ABSTRACT
V920, rVSVΔG-ZEBOV-GP, is a recombinant vesicular stomatitis-Zaire ebolavirus vaccine which has shown an acceptable safety profile and provides a protective immune response against Ebola virus disease (EVD) induced by Zaire ebolavirus in humans. The purpose of this study was to determine whether the V920 vaccine is capable of replicating in arthropod cell cultures of relevant vector species and of replicating in live mosquitoes. While the V920 vaccine replicated well in Vero cells, no replication was observed in Anopheles or Aedes mosquito, Culicoides biting midge, or Lutzomyia sand fly cells, nor in live Culex or Aedes mosquitoes following exposure through intrathoracic inoculation or feeding on a high-titer infectious blood meal. The insect taxa selected for use in this study represent actual and potential epidemic vectors of VSV. V920 vaccine inoculated into Cx. quinquefasciatus and Ae. aegypti mosquitoes demonstrated persistence of replication-competent virus following inoculation, consistent with the recognized biological stability of the vaccine, but no evidence for active virus replication in live mosquitoes was observed. Following administration of an infectious blood meal to Ae. aegypti and Cx. quinquefasciatus mosquitoes at a titer several log10 PFU more concentrated than would be observed in vaccinated individuals, no infection or dissemination of V920 was observed in either mosquito species. In vitro and in vivo data gathered during this study support minimal risk of the vector-borne potential of the V920 vaccine.
KEYWORDS: Arbovirus, Ebola virus, live-attenuated vaccine, vector competence, vesicular stomatitis virus
Introduction
The genus Ebolavirus of the family Filoviridae (Order: Mononegavirales) is comprised of five recognized species, with Zaire ebolavirus (ZEBOV) representing the prototype species. ZEBOV is a significant human pathogen with case fatality rates often reaching 90%. To date there have been numerous outbreaks of ZEBOV,1 the largest of which occurred in West Africa in 2014 and resulted in >28,000 human cases and >11,000 deaths.2,3 The high case fatality rate and magnitude of the 2014 outbreak in West Africa illustrates the pressing need for the development of a safe and efficacious vaccine to prevent future ZEBOV outbreaks.
ZEBOV particles are filamentous and enveloped.4 The ZEBOV genome consists of a non-segmented, negative-sense, single-stranded RNA molecule which is approximately 19kb and encodes eight proteins: nucleoprotein (NP), virion protein (VP) 35, VP40, glycoprotein (GP), secreted glycoprotein (sGP), VP30, VP24, and an RNA-dependent RNA polymerase (L).5,6 Notably, GP mediates attachment and fusion of the virion to affected cells.5,7 Previous studies have shown immunization against GP to be an effective means of eliciting a protective immune response against a lethal ZEBOV challenge due to GP containing important neutralization or other functional epitopes.8,9
Vesicular stomatitis virus (VSV) (Order: Mononegavirales; Family: Rhabdoviridae; Genus: Vesiculovirus) is an enveloped virus containing a non-segmented, single-stranded, negative-sense RNA genome. This approximately 11kb genome encodes five viral proteins: the nucleoprotein (N), phosphoprotein (P), matrix (M), glycoprotein (G), and the large protein (L).10 The epidemiology and ecology of naturally-circulating vesiculoviruses remains poorly understood, but VS viruses and/or serological evidence of exposure to VSV have been found in a diversity of domestic and wild vertebrate species.10-12 The two serotypes of VSV, VSV-Indiana and VSV-New Jersey are both transmitted to mammals by hematophagous insects as well as through direct contact via the transcutaneous or transmucosal route.10,12 Transmission competent insect vectors of VSV include biting midges (Culicoides spp.) phlebotomine sand flies (Lutzomyia and Phlebotomus spp.), black flies (Simulium spp.), and mosquitoes.13-19 Clinical illness in cattle, horses, and pigs as a result of VSV infection includes vesiculation, ulceration, and erosion of the oral and nasal mucosa and epithelial surface of the tongue, coronary bands, and teats.11,12 The prevalence of clinical cases in cattle herds is generally low (10%-20%), but seroprevalence within the herd may approach 100%.11
VSV has proven to be a successful vector in the development of several live-attenuated vaccine candidates due to its ability to accept and stably express foreign gene products from heterologous viruses.20-26 To develop a safe and efficacious single-dose vaccine against ZEBOV, the G gene of VSV was replaced with the immunogenic glycoprotein (GP) gene of ZEBOV, resulting in VSV virion particles expressing ZEBOV GP as the surface antigen.27-30 The resulting rVSVΔG-ZEBOV-GP construct, also referred to as V920, is a replication competent, live-attenuated vaccine that has attenuated replication and a narrower host-cell tropism in vitro than wild-type VSV.27 The resulting rVSVΔG-ZEBOV-GP construct has been tested in several animal models, including mice and non-human primates (NHPs), and has been shown to be safe and to elicit a robust, protective immune response.29,31-34 This vaccine has been tested in several clinical trials and has been shown to have an acceptable safety profile, to be immunogenic, and to be highly effective in preventing ebola virus disease (EVD) induced by ZEBOV in humans.35-38 A viremia is detectable, generally in the first few days after vaccination, but at low levels, as will be discussed below.39
However, due to the vector-borne potential of wild-type VSV, certain environmental concerns must be addressed. Development of live attenuated vaccines using an arbovirus as a vaccine vector introduces the risk that an immunized person might develop a viremia high enough for a susceptible insect to become infected with and potentially transmit the vaccine. This phenomenon was documented with the Venezuelan equine encephalitis virus vaccine TC-83, when TC-83 was isolated from mosquitoes in Louisiana following its use in horses to stop the 1969–72 epidemic in Texas.40 In the case of V920, while the backbone is an arbovirus, prior experimental evidence demonstrated that Ebola Reston virus was incapable of replication in arthropods.41 Therefore, we hypothesized that the V920 rVSVΔG-ZEBOV-GP vaccine would not replicate in arthropod cells or live mosquitoes. Furthermore, in addition to our inclusion of a wild-type VSV-Indiana strain (VSV-I) control throughout the study, we included another VSV construct with the G gene of VSV replaced with the structural cassette, sans capsid, of Semliki Forest virus (SFV), termed rVSV-SFV, as a control. The rationale for including rVSV-SFV, which we hypothesized would replicate in arthropods due to the natural transmission of SFV by mosquitoes, was to demonstrate that the inability of V920 to replicate in arthropod (in vitro and in vivo) was due to the replacement of the arbovirus envelope cassette with the ZEBOV GP gene. An experiment was conducted to determine whether V920 replicated in arthropod cells. We evaluated the replication kinetics of all three viruses in several relevant insect vector cell lines derived from mosquitoes (Genera: Aedes and Anopheles), biting midges (Genus: Culicoides), and sand flies (Genus: Lutzomyia). We also assessed the replication potential of V920 in live Aedes and Culex mosquitoes exposed via an infectious blood meal and intrathoracic (IT) inoculation. Through this study, we confirmed the inability of V920 to replicate in arthropods in vitro and in vivo, interestingly we also found that rVSV-SFV was also unable to replicate in arthropods in vitro and in vivo.
