ABSTRACT
Background: The incidence of measles in Yunnan Province among vaccine target-age children has decreased markedly after attaining and sustaining high 2-dose coverage of measles containing vaccine (MCV) through routine immunization services and supplementary immunization activities (SIAs). Most cases of measles now occur among adults. In 2015, we investigated a measles outbreak among adults to determine transmission patterns and the potential role of nosocomial transmission.
Methods: We enhanced measles surveillance using retrospective active case search. We conducted case investigations to determine sources of infection and routes of transmission; laboratory testing included serologic and molecular diagnostic methods.
Results: Twenty-two outbreak-associated cases of measles were identified; most (86.36%) were among individuals 20 to 39 years of age (range, 7 months to 43 years). We interviewed 19 individuals who had acquired measles. The first 3 cases were infected in Tibet; 12 (63%) were hospital-acquired infections; 2 (11%) were community-acquired; and 2 (11%) were family-contact cases. We conducted outbreak response immunization (ORI) that provided MCV without regard to vaccination status; 10,596 residents between 20 and 40 years of age were vaccinated. A serological survey conducted during the ORI showed that 84% of the 20–40 year-olds were immune to measles prior to vaccination. Post-vaccination serological testing showed 100% were immune.
Conclusions: Despite high population immunity among children and adolescents, imported measles virus transmission occurred among adults in a provincial cross-border area. Nosocomial transmission and measles immunity gaps among adults poses a threat to measles elimination and highlights the strategy of targeting adults during ORI to outbreaks with adult-to-adult transmission.
KEYWORDS: Measles, Outbreak, Adult, Approach, Elimination
Introduction
Prior to 1965, the annual reported measles incidence in Yunnan Province, China was greater than 1,700 cases per million population. In 1978, a one-dose, liquid-formulated measles vaccine (MV) schedule was established, with the dose administered at 8 months of age. In 1986, a 2-dose, lyophilized-preparation MV schedule was recommended, with the first dose at 8 months and the second at 7 years. In 2008, the Expanded Program on Immunization (EPI) changed the schedule to measles-rubella (MR) vaccine at 8 months and measles-mumps-rubella (MMR) vaccine at 18 months. Seroconversion to the 8-month MV dose is 94%.1 In 2008, a series of supplementary immunization activities (SIA) were used to vaccinate children born between 1992 and 2008, regardless of previous vaccination history. In November 2010, another SIA was conducted that targeted children born in 2009 and early 2010.
Continuous use of the 2-dose measles-containing vaccine (MCV) vaccination policy since 1986, coupled with the comprehensive SIA strategy, led to a marked decrease in measles, so that by 2010 a record low of only 100 cases of measles were reported. Between 2006 and 2016, the incidence of measles decreased by over 95%, and during this time the age distribution of measles cases changed – since 2009, few measles cases have been reported from age-groups targeted by SIAs, and the percentage of cases in the over-15-year-old age group increased from 17% before the series of SIAs to 28% in 2015.
During the measles elimination period, a stated research need is to identify the role of adults in measles virus transmission.2,3 Generally, adult measles is correlated with the incidence among children. The great reduction of measles incidence in every age group in Yunnan province – including children and adults – supports this assessment,4,5 which implies that high immunization rates among children will provide adequate herd immunity to prevent measles among adults. However, we have recently seen measles outbreaks in Yunnan among adults without documented transmission from children, raising our concern that susceptible adults could sustain transmission in community settings.
We report a measles outbreak in Deqin County (DQ) that followed an importation to Yunnan in 2015. We describe measles virus transmission from imported cases to local residents, including adult-to-adult transmission and adult-to-infant transmission. We describe sources of infection and the effect of outbreak response immunization, and we suggest control measures targeting adults.
