeting the elderly population in reducing emergency department utilisation | Literature review (RCTs and non-RCTs) |
36 | 1993–2013 | Australia (9): Canada (8); France (1); Italy (1); Singapore (1); UK (1); USA (15) | Asia (1); Europe (3); North America (23); Oceania (9) | NS | 5 | Yes | Yes | Assessment tool developed by the Effective Public Health Practice Project | Narrative and tabular |
| Frank and Wilson47 (2015) | To review Canadian models of care for frail seniors provided in primary care settings | Overview (RCTs and non-RCTs) |
6 | 2006–2015 | Canada (6) | North America (6) | NS | 2 | No | NS | None | Narrative |
| Handoll et al38 (2009) | To assess the effects of multidisciplinary rehabilitation for older patients with proximal fracture that has been surgically repaired | Systematic review and meta-analysis (RCTs and non-RCTs) |
13 | 1986–2008 | Australia (3); Canada (1); Spain (1); Sweden (2); Taiwan (1); UK (4) | Asia (1); Europe (7); North America (1); Oceania (3) | 2498 | 6 | Yes | No | Cochrane collaboration’s risk of bias tool | Narrative and tabular |
| Hickman et al39 (2015) | To identify multidisciplinary team interventions to optimise health outcomes for older people in acute care settings | Systematic review (RCTs) |
6 | 2005–2014 | Australia (1); Belgium (1); France (1); Finland (1); Spain (1); Taiwan (1) | Asia (1); Europe (4); Oceania (1) | 1558 | 3 | Yes | Yes | None | Narrative and tabular |
| Ke et al40 (2015) | To explore nurses’ views regarding implementing advance care planning for older people | Systematic review and metasynthesis of qualitative evidence |
18 | 1993–2013 | Australia (2); Canada (2); New Zealand (1); South Africa (1); Switzerland (1); UK (7); USA (4) | Africa (1); Europe (8); North America (6); Oceania (3) | NS | 4 | Yes | Yes | None | Narrative and tabular |
| Lowthian et al41 (2015) | To examine the effectiveness of emergency department community transition strategies | Systematic review and meta-analysis (RCTs and non-RCTs) |
11 papers concerning 9 studies | 1996–2013 | Australia (6); Canada (4); Hong Kong (1); Scotland (1); Singapore (1) | Asia (2); Europe (1); North America (4); Oceania (6) | 22 502 | 3 | Yes | No | Cochrane collaboration’s risk of bias tool | Narrative and tabular |
| McClure et al42 (2005) | To assess the effectiveness of population-based interventions for reducing fall-related injuries among older people | Systematic review (RCTs and non-RCTs) | 6 | 1996–2006 | Australia (1); Denmark (1); Norway (1); Sweden (2); Taiwan (1) | Asia (1): Europe (4); Oceania (1) | NS | 9 | Yes | No | Checklist of the Cochrane EPOC review group | Narrative and tabular |
| Phelan et al43 (2015) | To search for intervention strategies that have any measurable effect on acute care hospitalisations among community-dwelling adults with dementia | Systematic review (RCTs and non-RCTs) |
10 papers concerning 9 studies | 2002–2010 | Finland (1); The Netherlands (1); UK (1); USA (6) | Europe (3); North America (6) | 1332 | 9 | Yes | Yes | None | Narrative and tabular |
*n, number of studies may not sum to the number of primary studies included, as primary studies may have been undertaken in more than one country.
EPOC, Cochrane Effective Practice and Organisation of Care Review Group; GRADE, Grades of Recommendations, Assessment, Development and Evaluation; NS, not stated; RCT, randomised controlled trial.
Samples in included reviews
Collectively, the reviews included 219 primary studies from 222 papers, with the number of primary studies included in reviews ranging from 2 to 36, and the number of participants from 811 to 22 502. The number of participants in six reviews could not be determined.40 42 44–47
Geographic regions of primary studies
The region where the largest number of primary studies originated was North America (n=89, 47.6%), followed by Europe (n=60, 32.1%) and Oceania (n=31, 16.6%). The most common countries were the USA (n=60, 32.1%), Canada (n=29, 15.5%), Australia (n=28, 15%) and the UK (n=25, 13.4%).