Results
Growth curves in cell cultures
Virus replication was assessed in multiple arthropod cell lines (Figure 1), representing taxa that serve as actual or potential vectors of VSV in the field. All growth curves were conducted in triplicate at a multiplicity of infection (MOI) of 0.01. Back titrations were conducted for each inoculum and confirmed to be within two-fold of the desired inoculum titer. Each virus replicated to a high titer in Vero cells and caused significant cytopathic effect (CPE), confirming the utility of this cell line for virus quantification purposes (Figure 1A). In Anopheline (4a3b), Aedes (C6/36), biting midge (CuVa), and sand fly (LL-5) cell lines replication was observed for VSV-I but not for either V920 or rVSV-SFV (Figure 1B-E). For each cell line, virus titers of VSV-I were significantly higher (p-value < 0.05) than V920 and rVSV-SFV as determined by a two-way ANOVA with a Tukey's correction at each timepoint (Figure 1).
Figure 1.
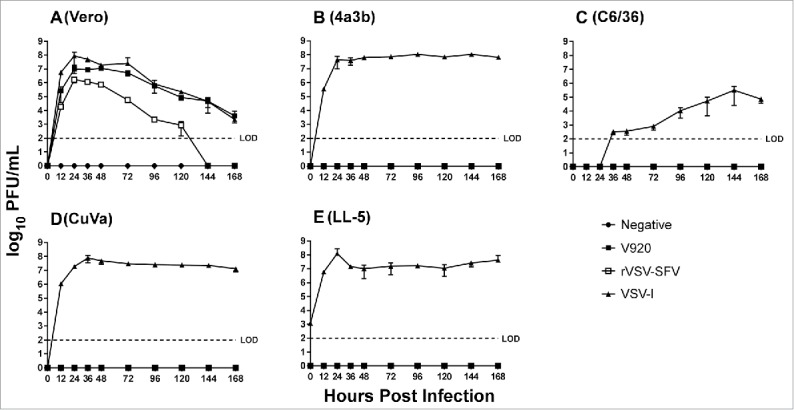
Comparison of growth kinetics of VSV-I, V920, and rVSV-SFV in A) Vero, B) 4a3b, C) C6/36, D) CuVa, and E) LL-5 cells when infected at MOI 0.01. Means and SEs from three independent replicates are shown. LOD = limit of detection (100 PFU/mL). Statistics were performed using a two-way ANOVA with Tukey's correction at each timepoint. P-values: Vero) 0.0211 (VSV-I v. V920) and 0.0073 (VSV-I v. rVSV-SFV); 4a3b) <0.0001 and <0.0001; C6/36) 0.0002 and 0.0002; CuVa) <0.0001 and <0.0001; LL-5) 0.0478 and 0.0478.
Intrathoracic inoculations
To assess the ability of V920 to replicate in mosquitoes Culex quinquefasciatus (Cx. quinquefasciatus) and Aedes aegypti (Ae. aegypti) were inoculated with VSV-I, V920, or rVSV-SFV. The stock titer for both VSV-I and V920 was 8.3 log10 PFU/mL; rVSV-SFV had a stock titer of 6.6 log10 PFU/mL. Mosquitoes were inoculated with 138 nl stock virus (approximately 4.4 log10 PFU for VSV-I and V920 and 2.7 log10 PFU for rVSV-SFV). Due to the very small volumes of virus inoculated, many of these doses fell below the limit of detection (LOD) of the assay and virus replication was not apparent until later timepoints (Table 1). Following inoculation 3–5 mosquitoes were harvested on days 0, 1, 2, 4, 8, 10, 14 and infectious virus was quantified by plaque assay on Vero cells.
Table 1.
Virus Titers (log10 PFU/mosquito) in Individual Mosquitoes Following Intrathoracic Inoculation.
| VSV-I |
V920 |
VSV-SFV |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PFU/mosquito (log10) |
PFU/mosquito (log10) |
PFU/mosquito (log10) |
||||||||||||||||
| Day Post Infection | Number of Positive Mosquitoes | A† | B | C | D | E | Number of Positive Mosquitoes | A | B | C | D | E | Number of Positive Mosquitoes | A | B | C | D | E |
| Culex quinquefasciatus titers post-IT inoculation | ||||||||||||||||||
| 0 | 4/5 | 2.2 | 1.7 | 2.3 | 0 | 2 | 4/5 | 2 | 2 | 2 | 2.2 | 0 | 0/3 | 0 | 0 | 0 | ||
| 1 | 2/5 | 0 | 0 | 3.9 | 4.1 | 0 | 4/4 | 1.4 | 1.4 | 2.4 | 1.7 | 0/3 | 0 | 0 | 0 | |||
| 2 | 4/4 | 4.4 | 4.4 | 4.3 | 5.1 | 0/4 | 0 | 0 | 0 | 0 | 0/3 | 0 | 0 | 0 | ||||
| 4 | 3/3 | 4.7 | 4.5 | 4.1 | 0/3 | 0 | 0 | 0 | 0/3 | 0 | 0 | 0 | ||||||
| 8 | 3/3 | 5.4 | 4.9 | 4.7 | 1/3 | 0 | 0 | 2.5 | 0/3 | 0 | 0 | 0 | ||||||
| 10 | 4/4 | 4.5 | 5.2 | 4.3 | 5.3 | 0/3 | 0 | 0 | 0 | 0/3 | 0 | 0 | 0 | |||||
| 12 | 3/3 | 3.9 | 4.4 | 3.7 | 0/3 | 0 | 0 | 0 | 0/3 | 0 | 0 | 0 | ||||||
| 14 | 4/4 | 3.8 | 3.7 | 3.5 | 3.8 | 0/4 | 0 | 0 | 0 | 0 | 0/3 | 0 | 0 | 0 | ||||
| Aedes aegypti titers post-IT inoculation. | ||||||||||||||||||
| 0 | 2/5 | 2.4 | 0 | 0 | 0 | 2.4 | 0/5 | 0 | 0 | 0 | 0 | 0 | 0/3 | 0 | 0 | 0 | ||
| 1 | 3/3 | 2.7 | 4.3 | 4.3 | 0/3 | 0 | 0 | 0 | 0/3 | 0 | 0 | 0 | ||||||
| 2 | 3/3 | 4.4 | 4.6 | 5.1 | 0/3 | 0 | 0 | 0 | 0/3 | 0 | 0 | 0 | ||||||
| 4 | 3/3 | 3.4 | 4.4 | 4.5 | 0/3 | 0 | 0 | 0 | 0/3 | 0 | 0 | 0 | ||||||
| 8 | 3/3 | 5.3 | 3.8 | 4.1 | 1/3 | 2.2 | 0 | 0 | 1/3 | 0 | 1.4 | 0 | ||||||
| 10 | 3/3 | 3.7 | 3.8 | 3.7 | 1/3 | 0 | 0 | 2.2 | 1/3 | 1.6 | 0 | 0 | ||||||
| 12 | 3/3 | 3.5 | 3.4 | 4.3 | 1/3 | 2.1 | 0 | 0 | 1/3 | 0 | 1.7 | 0 | ||||||
| 14 | 2/2 | 3.4 | 3.4 | 0/5 | 0 | 0 | 0 | 0 | 0 | 1/3 | 1.1 | 0 | 0 | |||||
Three-to-five mosquitoes were harvested at each timepoint, represented by specimens A-E.