Results
Outbreak profile
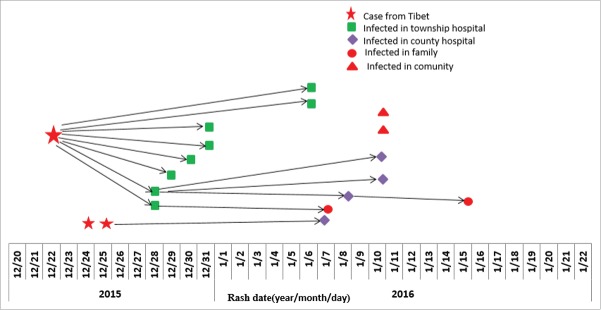
In total, 22 measles cases were confirmed out of 43 suspected cases, including 3 Tibet residents from the same community. The remaining 21 (48.84%, 21/43) suspected cases were discarded as neither measles nor rubella by laboratory testing. Among the 22 confirmed cases, their illness onset dates were between December 16, 2015 and January 21, 2016 (Figure 1). The male-to-female ratio was 1.75; there were no deaths. The 22 cases ranged in age from 7 months to 43 years. The majority (86.36%, 19/22) were young adults aged 20–39 years. By residency status, local cases resided in F township and S township, and the incidence rates were 0.33% (13/3,990) and 0.07% (6/8,625), respectively. The overall incidence of 31.73/100,000 for this outbreak was higher than that of any corresponding period between 2010 and 2014. Among the 22 cases, 20 (90.91%) had unknown vaccination status; the remaining 2 cases were documented to have been unvaccinated against measles.
Figure 1.
Number of reported measles cases by onset date and outbreak response vaccination.
All cases were laboratory confirmed; 16 were positive for measles IgM, and 20 cases had positive RT-PCR results. We conducted genetic sequencing for 3 cases: the index case from Tibet and 2 cases among local residents. Sequence analysis of the C-terminal 450 nucleotides of the N gene of 3 isolates revealed identical sequences of genotype H1a, the endemic genotype in China, suggesting a single chain of transmission. (Figure 2). The sequences of these viruses were closely related to the sequences of Chin9322/H1a that was one of the WHO reference strains available from GenBank. The minimum nucleotide divergence between the viruses and the H1a WHO reference strain (Chin9322) was 2% for the N gene and 2% for the H gene.
Figure 2.
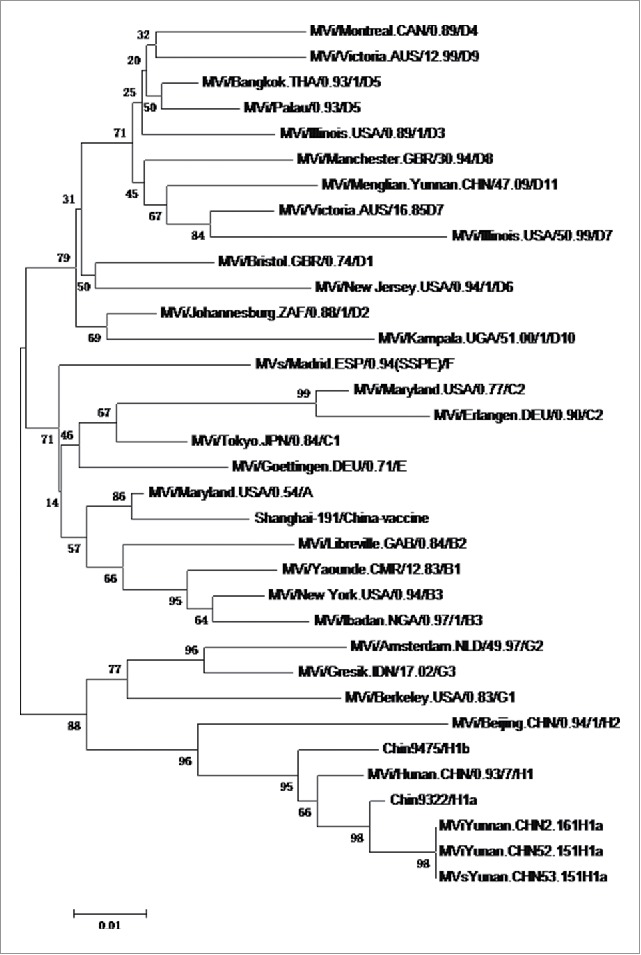
Phylogenetic analysis of the sequences of the nucleoprotein genes (450 nt) of the strains of measles virus from Deqin County, Yunnan Province, People's Republic of China. The tree shows sequences from Deqin viruses (circles) compared with World Health Organization (WHO) reference strains for each genotype. Scale bar indicates base substitutions per site.
