Abstract
Introduction
Weight gain and concerns about weight can influence a smoker’s ability to successfully quit, and young adults are a subgroup of smokers who are particularly concerned about the impact of quitting on their body weight. This study explored the associations between body mass index, weight perceptions, and smoking status among young adults.
Methods
The sample consisted of 4027 young adults between the ages of 18 and 29 who participated in a randomized control trial of the National Cancer Institute’s SmokefreeTXT program. Multivariable logistic regression models were used to examine the associations between weight related variables and smoking status.
Results
Obese participants had a 0.72 lower odds (95% CI: 0.62, 0.85) of reporting smoking at the end of the program than participants of normal weight, and this difference persisted over time. Weight perceptions were also associated with smoking status. Those who perceived themselves to be slightly underweight/underweight were more likely to report smoking than those who reported being just about the right weight (OR: 1.53, 95% CI: 1.20, 1.95), and those who strongly disagreed that smoking cigarettes helps people keep their weight down were less likely to report smoking at the end of treatment than those who neither agreed nor disagreed with this statement (OR: 0.69, 95% CI: 0.54, 0.87).
Conclusions
Weight related factors assessed at baseline predicted smoking status at the end of treatment and through long term follow-up. Smoking cessation programs that tailor content to addresses the specific needs of weight concerned smokers may enhance effectiveness.
Implications
This study explores the association between weight related factors and smoking status among young adults, a priority population for smoking cessation efforts. This study demonstrates that both actual weight and weight perceptions (eg, perception of body weight, perception of associations between smoking and weight) are associated with smoking outcomes, and thus need to be a considered in the development of smoking cessation programs.
Introduction
Smoking and obesity are two of the leading causes of death, and historically, an inverse association between smoking and weight has existed, such that smokers tend to weigh less than nonsmokers.1–5 Although overall smokers weigh less than never smokers, heavy smokers tend to weigh more than light smokers after adjusting for other factors, such as age and education.6
Given that smoking and obesity are cumulative risk factors for certain diseases (eg, cancer, heart disease), this can lead to accumulated risk in some individuals.5,7,8
Smokers who quit tend to gain weight, and thus, concerns about weight gain can affect smokers’ success when attempting to quit.9–12 Over a 10-year period, the average smoker who quits gains 4.9 kg of weight directly attributable to quitting smoking; however, this weight gain varies by baseline body mass index (BMI) category and number of cigarettes smoked per day.13
There are multiple mechanisms that can contribute to smokers gaining weight after quitting, including substituting food for cigarettes and experiencing a decrease in resting metabolism rates due to abstinence from nicotine.14–16 Certain subgroups of smokers, including women, young adults, and people who are overweight/obese, tend to be particularly concerned about the consequences of quitting on their weight, and therefore possible weight gain is a barrier to quitting.10,12,17,18
It is possible that concerns about weight gain can influence smokers’ use of cessation resources. One study found that although weight gain concerns did not predict treatment seeking among all smokers, it did predict treatment seeking among smokers who gained weight during a previous quit attempt, such that smokers who gained weight during a previous quit attempt were less likely to seek treatment.19 Given that concerns about weight gain can affect how successful smokers are when trying to quit, there is a need to better understand how weight and perceptions about weight influence cessation outcomes during quit attempts.
Young adults, a subgroup of smokers who tend to be particularly concerned about the impact of quitting on their weight, are also a priority group for smoking cessation because quitting before the age of 30 can eliminate “97% of the excess mortality caused by continuing smoking.”20 To examine the associations between body weight, weight perceptions, and smoking outcomes, we used a sample of young adults (18–29 years old) who were participating in a text-messaging smoking-cessation intervention. Mobile health (mHealth) technologies are increasingly being used to deliver behavioral interventions as such interventions have the ability to reach large segments of the population in a cost-effective manner.21,22 Although 64% of all Americans own a smartphone, 85% of young adults between the ages of 18 and 29 own a smartphone, and approximately three-quarters of young adult smartphone owners have used their phone in the last year to get information about a health condition,23 suggesting that young adults may be well suited to be reached through this platform. Having a better understanding of key factors that influence cessation outcomes (eg, weight gain concerns) may help to inform efforts to tailor text-messaging smoking-cessation programs.