Zeros indicate below LOD and not necessarily negative.
Overall, VSV-I replicated in both mosquito species, reaching peak titers of approximately 5 log10 PFU per mosquito between two and eight days post inoculation (dpi). Following inoculations of Cx. quinquefasciatus mosquitoes, V920 was recovered from one of three mosquitoes on eight days post inoculation. Furthermore, V920 was recovered from one of three Ae. aegypti mosquitoes on each days 8, 10, and 12 post inoculation. Additionally, rVSV-SFV was recovered from one of three mosquitoes on 8, 10, 12, and 14 dpi in Ae. aegypti mosquitoes; rVSV-SFV was not recovered from Cx. quinquefasciatus on any days post inoculation. Because the V920 and rVSV-SFV detections found in these few individual mosquitoes (33%) at these late timepoints and did not exceed the dose inoculated, these results are believed to represent detections of vaccine persisting in the mosquito following inoculation rather than the result of actively replicating virus. By comparison, VSV-I was found in 100% of inoculated mosquitoes after day 2 post inoculation and replicated to mean titers of approximately 3 log10 PFU, approximately 2–3 log10 higher than the inoculum dose by 1–2 days post-inoculation. The virus titers detected in mosquitoes were significantly different as measured by a Kruskal-Wallis test with a Dunn's multiple comparisons post-test. For Cx. quinquefasciatus mosquitoes, VSV-I was significantly different (p-value <0.05) from both V920 and rVSV-SFV, with p-values of 0.0036 and <0.0001, respectively. VSV-I was also significantly different in Ae. aegypti mosquitoes as compared to V920 and rVSV-SFV (p-values 0.0019 and 0.0011, respectively).
Oral infectivity
To determine if V920 was capable of infecting and disseminating from the mosquito midgut following oral exposure, and to further assess the presence of very low levels of V920 and rVSV-SFV persisting in IT inoculated mosquitoes, both Cx. quinquefasciatus and Ae. aegypti mosquitoes were exposed to infectious blood meals containing either VSV-I, V920, or rVSV-SFV. At 14 days post exposure bodies (a measure of midgut infection) and legs and wings (a measure of dissemination) were collected and assessed for presence of infectious virus. Blood meal titers were confirmed by back-titration. For Cx. quinquefasciatus mosquitoes, back-titers were: 7.8 log10 PFU/mL for VSV-I, 8.0 log10 PFU/mL for V920, and 6.4 log10 PFU/mL for rVSV-SFV. For Ae. aegypti mosquitoes back-titers were: 7.7 log10 PFU/mL for VSV-I, 8.1 log10 PFU/mL for V920, and 6.3 log10 PFU/mL for rVSV-SFV.
At 14 days post exposure, 2 of 48 Cx. quinquefasciatus mosquitoes became infected with VSV-I (Table 2). Both mosquitoes developed a disseminated infection. These data indicate the presence of a significant midgut infection barrier in Cx. quinquefasciatus when exposed to VSV-I. For Ae. aegypti, 10 of 48 mosquitoes became infected with VSV-I and 9 of those developed a disseminated infection (Table 3). These data demonstrate that while Ae. aegypti mosquitoes were more susceptible to infection with VSV-I than Cx. quinquefasciatus, a moderate midgut infection barrier is still present in this species. No Ae. aegypti or Cx. quinquefasciatus mosquitoes became infected with either V920 or rVSV-SFV. Titers of recovered virus in each mosquito are recorded in Tables S1-2.
Table 2.
Virus Positive Culex quinquefasciatus on Day 14 Post Blood Feed.
| VSV-I† | VSV-SFV | V920 | |
|---|---|---|---|
| Bodies (IS) | 2/48 | 0/48 | 0/48 |
| Legs & Wings (DI) | 2/48 | 0/48 | 0/48 |
IS = Infection Status
DI = Disseminated Infection
Mosquitoes that were positive for DI were also had a positive IS
Table 3.
Virus Positive Aedes aegypti on Day 14 Post Blood Feed.
| VSV-I† | VSV-SFV | V920 | |
|---|---|---|---|
| Bodies (IS) | 10/48 | 0/48 | 0/48 |
| Legs & Wings (DI) | 9/48 | 0/48 | 0/48 |
IS = Infection Status
DI = Disseminated Infection
Mosquitoes that were positive for DI were also had a positive IS
Virus stability in mosquito suspension
A virus stability experiment was conducted using mosquito homogenates spiked with virus and incubated at 28°C for 14 days to follow-up on the detection of V920 and rVSV-SFV in live mosquitoes at later experimental time points (8–12 days) following IT inoculation (Table 1). Since the titer of the virus detected in these mosquitoes did not exceed the titer of the original inoculum, we hypothesized that the virus detected was due to the persistence of stable, replication-competent virus from the original inoculum rather than the result of active replication in mosquito tissues. This experiment revealed that the titer of all viruses declined over time, but replication-competent virus particles were present in mosquito homogenate out to 7 days in Cx. quinquefasciatus and 14 days in Ae. aegypti (Figure 2). A two-way ANOVA was conducted with a Tukey's multiple comparisons test to compare the mean titer of each virus group. In comparing virus stability between VSV-I and V920, virus titers were significantly different in both Aedes and Culex mosquito suspensions. A similar pattern was observed in comparing virus stability between VSV-I and rVSV-SFV. These results are consistent with the results of the IT inoculations, and further support our hypothesis that, while low levels of thermostable virus may persist, it is highly unlikely that V920 replicates in mosquitoes following IT inoculation.
Figure 2.
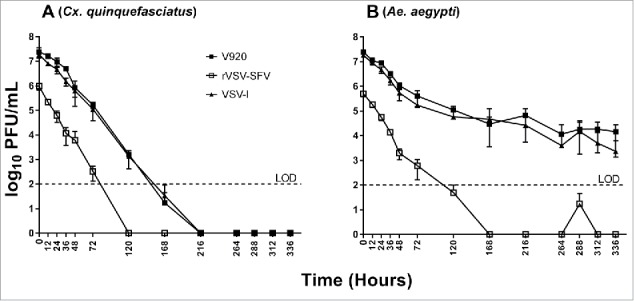
Stability of VSV-I, V920, and rVSV-SFV in A) Culex quinquefasciatus and B) Ae. aegypti mosquito homogenate. Means and SEs from three independent replicates are shown. LOD = limit of detection (100 PFU/mL). Statistics were performed using a two-way ANOVA with Tukey's correction at each timepoint. P-values: Cx. quinquefasciatus) 0.0101 (VSV-I v. V920) and 0.0016 (VSV-I v. rVSV-SFV); Ae. aegypti) 0.0200 and 0.0004.