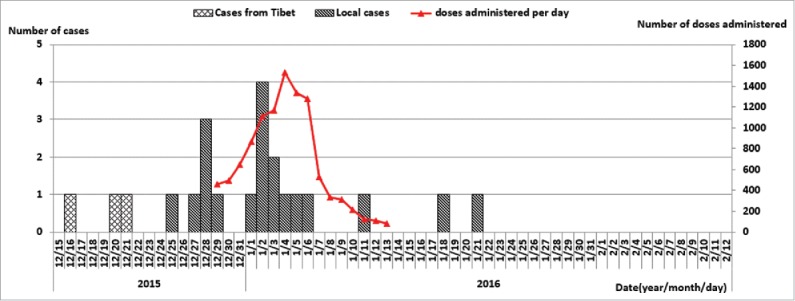
Chains of transmission
We interviewed 19 (86%) of the 22 confirmed cases. We found direct and indirect contact among these cases. Three (16%) were imported cases from Tibet, outside of the county; 2 (11%) were community acquired cases, 2 (11%) were family-contact cases, and 12 (63%) were hospital-contact cases (Figure 3).
Figure 3.
Transmission chains of measles cases with contact histories.
The index case was a 27-year-old man from Tibet who visited DQ County. He had fever on December 16, 2015 and developed a rash on December 21. He went to a township hospital (Hospital A) in DQ county where he received an intravenous infusion for an upper respiratory tract infection in an outpatient infusion room between December 19 and 24 – during his infectious period. He was not recognized as having measles until he was transported to a county-level hospital (Hospital B) on December 25. During the 7–21 days before his rash onset, he had an exposure history for a measles-like illness in Tibet.
Twelve cases had been exposure to measles at hospitals during their incubation periods. Eight had been exposed to the index case in Hospital A's transfusion room; 2 Hospital B heath care workers who had contact with confirmed cases developed measles; and 2 were infected during visits to the county hospital (Hospital B) as family members of hospitalized patients.
Although the outbreak started with adult-to-adult transmission in hospital A, young infants and children subsequently became infected. The index case led to three generations of measles transmission, infecting eight others.
Outbreak response immunization
ORI was started 4 days after the first measles case was reported, and involved non-selective (without regard to vaccination history) vaccination targeting 20–40 year-old adults living near a measles case. As the outbreak continued, ORI was intensified. From December 29 through January 13, ORI activities were conducted every day, as soon as a measles case was reported. During these 2 weeks, local public health workers, using media channels to urge adults 20 to 40 years of age to get vaccinated, managed to vaccinate a total of 10,598 adults. In total, 88% of adults from F township and 82% of adults from S township were vaccinated.
Serum samples from 100 individuals, 20–40 years of age were tested prior to the ORI. Eighty-four (84%) had serological evidence of immunity to measles (positive IgG), and the average GMT among this group was 374.64 mIU/ml. Approximately 1 month after the ORI, the average GMT increased to 1,452.87mIU/ml and the seropositive rate increased to 100%. The last case of the outbreak had rash onset in mid-January.
Discussion
We have described an outbreak of measles that occurred primarily among adults, that was started from an inter-province importation, and that was sustained by adult-to-adult transmission in semi-autonomous ethnic minority areas. Transmission was initially confined to adults, but measles virus was eventually transmitted to infants too young for routine measles vaccination. DQ County is known to have high MCV coverage among children 2–19 years of age through routine immunization and SIAs, and no cases occurred in this age group.