Methods
Participants
The sample for this analysis consisted of participants in a 3-arm, randomized controlled trial that compared the National Cancer Institute’s SmokefreeTXT program, a 6-week, text–message-based smoking-cessation intervention, to two modified versions of the program that varied in the types and number of messages sent.24 The first arm included periodic cessation assessments and quit date reminder messages. The second arm included cessation assessments, quit date reminder messages, and 2 weeks of quit-date preparation messages. The third arm included the full SmokefreeTXT program; that is, cessation assessments, quit-day reminder messages, 2 weeks of pre-quit-date preparation messages, 6 weeks of post-quit-date motivational support, tips on preparing to quit, advice on managing cravings, suggestions of smoke-free activities, relevant smoking facts, and recognition of cessation milestones. None of the messages were about weight management.
The full sample, 4027 young adults, was used in this analysis. They were US smokers between the ages of 18 and 29 years old who were interested in quitting smoking in 30 days but who were not receiving treatment to quit smoking at the time. Recruitment strategies included online advertising and search ads via Facebook, Craigslist, Pandora, and Google, Yahoo! and Bing, and email recruitment via market research panels.24 To enroll in the study, participants had to report having smoked at least five of the past 30 days and to have unlimited text messaging availability on their mobile phones. In addition to having to meet the inclusion criteria, participants had to complete a baseline survey. This study received Institutional Review Board approval from the National Cancer Institute.
Measures
To begin, participants completed a Web-based, self-administered survey at baseline. Their quit date was set for 2 weeks after the date they finished the baseline survey. They also completed additional surveys at 1 week post quit date (3 weeks), the end of the program (8 weeks), 3 months post-treatment (20 weeks), and 6 months post-treatment (32 weeks). Participants received $20 gift cards for each follow-up survey completed, for a total of up to $80. The baseline survey included questions about smoking history, demographic characteristics, psychosocial characteristics, and smoking status. The 3-week and 8-week surveys included questions about smoking attitudes, perceptions, and behaviors as well as engagement with the intervention. The 20-week and 32-week surveys focused on smoking attitudes, perceptions, and behaviors. The response rate for the 3-week survey was 74.7% (n = 3009), for the 8-week survey was 71.5% (n = 2881), for the 20-week survey was 66.4% (n = 2675), and for the 32-week survey was 64.4% (n = 2603).25
Our primary dependent variable was the smoking status at the end of the program (ie, at 8 weeks), and the secondary dependent variables were the smoking statuses at post-treatment follow-up assessments (ie, at 20 weeks and 32 weeks). To assess smoking status, we asked the question “Have you smoked at all, even a puff, in the last 7 days?” Our primary independent variables were the participants’ BMI category, weight perception, expectancies about smoking and weight; all of these independent variables were assessed at baseline. Participants’ BMI was calculated using self-reported weight and height to categorize them as underweight, normal, overweight, or obese, the standard health risk classifications designated by the Centers for Disease Control and Prevention (see http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html#InterpretedAdults).
To assess expectancies about smoking and weight, we asked participants to rate the statement “Smoking cigarettes helps people keep their weight down” using a 5-point scale, with the responses (1) strongly agree, (2) agree, (3) neither agree nor disagree, (4) disagree, or (5) strongly disagree. This question was adapted from the Smoking Consequences Questionnaire.26 We assessed weight perception with the question “Right now, do you feel you are overweight, slightly overweight, just about the right weight for you, slightly underweight, or underweight?”27 Slightly underweight and underweight responses were collapsed into a single category, after confirming that they did not differ with respect to smoking outcomes, because of the small number of individuals in these weight categories.
We also assessed the following variables at baseline and controlled for them in multivariable models: age (in years), gender, household income, and daily smoker (yes/no). Household income categories were less than $35 000, $35 000–$70 000, and more than $70 000. Smokers were classified as daily smokers if they reported smoking every day over the past month, and as nondaily smokers if they reported smoking less frequently than that.