Integrated care interventions and their elements
The types of integrated care interventions are summarised in table 2. Most reviews reported on a combination of interventions that were clinically (micro level) or professionally (meso level) focused (n=11, 73%). Only one review reported on a combination of an organisational/service (meso) and system (macro) level integrated care intervention.42 The reported interventions were all multifaceted, with most containing two or more discrete elements that consistently featured case management and multidisciplinary planning and/or care delivery. The most commonly reported elements of the integrated care models reported were multidisciplinary team care (n=11, 73%), comprehensive assessment (n=11, 73%), case management (n=5, 33%), systematic risk factor screening (n=5, 33%), patient education (n=4, 27%), professional education (n=4, 27%), home visits (n=4, 27%) and medication review (n=4, 27%). These eight most common elements aligned with strategies of the WHO Framework on Integrated People-Centred Health Services, including: (1) creating and enabling environment; (2) coordinating services within and across sectors; and (3) reorienting the model of care. Across the included reviews, the following care providers were frequently represented in the integrated care interventions: nurses (n=12, 80%), physiotherapists (n=10, 67%), general practitioners (n=9, 60%) and social workers (n=9, 60%). The majority of included reviews reported on hospitalisation (n=11, 73%), physical functioning (eg, self-reported activities of daily living, dependence, and so on) (n=9, 60%), cost and resource utilisation (n=7, 47%) and mortality (n=7, 47%) as outcomes of the intervention(s).
Table 2.
Summary of elements of the integrated care models reported across reviews
| Review (year) | Study population(s) and (setting) | Health system level of intervention(s) reported | Type(s) of integrated care intervention(s) | Key care or service elements within integrated care intervention(s) (n*) |
Discipline providers included | Description of control(s) | Outcome(s) reported | |||||||||||
| NU | GT | PH | GP | PA | PT | OT | DT | PS | SW | MS | OS | |||||||
| Alldred et al33 (2016) | People aged ≥65 years (living in care homes) | Professional (meso) level | Case management; multidisciplinary team care | Medication review (10); multidisciplinary team (4); professional education (5); clinical information management (1) | ● | ● | ● | ● | ● | ● | Usual care (by general practitioner) | Mortality; hospitalisation; adverse drug events; HRQoL; cost and resource utilisation | ||||||
| Berthelsen and Kristensson34 (2015) | Informal caregivers to people aged >65 years (community care settings) | Clinical (micro) level | Case management; individual multidisciplinary care plan; self-management | Case management (4); patient education (3) | ● | ● | ● | ● | Usual care | Quality of care; physical functioning; psychological functioning | ||||||||
| Brown et al35 (2015) | People aged ≥60 years (receiving medical care in medical day hospitals) | Clinical (micro) level; professional (meso) level | Individual multidisciplinary care plan; multidisciplinary team care | Multidisciplinary team (7); comprehensive assessment (5) | ● | ● | ● | ● | ● | ● | ● | ● | No comprehensive care; domiciliary care; or comprehensive care | Mortality; cost and resource utilisation; patient satisfaction; physical functioning | ||||
| Cochrane et al36 (2016) | People aged ≥65 years (living in own home) | Clinical (micro) level | Patient education; information provision to clients; individual multidisciplinary care plan; self-management | Medication review (1); comprehensive assessment (1); case management (1) | ● | ● | Usual care (standard home care) | Mortality; hospitalisation; HRQoL; cost and resource utilisation; physical functioning | ||||||||||
| Costa-de Lima et al44 (2015) | People aged ≥60 years (community-dwelling people receiving care in primary care settings) | Clinical (micro) level; professional (meso) level | Case management; multidisciplinary care team; individual multidisciplinary care plan; interprofessional education | Case management; multidisciplinary team; comprehensive assessment; systematic risk screening; home visits; medication review; patient education; professional education | ● | ● | ● | ● | ● | ● | ● | ● | ● | NS | Mortality; hospitalisation; patient satisfaction; physical functioning | |||
| Deschodt et al45 (2016) | Geriatric patients aged ≥60 years (within hospital settings—medical, surgical and intensive care units and emergency departments) | Clinical (micro) level; professional (meso) level | Case management; individual multidisciplinary care plan; multidisciplinary team care | Comprehensive assessment; systematic risk screening; multidisciplinary team | ● | ● | ● | ● | ● | ● | ● | NS | Physical functioning; psychological functioning; social functioning | |||||