Discussion
This study demonstrated that the V920 Ebola virus vaccine, rVSVΔG-ZEBOV-GP, does not replicate in any of the arthropod cell lines examined nor in live Culex or Aedes mosquitoes following intrathoracic inoculation (IT) or oral exposure. Wild-type VSV-I is recognized for its potential to be transmitted by diverse taxa of arthropod vectors including mosquitoes, sand flies, and biting midges.13,14,17,19,42 Further, active replication of VSV-I in IT-inoculated Ae. aegypti mosquitoes has been previously demonstrated.43,44 Hence, the cell lines and mosquito genera used in this study were selected based on previous field isolations of VSV13,14 or demonstrated laboratory competence17,19,42-44 of these insect groups for replication or transmission of VSV. As expected, VSV-I replicated in all cell lines examined as well as both genera of mosquitoes, demonstrating the relevance of the arthropod groups included in this study and the importance of evaluating the replication potential of the V920 vaccine in diverse insect taxa.
As expected, substitution of the glycoprotein of a non-vector-borne virus (ZEBOV) ablated the ability of VSV to infect and replicate in various arthropod cell lines as well as in live mosquitoes. All three viruses were replication-competent in Vero cells. However, only VSV-I grew in C6/36 (Ae. albopictus), 4a3b (An. gambiae), CuVa (C. sonorensis), and LL-5 (L. longipalpis) cells or live Culex or Aedes mosquitoes. Overall, these results support the work of Turell et al. (1996) who found no replication of Ebola Reston virus when this virus was inoculated into mosquitoes or ticks.41 While we expected that V920 would not replicate in arthropod cells, the inability of rVSV-SFV to replicate in arthropod cells was unexpected. The purpose of including rVSV-SFV was to show that if the glycoprotein of VSV were replaced with that of another arbovirus (in this case SFV) the resulting recombinant VSV would be capable of replicating in arthropod cells. While the results confirm our main hypothesis, that V920 is incapable of replicating in arthropod cells, the results obtained with rVSV-SFV demonstrate the need for more research into the mechanism for determination of host range in VSV chimeric viruses. Indeed, this system could lead to many insights regarding the infection of arthropod cells. The rVSV-SFV construct has the VSV G gene replaced with the full structural cassette of SFV, sans capsid. Given the ability rVSV-SFV to replicate in cells derived from a vertebrate host and not of those derived from arthropods, this construct could be used to determine key mediators of host range infection and of alphaviruses and arboviruses in general. The specific step of viral replication that is preventing the formation of progeny virions in arthropod cells exposed to rVSV-SFV is currently unknown. However, the most likely block is occurring at the point of attachment and entry for the virus. The mechanism associated with virus attachment and entry in arthropods has long remained cryptic for alphaviruses and other arboviruses.45 This tool could lead to important insights regarding the mechanisms intrinsic to both virus and arthropod that allow an infection to progress.
Our experiments revealed that the replication kinetics of VSV-I in C6/36 cells was atypical compared to that in the other arthropod cell lines (Figure 1C). Given a differential susceptibility of mosquito cell types to infection with VSV, the cells comprising the C6/36 cell line, derived from larval Ae. albopictus, are perhaps not as permissive to infection with VSV as compared with the cell types available to these viruses infecting live mosquitoes. Bergold et al. (1968) studied the tissue tropism of VSV-I and VSV-New Jersey strains in Ae. aegypti following intrathoracic inoculation and demonstrated that while VSV infected a diversity of mosquito tissues over the course of infection, virus concentrations per microgram of tissue were highest in the thoracic and abdominal ganglia at 8 days post inoculation, and the salivary glands at 20 days post inoculation.44 The C6/36 clone, derived from the original SAAR Ae. albopictus cell line, was selected for its increased permissiveness to replication of dengue and chikungunya viruses.46 However, this selection may have favored replication of some viruses but not others. The specific reason why the C6/36 cell line did not support replication of VSV-I to the same extent as the other arthropod cell lines, despite replication of this virus in a closely-related live mosquito vector species, deserves further study.
The V920 vaccine inoculated into Cx quinquefasciatus and Ae. aegypti mosquitoes demonstrated the presence of replication-competent virus in a small proportion of intrathoracically-inoculated mosquitoes at low titer following inoculation (Table 1). The results from follow-up experiments investigating virus stability in a homogenized mosquito matrix are consistent with the data from the IT-inoculations, and support the hypothesis that the low-level persistence of V920 in a few mosquitoes is due to the biological stability of the virus rather than active replication (Figure 2). Persistent, replication-competent virus particles for both VSV-I and V920 were present in the homogenized mosquito matrix for 7 days in Cx. quinquefasciatus homogenate, and for 14 days in Ae. aegypti homogenate (Figure 2). Additionally, rVSV-SFV was detected intermittently out to 12 days in Ae. aegypti. These results are consistent with the results of the intrathoracic inoculations, whereby persistent V920 was detected in inoculated Cx. quinquefasciatus 8 days post-inoculation, and in Ae. aegypti 12 days post inoculation (Table 1). Why virus persistence in Ae. aegypti was longer than in Cx. quinquefasciatus for both the biological stability test and the intrathoracic inoculations is unclear. While mosquito homogenate is a very different environment for a virus as compared to live mosquito tissues, these data provide evidence that replication-competent virus particles of the V920 vaccine are able to persist in a disrupted environment for one to two weeks (Figure 2). Therefore, the V920 vaccine detected in mosquitoes following IT inoculations most likely represented residual inoculum and was not the result of active replication in mosquito tissues. This conclusion is also supported by the failure of V920 to replicate in vitro in mosquito cells. Development of a positive strand-specific RT-PCR would be one approach to specifically test for the presence of actively-replicating virus in these samples from IT-inoculated mosquitoes.47
Importantly, we demonstrated that V920 failed to infect mosquitoes following oral exposure through an infected to a blood meal containing a high concentration of virus. This experiment evaluated the only way that mosquitoes could become infected with V920 under natural conditions – by blood-feeding on vaccinated humans. Wild-type VSV-I was shown to infect both Ae. aegypti and Cx. quinquefasciatus mosquitoes, although a midgut infection barrier was present in both species (Tables 2 & 3). These results are consistent with a study that found moderate levels of virus dissemination in Ae. aegypti mosquitoes fed on viremic mice infected with VSV-I.48 Infectious blood meal titers during these experiments were maximized to ensure that the probability of mosquitoes becoming infected was as high as possible. In the case of V920, mosquitoes exposed to >8 log10 PFU/mL of virus did not become infected. Importantly, humans vaccinated with V920 develop only transient viremias peaking at approximately 3 log10 PFU/mL.35 The probability of mosquitoes becoming infected after feeding on an infectious blood meal significantly declines below titers of 5 log10 PFU/mL due to the small size of the mosquito blood meal and the likelihood of imbibing a virus particle at low circulating concentrations.49 Therefore, our data and the quantitative viremia data from clinical studies indicate an extremely low probability of mosquitoes becoming infected from feeding on a vaccinated individual. Considering that the V920 vaccine lacks the surface glycoprotein of an arbovirus, did not replicate in mosquito, biting midge, or sand fly cells, and did not infect relevant mosquito vector species, our results support an extremely low risk of arthropod-borne transmission of this vaccine.