Analytic Procedures
We examined the associations between baseline BMI category and demographic characteristics using chi-square tests for categorical variables and analysis of variance (ANOVA) for continuous variables. We also assessed the bivariate associations among baseline BMI categories, weight perceptions, and expectancies about smoking and weight using chi-square tests. To assess the associations between the weight-related variables and smoking status, controlling for age in years, gender (male/female), income (<$35 000, $35 000–$70 000, $≥70 000), daily smoking status, and study arm, we constructed multivariable logistic regression models. In the primary analysis, participants who did not respond to the smoking status question at a given assessment point were categorized as smokers in those respective analyses. The 8-week, end-of-treatment smoking status analysis was the primary analytic time point. We also conducted a respondents only analysis as a sensitivity analysis; deviations of those results from the primary analysis are noted. All analyses were conducted using SAS 9.3 (Cary, NC). We conducted two-sided significance testing and considered a p value of less than .05 as statistically significant.
Results
Most participants were female (70.2%) and were daily smokers (80.3%). More than half had a household income of less than $35 000 (57.3%), and participants’ mean age was 24.6 years (see Table 1). With respect to BMI, 5.1% of participants were classified as underweight, 42.0% were of normal weight, 24.6% were overweight, and 28.4% were obese. In bivariate analyses, participants in different BMI categories varied with respect to gender, age, and income; however, they did not differ by study arm or by percentage of daily smokers.
Table 1.
Sample Characteristics (N = 4027)
| Total | Underweight 5.1% (n = 205) | Normal 42.0% (n = 1690) | Overweight 24.6% (n = 989) | Obese 28.4% (n = 1143) | p | |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 29.8 (1200) | 31.2 (64) | 31.5 (532) | 36.1 (357) | 21.6 (247) | <.01 |
| Female | 70.2 (2825) | 68.8 (141) | 68.5 (1158) | 63.9 (631) | 78.4 (895) | |
| Age (mean, SD) | 24.6 (3.3) | 23.8 (3.3) | 24.2 (3.4) | 24.7 (3.2) | 25.2 (3.0) | <.01 |
| Income | ||||||
| Less than $35 000 | 57.3 (2306) | 57.6 (118) | 54.6 (921) | 55.5 (549) | 62.8 (718) | <.01 |
| Between $35 000 and $70 000 | 23.7 (954) | 20.0 (41) | 23.3 (393) | 26.5 (262) | 22.6 (258) | |
| Over $70 000 | 7.6 (306) | 8.3 (17) | 9.0 (151) | 7.8 (77) | 5.3 (61) | |
| Refuse | 11.4 (458) | 14.1 (29) | 13.2 (222) | 10.2 (101) | 9.3 (106) | |
| Daily smoker | ||||||
| Yes | 80.3 (3234) | 80.0 (164) | 79.0 (1335) | 80.2 (793) | 82.4 (942) | .16 |
| No | 19.7 (793) | 20.0 (41) | 21.0 (355) | 19.8 (196) | 17.6 (201) | |
| Study arm | ||||||
| 1 | 32.6 (1313) | 27.8 (57) | 32.3 (545) | 33.5 (331) | 33.3 (380) | .30 |
| 2 | 34.8 (1400) | 41.0 (84) | 34.7 (587) | 35.7 (353) | 32.9 (376) | |
| 3 | 32.6 (1314) | 31.2 (64) | 33.0 (558) | 30.8 (305) | 33.9 (387) | |
| Weight perceptions | ||||||
| Slightly underweight/underweight | 12.3% (493) | 64.9% (133) | 20.4% (344) | 1.5% (15) | 0.10% (1) | <.01 |
| Just about the right weight | 24.7% (992) | 21.5% (44) | 45.7% (772) | 15.5% (153) | 2.0% (23) | |
| Slightly overweight | 31.5% (1266) | 8.3% (17) | 30.1% (508) | 54.1% (534) | 18.1% (207) | |
| Overweight | 31.6% (1273) | 5.4% (11) | 3.9% (66) | 28.9% (285) | 79.8% (911) | |
| Smoking expectancy about weight “Smoking cigarettes helps people keep their weight down” | ||||||
| Strongly agree/agree | 35.9 (1442) | 41.2% (84) | 40.6% (684) | 35.7% (352) | 28.3% (322) | <.01 |