| Ellis et al37 (2011) | People aged ≥65 years (admitted to hospital) | Clinical (micro) level; professional (meso) level | Case management; individual multidisciplinary care plan; multidisciplinary team care | Comprehensive assessment (22); multidisciplinary team (22); discharge planning (4) | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | Usual care | Mortality; hospitalisation; cost and resource utilisation; physical functioning; psychological functioning | ||
| Fan et al46 (2015) | People aged ≥60 years (community based (home or outpatients) and hospital based (emergency department or hospital ward)) | Clinical (micro) level; professional (meso) level | Case management; individual multidisciplinary care plan; multidisciplinary team care | Multidisciplinary team (7); comprehensive assessment (5) | ● | ● | ● | ● | ● | ● | NS | Hospitalisation; cost and resource utilisation | ||||||
| Frank and Wilson47 (2015) | People aged ≥64 years (community-based care) | Clinical (micro) level; professional (meso) level | Case management; individual multidisciplinary care plan; multidisciplinary team care | Case management (2); comprehensive assessment (2); multidisciplinary team (3); systematic risk screening (1); discharge planning (1) | ● | ● | ● | ● | ● | NS | Hospitalisation; quality of care; cost and resource utilisation | |||||||
| Handoll et al38 (2009) | People aged ≥50 years with surgically repaired proximal femur fracture (inpatient, home and ambulatory care) | Clinical (micro) level; professional (meso) level | Case management; individual multidisciplinary care plan; multidisciplinary team care | Comprehensive assessment (6); multidisciplinary team (12); discharge planning (9); home visits (2) | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | Usual care | Mortality; hospitalisation; adverse events; physical functioning | ||
| Hickman et al39 (2015) | People aged ≥65 years (acute care inpatient setting) | Clinical (micro) level; professional (meso) level | Case management; individual multidisciplinary care plan; self-management; multidisciplinary team care | Comprehensive assessment (4); multidisciplinary team (6); discharge planning (4); medication review (1); patient education (1) | ● | ● | ● | ● | ● | ● | ● | ● | ● | NS | Hospitalisation; adverse events; HRQoL; physical functioning | |||
| Ke et al40 (2015) | Nurses caring for older people (hospital, community-based services and facility-based services) |
Clinical (micro) level; professional (meso) level | Centrality of client needs; patient education; interaction between professional and client; active client participation; multidisciplinary team care | Patient education; professional education | ● | ● | ● | ● | ● | NA | NS | |||||||
| Lowthian et al41 (2015) | People aged ≥65 years (emergency department) | Clinical (micro) level; professional (meso) level | Case management; individual multidisciplinary care plan; multidisciplinary team care | Comprehensive assessment (7); multidisciplinary team (1); discharge planning (8); systematic risk screening (3) | Usual care | Hospitalisation; physical functioning | ||||||||||||
| McClure et al42 (2005) | People aged ≥65 years (population based in a community) | Organisational (meso) level; system (macro) level | Social value creation; stakeholder management; interorganisational governance; population needs assessment | Population health interventions (5); policy interventions (1); professional education (1); home visits (3) | ● | ● | ● | Similar population | Mortality; hospitalisation; adverse events; cost and resource utilisation | |||||||||
| Phelan et al43 (2015) | People aged ≥55 years with dementia (community dwelling) | Clinical (micro) level; professional (meso) level | Case management; multidisciplinary team care; individual multidisciplinary care plan; interprofessional education | Case management (4); multidisciplinary team (4); comprehensive assessment (4); home visits (1); interprofessional education (1) | NS | Hospitalisation | ||||||||||||
*n, number of studies is reported where stated by the review authors. Not all reviews reported the number of primary studies that include specific care or service elements.
DT, dietitian; GP, general practitioner; GT, geriatrician; HRQoL, health-related quality of life; MS, medical specialist; NA, not applicable; NS, not stated; NU, nurse; OS, other staff; OT, occupational therapist; PA, pharmacist; PH, physician; PS, psychologist; PT, physiotherapist; SW, social worker.
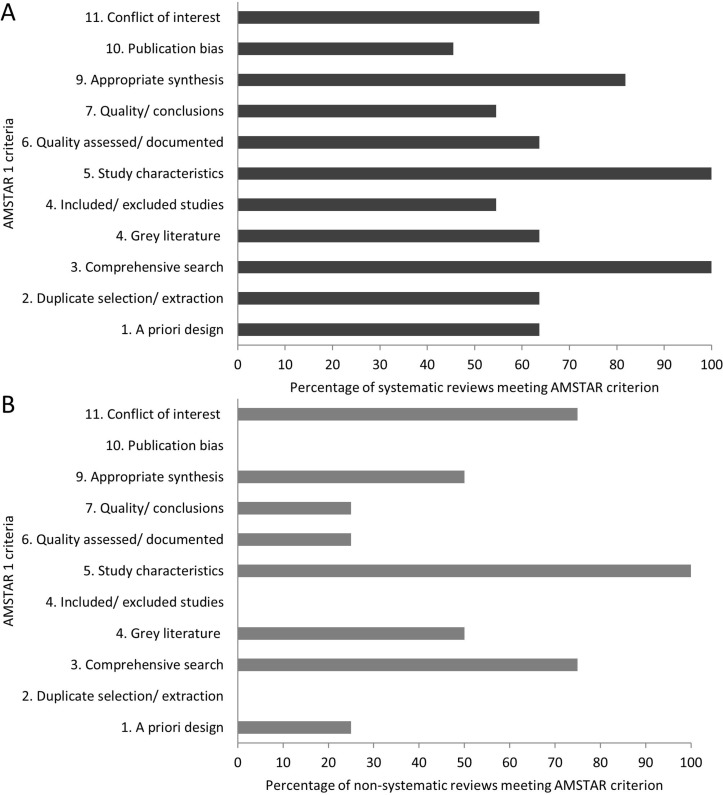
Methodological quality
The overall methodological quality of the included reviews is summarised in figure 2. The overall median (IQR) AMSTAR 1 score was 7 (6.5), compared with 9 (7.5) among systematic reviews and 4.5 (3.25) among non-systematic reviews. Seven reviews (47%), all systematic reviews, were of high quality (AMSTAR 1 score ≥8). While most reviews reported study characteristics, undertook a comprehensive search and identified possible conflicts of interest, non-systematic reviews scored poorly across other AMSTAR 1 domains.
