Abstract
Purpose
Geospatial, contextual, and multilevel research is integral to cancer prevention and control. NCI-designated Cancer Centers are at the forefront of cancer research, therefore this paper sought to review the geospatial, contextual, and multilevel research at these cancer centers.
Methods
Investigators used PubMed and Web of Science to compile geospatial publications from 1971 to February 2016 with cancer center-affiliated authors. Relevant abstracts were pulled and classified by six geospatial approaches, eight geospatial scales, and eight cancer sites.
Results
The searches identified 802 geospatial, contextual, and multilevel publications with authors affiliated at 60 of the 68 NCI-designated Cancer Centers. Over 90% were published after 2000. Five cancer centers accounted for approximately 50% of total publications, and 30 cancer centers (less than half) accounted for over 85% of total publications. Publications covered all geospatial approaches and scales to varying degrees, and 90% dealt with cancer.
Conclusions
The NCI-designated Cancer Center network is increasingly pursuing geospatial, contextual, and multilevel cancer research, although many cancer centers still conduct limited to no research in this area. Expanding geospatial efforts to research programs across all cancer centers will further enrich cancer prevention and control. Similar reviews may benefit other domestic and international cancer research institutions.
Keywords: cancer, geospatial, contextual, multilevel, geography, neighborhood
Introduction
Geospatial methods have advanced rapidly in recent decades to include geographic information systems (GIS), Global Positioning Systems (GPS), and other location-based technology alongside improved mapping techniques. This methodological progress has transformed geospatial data collection and multilevel analysis, and holds significant promise to enhance cancer research across the entire cancer control continuum [1–3]. The National Cancer Institute (NCI) in the United States has supported geospatial, contextual, and multilevel cancer research for over 40 years. NCI-affiliated researchers published state-level cancer mortality rates as early as 1971 [4, 5], followed by county-level cancer mortality rates in 1974 [5, 6]. In 1973, NCI also initiated the Surveillance, Epidemiology, and End Results (SEER) program to compile detailed cancer incidence, mortality, and survival data across diverse U.S. regions and cohorts [7], and has since added several web resources conducive to geospatial cancer analysis [8, 9].
Internationally, cancer control researchers and public health agencies have also demonstrated commitment to applying geospatial approaches. The International Agency for Research on Cancer (IARC) and the International Association of Cancer Registries (IACR), organizations both associated with the World Health Organization (WHO), regularly compile global cancer data into comprehensive reports and interactive graphics that facilitate geospatial cancer analysis [10–12]. These activities complement specific research projects in many countries. Examples include mapping colorectal cancer incidence in China [13], assessing area-level socioeconomic components and testicular cancer survival in England [14], and examining air quality and cancer mortality in Brazil [15].
One prominent feature of the U.S. cancer research landscape is the NCI-designated Cancer Center network, which has grown to 69 cancer centers that cover geographically and demographically diverse catchment areas [16]. NCI-designated Cancer Centers have applied a geospatial perspective to cancer research since at least the 1980s [17], but this research has not been explored systematically. The purpose of this paper was to summarize the level and scope of geospatial, contextual, and multilevel research conducted by researchers affiliated with NCI-designated Cancer Centers. Future reviews could mirror the approach described here to summarize the penetration of geospatial research into the cancer control efforts of diverse institutions and countries.
Methods
A comprehensive literature search was conducted in PubMed and Web of Science in March 2016 to identify geospatial, contextual, and multilevel research that included one or more authors reporting an affiliation with one or more NCI-designated Cancer Centers. The keywords “geospatial OR spatial OR contextual OR multilevel OR county OR neighborhood OR residence OR environment OR urban OR rural OR geography OR geographic OR census OR resident characteristics OR latitude OR latitudes” were searched in combination with 112 cancer center name variations (Online Resource 1). These searches captured research at 68 of the 69 NCI-designated Cancer Centers; the Tisch Cancer Institute at Mount Sinai had not received NCI designation at the start of the search process and was therefore omitted.