Methods
Cell lines
Vero (African green monkey kidney) cells (ATCC CCL-81) were maintained in Dulbecco's minimal essential media (DMEM) supplemented with 5% fetal bovine serum (FBS) 1% nonessential amino acids, 1% sodium pyruvate, 1% penicillin/streptomycin (P/S), 0.1% gentamycin, 0.1% amphotericin B. Cells were stored in a humidified incubator at 37°C in 5% CO2. C6/36 (Aedes albopictus) cells (ATCC CRL-1660) were maintained in DMEM supplemented with 5% FBS and 1% P/S. 4a3b (Anopheles gambia) cells50 were maintained in Schneider's media supplemented with 10% FBS and 1% P/S. LL-5 (sand fly; Lutzomyia longipalpis) cells51 were maintained in Schneider's media supplemented with 20% FBS and 1% P/S. Media for CuVa (biting midge; Culicoides sonorensis, formerly C. varipennis) cells52 was formulated by adding 24.5 g powdered Schneider's media (Sigma-Aldrich; St. Louis, MO) to 800mL water. While being stirred continuously the following was added to the media: 0.4 g sodium bicarbonate, 58.5 mg L-glutamine, 6.0 mg reduced glutathione, 30.0 mg L-asparagine, 0.18mg bovine insulin @ 25 U/mg. The pH was then brought to 9.2 via the addition of ∼2.1 g NaOH pellets and stirred for 10 minutes. After stirring, pH was then brought down to 6.7 via the addition of ∼4 mL 12.1N HCl. 0.6 g CaCl was dissolved in 50 mL water and added to media via transfer pipette to prevent formation of precipitates. Water was then added to bring total volume to 1 L and media was filtered through a 0.22 µm filter prior to the supplementation of 15% FBS. All arthropod cells were stored in a humidified incubator at 28°C in 5% CO2. The passage ranges of the cell cultures used during these experiments were as follows: Vero (passages 8–96), C6/36 (6–12), CuVa (17–36), LL-5 (94–100), 4a3b (91–121). All cell cultures tested negative for mycoplasma.
Mosquitoes
Mosquito species used the study were Ae. aegypti strain Poza Rica and Cx. quinquefasciatus. The Poza Rica strain of Ae. aegypti (year established 2012) was originally sourced from field-collected material from Poza Rica, Mexico; approximately generation F15. The Cx. quinquefasciatus colony was originally collected in Sebring county Florida in 1988 and is continuously maintained at AIDL. Mosquitoes were reared under ACL2 conditions in the Infectious Disease Research Center (IDRC) Discovery Suite on the CSU foothills campus at 26–27°C with a 16:8 light: dark cycle and 70%-80% relative humidity. Approximately 5–7 days after emergence, adult female mosquitoes were transported to the IDRC Phase III virology (BSL3) suite for experimental infection.
Virus
V920 rVSVΔG-ZEBOV-GP vaccine lot number 003 12 14 (clinical trial material made in accordance with Good Manufacturing Practices) was used in this study. A fresh vial of virus was thawed for every experiment. Prior to experimentation, the virus titer of the lot was confirmed as 8.3 log10 PFU/ml by titrating one vial of the V920 by Vero cell plaque assay in triplicate as previously described.53
rVSV-SFV was provided by Sean Whelan of Harvard University. rVSV-SFV is a VSV-I virus with the G protein replaced with the structural cassette of SFV sans capsid. Additional stocks were generated on Vero cells via infection at a MOI of 0.01. Infectious media was harvested 48 hours post infection (hpi), clarified via centrifugation at 4800xg for 30 minutes, FBS concentration brought to 20%, and stored at -80°C. Virus titer was determined via Vero cell plaque assay prior to experimentation as previously described.53
Wild-type VSV-I, strain 98–3514, isolated from a horse during the 1998 outbreak in Colorado, was obtained internally at Colorado State University (CSU) for use as a positive control in this study. No further information was available regarding the passage history of this virus or the case history of the animal from which it was isolated. The virus was verified as Indiana strain by the CSU Veterinary Diagnostic Laboratory by quantitative reverse transcriptase polymerase chain reaction (qRT-PCR) (Ct = 14.96). Additional stocks were generated as described above and virus titer determined via Vero cell plaque assay prior to experimentation as previously described.53
Growth curves
Growth kinetics of all viruses were assessed in cell culture. Flasks (25 cm2) of Vero, 4a3b, C6/36, LL-5, and CuVa cells were inoculated in triplicate for each virus and a mock infected control at a MOI of 0.01. An additional mock flask for each cell line was used to count cells prior to inoculation for accurate MOI calculations. Inoculum was allowed to adsorb for one hour at the appropriate temperature (37°C for Vero cells, and 28°C for insect cells). Following incubation virus inoculum was removed. Vero cells were washed 3 times with 1x phosphate buffered saline (PBS) and insect cells were washed 3 times with the appropriate cell culture media, and maintenance media added. At 0, 12, 24, 36, 48, 72, 96, 120, 144, and 168 hours post-infection, 500 μL supernatant was harvested, brought to 20% FBS, and frozen at -80°C for later plaque titration. Back titrations were conducted on aliquots of all inoculums and confirmed to be within 2-fold of the desired titer. Viral titers from supernatant samples were determined by Vero cell plaque assay.53
Intrathoracic inoculations
To test for virus replication in vivo, groups of at least 50 Cx. quinquefasciatus and Ae. aegypti mosquitoes were IT inoculated with 138 nL stock virus suspension using a Drummond Scientific Nanoject II Auto-Nanoliter Injector (exact inoculum doses provided in the Results). For all inoculations, approximately 5–7 day old female mosquitoes were used. The exact age of the mosquitoes is not known, as pupation and emergence are slightly asynchronous. Mosquitoes were housed in screened paperboard pint containers held at 28˚C, 95% relative humidity, and 16:8 light: dark cycle. Mosquitoes were provided sugar and water ad libitum. Three to five mosquitoes were harvested immediately after inoculation for titration of virus inoculum, and on Days 1, 2, 4, 8, 12, and 14 post inoculation. Mosquitoes were homogenized in 2 mL Eppendorf Safe-Lock tubes with a steal bead and 250 µl mosquito diluent (PBS supplemented with 20% FBS, 50 μg/mL P/S, 50 μg/mL gentamycin, 2.5 μg/mL amphotericin B) via trituration at 25 seconds−1 for one minute with a Retsch Mixer Mill MM400. Debris from mosquitoes were centrifuged at 15,000xg for 5 minutes at 4°C. Clarified supernatant was used to determine virus titer on Vero cells as previously described.53
Oral infections
To assess virus infection and dissemination in each mosquito species following oral exposure through an infectious blood meal, groups of Ae. aegypti and Cx. quinquefasciatus mosquitoes were exposed to VSV-I, V920, or rVSV-SFV. Approximately 5–7 day-old mosquitoes were administered a blood meal containing 1000 μL defibrinated sheep blood, 5 mM adenosine triphosphate (ATP) and 1000 μL thawed virus stock. Virus stocks were not diluted prior to blood meal preparation to maximize the virus concentration to which mosquitoes were exposed. Infectious blood meals were provided via water heated (37°C) glass membrane feeders using hog gut as the membrane. Following one-hour feeding, mosquitoes were anesthetized at 4°C and fully-engorged females were separated into new cartons and maintained on sucrose and water at 28°C for 14 days. Back-titrations of each infectious blood meal were performed on Vero cells to confirm virus titers in the infectious blood meal (titers provided in the Results).