Figure 2.
Summary of Assessment of Multiple Systematic Reviews (AMSTAR) 1 quality appraisal scores for 11 systematic reviews (A) and four non-systematic reviews (B).
Discussion
We sought to review the elements of integrated care approaches for older people, not the comparative effectiveness of these elements, which was the focus of an earlier review in the context of managing multimorbidity in primary care.49 Our review identified 15 reviews where quality scores were mostly moderate to high. The evidence was derived from high-income settings where governance and delivery of healthcare operates under various publicly and privately funded models. Among the reviews included, the integrated care interventions reported in primary studies were largely multifaceted with the majority of specific elements targeting clinical (micro) level integration strategies for older people, consistent with the results of earlier reviews.12 49 Notably, we only identified one review considering macro level integration strategies,42 and this review aligned with a broader range of components of the WHO Framework on Integrated People-Centred Health Services.
Multidisciplinary team care, comprehensive assessment and case management were the most common elements identified across the integrated care interventions, consistent with the WHO ICOPE approach and an earlier non-systematic review50. These specific elements are also suggested to be the most effective for integrated care approaches that target management of multimorbidity.49 Interprofessional education and patient education were less commonly identified as explicit elements, although it may be that education was implicit in other elements, such as self-management. While some reviews identified self-management as an element of the intervention, this was not widespread, tending to reflect a service-focused approach to integrated care interventions. Outcomes of integrated care interventions predominantly focused on hospitalisation, physical functioning and mortality among older people.
Overall, we observed a relative low proportion of organisational (meso) level and system (macro) level integration interventions (and therefore elements), compared with micro level interventions, in the included reviews. The emphasis on the micro level is consistent with findings on studies of development and implementation of models of care generally.12 19 21 23 49 51 This disproportionate micro level emphasis most likely reflects the complexity in tackling whole-of-system issues (ie, from the micro level through to the macro level), both in terms of implementation and measurement complexity, resulting in a one-dimensional focus to integrated care interventions and their evaluation.52 Health and/or social care system change or re-emphasis requires targeted interventions at multiple levels —micro, meso and macro.53 While a disproportionate focus at one level may lead to change and efficiency at that level, it will most likely not be sustained in a broader system, without due consideration of interlevel interactions.50 In the context of evaluation, micro level research or evaluation activities are generally simpler to conduct and procure funding. Conversely, system (macro) level interventions that focus on policy and systems are inherently more complex and represent an emerging area of evaluation science and the establishment of guiding organisations such as the Alliance for Health Policy and Systems Research at WHO. Support for research or evaluation activities that target organisational/service and system-level integration strategies is important and should be undertaken in partnership with stakeholders at all levels of the health system.51 53 The underlying assumption is that a significant impact on clinical, quality of care and economic outcomes requires various multiple interacting interventions targeted at multiple clinical, professional, organisational and system levels.19 The WHO Framework on Integrated People-Centred Health Services provides important guidance in this area.9 17 Until the existing evidence base is supplemented by a volume of new data measuring the effect of clinical (micro) level, service/organisational (meso) level and system (macro) level integration interventions across different contexts, definitive conclusions to support the design of specific, multilevel integrated care approaches are limited.