For consideration, studies had to be published between January 1971 and February 2016, involve at least one author with an NCI-designated Cancer Center affiliation, include one or more of the designated keywords in the title or abstract, and contain a spatial comparison between at least two different locations. Thus, a study that investigated travel time to cancer treatment for different sites within Western Washington [18] would be included, but a study that investigated cancer incidence in the general Western Washington region [19] would be omitted. Although both studies satisfied the first three criteria listed above, the former compared different areas within a region, while the latter reported on one area without an intra- or inter-regional comparison. Titles and abstracts were screened and relevant abstracts were then collated and coded by geospatial approach, cancer site, and geospatial scale. After iterative work to establish definitions for geospatial approach and cancer site, one PhD-level reviewer and one Master’s-level reviewer dual coded 11.5% of the abstracts to further refine the categories selected. The remaining abstracts were coded by a single reviewer. Subsequently, one PhD-level reviewer and one Bachelor’s-level reviewer dual coded 12.5% of the abstracts to establish a coding scheme by geospatial scale. The remaining abstracts were coded by a single reviewer. Topic area experts from the NCI Division of Cancer Control and Population Sciences supervised this process and contributed when questions arose concerning specific abstracts.
Investigators classified abstracts by six geospatial approaches: 1) spatial distribution, 2) proximities, 3) urban/rural differences, 4) community environment, 5) geospatial methods/mathematical models, and 6) environmental health. Descriptions and examples for each category are listed in Table 1 [20–25]. Abstracts that dealt with both community environment and spatial distribution were categorized as community environment. Abstracts that dealt with urban/rural differences as well as spatial distribution and/or community environment were categorized as urban/rural differences. Abstracts that dealt with proximities as well as spatial distribution, urban/rural differences, and/or community environment were categorized as proximities. Investigators also classified abstracts by eight cancer site categories: 1) breast, 2) prostate, 3) colorectal, 4) other site (e.g., cervical, lung, melanoma), 5) several sites, 6) all cancers/mortality, 7) cancer risk factors and prevention, and 8) non-cancer outcomes. Investigators then classified abstracts by eight geospatial scales: 1) continents and countries, 2) states, provinces, and multi-state regions, 3) cities and counties, 4) zip codes, census tracts, and block groups, 5) urban/rural area, 6) coordinates and exact locations, 7) neighborhoods and communities, and 8) unspecified geographic area. Abstracts that discussed multiple scales were assigned to the scale with the finest unit of analysis mentioned; for this review, unspecified geographic area was considered the largest scale, while coordinates and exact location was considered the smallest scale. For example, if an abstract mentioned an unspecified geographic area and census tracts, it was assigned to group four.
Table 1.
Descriptions and examplesa of the six geospatial approach categories used to classify abstracts
| Geospatial Approach | Description | Example |
|---|---|---|
| Spatial Distribution | Compares ≥ 2 geographic locations (e.g., countries, states, counties, latitudes) | “describe the county-level geographic distribution of human papillomavirus (HPV) vaccine coverage among young women aged 18–26 in Texas” [20] |
| Proximities | Investigates distance or travel time to health care resources | “evaluated associations between overall survival and progression-free survival and the distance from the patient residence to the treating institution” [21] |
| Urban/Rural Differences | Specifically compares urban, suburban, and rural areas; metropolitan and non-metropolitan areas | “evaluated the effect of rural versus urban residence on colon cancer risk and stage of disease at diagnosis” [22] |
| Community Environment | Assesses geographic contextual factors (e.g., built environment, socioeconomic indicators) | “examined associations between census-tract poverty and [colorectal cancer] incidence and stage” [23] |
| Geospatial Methods / Mathematical Models | Tests innovative technologies and data analysis techniques | “review [Kernel density estimation], and introduce the technique of utilizing an adaptive bandwidth to address the underlying heterogeneous population distributions common in public health research” [24] |
| Environmental Health | Examines geographic differences in toxins and other exposures | “evaluating the association between traffic-related hazardous air pollutants [i.e., census tract-level pollutant concentrations] and the incidence of childhood central nervous system (CNS) tumors” [25] |
Use of these six examples is in no way an endorsement of the research, authors, or institutions involved
Results
The literature searches yielded 5,410 PubMed citations and 10,004 Web of Science citations, which resulted in 9,881 unique citations screened. Citations that did not include abstracts (n=10) or address geospatial approaches to cancer despite including one or more keywords (n=9,069) were excluded. This left 802 total publications that involved geospatial, contextual, and multilevel research coauthored by researchers affiliated with NCI-designated Cancer Centers. Approximately 85% of publications (n=685) involved a single cancer center, while the remaining 117 publications were shared by two (n=92), three (n=16), four (n=4), five (n=1), six (n=1) and eight (n=3) cancer centers. The first published geospatial study affiliated with an NCI-designated Cancer Center appeared in 1980, but few studies were published until after 2000. Over 90% (n=725) of the 802 identified publications appeared after 2000, with 59% (n=472) published since 2010.