| Neither agree nor disagree | 29.3% (1174) | 35.8% (73) | 30.5% (514) | 30.0% (295) | 25.6% (292) | |
| Strongly disagree/disagree | 34.8% (1398) | 23.0% (47) | 28.9% (488) | 34.3% (338) | 46.1% (525) | |
BMI Category and Smoking Status
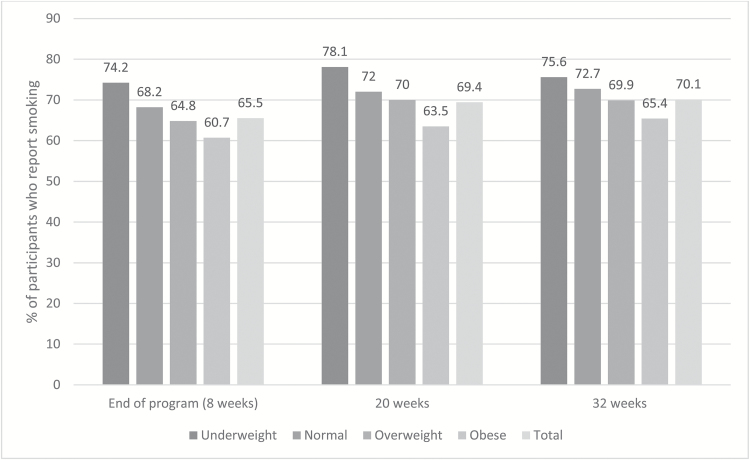
Obese participants were less likely to report smoking at the end of the treatment period (8 weeks) than participants of normal weight, and this difference persisted over time (see Figure 1). At 8 weeks, 74.2% of underweight, 68.2% of normal weight, 64.8% of overweight, and 60.7% of obese participants reported smoking. After controlling for covariates in multivariable logistic regression models, BMI remained a significant predictor of smoking status at 8 weeks. Specifically, those who were obese had 0.72 lower odds (95% CI: 0.62, 0.85) of reporting smoking than those of normal weight. This difference persisted across the follow-up assessments (ie, odds ratio [OR] for week 20 assessment: 0.69, 95% CI: 0.59, 0.82; OR for week 32 assessment: 0.73, 95% CI: 0.62, 0.86). When including only respondents (n = 2873, 2662, and 2601 at 8 weeks, 20 weeks, and 32 weeks, respectively), over time, the same pattern emerged for obese smokers compared to normal weight smokers (data not shown). At 8 weeks, participants who were overweight at baseline were marginally less likely than those who were of normal weight at baseline to report smoking (OR: 0.83, 95% CI: 0.69, 1.00), and underweight participants were more likely to report smoking than normal weight individuals (OR: 1.50, 95% CI: 1.05, 2.14); however, these associations became nonsignificant at 20 weeks and 32 weeks.
Figure 1.
Percentage of participants who report smoking at each follow-up assessment by BMI category.
Weight-Related Perceptions
In multivariable logistic regression analyses, those who perceived themselves as slightly underweight/underweight were more likely to report smoking than those who reported being just about the right weight (OR: 1.53, 95% CI: 1.20, 1.95). Given the association between BMI category and weight perception (see Table 2), we ran a logistic regression model to also control for BMI category, and this association persisted (OR: 1.43, 95% CI: 1.11, 1.84; see Table 2). Across follow-up smoking status assessments, this increased likelihood of smoking among those who perceived themselves to be slightly underweight/underweight at baseline compared to those who perceived themselves to be at just about the right weight persisted (week 20: OR: 1.38, 95% CI: 1.06, 1.80; week 32: OR: 1.33, 95% CI: 1.02, 1.73). In the analysis restricted to respondents only, the association between perceived slightly underweight/underweight became nonsignificant after controlling for BMI (data not shown).
Table 2.
Multivariable Logistic Regression Model of Weight Perception on Likelihood of Smoking at the End of Treatmenta
| Odds ratio (95% CI) | p | |
|---|---|---|
| Weight perception (refb: just about the right weight) | ||
| Overweight | 1.22 (0.95, 1.56) | .03 |
| Slightly overweight | 1.21 (1.00, 1.47) | |
| Slightly underweight/underweight | 1.43 (1.11, 1.84) | |
| Gender (ref: male) | ||
| Female | 1.09 (0.94, 1.271 | .24 |
| Age | 0.99 (0.97, 1.01) | .15 |
| Income (ref: less than $35 000) | ||
| $35 000 to $70 000 | 0.92 (0.78, 1.08) | .38 |
| More than $70 000 | 0.99 (0.77, 1.28) | |
| Prefer not to answer | 1.14 (0.91, 1.42) | |
| Daily smoker (ref: no) | ||
| Yes | 1.34 (1.14, 1.58) | <.01 |
| BMI (ref: normal) | ||
| Underweight | 1.19 (0.84, 1.68) | <.01 |
| Overweight | 0.85 (0.70, 1.03) | |
| Obese | 0.68 (0.54, 0.86) | |
aControlled for study arm.
bref: reference group.