Measles transmission occurred in hospitals during the early stage of the outbreak, and health care workers who acquired measles were part of chains of transmission. Outbreak response immunization that targeted adults appeared to be necessary to stop transmission, and may have been effective at decreasing the magnitude and duration of the outbreak.
This outbreak illustrates a challenge with adult measles susceptibility in China. As the incidence of measles declines, population exposure to measles virus becomes increasingly rare, and as described by Ma and colleagues.3 Adult measles outbreaks are reported frequently6-11 and are becoming an emerging pattern of outbreaks in Yunnan and other parts of China. Recent serological survey-based evidence has shown protection levels among adults in DQ County to be 93.18% among individuals over 18 years old,12 which is lower than among DQ County children and lower than the herd immunity threshold for measles.
Our report is consistent with the literature on nosocomial measles transmission, as virus transmission among several of the adults occurred in hospital settings.13,14 Our study raises the possibility that the structures of medical facilities, susceptibility of hospital staff, and a lack of health care worker vaccination efforts may have to be contributed to measles transmission. This possibility is supported by three points. First, it is easy to transmit measles in medical facilities such as crowded infusion rooms with inadequate airflow.15 Airborne transmission is nearly inevitable if an infectious person is in such a room with susceptible individuals. Second, the index of suspicion of hospital staff to a diagnosis of measles was apparently low. The first case from Tibet had an illness consistent with measles, but the diagnosis was not made and the patient was not isolated. Third, a triage system was not enforced – outpatients with fever should have rooms separated from non-febrile patients. We noticed that patients with fever still went to the general infusion room.
To eliminate measles in China, adult susceptibility and nosocomial transmission may both have to be reduced. Recent measles outbreaks among adults in China are providing evidence for action. China's complicated and variable measles vaccination policies since the 1960s, coupled with the wide age range of adults that appear to have significant susceptibility to measles, make campaigns targeting adults difficult and inefficient: most adults are immune but cannot prove their vaccination status through records. Recent serologic surveys showed that seropositive levels among 20–30 year-old adults were the lowest among the all age groups, with exception of infants too young to vaccinate.16-18As Ma and colleagues stated, a realistic and possibly important vaccination strategy to target adults is outbreak response immunization (ORI). ORI is recommended in most outbreak settings in middle- and low-income countries.19 During the outbreak in DQ County, ORI did target adults, and without regard to vaccination status. Following ORI, the epidemic curve appears consistent with a positive impact of this ORI. The serology results supported our assertion that ORI had an impact, since 84% of adults were immune prior to vaccination, and all were immune following vaccination. This outbreak demonstrated that a rapid response, even with relatively high pre-response coverage, may be able to avert more cases.20
Our investigation supports the concept of a “diagonal” approach to measles elimination21 in which the visibility and high transmissibility of measles can help epidemiologists identify program areas to strengthen. Two program areas to strengthen are hospital infection prevention and control and adult susceptibility to measles. The diagonal approach shows another program area to strengthen. Because measles was imported from another province and spread through a semi-autonomous minority region, our province has a vulnerability that goes beyond our borders. It will therefore be important that the Tibetan immunization program receives technical and other resources for strengthening its program. Strengthening routine immunization and measles immunity in high-incidence provinces is going to be necessary as a longer-term response to lessons learned from this outbreak. Measles elimination provide an opportunity to institute a “diagonal” approach, in which it is possible to leverage resources available to strengthen immunization program.
We believe that our study supports three recommendations. First, public health officials should stay alert for adult-to-adult transmission of measles in outbreaks, and should consider early vaccination of adults in outbreaks, Second, hospital infection control programs should take action, including enhancing provider awareness of the clinical presentation of measles, ensuring that measles prevention is included in infection control guidelines, and offering measles and rubella vaccine to health care workers. Third, outbreaks should be analyzed to identify which provinces are spreading measles virus to other provinces to help strengthen the programs in the measles-virus-spreading provinces.