We also observed less emphasis on outcomes that consider patients’ experiences of care (eg, satisfaction, quality of care) and constructs or tools that characterise functional ability. Whereas these outcomes are person centred, the outcomes reported in most reviews tended to be service or system centred, reflecting the historical orientation of health systems/services and measurement, which has not been person focused. This observation outlines the need to orient interventions and measurement to better reflect person-centred outcomes (such as patient-reported outcome measures (PROMs)) and experiences of care (such as patient-reported experiences meeasures (PREMs)) to support innovation in person-centred approaches to care planning and delivery,54 which is the key focus of the WHO approach to healthy ageing and achieving efficient and sustainable health and long-term care systems.2
Building multidisciplinary workforce capacity to better deliver integrated care models and meet the needs of older people is a key recommendation of the WHO World Report on Ageing and Health2 and consistent with emerging evidence for delivering integrated care for older people with complex health needs.55 In this review, interventions were most commonly directed towards building capacity in nurses, physiotherapists, general practitioners and social workers to deliver integrated care. These discipline foci highlight the importance of addressing health and social care needs, dealing with whole of health and addressing multimorbidity, and in particular maintaining a strong focus on enabling physical and mental capacity which reflect key domains of intrinsic capacity.2 The breadth of the health and social care workforce disciplines included in integrated care interventions also points to the need for requisite knowledge and skills across a workforce to deliver integrated health and social care6 56 and a need to broaden the membership of care teams in some settings.57 In particular, a contemporary understanding of integrated care practices is needed, which supports communication and shared care and responsibility across health and social care providers as well as the knowledge and skills to work with, and refer to, community services which may include the non-government and unpaid sectors. Developing capacity in the workforce to meet these emerging knowledge and skills demands will require targeted interdisciplinary professional development for the current and emerging workforce, as well as systems to support integrated care practices.6 58
Methodological considerations
The quality of the evidence offered in the included reviews was variable. Unsurprisingly, systematic reviews were rated as much higher quality than non-systematic reviews. We elected to include all review types in order to synthesise a wide body of literature concerning the reported elements of integrated care models, rather than just limiting our search to RCTs in systematic reviews. We used the AMSTAR 1 critical appraisal tool to assess overall methodological quality of the included reviews. While AMSTAR 1 is currently the most commonly used tool, we acknowledge that AMSTAR 2 has recently been released and may be more appropriate for quality appraisal in future reviews that include non-randomised trials,59 although users’ experiences with this modified tool remain uncertain. AMSTAR 1 is limited in its application to assessing risk of bias, which is addressed by AMSTAR 2 and the new Rik of Bias in Systematic Reviews (ROBIS) tool.60
Future directions
As most existing studies focus on interventions aimed at coordinating care at the clinical (micro) level, additional longitudinal cross-sectoral research and programme evaluation could help identify the effectiveness of interventions targeted at a wider range of clinical, professional, organisational and system levels of care.10 19 21 Given the disproportionate focus on micro level strategies to date, there is a need for a greater focus on meso level and macro level strategies to achieve implementation of integrated care at scale. While the current review provides evidence for elements of integrated care approaches, it is now important to link these elements with outcomes in different settings, given the critical importance of ‘setting’ or ‘context’ in determining outcomes and sustainable implementation.19 53 In particular, interventions that integrate health and social care are needed to better understand how services and systems can better respond to the holistic needs of older people. A more extensive web of evidence is needed for low and middle-income settings.18
Strengths and limitations
This review adopted a pragmatic approach to identify and synthesise recent overview evidence about the elements of integrated care models for older people, building on an existing taxonomy and Rainbow Model of Integrated Care.10 24 The approach aligns with the principles of undertaking rapid reviews for strengthening health policy and systems.61 The strength of this approach to evidence synthesis is that it includes a broader of web of evidence than would otherwise be available from a systematic review of primary studies within the same time period. Our review is also unique in the context that the focus of the review was to synthesise evidence for the elements of integrated care interventions, not the comparative effectiveness of the interventions themselves. An overview of elements for effective integrated care models is critical to informing implementation of integrated care approaches at scale. It is also critical to link this evidence with evidence for barriers and facilitators to integrated care appappraches for older people across different contexts.50 Although the search period was limited to recent reviews for non-Cochrane reviews and to two databases without grey literature searches, which may have resulted in some relevant reviews and recent primary studies not being included, a systematic search method was used to identify recent reviews and a quality appraisal undertaken.30 A single reviewer being responsible for screening and quality appraisal represents a possible rater bias, although in rapid reviews this practice is more common.61 Our review team was multidisciplinary, including content and methods experts. Given that non-systematic reviews were also included, the quality of these evidence sources was lower and important characterising data for the primary studies were often incompletely reported. Nonetheless, we did not exclude reviews on the basis of quality or design, since our aim was not to report comparative effectiveness. This a priori design decision provided an ‘all in’ approach to evidence synthesis, ensuring that the maximum breadth of evidence reported in the literature was included. This approach is important in providing data to inform implementation activities in health systems.53 62 The majority of the evidence included was sourced from high-income countries and the transferability of the findings may not be relevant to low and middle-income settings.
Conclusion
This review is the first to systematically search and synthesise review evidence for elements of integrated care interventions for older people. Our findings show that integrated care strategies for older people focus particularly on micro clinical processes and there is a relative lack of evidence regarding meso level and macro level integration strategies. Key elements of existing models include multidisciplinary team care, comprehensive assessment and case management. This evidence can help inform the design of integrated care interventions for older people and inform the implementation of the WHO ICOPE approach.