Smoking Expectancy About Weight
Participants who were underweight or normal weight were more likely than those who were overweight or obese to agree with the smoking expectancy “Smoking cigarettes helps people keep their weight down” (see Table 1). Participants who strongly disagreed with this statement were less likely to report smoking at the end of treatment than those who neither agreed nor disagreed with this statement (OR: 0.69, 95% CI: 0.54, 0.87; see Table 3).
Table 3.
Multivariable Logistic Model of Smoking Expectancy of Weight on the Likelihood of Smoking at the End of Treatmenta
| Odds ratio (95% CI) | p | |
|---|---|---|
| Smoking expectancy about weight (refb: neither agree nor disagree) | ||
| Strongly agree | 0.90 (0.66, 1.21) | .02 |
| Agree | 1.01 (0.83, 1.22) | |
| Disagree | 0.99 (0.80, 1.23) | |
| Strongly disagree | 0.69 (0.54, 0.87) | |
| Gender (ref: male) | ||
| Female | 1.11 (0.94, 1.30) | .23 |
| Age | 1.00 (0.97, 1.02) | .71 |
| Income (ref: less than $35 000) | ||
| $35 000 to $70 000 | 1.01 (0.85, 1.21) | .38 |
| More than $70 000 | 1.27 (0.97, 1.67) | |
| Prefer not to answer | 1.00 (0.77, 1.29) | |
| Daily smoker (ref: no) | ||
| Yes | 1.23 (1.02, 1.47) | .03 |
| BMI (ref: normal) | ||
| Underweight | 1.51 (1.05, 2.15) | <.01 |
| Overweight | 0.83 (0.69, 1.01) | |
| Obese | 0.78 (0.65, 0.94) | |
aControlled for study arm.
bref: reference group.
Discussion
In this study, which assessed the smoking status of a large sample of smokers between the ages of 18 and 29 who participated in a randomized controlled trial of a text-messaging cessation program, we found that those who were obese were less likely to report smoking at the end of the program than those of normal weight, with 60.7% of obese participants reporting smoking compared to 68.2% of normal weight participants. This increased likelihood of not smoking among obese participants compared to those of normal weight persisted over the 20-week and 32-week follow-up periods.
There is limited research that explores that association between baseline BMI and smoking cessation, and the studies that have been done have inconsistent findings. For example, one study found that among men, overweight and obese smokers had significantly higher cessation rates than normal weight smokers; however there were no significant differences in cessation outcomes for women by BMI.28 In contrast, Swan and colleagues found that among women smokers, those with a higher BMI had the lowest abstinence rates; however, BMI did not predict smoking cessation among men.29 A study of Quitline users found no significant associations between baseline weight and cessation outcomes.30 Future research is needed to further explore the relationship between baseline body weight and cessation outcomes, and potential moderators of this relationship (eg, gender, age, past quit attempts) in a more nuanced way.
Weight perceptions were also associated with smoking rates at the end of treatment; that is, participants who perceived themselves to be slightly underweight/underweight were more likely to report smoking at the end of treatment than those who perceived themselves to be just about the right weight, even after controlling for BMI category. Also, those who strongly disagreed that people smoke to keep their weight down were less likely to report smoking than those who neither agreed nor disagreed with this sentiment.