Methods
Setting
Located in D Tibetan Autonomous Prefecture, DQ County is in northwest Yunnan Province, sharing a 107.3-kilometer border with Tibet Autonomous Region. D Autonomous Prefecture is a designated ethnic minority region inhabited by Tibetans, who account for more than 36 percent of its present 406,000 population. In China, regional ethnic autonomous regions are geographic areas where various ethnic minorities live in compact communities that are legally recognized under the unified leadership of the central government and exercise certain rights of self-government. Three of the 8 townships in DQ County share a border with Tibet, and border inhabitants of each province interact frequently. In 2014, the DQ County population was 59,000, mostly Tibetan people.
Two rounds of SIAs had been conducted in DQ County: a catch-up SIA in November 2008 targeting children born between May 1994 and August 2008, and a follow-up SIA in September 2010 targeting children born between 2004 and 2010 – part of a nationwide campaign. Thus, in DQ County, all birth cohorts from 1994 through 2010 have been covered by at least 1 non-selective SIA. During 2010 and 2011, there no measles cases reported in DQ County; 6 cases were reported from 2012 through November 2015.
Three measles cases, all among adults, were reported on December 19, 2015, representing an incidence of 4.4 per 100,000 total population. The cases raised our concern about sources of infection and transmission routes, and prompted an evaluation of the effectiveness of outbreak response immunization. We conducted our field investigation from Dec 2015 to Jun 2016.
Outbreak investigation
In accordance with the Chinese Measles Surveillance Guidelines, measles is nationally notifiable to a case-based, laboratory-supported, Internet-based surveillance system, with reporting from local CDCs, hospitals, and other health agencies. County-level CDC staff are responsible for case investigation and collection and transportation of specimens. A suspected case of measles was defined by the following criteria: any person with fever (temperature, ≥37.5°C), generalized maculopapular rash, and one or more of the following symptoms: cough, coryza, or conjunctivitis – consistent with World Health Organization (WHO) criteria. We attempted laboratory confirmation for all suspected cases. Vaccination status of each case was determined using parent-held vaccination certificates. Self-reported receipt of vaccine without written documentation was classified as unknown vaccination status.
Based on China's National Measles Surveillance guidelines, an outbreak is defined as the occurrence of 2 or more measles cases in a group setting (community, school, company, buildings) within 10 days. During an outbreak, any measles case with an epidemiological link with reported cases would be identified as an outbreak case. An outbreak is declared over when no epidemiologically linked case occurs within 21 days from the onset of the last known measles case.
To facilitate determining sources of infection and transmission chains, we conducted a retrospective active case search for additional measles cases; identified suspected cases were reported through the measles surveillance system. We reviewed medical records from all township- and county-level hospitals in DQ County, and local staff conducted house-to-house active searches for measles cases in the affected townships and neighboring areas.
We conducted in-house interviews of all confirmed measles cases to collect detailed activity histories, including contact with other fever and rash illness patients, places they visited, and hospitals and clinics they visited from 21 days before their rash onset through 5 days after rash onset. This time frame was categorized as the “incubation period” (7–21 days prior to rash onset) and the “transmissibility period” (5 days before through 5 days after rash onset). A nosocomial measles case was defined as a confirmed case who had contact with another confirmed case in a hospital or health care facility during the 7–21 days prior to rash onset, in which a thorough investigation of contacts excludes other sources of infection. An imported measles case was defined as exposure to measles virus outside the DQ County during the 7–21 days prior rash onset in which a thorough investigation of contacts excludes a local source of infection. Family contact acquired infection was defined as one or more measles cases occurring during their transmissibility period within the same family during the 7–21 days prior to rash onset. Community acquired infection was defined as contact with measles cases in the same or neighboring villages, workplaces, or other locations outside of healthcare facilities or the home.