Supplementary Material
Footnotes
Contributors: JAT, PPV and IAC conceived the study. PPV designed the methods and undertook the search, appraisal, extraction and reporting of the data, with a subset performed by AMB. AMB and PPV drafted the manuscript, and all the authors revised it for intellectual content. All authors read and approved the final manuscript.
Funding: The authors gratefully acknowledge the financial support for the broader programme of work provided by the Japanese Ministry of Health, Labour and Welfare. AMB is supported by a fellowship awarded by the Australian National Health and Medical Research Council (No 1132548) and the Global Alliance for Musculoskeletal Health with funding from the International League of Associations for Rheumatology (ILAR) and Curtin University (Australia).
Disclaimer: The views expressed in this paper are those of the authors and do not necessarily reflect the views of WHO.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1260–344. 10.1016/S0140-6736(17)32130-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation. World report on ageing and health. Geneva: WHO, 2015. [Google Scholar]
- 3.Barnett K, Mercer SW, Norbury M, et al. . Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37–43. 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 4.Harrison C, Henderson J, Miller G, et al. . The prevalence of diagnosed chronic conditions and multimorbidity in Australia: a method for estimating population prevalence from general practice patient encounter data. PLoS One 2017;12:e0172935 10.1371/journal.pone.0172935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marengoni A, Angleman S, Melis R, et al. . Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev 2011;10:430–9. 10.1016/j.arr.2011.03.003 [DOI] [PubMed] [Google Scholar]
- 6.Araujo de Carvalho I, Epping-Jordan J, Pot AM, et al. . Organizing integrated health-care services to meet older people’s needs. Bull World Health Organ 2017;95:756–63. 10.2471/BLT.16.187617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Briggs AM, Dreinhöfer KE. Rehabilitation 2030: A Call to Action Relevant to Improving Musculoskeletal Health Care Globally. J Ortho Sports Physic Ther 2017;47:297–300. 10.2519/jospt.2017.0105 [DOI] [PubMed] [Google Scholar]
- 8.World Health Organisation. Global strategy and action plan on ageing and health. Geneva: World Health Organization, 2016. [Google Scholar]
- 9.World Health Organization. Framework on integrated, people-centred health services. Geneva: World Health Organization, 2016. [Google Scholar]
- 10.Valentijn PP, Schepman SM, Opheij W, et al. . Understanding integrated care: a comprehensive conceptual framework based on the integrative functions of primary care. Int J Integr Care 2013;13:e010 10.5334/ijic.886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johri M, Beland F, Bergman H. International experiments in integrated care for the elderly: a synthesis of the evidence. Int J Geriatr Psychiatry 2003;18:222–35. 10.1002/gps.819 [DOI] [PubMed] [Google Scholar]
- 12.Eklund K, Wilhelmson K. Outcomes of coordinated and integrated interventions targeting frail elderly people: a systematic review of randomised controlled trials. Health Soc Care Community 2009;17:447–58. 10.1111/j.1365-2524.2009.00844.x [DOI] [PubMed] [Google Scholar]
- 13.Elkan R, Kendrick D, Dewey M, et al. . Effectiveness of home based support for older people: systematic review and meta-analysis. BMJ 2001;323:719–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernabei R, Landi F, Gambassi G, et al. . Randomised trial of impact of model of integrated care and case management for older people living in the community. BMJ 1998;316:1348–51. 10.1136/bmj.316.7141.1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Low LF, Yap M, Brodaty H. A systematic review of different models of home and community care services for older persons. BMC Health Serv Res 2011;11:93 10.1186/1472-6963-11-93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baztán JJ, Suárez-García FM, López-Arrieta J, et al. . Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta-analysis. BMJ 2009;338:b50 10.1136/bmj.b50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. WHO global strategy on integrated people-centred health services 2016-2026. Geneva: WHO, 2015. [Google Scholar]
- 18.Mounier-Jack S, Mayhew SH, Mays N. Integrated care: learning between high-income, and low- and middle-income country health systems. Health Policy Plan 2017;32(Suppl 4):iv6–12. 10.1093/heapol/czx039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Valentijn PP, Biermann C, Bruijnzeels MA. Value-based integrated (renal) care: setting a development agenda for research and implementation strategies. BMC Health Serv Res 2016;16:330 10.1186/s12913-016-1586-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Breton M, Gray CS, Sheridan N, et al. . Implementing community based primary healthcare for older adults with complex needs in Quebec, Ontario and New-Zealand: describing nine cases. Int J Integr Care 2017;17:12 10.5334/ijic.2506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Angus L, Valentijn PP. From micro to macro: assessing implementation of integrated care in Australia. Aust J Prim Health 2018;24:59-65 10.1071/PY17024 [DOI] [PubMed] [Google Scholar]