Almost 90% (n=60) of NCI-designated Cancer Centers participated in geospatial, contextual, and multilevel research published between 1971 and February 2016. The eight cancer centers that did not included one Cancer Center and seven Basic Laboratory Cancer Centers (see Online Resource 2 for publication totals by cancer center). The average number of publications per cancer center was 14. Omitting the Basic Laboratory Cancer Centers increased this to 16 publications. A small minority of cancer centers, however, accounted for the majority of all publications (Figure 1). The five cancer centers with the most publications were Fred Hutchinson/University of Washington Cancer Consortium (n=127), Dana-Farber/Harvard Cancer Center (n=109), The University of Texas MD Anderson Cancer Center (n=109), Memorial Sloan-Kettering Cancer Center (n=73), and Alvin J. Siteman Cancer Center (n=55) (Online Resource 2). Publications that involved only these five cancer centers comprised approximately 50% (n=383) of the total identified geospatial studies with an NCI-designated Cancer Center affiliation. Fifteen cancer centers comprised over 70% (n=564) of the total identified publications, and just under half of all cancer centers contributed to over 85% (n=693) of the total yield. These results were similar regardless of whether the 117 shared studies were assigned to the affiliated cancer center with the most or the least publications (Figure 1).
Fig. 1.
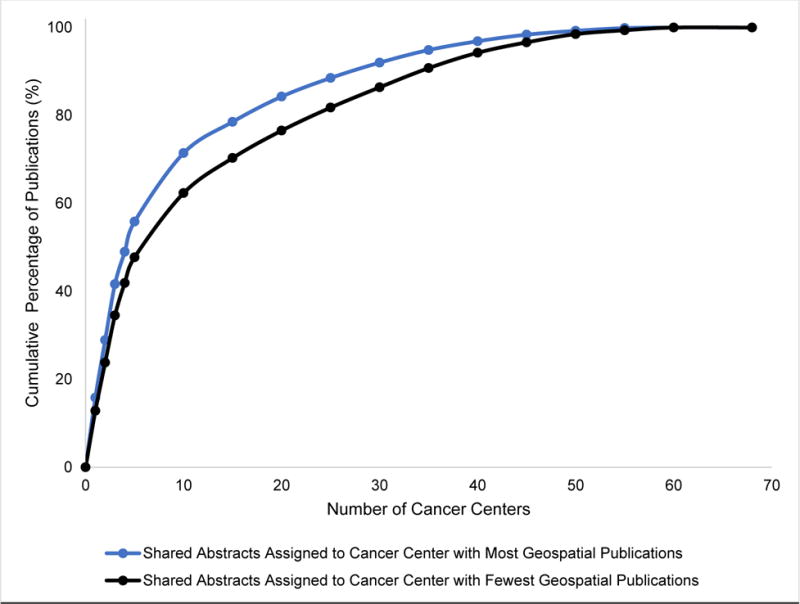
Cumulative percentage of geospatial publications across NCI-designated Cancer Centers. The upper line assigns abstracts with two or more distinct cancer center affiliations to the cancer center with the most geospatial publications. The lower line assigns abstracts with two or more distinct cancer center affiliations to the cancer center with the fewest geospatial publications. The circular markers represent 0, 1, 2, 3, 4, 5, 10, 15, 20, 25, 30, 35, 40, 45, 50, 55, 60, and 68 cancer centers, respectively
Publications encompassed a variety of geospatial approaches, as shown in Figure 2A. Over 40% (n=343) dealt primarily with the spatial distribution of disease rates, health behaviors, and other public health topics. Studies that primarily investigated community-level factors (n=172) and urban/rural differences (n=154) each contributed to 20% of the total. The remaining publications (n=133) examined environmental exposures, proximity to health services, and geospatial methodologies. Additionally, over 90% of publications (n=723) focused on cancer or cancer-related health behaviors, as depicted in Figure 2B. Half (n=403) investigated one cancer, and an additional 15% (n=122) looked at all cancers or all-cause mortality. Breast, prostate, and colorectal cancer, in that order, were the most common cancers assessed; additional cancers included cervical cancer, lung cancer, melanoma, and lymphoma. For the 10% (n=79) of publications on non-cancer outcomes, research topics included HIV, cardiovascular disease, and mental health. There was also variation in geospatial scale among publications, as illustrated in Figure 2C. Almost 12% (n=95) investigated primarily at the country level, with an additional 20% at either the state or county levels. Another 16% (n=127) used urban/rural area, while 14% (n=114) used exact locations. Slightly fewer abstracts used census tracts or employed a neighborhood scale. Unspecified geographic area was the most prevalent spatial scale mentioned in abstracts and accounted for 18.5% (n=148) of publications.