At 14 days post exposure, to allow plenty of time for dissemination to occur, 48 mosquitoes from each group were anesthetized by cold treatment at 4°C. Legs & wings were removed and transferred into a 2 mL Eppendorf Safe-Lock tube containing 250 μL mosquito diluent, and a stainless steel bead for homogenization. Bodies were placed in a separate 2 ml Eppendorf Safe-Lock tube prepared similarly. Mosquito tissues were prepped and titrated as described above.
Virus stability
To address questions regarding vaccine stability in IT inoculated mosquitoes, an experiment was designed whereby a suspension of homogenized Culex or Aedes mosquitoes was spiked with approximately 7 log10 PFU of wt VSV-I or V920 and 6 log10 PFU rVSV-SFV and incubated at 28°C in triplicate. Mosquito suspensions contained five mosquitoes homogenized in 1000 μL mosquito diluent. Ten microliters gentamycin and 1 μl amphotericin B were added to each sample every other day to prevent bacterial and fungal growth arising from mosquito homogenate. Aliquots of spiked homogenate were titrated at 12, 24, 36, 48, 72, 120, and 168 hours post infection by Vero cell plaque assay.53
Ethics statement
USDA Animal and Plant Health Inspection Service (APHIS) permit 132194 issued to Dr. Rebekah Kading permitted receipt of domestic strains of VSV. This research project was approved by the CSU Institutional Biosafety Committee (protocol 16–095B).
Supplementary Material
Funding Statement
This project was funded by the Defense Threat Reduction Agency (HDTRA1-15-C-0058). Any opinion, findings, and conclusion or recommendations expressed in this material are solely those of the authors.
Disclosure of potential conflicts of interest
T.P.M. is an employee of New Link Genetics.
Acknowledgments
We would like to thank Ken Olson and Greg Ebel, Colorado State University, for providing the 4a3b and C6/36, respectively. We also thank the United States Department of Agriculture, Agricultural Research Service, Arthropod-borne Animal Diseases Research Unit in Manhattan, Kansas for providing the CuVa cells. Furthermore, we thank Robert Tesh, University of Texas Medical Branch, for providing the LL-5 cells. We are grateful to Kelly Scappaticci and Brian Martin at NewLink Genetics and Sheri Dubey at Merck & Co. for their assistance and advice in many aspects of the study. The rVSV-SFV construct was generously provided by Dr. Sean Whelan, Department of Microbiology and Immunology, Harvard University.
Contributions
Conceptualization, R.C.K. and T.P.M.; Methodology, R.C.K. and N.A.B.; Investigation, N.A.B. and M.R.M.; Data Curation, N.A.B.; Resources, T.P.M.; Writing – Original Draft, N.A.B., M.R.M., and R.C.K.; Writing – Review & Editing, N.A.B., R.C.K., M.R.M., and T.P.M.; Visualization, N.A.B.; Supervision, R.C.K. and N.A.B.; Project Administration and Funding Acquisition, T.P.M., R.C.K.; Guarantor, R.C.K.
References
- 1.Muyembe-Tamfum JJ, Mulangu S, Masumu J, Kayembe JM, Kemp A, Paweska JT. Ebola virus outbreaks in Africa: Past and present. Onderstepoort J of Vet Res. 2012;79(2):06–13. https://doi.org/ 10.4102/ojvr.v79i2.451. [DOI] [PubMed] [Google Scholar]
- 2.Friedrich M. Ebola Outbreak in West Africa. JAMA. 2014;311(19):1958–8. [Google Scholar]
- 3.WHO April 17 Ebola situation reports. World Health Organization http://apps.who.int/ebola/ebola-situation-reports. Accessed 2017April17. [Google Scholar]
- 4.Feldmann H, Sanchez A, Geisbert TW. Filoviridae. In: Knipe DM, Howley PM, Fields Virol. Volume 1 Philadelphia: (PA: ):Lippincott Williams & Wilkins;2013. p 923–56. [Google Scholar]
- 5.Lee JE, Saphire EO. Ebolavirus glycoprotein structure and mechanism of entry. Future Virol. 2009;4(6):621–35. https://doi.org/ 10.2217/fvl.09.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Feldmann H, Geisbert TW. Ebola haemorrhagic fever. Lancet. 2011;377(9768):849–62. https://doi.org/ 10.1016/S0140-6736(10)60667-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JE, Fusco ML, Hessell AJ, Oswald WB, Burton DR, Saphire EO. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature. 2008;454(7201):177–82. https://doi.org/ 10.1038/nature07082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marzi A, Yoshida R, Miyamoto H, Ishijima M, Suzuki Y, Higuchi M, Matsuyama Y, Igarashi M, Nakayama E, Kuroda M, and others . Protective efficacy of neutralizing monoclonal antibodies in a nonhuman primate model of Ebola hemorrhagic fever. PLoS One. 2012;7(4):e36192. https://doi.org/ 10.1371/journal.pone.0036192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qiu X, Fernando L, Melito PL, Audet J, Feldmann H, Kobinger G, Alimonti JB, Jones SM. Ebola GP-specific monoclonal antibodies protect mice and guinea pigs from lethal Ebola virus infection. PLoS Negl Trop Dis. 2012;6(3):e1575. https://doi.org/ 10.1371/journal.pntd.0001575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Virus Taxonomy, Classification and Nomenclature of Viruses, Ninth Report of the International Committee on Taxonomy of Viruses. AMQ King, MJ Adams, EB Carstens, EJ Lefkowitz, editors. Amsterdam: Elsevier Academic Press; 2012. p 1327. [Google Scholar]
- 11.Traub-Dargatz J, Pelzel-CcCluskey A. Overview of Vesicular Stomatitis. Merck Vet Man. Philadelphia:National Publishing Inc.;2016. p 495–6. [Google Scholar]
- 12.Lyles DS, Kuzmin IV, Rupprecht CE. Rhabdoviridae. In: Knipe DM, Howley PM, editors. Fields Virol. Volume 1. Philadelphia, (PA: ):Lippincott Williams & Wilkins;2013. p 885–922. [Google Scholar]
- 13.Sudia WD, Fields BN, Calisher CH. The Isolation of Vesicular Stomatitis Virus (Indiana Strain) and Other Viruses from Mosquitoes in New Mexico, 19651. Am J Epidemiol. 1967;86(3):598–602. https://doi.org/ 10.1093/oxfordjournals.aje.a120769. [DOI] [PubMed] [Google Scholar]