There are different possible explanations for our findings. In terms of differences in smoking rates by BMI category, one possibility is that individuals of normal weight are more likely to smoke in part for weight control reasons and that experiencing an increase in weight following a quit attempt may result in a smoking relapse. Although we did not ask participants whether they were smoking for weight control, the expectancy about smoking and weight question (“Smoking cigarettes help people keep their weight down”) did tap into this, and underweight (41.2%) and normal weight (40.6%) participants were more likely to agree or strongly agree with this statement than overweight (35.7%) and obese (28.3%) participants. This is consistent with other research that has shown that individuals with lower BMIs are more likely to be weight concerned.31 Furthermore, those who strongly disagreed with the belief that smoking helped to keep weight down were more likely to be abstinent at the end of treatment. Individuals who do perceive a relationship between smoking cessation and weight gain might be more prone to relapse if weight gain occurs.10
Another possibility is that obese smokers have co-morbidities (eg, cardiac disease) that increase their motivation to and efficacy in quitting smoking. However, the young age of the sample suggests this is unlikely. Obese smokers might be more likely to have been told by a physician that they should quit given their multiple risk factors for disease.
Although underweight smokers were not more likely to smoke than normal weight smokers in multivariable analyses, participants who perceived themselves to be slightly underweight/underweight were more likely to be smoking at the end of treatment and at subsequent follow-ups. It is possible that individuals who perceive themselves to be underweight are more concerned about their weight, and previous research has found that those who are more concerned about weight are more likely to relapse to smoking.9,32
Given the interconnectedness of smoking status and weight and the fact that cessation-related weight gain might result in relapse, weight-related quitting concerns are a factor that can be tailored within smoking-cessation programs. This might take the form of addressing concerns about weight gain (eg, increasing users’ knowledge of what to expect in terms of weight change when quitting, assuring users that the health benefits of quitting smoking outweigh the potential risks of weight gain). For example, mindfulness techniques, such as being able to describe and give labels to one’s feelings, in this case weight concerns, have been found to help reduce smoking episodes among weight-concerned smokers.33 Cognitive behavioral therapy to address weight related concerns has also been found effective in increasing smoking abstinence rates.34,35
A substantial number of the participants who quit smoking within this trial were overweight or obese. As such, it is worthwhile exploring the connection between smoking and obesity-related behaviors as well as the potential benefit of encouraging smokers to adopt other health behaviors during a quit attempt. For example, integrating information about healthy eating and increased physical activity into text-messaging cessation programs may help to support weight maintenance or weight loss during a quit attempt. Given that many smokers in the general population are overweight or obese,36 there is value in addressing related health risk behaviors with this population. Particularly among young adults (under the age of 30), smoking cessation and weight loss are often behavioral goals that are set simultaneously,18 supporting the potential utility of interventions that facilitate multiple behavior changes. There is growing evidence supporting the effectiveness of multiple health behavior change interventions over single health change interventions.37–39 While this study focused specifically on baseline BMI, future research can examine how multiple health behavior change interventions impact weight change and cessation outcomes.
This study had some limitations that warrant consideration. We used a convenience sample recruited for a cessation randomized controlled trial, and therefore, the findings may not be generalizable to all 18- to 29-year-old smokers or to the population of smokers as a whole. Also, that these analyses are based on self-reported data is another potential limitation, as both weight and smoking status are subject to response bias or error. Nonresponse rates for smoking status were relatively high, ranging from 28.5% to 35.5%. To assess the possible impact of nonresponse, two sets of analyses were conducted: one categorizing nonrespondents as smokers and another including only respondents. For the most part, findings from both analyses were consistent. Furthermore, we examined outcomes over multiple follow-up points and found that significant associations often held over time. However, this was a post hoc exploratory analysis and multiple comparisons increase the likelihood of a Type I error.
The findings from this study provide further evidence of the association between weight and smoking-cessation outcomes. Furthermore, these findings suggest that effective strategies for addressing smoking cessation and weight concerns are needed. Future research should continue to explore how post-cessation weight gain and weight expectancies affect smokers’ quit attempts and changes in smoking status over time. This information can be used to help inform intervention development. mHealth cessation programs can be of particular value in this domain because they can be tailored to the individual. Data on weight, height, and weight-related perceptions and expectancies can be collected during enrollment, and using this information individuals can be sent messages tailored to their needs in an effort to strengthen the program’s effectiveness.
Funding
This study was funded in part by National Institutes of Health, National Cancer Institute HHSN261201400002B, HHSN26100006, HHSN26100007.
Declaration of Interests
None declared.