Fig. 2a.
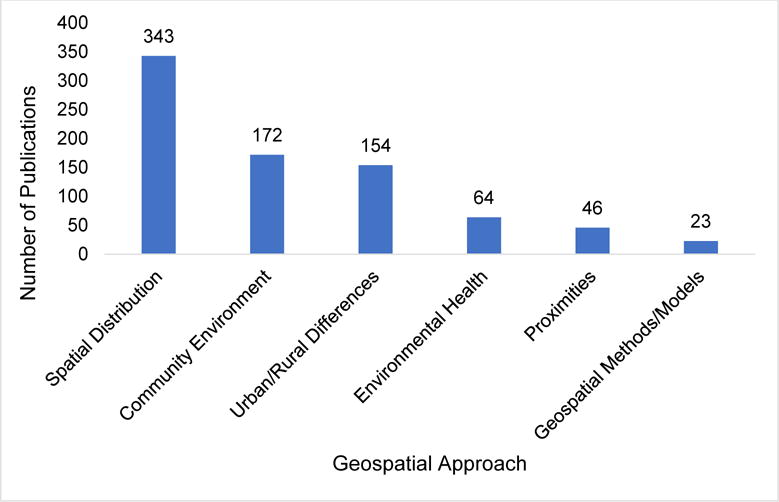
Number of publications per geospatial approach
Fig. 2b.
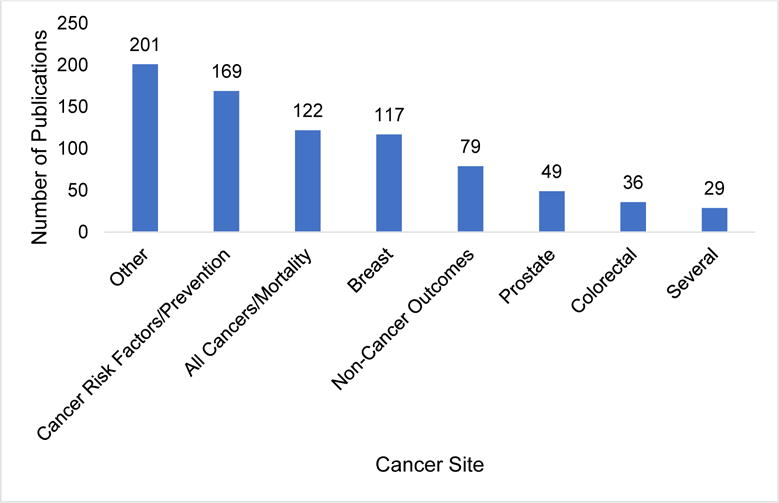
Number of publications per cancer site
Fig. 2c.
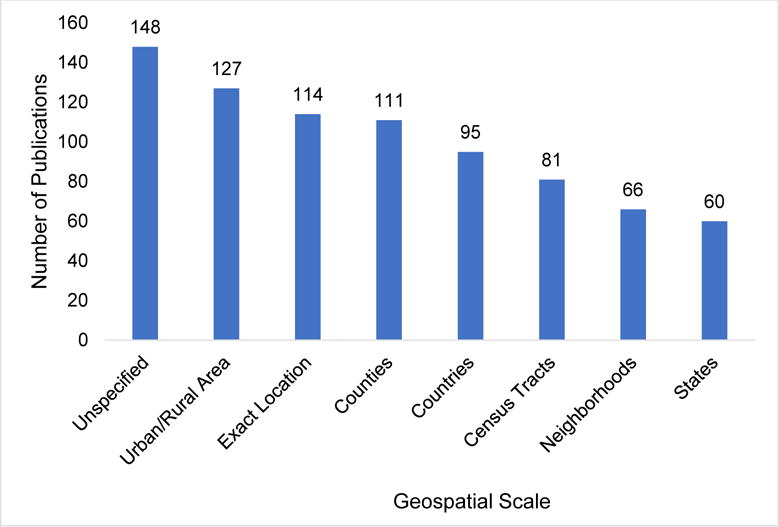
Number of publications per geospatial scale
Discussion
This analysis indicates that NCI-designated Cancer Centers contribute to a broad array of geospatial, contextual, and multilevel research, although this commitment varies widely by cancer center. Overall, there are three notable elements that characterize the geospatial research landscape at NCI-designated Cancer Centers. First, geospatial cancer research at most centers is at an early stage but is also growing at some centers, with nearly all studies published after 2000 and most published after 2010. This finding coincides with rapid growth in tools, methods, and computational capabilities relevant to the geospatial field. Second, geospatial research among NCI-designated Cancer Centers is relatively concentrated – five institutions were the sole cancer centers affiliated with approximately 50% of all identified publications. Over half of cancer centers contributed to less than 15% of the total, even if the seven Basic Laboratory Cancer Centers are excluded. Some institutions are larger and receive more funding than others, therefore it is not expected that each contributes equally to geospatial cancer research; it is plausible that given their available resources, the top five cancer centers publishing geospatial research should be responsible for half of the total publication yield. The observation that over half of cancer centers have published minimally in this area, however, suggests that many of these institutions have limited expertise in this area of research or do not consider it to be a priority.