Laboratory testing
Cases were classified as laboratory-confirmed on the evidence of positive serology for measles immunoglobulin M (IgM), and/or presence of measles RNA, and/or positive measles virus isolation. Serological testing for measles IgM antibody was conducted by enzyme-linked immunosorbent assay (Zhuhai SEZ Haitai Biological Pharmaceuticals 346 Co., Ltd., Zhuhai, China) by the county CDC. Throat swabs and urine specimens were collected for detection of measles RNA by real time reverse-transcription polymerase chain reaction by the prefecture CDC. Specimens with positive results were sent to provincial measles/rubella laboratory for confirmatory test by RT-PCR and virus isolation in cell cultures (Vero/SLAM). Nucleic acid from positive viral cultures was extracted, amplified, and sequenced to determine measles virus genotype.
The measles/rubella laboratory networks in Yunnan province is evaluated by China CDC and has exceeded the WHO measles surveillance quality indicators requirements since 2013. Yunnan provincial measles/rubella laboratory is a WHO-accredited laboratory that attained a perfect score on WHO's proficiency testing (PT) program in 2014.
Effect of emergency immunization
We conducted a serological survey in December, 2015 and January, 2016 to assess measles immunity and the effect of outbreak response immunization (ORI). Serum samples were obtained from 100 DQ County residents between 20 and 40 years of age prior to the outbreak response immunization effort and an independent 100 residents 28 days after the immunization effort. Anti-measles antibody (IgG) was measured using commercially available ELISA kits (Virion Serion). Laboratory results were interpreted in accordance with the manufacturer's criteria. The positive cut-off value was 200 mIU/mL, and weakly-positive samples (150–200 mIU/mL) were considered equivocal. A value of <150 mIU/mL was considered negative.
Ethical considerations
Measles outbreak investigations are considered by Yunnan CDC's Ethical Review Committee to be exempt from IRB review as they are considered public health program evaluation. Informed consent was obtained prior to blood draws. Individual identifying data were not retained in analytic data sets.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.Ze WY, Diao LD, Xu AQ. Expanded program on immunization. 2nd ed. Shanghai: Shanghai Publishing House of Scientific and Technological Literature, 2001:359–82. [Google Scholar]
- 2.WHO Proceedings of the Global Technical Consultation to assess the feasibility of measles eradication, 28–30 July 2010. J Infect Dis. 2011;204(July (Suppl.1)):S4–13. [DOI] [PubMed] [Google Scholar]
- 3.Ma C, Yan SH, Su QR, Hao L, Tang S, An Z, He Y, Fan G, Rodewald L, Wang H. Measles transmission among adults with spread to children during an outbreak: Implications for measles elimination in China, 2014. Vaccine. 2016;34(June):6539–6544. doi: 10.1016/j.vaccine.2016.02.051. [DOI] [PubMed] [Google Scholar]
- 4.Ma C, Su QR, Hao LX, Wen N, Fan CX, Cao L, Li L. Measles epidemiology characteristics and progress toward measles elimination in China, 2012–2013. Chin J Vaccine Immun. 2014;20(3):193–199. [Google Scholar]
- 5.Ma C, Hao LX, Su QR, Ma J, Zhang Y, Cao L, Luo HM. Measles epidemiology and progress towards measles elimination in China, 2011. Chin J Vaccine Immun. 2012;18(3):193–9. [Google Scholar]