- 22.van Rensburg AJ, Fourie P. Health policy and integrated mental health care in the SADC region: strategic clarification using the Rainbow Model. Int J Ment Health Syst 2016;10:49 10.1186/s13033-016-0081-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Briggs AM, Chan M, Slater H. Models of Care for musculoskeletal health: Moving towards meaningful implementation and evaluation across conditions and care settings. Best Pract Res Clin Rheumatol 2016;30:359–74. 10.1016/j.berh.2016.09.009 [DOI] [PubMed] [Google Scholar]
- 24.Valentijn PP, Boesveld IC, van der Klauw DM, et al. . Towards a taxonomy for integrated care: a mixed-methods study. Int J Integr Care 2015;15:e003 10.5334/ijic.1513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kodner DL. All together now: a conceptual exploration of integrated care. Healthc Q 2009;13 Spec No:6–15. 10.12927/hcq.2009.21091 [DOI] [PubMed] [Google Scholar]
- 26.Elissen AM, Steuten LM, Lemmens LC, et al. . Meta-analysis of the effectiveness of chronic care management for diabetes: investigating heterogeneity in outcomes. J Eval Clin Pract 2013;19:753–62. 10.1111/j.1365-2753.2012.01817.x [DOI] [PubMed] [Google Scholar]
- 27.Drewes HW, Steuten LM, Lemmens LC, et al. . The effectiveness of chronic care management for heart failure: meta-regression analyses to explain the heterogeneity in outcomes. Health Serv Res 2012;47:1926–59. 10.1111/j.1475-6773.2012.01396.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pollock M, Fernandes RM, Hartling L. Evaluation of AMSTAR to assess the methodological quality of systematic reviews in overviews of reviews of healthcare interventions. BMC Med Res Methodol 2017;17:48 10.1186/s12874-017-0325-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Valentijn PP, Pereira FA, Ruospo M, et al. . Person-centered integrated care for chronic kidney disease: a systematic review and meta-analysis of randomized controlled trials. Clin J Am Soc Nephrol 2018;13 10.2215/CJN.09960917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J 2009;26:91–108. 10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- 32.Shea BJ, Hamel C, Wells GA, et al. . AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol 2009;62:1013–20. 10.1016/j.jclinepi.2008.10.009 [DOI] [PubMed] [Google Scholar]
- 33.Alldred DP, Kennedy MC, Hughes C, et al. . Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst Rev 2016;2:CD009095 10.1002/14651858.CD009095.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berthelsen CB, Kristensson J. The content, dissemination and effects of case management interventions for informal caregivers of older adults: a systematic review. Int J Nurs Stud 2015;52:988–1002. 10.1016/j.ijnurstu.2015.01.006 [DOI] [PubMed] [Google Scholar]
- 35.Brown L, Forster A, Young J, et al. . Medical day hospital care for older people versus alternative forms of care. Cochrane Database Syst Rev 2015;6:CD001730 10.1002/14651858.CD001730.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cochrane A, Furlong M, McGilloway S, et al. . Time-limited home-care reablement services for maintaining and improving the functional independence of older adults. Cochrane Database Syst Rev 2016;10:CD010825 10.1002/14651858.CD010825.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ellis G, Whitehead MA, O’Neill D, et al. . Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev 2011:CD006211 10.1002/14651858.CD006211.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Handoll HH, Cameron ID, Mak JC, et al. . Multidisciplinary rehabilitation for older people with hip fractures. Cochrane Database Syst Rev 2009:CD007125 10.1002/14651858.CD007125.pub2 [DOI] [PubMed] [Google Scholar]
- 39.Hickman LD, Phillips JL, Newton PJ, et al. . Multidisciplinary team interventions to optimise health outcomes for older people in acute care settings: a systematic review. Arch Gerontol Geriatr 2015;61:322–9. 10.1016/j.archger.2015.06.021 [DOI] [PubMed] [Google Scholar]
- 40.Ke LS, Huang X, O’Connor M, et al. . Nurses' views regarding implementing advance care planning for older people: a systematic review and synthesis of qualitative studies. J Clin Nurs 2015;24:2057–73. 10.1111/jocn.12853 [DOI] [PubMed] [Google Scholar]
- 41.Lowthian JA, McGinnes RA, Brand CA, et al. . Discharging older patients from the emergency department effectively: a systematic review and meta-analysis. Age Ageing 2015;44:761–70. 10.1093/ageing/afv102 [DOI] [PubMed] [Google Scholar]