Lastly, geospatial research at these cancer centers, as presented in abstracts, covers a variety of geospatial scales, approaches, and cancer sites but still leans toward the descriptive. The presence of multiple scales in the abstracts of this body of work is encouraging given that different scales are more appropriate for distinct geospatial research questions, and solely relying on one or two may ignore broad swaths of the geospatial research landscape. Still, the almost 20% of abstracts that described an unclear geographic area indicate that investigators should consider including more specific details when summarizing their research. This would likely entail adding only a few words (e.g., changing “geographic location” to “U.S. Census region”).
Regarding geospatial approaches, a plurality of studies focused primarily on documenting the spatial distributions of cancer incidence and mortality or cancer-related exposures. Many of these papers reported differences among countries, states, or counties. Nonetheless, other studies did examine specific contextual features and often used multilevel analysis alongside descriptive statistics. These studies typically categorized administrative regions according to urban/rural classifications [22] or socioeconomic status [23], or overlaid spatial data with travel distances [21] or toxicity information [25]. This divergence reflects the combined themes of “spatial” and “platial” perspectives that constitute much of current geospatial research [26]. Place complements, not supplants, geographic space by incorporating psychosocial inputs, historical dynamics, multilevel factors, and other contextual elements that can yield deeper, more refined insights into the what, how, and why of cancer-related outcomes and risk factors [26, 27]. Promoting space and place perspectives in tandem at NCI-designated Cancer Centers may bolster research to better understand population health and determine how geospatial thinking may contribute to research across the entire cancer control continuum.
There are several key challenges to fulfilling the promise of geospatial research concerning cancer control. One involves the difficulty of working with existing data. Investigators interested in aggregating multiple data sets, such as those from several SEER registries or from extant cohort studies, are often required to submit separate proposals for IRB approval to each data source. In addition, SEER-Medicare data regulations dictate that only investigators at the requesting institution may analyze the data [28]. This organizational feature represents a significant barrier to collaboration and data aggregation and analysis. Clearly, it arises because home address and other spatial data are personal identifiers linked to sensitive health and other data. Adequate tools to allow analysis of such data while safeguarding privacy exist but have not been widely tested or adopted, which in the meantime stymies data sharing and impedes other researchers from reproducing or expanding upon prior research [2, 29]. The Beau Biden Cancer MoonshotSM initiative is supporting NCI efforts to develop a Cancer Data Ecosystem [30]; such an “ecosystem” could include elements designed to facilitate analysis of geospatial data while protecting privacy.
Given the mounting interest in applying geospatial approaches to cancer research, NCI held its first Conference on Geospatial Approaches to Cancer Control and Population Sciences in September 2016 [31] to share current research efforts and establish future directions for the field. Discussions culminated in a Cancer Epidemiology, Biomarkers & Prevention (CEPB) journal focus issue in April 2017 with 12 original articles and two thought pieces, of which five included cancer center-affiliated researchers [32]. The articles coalesced around two primary themes that may help guide future geospatial cancer research: health disparities and novel operational definitions of the environment. Geospatial research for cancer control can contribute to describing existing and emerging cancer disparities and elucidating their underlying causes; for example, several papers highlighted the importance of residential segregation as a correlate of observed disparate cancer outcomes [27, 33, 34]. Additionally, etiologic and intervention studies could benefit from innovative environmental metrics such as measures of zoning or “green” environmental elements, as well as from gathering more comprehensive residential histories [2, 35, 36].