- 6.Ma C, Hao LX, Su QR, Wen N, Fang CX, Yang H, Li L, Wang HQ. Measles Epidemiology in China, 2014. Disease Surveillance. 2015;30(10):818–823. [Google Scholar]
- 7.Shi Y, Zhang JF, Hu JY, Tao LN. Analysis on measles epidemiological characteristics in Shanghai from 1999–2004. Chin J Vaccine Immun. 2006;12(1):32–34. [Google Scholar]
- 8.Liu YB, Lu PS, Zhou CN, et al.. Immunity to measles virus in population aged ≥15 years in Jiangsu province. Chin J Public Health. 2013;29(12):1842–1844. [Google Scholar]
- 9.Xu Q, Xu AQ Song LZ, Wang CY, Zhang XM, Cao GQ, Zhang L, Xiao ZK, Wang M. Epidemiological analysis on measles outbreak among adults. Chin J Vaccine Immun. 2007;13(5):440–443. [Google Scholar]
- 10.Ch Li, GX Yin, Gu SY, et al.. Investigation of a measles in adults in Xi Ujimq in banner of Xilin Gol League, Inner Mongolia. Disease Surveillance. 2015;30(2):160–161. [Google Scholar]
- 11.Ge S, Wang S, Han BH, Liu F, Zhang Z, Ma R, Lu L. Investigation of an outbreak of measles in adults in Beijing, 2014. Disease Surveillance. 2016;31(3):260–262. [Google Scholar]
- 12.Sang M, Hu XT. Immunity to measles virus in population in Deqing County, 2013. Soft Science of Health. 2014;28(1):43–50. [Google Scholar]
- 13.Chen SY, Anderson S, Kutty PK, Lugo F, McDonald M, Rota PA, Ortega-Sanchez IR, Komatsu K, Armstrong GL, Sunenshine R, Seward JF. Health care-associated measles outbreak in the United States after an importation: challenges and economic impact. J Infect Dis. 2011;203(11):1517–1525. doi: 10.1093/infdis/jir115. PMID:21531693. [DOI] [PubMed] [Google Scholar]
- 14.Chen EF, He HQ, Li Q, Ma R, Wang FY, Qiu CH, Zhao YR, Fu J.. Case-control study on epidemiology factors of measles in Zhejiang Province in 2008. Chin J Vaccine Immun. 2010;16(1):11–14. [PubMed] [Google Scholar]
- 15.Zhang DL. A hospital-associated measles outbreak among individuals not targeted for vaccination in eastern China, Vaccine. 2015;33 (June) 4100–4104. doi: 10.1016/j.vaccine.2015.06.066. PMID:26117147. [DOI] [PubMed] [Google Scholar]
- 16.Xiong Y, Wang D, Lin W, Tang H, Chen S, Ni J. Age-related changes in serological susceptibility patterns to measles: results from a seroepidemiological study in Dongguan, China. Human Vaccines & Immunotherapeutics, 2014;10(4):1097. doi: 10.4161/hv.27734. PMID:24448194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ding YX, Sun J, Tian H. Analysis for Measles Antibody and Susceptibility in Tianjin Municipality. Chin J Vaccine Immun. 2013;19(4):301–303. [Google Scholar]
- 18.Li J, Lu L, Chen M, Huang F, Zeng Y, Li XM, Ma R, Pan JB, Sun M, Sun H, et al.. Analysis of measles immunity level in persistent populations in Beijing, 2012. China J Prev Med. 2013;47(10):916–919. [PubMed] [Google Scholar]
- 19.Cairns KL, Perry RT, Ryman TK, Nandy RK, Grais RF. Should outbreak response immunization be recommended for measles outbreaks in middle- and low-income countries? An update. J Infect Dis 2011;204(July (1 Suppl.)):S35–46. doi: 10.1093/infdis/jir072. PMID:21666184. [DOI] [PubMed] [Google Scholar]
- 20.WHO Measles elimination field guide; 2013. Available from: http://www.wpro.who.int/immunization/documents/measles_elimination_field_guide_2013/en/.
- 21.Orenstein WA, Seib K. Beyond vertical and horizontal programs: a diagonal approach to building national immunization programs through measles elimination. Expert Rev Vaccines. 2016;15(7):791–793. doi: 10.1586/14760584.2016.1165614. PMID:26967373. [DOI] [PubMed] [Google Scholar]