- 14.Tesh RB, Chaniotis BN, Peralta PH, Johnson KM. Ecology of viruses isolated from Panamanian phlebotomine sandflies. Am J Trop Med Hyg. 1974;23(2):258–69. https://doi.org/ 10.4269/ajtmh.1974.23.258. [DOI] [PubMed] [Google Scholar]
- 15.Francy DB, Moore CG, Smith GC, Jakob WL, Taylor SA, Calisher CH. Epizootic vesicular stomatitis in Colorado, 1982: isolation of virus from insects collected along the northern Colorado Rocky Mountain Front Range. J Med Entomol. 1988;25(5):343–7. https://doi.org/ 10.1093/jmedent/25.5.343. [DOI] [PubMed] [Google Scholar]
- 16.Webb PA, Holbrook RF. Vesicular stomatitis. In: Monath TP, editor The arboviruses: epidemiology and ecology. Volume 5 Boca Raton, (FL: ):CRC Press;1989. p 1–29. [Google Scholar]
- 17.Comer JA, Tesh RB, Modi GB, Corn JL, Nettles VF. Vesicular stomatitis virus, New Jersy serotype: replication in and transmission by Lutzomyia shannoni (diptera: psychodidae). Am J of Trop Med Hyg. 1990;42(5):483–490. https://doi.org/ 10.4269/ajtmh.1990.42.483. [DOI] [PubMed] [Google Scholar]
- 18.Cupp EW, Mare CJ, Cupp MS, Ramberg FB. Biological Transmission of vesicular stomatitis virus (New Jersey) by Simulium vittatum (dipera: simuliidae). J Med Entomol. 1992;29(2):137–140. https://doi.org/ 10.1093/jmedent/29.2.137. [DOI] [PubMed] [Google Scholar]
- 19.Drolet BS, Campbell CL, Stuart MA, Wilson WC. Vector competence of Culicoides sonorensis (Diptera: Ceratopogonidae) for vesicular stomatitis virus. J Med Entomol. 2005;42(3):409–18. https://doi.org/ 10.1093/jmedent/42.3.409. [DOI] [PubMed] [Google Scholar]
- 20.Schnell MJ, Buonocore L, Whitt MA, Rose JK. The minimal conserved transcription stop-start signal promotes stable expression of a foreign gene in vesicular stomatitis virus. J Virol. 1996;70(4):2318–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kahn JS, Roberts A, Weibel C, Buonocore L, Rose JK. Replication-competent or attenuated, nonpropagating vesicular stomatitis viruses expressing respiratory syncytial virus (RSV) antigens protect mice against RSV challenge. J Virol. 2001;75(22):11079–87. https://doi.org/ 10.1128/JVI.75.22.11079-11087.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kapadia SU, Rose JK, Lamirande E, Vogel L, Subbarao K, Roberts A. Long-term protection from SARS coronavirus infection conferred by a single immunization with an attenuated VSV-based vaccine. Virology. 2005;340(2):174–82. https://doi.org/ 10.1016/j.virol.2005.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cobleigh MA, Buonocore L, Uprichard SL, Rose JK, Robek MD. A vesicular stomatitis virus-based hepatitis B virus vaccine vector provides protection against challenge in a single dose. J Virol. 2010;84(15):7513–22. https://doi.org/ 10.1128/JVI.00200-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chattopadhyay A, Wang E, Seymour R, Weaver SC, Rose JK. A chimeric vesiculo/alphavirus is an effective alphavirus vaccine. J Virol. 2013;87(1):395–402. https://doi.org/ 10.1128/JVI.01860-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mire CE, Matassov D, Geisbert JB, Latham TE, Agans KN, Xu R, Ota-Setlik A, Egan MA, Fenton KA, Clarke DK and others. Single-dose attenuated Vesiculovax vaccines protect primates against Ebola Makona virus. Nature. 2015;520(7549):688–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nasar F, Matassov D, Seymour RL, Latham T, Gorchakov RV, Nowak RM, Leal G, Hamm S, Eldridge JH, Tesh RB and others. Recombinant Isfahan Virus and Vesicular Stomatitis Virus Vaccine Vectors Provide Durable, Multivalent, Single-Dose Protection against Lethal Alphavirus Challenge. J Virol. 2017;91(8). https://doi.org/ 10.1128/JVI.01729-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garbutt M, Liebscher R, Wahl-Jensen V, Jones S, Möller P, Wagner R, Volchkov V, Klenk H-D, Feldmann H, Ströher U. Properties of Replication-Competent Vesicular Stomatitis Virus Vectors Expressing Glycoproteins of Filoviruses and Arenaviruses. J Virol. 2004;78(10):5458–5465. https://doi.org/ 10.1128/JVI.78.10.5458-5465.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jones SM, Feldmann H, Stroher U, Geisbert JB, Fernando L, Grolla A, Klenk H-D, Sullivan NJ, Volchkov VE, Fritz EA and others Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med. 2005;11(7):786–90. https://doi.org/ 10.1038/nm1258. [DOI] [PubMed] [Google Scholar]
- 29.Geisbert TW, Feldmann H. Recombinant vesicular stomatitis virus-based vaccines against Ebola and Marburg virus infections. J Infect Dis. 2011;204(Suppl 3):S1075–81. https://doi.org/ 10.1093/infdis/jir349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Geisbert TW, Geisbert JB, Leung A, Daddario-DiCaprio KM, Hensley LE, Grolla A, Feldmann H. Single-injection vaccine protects nonhuman primates against infection with marburg virus and three species of ebola virus. J Virol. 2009;83(14):7296–304. https://doi.org/ 10.1128/JVI.00561-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson JE, Nasar F, Coleman JW, Price RE, Javadian A, Draper K, Lee M, Reilly PA, Clarke DK, Hendry RM and others Neurovirulence properties of recombinant vesicular stomatitis virus vectors in non-human primates. Virology. 2007;360(1):36–49. https://doi.org/ 10.1016/j.virol.2006.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Geisbert TW, Daddario-Dicaprio KM, Geisbert JB, Reed DS, Feldmann F, Grolla A, Stroher U, Fritz EA, Hensley LE, Jones SM and others Vesicular stomatitis virus-based vaccines protect nonhuman primates against aerosol challenge with Ebola and Marburg viruses. Vaccine. 2008;26(52):6894–900. https://doi.org/ 10.1016/j.vaccine.2008.09.