- 42.McClure R, Turner C, Peel N, et al. . Population-based interventions for the prevention of fall-related injuries in older people. Cochrane Database Syst Rev 2005;1:CD004441 10.1002/14651858.CD004441.pub2 [DOI] [PubMed] [Google Scholar]
- 43.Phelan EA, Debnam KJ, Anderson LA, et al. . A systematic review of intervention studies to prevent hospitalizations of community-dwelling older adults with dementia. Med Care 2015;53:207–13. 10.1097/MLR.0000000000000294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Costa-de Lima K, Peixoto-Veras R, Pereira-Caldas C, et al. . Effectiveness of intervention programs in primary care for the robust elderly. Salud Publica Mex 2015;57:265–74. [DOI] [PubMed] [Google Scholar]
- 45.Deschodt M, Claes V, Van Grootven B, et al. . Structure and processes of interdisciplinary geriatric consultation teams in acute care hospitals: A scoping review. Int J Nurs Stud 2016;55:98–114. 10.1016/j.ijnurstu.2015.09.015 [DOI] [PubMed] [Google Scholar]
- 46.Fan L, Lukin W, Zhao J, et al. . Interventions targeting the elderly population to reduce emergency department utilisation: a literature review. Emerg Med J 2015;32:738–43. 10.1136/emermed-2014-203770 [DOI] [PubMed] [Google Scholar]
- 47.Frank C, Wilson CR. Models of primary care for frail patients. Can Fam Physician 2015;61:601–6. [PMC free article] [PubMed] [Google Scholar]
- 48.Handoll HH, Brorson S. Interventions for treating proximal humeral fractures in adults. Cochrane Database Syst Rev 2015:CD000434 10.1002/14651858.CD000434.pub4 [DOI] [PubMed] [Google Scholar]
- 49.Smith SM, Soubhi H, Fortin M, et al. . Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ 2012;345:e5205 10.1136/bmj.e5205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Threapleton DE, Chung RY, Wong SYS, et al. . Integrated care for older populations and its implementation facilitators and barriers: A rapid scoping review. Int J Qual Health Care 2017;29:327–34. 10.1093/intqhc/mzx041 [DOI] [PubMed] [Google Scholar]
- 51.Valentijn PP, Ruwaard D, Vrijhoef HJ, et al. . Collaboration processes and perceived effectiveness of integrated care projects in primary care: a longitudinal mixed-methods study. BMC Health Serv Res 2015;15:463 10.1186/s12913-015-1125-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tsasis P, Evans JM, Owen S. Reframing the challenges to integrated care: a complex-adaptive systems perspective. Int J Integr Care 2012;12:e190 10.5334/ijic.843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Briggs AM, Jordan JE, Jennings M, et al. . Supporting the evaluation and implementation of musculoskeletal models of care: A globally informed framework for judging readiness and success. Arthritis Care Res 2017;69:567–77. 10.1002/acr.22948 [DOI] [PubMed] [Google Scholar]
- 54.Coventry PA, Small N, Panagioti M, et al. . Living with complexity; marshalling resources: a systematic review and qualitative meta-synthesis of lived experience of mental and physical multimorbidity. BMC Fam Pract 2015;16:171 10.1186/s12875-015-0345-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shakib S, Dundon BK, Maddison J, et al. . Effect of a multidisciplinary outpatient model of care on health outcomes in older patients with multimorbidity: A retrospective case control study. PLoS One 2016;11:e0161382 10.1371/journal.pone.0161382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Black DR. Preparing the workforce for integrated healthcare: A systematic review. Soc Work Health Care 2017;56:914–42. 10.1080/00981389.2017.1371098 [DOI] [PubMed] [Google Scholar]
- 57.Kuluski K, Ho JW, Hans PK, et al. . Community care for people with complex care needs: bridging the gap between health and social care. Int J Integr Care 2017;17:2 10.5334/ijic.2944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gardner P, Slater H, Jordan JE, et al. . Physiotherapy students’ perspectives of online e-learning for interdisciplinary management of chronic health conditions: a qualitative study. BMC Med Educ 2016;16:62 10.1186/s12909-016-0593-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shea BJ, Reeves BC, Wells G, et al. . AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017;358:j4008 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Whiting P, Savović J, Higgins JP, et al. . ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol 2016;69:225–34. 10.1016/j.jclinepi.2015.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tricco AC, Langlois EV, Strauss SE. Rpaid reviews to strengthen health policy and systems: a practical guide. Geneva: World Health Organization, 2017. [Google Scholar]
- 62.Langlois EV, Tunçalp Ö, Norris SL, et al. . Qualitative evidence to improve guidelines and health decision-making. Bull World Health Organ 2018;96:79–79A. 10.2471/BLT.17.206540 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-021194supp001.pdf (116.3KB, pdf)
bmjopen-2017-021194supp002.pdf (76.1KB, pdf)