References
- 1. Wack JT, Rodin J. Smoking and its effects on body weight and the systems of caloric regulation. Am J Clin Nutr. 1982;35(2):366–380. [DOI] [PubMed] [Google Scholar]
- 2. Jacobs DR, Jr, Gottenborg S. Smoking and weight: the Minnesota Lipid Research Clinic. Am J Public Health. 1981;71(4):391–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Albanes D, Jones DY, Micozzi MS, Mattson ME. Associations between smoking and body weight in the US population: analysis of NHANES II. Am J Public Health. 1987;77(4):439–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Flegal KM, Troiano RP, Pamuk ER, Kuczmarski RJ, Campbell SM. The influence of smoking cessation on the prevalence of overweight in the United States. N Engl J Med. 1995;333(18):1165–1170. [DOI] [PubMed] [Google Scholar]
- 5. Collaboration PS. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. The Lancet. 2009;373(9669):1083–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chiolero A, Faeh D, Paccaud F, Cornuz J. Consequences of smoking for body weight, body fat distribution, and insulin resistance. Am J Clin Nutr. 2008;87(4):801–809. [DOI] [PubMed] [Google Scholar]
- 7. Freedman DM, Sigurdson AJ, Rajaraman P, Doody MM, Linet MS, Ron E. The mortality risk of smoking and obesity combined. Am J Prev Med. 2006;31(5):355–362. [DOI] [PubMed] [Google Scholar]
- 8. Chyou PH, Burchfiel CM, Yano K, et al. Obesity, alcohol consumption, smoking, and mortality. Ann Epidemiol. 1997;7(4):311–317. [DOI] [PubMed] [Google Scholar]
- 9. Meyers AW, Klesges RC, Winders SE, Ward KD, Peterson BA, Eck LH. Are weight concerns predictive of smoking cessation? A prospective analysis. J Consult Clin Psychol. 1997;65(3):448–452. [DOI] [PubMed] [Google Scholar]
- 10. Pomerleau CS, Zucker AN, Stewart AJ. Characterizing concerns about post-cessation weight gain: results from a national survey of women smokers. Nicotine Tob Res. 2001;3(1):51–60. [DOI] [PubMed] [Google Scholar]
- 11. Clark MM, Decker PA, Offord KP, et al. Weight concerns among male smokers. Addict Behav. 2004;29(8):1637–1641. [DOI] [PubMed] [Google Scholar]
- 12. Levine MD, Bush T, Magnusson B, Cheng Y, Chen X. Smoking-related weight concerns and obesity: differences among normal weight, overweight, and obese smokers using a telephone tobacco quitline. Nicotine Tob Res. 2013;15(6):1136–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Veldheer S, Yingst J, Zhu J, Foulds J. Ten-year weight gain in smokers who quit, smokers who continued smoking and never smokers in the United States, NHANES 2003-2012. Int J Obes (Lond). 2015;39(12):1727–1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Audrain‐McGovern J, Benowitz N. Cigarette smoking, nicotine, and body weight. Clin Pharmacol Ther. 2011;90(1):164–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dallosso HM, James WP. The role of smoking in the regulation of energy balance. Int J Obes. 1984;8(4):365–375. [PubMed] [Google Scholar]
- 16. Filozof C, Fernández Pinilla MC, Fernández-Cruz A. Smoking cessation and weight gain. Obes Rev. 2004;5(2):95–103. [DOI] [PubMed] [Google Scholar]
- 17. Pisinger C, Jorgensen T. Weight concerns and smoking in a general population: the Inter99 study. Prev Med. 2007;44(4):283–289. [DOI] [PubMed] [Google Scholar]
- 18. Wee CC, Rigotti NA, Davis RB, Phillips RS. Relationship between smoking and weight control efforts among adults in the united states. Arch Intern Med. 2001;161(4):546–550. [DOI] [PubMed] [Google Scholar]
- 19. Veldheer S, Yingst J, Foulds G, et al. Once bitten, twice shy: concern about gaining weight after smoking cessation and its association with seeking treatment. Int J Clin Pract. 2014;68(3):388–395. [DOI] [PubMed] [Google Scholar]