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Geisbert TW, Daddario-DiCaprio KM, Lewis MG, Geisbert JB, Grolla A, Leung A, Paragas J, Matthias L, Smith MA, Jones SM and others Vesicular Stomatitis Virus-Based Ebola Vaccine Is Well-Tolerated and Protects Immunocompromised Nonhuman Primates. PLoS Path. 2008;4(11):e1000225. https://doi.org/ 10.1371/journal.ppat.1000225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Qiu X, Fernando L, Alimonti JB, Melito PL, Feldmann F, Dick D, Stroher U, Feldmann H, Jones SM. Mucosal immunization of cynomolgus macaques with the VSVDeltaG/ZEBOVGP vaccine stimulates strong ebola GP-specific immune responses. PLoS One. 2009;4(5):e5547. https://doi.org/ 10.1371/journal.pone.0005547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Agnandji ST, Huttner A, Zinser ME, Njuguna P, Dahlke C, Fernandes JF, Yerly S, Dayer J-A, Kraehling V, Kasonta R and others Phase 1 Trials of rVSV Ebola Vaccine in Africa and Europe. NEJM. 2016;374(17):1647–1660. https://doi.org/ 10.1056/NEJMoa1502924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Huttner A, Dayer J-A, Yerly S, Combescure C, Auderset F, Desmeules J, Eickmann M, Finckh A, Goncalves AR, Hooper JW and others The effect of dose on the safety and immunogenicity of the VSV Ebola candidate vaccine: a randomised double-blind, placebo-controlled phase 1/2 trial. Lancet Infect Dis. 2015;15(10):1156–1166. https://doi.org/ 10.1016/S1473-3099(15)00154-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Henao-Restrepo AM, Camacho A, Longini IM, Watson CH, Edmunds WJ, Egger M, Carroll MW, Dean NE, Diatta I, Doumbia M and others Efficacy and effectiveness of an rVSV-vectored vaccine in preventing Ebola virus disease: final results from the Guinea ring vaccination, open-label, cluster-randomised trial (Ebola Ca Suffit!). Lancet. 2017;389(10068):505–518. https://doi.org/ 10.1016/S0140-6736(16)32621-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Regules JA, Beigel JH, Paolino KM, Voell J, Castellano AR, Hu Z, Muñoz P, Moon JE, Ruck RC, Bennett JW and others . A Recombinant Vesicular Stomatitis Virus Ebola Vaccine. NEJM. 2017;376(4):330–341. https://doi.org/ 10.1056/NEJMoa1414216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Heppner DG Jr., Kemp TL, Martin BK, Ramsey WJ, Nichols R, Dasen EJ, Link CJ, Das R, Xu ZJ, Sheldon EA and others . Safety and immunogenicity of the rVSV∆G-ZEBOV-GP Ebola virus vaccine candidate in healthy adults: a phase 1b randomised, multicentre, double-blind, placebo-controlled, dose-response study. Lancet Infect Dis. 2017;17(8):854–866. https://doi.org/ 10.1016/S1473-3099(17)30313-4. [DOI] [PubMed] [Google Scholar]
- 40.Pedersen CE Jr., Robinson DM, Cole FE Jr.. Isolation of the vaccine strain of Venezuelan equine encephalomyelitis virus from mosquitoes in Louisiana. Am J Epidemiol. 1972;95(5):490–6. https://doi.org/ 10.1093/oxfordjournals.aje.a121416. [DOI] [PubMed] [Google Scholar]
- 41.Turell MJ, Bressler DS, Rossi CA. Short report: lack of virus replication in arthropods after intrathoracic inoculation of Ebola Reston virus. Am J Trop Med Hyg. 1996;55(1):89–90. https://doi.org/ 10.4269/ajtmh.1996.55.89. [DOI] [PubMed] [Google Scholar]
- 42.Nunamaker RA, De León AAP Campbell CL, Lonning SM. Oral Infection of Culicoides sonorensis (Diptera: Ceratopogonidae) by Vesicular Stomatitis Virus. J Med Entomol. 2000;37(5):784–786. https://doi.org/ 10.1603/0022-2585-37.5.784. [DOI] [PubMed] [Google Scholar]
- 43.Mussgay M, Suarez O. Multiplication of Vesicular Stomatitis Virus in Aedes Aegypti (L) Mosquitoes. Virology. 1962;17(1):202-&. https://doi.org/ 10.1016/0042-6822(62)90100-9. [DOI] [PubMed] [Google Scholar]
- 44.Bergold GH, Suárez OM, Munz K. Multiplication in and transmission by Aedes aegypti of vesicular stomatitis virus. J Invertebr Pathol. 1968;11(3):406–428. https://doi.org/ 10.1016/0022-2011(68)90190-0. [DOI] [PubMed] [Google Scholar]
- 45.Kononchik JP, Hernandez R, Brown DT. An alternative pathway for alphavirus entry. Virology Journal. 2011;8(1):304. https://doi.org/ 10.1186/1743-422X-8-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Igarashi A. Isolation of a Singh's Aedes albopictus Cell Clone Sensitive to Dengue and Chikungunya Viruses. J Gen Virol. 1978;40(3):531–544. https://doi.org/ 10.1099/0022-1317-40-3-531. [DOI] [PubMed] [Google Scholar]
- 47.Kawakami E, Watanabe T, Fujii K, Goto H, Watanabe S, Noda T, Kawaoka Y. Strand-specific real-time RT-PCR for distinguishing influenza vRNA, cRNA, and mRNA. J Virol Methods. 2011;173(1):1–6. https://doi.org/ 10.1016/j.jviromet.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu I, Zee Y. The pathogenesis of vesicular stomatitis virus, serotype Indiana, in Aedes aegypti mosquitoes, after imbibition of a viremic blood meal. Arch Virol. 1976;52:259–262. https://doi.org/ 10.1007/BF01348023. [DOI] [PubMed] [Google Scholar]
- 49.Kading RC, Biggerstaff BJ, Young G, Komar N. Mosquitoes Used to Draw Blood for Arbovirus Viremia Determinations in Small Vertebrates. PLoS One. 2014;9(6):e99342. https://doi.org/ 10.1371/journal.pone.0099342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Müller H-M, Dimopoulos G, Blass C, Kafatos FC. A Hemocyte-like Cell Line Established from the Malaria VectorAnopheles gambiae Expresses Six Prophenoloxidase Genes. J Biol Chem. 1999;274(17):11727–35. https://doi.org/ 10.1074/jbc.274.17.11727. [DOI] [PubMed] [Google Scholar]
- 51.Tesh RB, Modi GB. Development of a Continuous Cell Line from the Sand Fly Lutzomyia Longipalpis (Diptera: Psychodidae), and its Susceptibility to Infection with Arboviruses1. J Med Entomol. 1983;20(2):199–202. https://doi.org/ 10.1093/jmedent/20.2.199. [DOI] [PubMed] [Google Scholar]
- 52.Wechsler SJ, McHolland LE, Tabachnick WJ. Cell lines from Culicoides variipennis (Diptera: Ceratopogonidae) support replication of bluetongue virus. J Invertebr Pathol. 1989;54(3):385–393. https://doi.org/ 10.1016/0022-2011(89)90123-7. [DOI] [PubMed] [Google Scholar]
- 53.Beaty B, Calisher C, Shope R. Arboviruses. Diagnostic procedures for viral, rickettsial and chlamydial infections. 6 Washington, (DC):American Public Health Association;1989. p 797–856. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