In fact, this latter theme ties into a rapidly evolving methodological research area that may also be worth pursuing for cancer control – further developing groundbreaking techniques to collect and analyze geospatial data. For example, better spatial data and community input could be obtained via community-based participatory approaches, mixed methods, or citizen science. By providing a stronger grassroots perspective on space and place, these approaches potentially afford researchers a source of both highly granular geographic data and critical measures of spatially delineated social and cultural factors that could enhance population-level cancer research [37, 38].
Conclusions
Many NCI-designated Cancer Centers (and potentially cancer research centers worldwide) appear to lack active research programs using geospatial, contextual, and multilevel approaches to understand cancer incidence, mortality, and control. No biomedical researcher would plan or conduct a study without a statistician as part of the research team; by contrast, geographers are often consulted when studies are near completion with the somewhat plaintive question – “It looks like the geographic areas I studied differ, how can I address that in my analysis?” Cancer prevention and control research often spans multiple disciplines and may be enhanced by transdisciplinary teams [39, 40]. A growing emphasis on space and place as correlates of health and health disparities, as well as recent interest in better defining and serving cancer center catchment areas, suggest that investment in geospatial expertise and collaboration could accelerate progress in addressing cancer prevention and control. This review provides information about a specific class of U.S. cancer centers, although the observations detailed here may be applicable to other cancer research programs and institutions. Similar analyses in other countries could be useful to inform funding decisions by policymakers and to stimulate research on geospatial approaches to cancer control.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge Drs. Gary Ellison and Stephen Taplin, members of the National Cancer Institute (NCI) multilevel, contextual, and geospatial working group, for discussion and comments.
Compliance with Ethical Standards: This article does not contain any studies with human participants or animals performed by any of the authors.
Funding Support: The authors declare no specific sources of funding.
Footnotes
Author Contributions: DB conceived of, and DB and AYO oversaw, the project; RWK, BLT, MAC, and BB carried out the searches, screened abstracts, and helped develop scoring criteria. RWK analyzed results and drafted the paper. All authors edited successive versions of the paper.
The authors declare that they have no conflict of interest.
Contributor Information
Robert W Korycinski, Division of Cancer Prevention, National Cancer Institute, Bethesda, MD 20892; http://orcid.org/0000-0002-2870-2130.
Bethany L Tennant, ICF, Fairfax, VA 22031.
Michelle A Cawley, ICF, Fairfax, VA 22031.
Bonny Bloodgood, ICF, Fairfax, VA 22031.
April Y Oh, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD 20892.
David Berrigan, Division of Cancer Control and Population Sciences, National Cancer Institute, Bethesda, MD 20892.
References
- 1.Richardson DB, Volkow ND, Kwan MP, Kaplan RM, Goodchild MF, Croyle RT. Spatial turn in health research. Science. 2013;339:1390–1392. doi: 10.1126/science.1232257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schootman M, Gomez SL, Henry KA, Paskett ED, Ellison GL, Oh A, Taplin SH, Tatalovich Z, Berrigan DA. Geospatial approaches to cancer control and population sciences. Cancer Epidemiol Biomarkers Prev. 2017;26:472–475. doi: 10.1158/1055-9965.EPI-17-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002;156:471–482. doi: 10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 4.Burbank F. Patterns in cancer mortality in the United States: 1950-1967. Natl Cancer Inst Monogr. 1971;71:1–594. [PubMed] [Google Scholar]
- 5.Mason TJ, McKay FW, Hoover R, Blot WJ, Fraumeni JF., Jr . Atlas of Cancer Mortality for U.S. Counties: 1950–1969. U.S. Department of Health, Education, and Welfare; 1975. https://archive.org/details/atlasofcancermor00nati_0. Accessed 14 August 2017. [Google Scholar]
- 6.Mason TJ, McKay FW. U.S. Cancer Mortality by County: 1950–1969. U.S. Department of Health, Education, and Welfare; 1974. https://catalog.hathitrust.org/Record/011324517. Accessed 14 August 2017. [Google Scholar]
- 7.National Cancer Institute (n.d.) About the SEER program. https://seer.cancer.gov/about/index.html. Accessed 22 May 2017
- 8.National Cancer Institute (n.d.) Geographic information systems and science for cancer control. https://gis.cancer.gov/. Accessed 22 May 2017.
- 9.National Cancer Institute, Centers for Disease Control and Prevention (n.d.) State cancer profiles. https://statecancerprofiles.cancer.gov/index.html. Accessed 22 May 2017.