- 20. Pirie K, Peto R, Reeves GK, Green J, Beral V; Million Women Study Collaborators The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet. 2013;381(9861):133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Guerriero C, Cairns J, Roberts I, Rodgers A, Whittaker R, Free C. The cost-effectiveness of smoking cessation support delivered by mobile phone text messaging: Txt2stop. Eur J Health Econ. 2013;14(5):789–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Whittaker R, McRobbie H, Bullen C, Borland R, Rodgers A, Gu Y. Mobile phone‐based interventions for smoking cessation. Cochrane Database Syst Rev. 2012;11:Art. No: CD006611. [DOI] [PubMed] [Google Scholar]
- 23. Smith A, McGeeney K, Duggan M, Rainie L, Keeter S. The Smartphone Difference. Washington, DC: Pew Research Center; 2015. [Google Scholar]
- 24. Squiers L, Augustson E, Brown D, et al. An experimental comparison of mobile texting programs to help young adults quit smoking. Health Systems. 2016. [Google Scholar]
- 25. Squiers L, Brown D, Parvanta S, et al. The SmokefreeTXT (SFTXT) Study: web and mobile data collection to evaluate smoking cessation for young adults. JMIR Res Protoc. 2016;5(2):e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Brandon TH, Baker TB. The Smoking Consequences Questionnaire: The subjective expected utility of smoking in college students. Psychol Assess. 1991;3(3):484. [Google Scholar]
- 27. Squiers L, Renaud J, McCormack L, Tzeng J, Bann C, Williams P. How accurate are Americans’ perceptions of their own weight?J Health Commun. 2014;19(7):795–812. [DOI] [PubMed] [Google Scholar]
- 28. Twardella D, Loew M, Rothenbacher D, Stegmaier C, Ziegler H, Brenner H. The impact of body weight on smoking cessation in German adults. Prev Med. 2006;42(2):109–113. [DOI] [PubMed] [Google Scholar]
- 29. Swan GE, Javitz HS, Jack LM, Curry SJ, McAfee T. Heterogeneity in 12-month outcome among female and male smokers. Addiction. 2004;99(2):237–250. [DOI] [PubMed] [Google Scholar]
- 30. Bush TM, Levine MD, Magnusson B, et al. Impact of baseline weight on smoking cessation and weight gain in quitlines. Ann Behav Med. 2014;47(2):208–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Clark MM, Hurt RD, Croghan IT, et al. The prevalence of weight concerns in a smoking abstinence clinical trial. Addict Behav. 2006;31(7):1144–1152. [DOI] [PubMed] [Google Scholar]
- 32. Jeffery RW, Hennrikus DJ, Lando HA, Murray DM, Liu JW. Reconciling conflicting findings regarding postcessation weight concerns and success in smoking cessation. Health Psychol. 2000;19(3):242–246. [DOI] [PubMed] [Google Scholar]
- 33. Adams CE, McVay MA, Stewart DW, et al. Mindfulness ameliorates the relationship between weight concerns and smoking behavior in female smokers: a cross-sectional investigation. Mindfulness (N Y). 2014;5(2):179–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Perkins KA, Marcus MD, Levine MD, et al. Cognitive-behavioral therapy to reduce weight concerns improves smoking cessation outcome in weight-concerned women. J Consult Clin Psychol. 2001;69(4):604–613. [PubMed] [Google Scholar]
- 35. Levine MD, Perkins KA, Kalarchian MA, et al. Bupropion and cognitive behavioral therapy for weight-concerned women smokers. Arch Intern Med. 2010;170(6):543–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. LaRowe TL, Piper ME, Schlam TR, Fiore MC, Baker TB. Obesity and smoking: comparing cessation treatment seekers with the general smoking population. Obesity (Silver Spring). 2009;17(6):1301–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Prochaska JJ, Prochaska JO. A review of multiple health behavior change interventions for primary prevention. Am J Lifestyle Med. 2011;5(3):208–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. James E, Freund M, Booth A, et al. Comparative efficacy of simultaneous versus sequential multiple health behavior change interventions among adults: A systematic review of randomised trials. Prev Med. 2016;89:211–223. [DOI] [PubMed] [Google Scholar]
- 39. Spring B, Howe D, Berendsen M, et al. Behavioral intervention to promote smoking cessation and prevent weight gain: a systematic review and meta-analysis. Addiction. 2009;104(9):1472–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]