- 10.Forman D, Bray F, Brewster DH, Gombe Mbalawa C, Kohler B, Piñeros M, Steliarova-Foucher E, Swaminathan R, Ferlay J. Cancer incidence in five continents volume X. IARC Scientific Publications; 2014. http://publications.iarc.fr/Book-And-Report-Series/Iarc-Scientific-Publications/Cancer-Incidence-In-Five-Continents-Volume-X-2014. Accessed 15 August 2017. [DOI] [PubMed] [Google Scholar]
- 11.Boyle P, Smans M. IARC Scientific Publications; 2008. Atlas of cancer mortality in the European Union and the European Economic Area 1993–1997. http://publications.iarc.fr/Book-And-Report-Series/Iarc-Scientific-Publications/Atlas-Of-Cancer-Mortality-In-The-European-Union-And-The-European-Economic-Area-1993-1997-2008. Accessed 15 August 2017. [PubMed] [Google Scholar]
- 12.International Agency for Research on Cancer (n.d.) Cancer today. http://gco.iarc.fr/today/home. Accessed 15 August 2017.
- 13.Li K, Lin GZ, Li Y, Dong H, Xu H, Song SF, Liang YR, Liu HZ. Spatio-temporal analysis of the incidence of colorectal cancer in Guangzhou, 2010-2014. Chin J Cancer. 2017;36:60. doi: 10.1186/s40880-017-0231-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McNally RJ, Basta NO, Errington S, James PW, Norman PD, Hale JP, Pearce MS. Socioeconomic patterning in the incidence and survival of teenage and young adult men aged between 15 and 24 years diagnosed with non-seminoma testicular cancer in northern England. Urol Oncol. 2015;33:506.e9–506.e14. doi: 10.1016/j.urolonc.2015.07.014. [DOI] [PubMed] [Google Scholar]
- 15.Yanagi Y, de Assunção JV, Barrozo LV. The impact of atmospheric particulate matter on cancer incidence and mortality in the city of São Paulo, Brazil. Cad Saude Publica. 2012;28:1737–1748. doi: 10.1590/S0102-311X2012000900012. [DOI] [PubMed] [Google Scholar]
- 16.National Cancer Institute (n.d.) NCI-designated cancer centers. https://www.cancer.gov/research/nci-role/cancer-centers. Accessed 22 May 2017.
- 17.Polissar L. The effect of migration on comparison of disease rates in geographic studies in the United States. Am J Epidemiol. 1980;111:175–182. doi: 10.1093/oxfordjournals.aje.a112885. [DOI] [PubMed] [Google Scholar]
- 18.Onega T, Cook A, Kirlin B, Shi X, Alford-Teaster J, Tuzzio L, Buist DS. The influence of travel time on breast cancer characteristics, receipt of primary therapy, and surveillance mammography. Breast Cancer Res Treat. 2011;129:269–275. doi: 10.1007/s10549-011-1549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norsted TL, White E. Cancer incidence among native Americans of western Washington. Int J Epidemiol. 1989;18:22–27. doi: 10.1093/ije/18.1.22. [DOI] [PubMed] [Google Scholar]
- 20.Eberth JM, Zhang X, Hossain M, Tiro JA, Holt JB, Vernon SW. County-level estimates of human papillomavirus vaccine coverage among young adult women in Texas, 2008. Tex Public Health J. 2013;65:37–40. [PMC free article] [PubMed] [Google Scholar]
- 21.Lamont EB, Hayreh D, Pickett KE, Dignam JJ, List MA, Stenson KM, Haraf DJ, Brockstein BE, Sellergren SA, Vokes EE. Is patient travel distance associated with survival on phase II clinical trials in oncology? J Natl Cancer Inst. 2003;95:1370–1375. doi: 10.1093/jnci/djg035. [DOI] [PubMed] [Google Scholar]
- 22.Kinney AY, Harrell J, Slattery M, Martin C, Sandler RS. Rural-urban differences in colon cancer risk in blacks and whites: the North Carolina Colon Cancer Study. J Rural Health. 2006;22:124–130. doi: 10.1111/j.1748-0361.2006.00021.x. [DOI] [PubMed] [Google Scholar]
- 23.Henry KA, Sherman RL, McDonald K, Johnson CJ, Lin G, Stroup AM, Boscoe FP. Associations of census-tract poverty with subsite-specific colorectal cancer incidence rates and stage of disease at diagnosis in the United States. J Cancer Epidemiol. 2014 doi: 10.1155/2014/823484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carlos HA, Shi X, Sargent J, Tanski S, Berke EM. Density estimation and adaptive bandwidths: a primer for public health practitioners. Int J Health Geogr. 2010;9:39. doi: 10.1186/1476-072X-9-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Danysh HE, Mitchell LE, Zhang K, Scheurer ME, Lupo P. Traffic-related air pollution and the incidence of childhood central nervous system tumors: Texas, 2001-2009. Pediatr Blood Cancer. 2015;62:1572–1578. doi: 10.1002/pbc.25549. [DOI] [PubMed] [Google Scholar]
- 26.Goodchild MF. Space, place and health. Ann GIS. 2015;21:97–100. doi: 10.1080/19475683.2015.1007895. [DOI] [Google Scholar]
- 27.Krieger N. Follow the North Star: why space, place, and power matter for geospatial approaches to cancer control and health equity. Cancer Epidemiol Biomarkers Prev. 2017;26:476–479. doi: 10.1158/1055-9965.EPI-16-1018. [DOI] [PubMed] [Google Scholar]
- 28.National Cancer Institute. SEER-Medicare: required documents & instructions for submitting requests. 2017 https://healthcaredelivery.cancer.gov/seermedicare/obtain/requests.html. Accessed 20 December 2017.
- 29.Richardson DB, Kwan MP, Alter G, McKendry JE. Replication of scientific research: addressing geoprivacy, confidentiality, and data sharing challenges in geospatial research. Ann GIS. 2015;21:101–110. doi: 10.1080/19475683.2015.1027792. [DOI] [Google Scholar]
- 30.Blue Ribbon Panel. Cancer Moonshot Blue Ribbon Panel report 2016. 2016 https://www.cancer.gov/research/key-initiatives/moonshot-cancer-initiative/blue-ribbon-panel#ui-id-3. Accessed 1 June 2017.
- 31.National Cancer Institute. Conference on geospatial approaches to cancer control and population sciences. 2016 https://epi.grants.cancer.gov/events/geospatial/. Accessed 2 June 2017.
- 32.Cancer Epidemiology, Biomarkers & Prevention. Table of contents. 2017 http://cebp.aacrjournals.org/content/26/4. Accessed 2 June 2017.
- 33.Bemanian A, Beyer KMM. Measures matter: the local exposure/isolation (LEx/Is) metrics and relationships between local-level segregation and breast cancer survival. Cancer Epidemiol Biomarkers Prev. 2017;26:516–524. doi: 10.1158/1055-9965.EPI-16-0926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou Y, Bemanian A, Beyer KMM. Housing discrimination, residential racial segregation, and colorectal cancer survival in southeastern Wisconsin. Cancer Epidemiol Biomarkers Prev. 2017;26:561–568. doi: 10.1158/1055-9965.EPI-16-0929. [DOI] [PubMed] [Google Scholar]
- 35.Nicholson LM, Leider J, Chriqui JF. Exploring the linkage between activity-friendly zoning, inactivity, and cancer incidence in the United States. Cancer Epidemiol Biomarkers Prev. 2017;26:578–586. doi: 10.1158/1055-9965.EPI-16-0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.James P, Hart JE, Hipp JA, Mitchell JA, Kerr J, Hurvitz PM, Glanz K, Laden F. GPS-based exposure to greenness and walkability and accelerometry-based physical activity. Cancer Epidemiol Biomarkers Prev. 2017;26:525–532. doi: 10.1158/1055-9965.EPI-16-0925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.King AC, Winter SJ, Sheats JL, et al. Leveraging citizen science and information technology for population physical activity promotion. Transl J Am Coll Sports Med. 2016;1:30–44. doi: 10.1249/TJX.0000000000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rosas LG, Salvo D, Winter SJ, Cortes D, Rivera J, Rodriguez NM, King AC. Harnessing technology and citizen science to support neighborhoods that promote active living in Mexico. J Urban Health. 2016;93:953–973. doi: 10.1007/s11524-016-0081-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hall KL, Feng AX, Moser RP, Stokols D, Taylor BK. Moving the science of team science forward: collaboration and creativity. Am J Prev Med. 2008;35:S243–S249. doi: 10.1016/j.amepre.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hall KL, Stokols D, Stipelman BA, Vogel AL, Feng A, Masimore B, Morgan G, Moser RP, Marcus SE, Berrigan D. Assessing the value of team science: a study comparing center- and investigator-initiated grants. Am J Prev Med. 2012;42:157–163. doi: 10.1016/j.amepre.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


