Abstract
Introduction
Young adults with hyperlipidemia, hypertension, and diabetes are at increased risk of developing heart disease later in life. Despite emphasis on early screening, little is known about awareness of these risk factors in young adulthood.
Methods
Data from the nationally representative cross-sectional survey National Health and Nutrition Examination Survey 2011–2014 were analyzed in 2017 to estimate the prevalence of self-reported awareness of hypercholesterolemia, hypertension, and diabetes in U.S. young adults aged 18–39 years (n=11,083). Prevalence estimates were weighted to population estimates using survey procedures, and predictors of awareness were identified using weighted logistic regression.
Results
Among U.S. young adults, the prevalence of hypercholesterolemia, hypertension, and diabetes was 8.8% (SE=0.4%), 7.3% (SE=0.3%), and 2.6% (SE=0.2%), respectively. The prevalence of borderline high cholesterol, blood pressure, and blood glucose were substantially higher (21.6% [SE= 0.6%], 26.9% [SE=0.7%], and 18.9% [SE=0.6%], respectively). Awareness was low for hypercholesterolemia (56.9% [SE=2.4%]) and moderate for hypertension and diabetes (62.7% [SE=2.4%] and 70.0% [SE=2.7%]); <25% of young adults with borderline levels of these risk factors were aware of their risk. Correlates of risk factor awareness included older age, insurance status, family income above the poverty line, U.S. origin, having a usual source of health care, and the presence of comorbid conditions.
Conclusions
Despite the high prevalence of cardiovascular risk factors in U.S. young adults, awareness remains less than ideal. Interventions that target access may increase awareness and facilitate achieving treatment goals in young adults.
INTRODUCTION
Atherosclerosis begins early in life and can lead to coronary heart disease (CHD) in older adulthood.1,2 Young adults with cardiovascular risk factors are at increased risk of CHD later in life, and even borderline levels of these risk factors are associated with atherosclerotic changes that persist into adulthood.1,3–9 Moreover, studies have shown that individuals who reach middle- age with favorable levels of major cardiovascular risk factors have a significantly lower incidence of cardiovascular disease and greater longevity, highlighting the imperative for recognizing and treating cardiovascular risk factors early in life.10–12 As a result, many guidelines now recommend universal screening for hypertension and hyperlipidemia in children and adolescents.13,14 By contrast, screening for cardiovascular risk factors in young adults is recommended primarily among patients with identified CHD risk factors.15,16
Despite the emphasis on early but selective screening, little is known about patient awareness of these risk factors in young adulthood. Prior literature suggests that the prevalence of suboptimal cholesterol, blood pressure, and blood glucose in young adults may be as high as 38%, 7%, and 4.5%, respectively.17–21 Although a few studies have examined undiagnosed hypercholesterolemia, hypertension, and diabetes in U.S. adults,19,21–27 no studies have evaluated awareness across multiple risk factors, in patients with borderline levels of these risk factors, or in young adults specifically.
Accordingly, this study aims to quantify the prevalence of self-reported awareness among U.S. young adults with hypercholesterolemia, hypertension, or diabetes, and to identify sociodemographic and clinical correlates of awareness. Such information is critical to identifying gaps in screening and education in order to better target populations who are undiagnosed or unaware of their cardiovascular risk.
METHODS
Study Sample
Data from the 2005–2014 National Health and Nutrition Examination Survey (NHANES) were used to evaluate the prevalence of self-reported awareness of high and borderline cholesterol, blood pressure, and blood glucose in U.S. young adults aged 18 to 39 years. Conducted by the National Center for Health Statistics, NHANES uses a stratified, multistage sampling design to obtain a nationally representative sample of the U.S. non-institutionalized civilian population. It collects detailed information on participant demographic, socioeconomic, and health-related characteristics through in-home interviews and clinical assessments. All non-pregnant participants aged 18 to 39 years were included in this sample (n=11,083).
Measures
Detailed descriptions about blood collection and processing are provided in the NHANES Laboratory/Medical Technologists Procedures Manual. Specimens for total cholesterol, glycosylated hemoglobin, and serum glucose were stored under refrigerated conditions and shipped weekly to the University of Minnesota or the University of Missouri-Columbia for processing. Blood pressure was measured by auscultation three consecutive times after participants had been seated for 5 minutes.
High and borderline levels of blood cholesterol, blood pressure, and blood glucose were defined using the 2013 American Heart Association/American College of Cardiology Guidelines28 and prior studies using NHANES.17,19,24,26,29,30 Hypercholesterolemia was defined as total cholesterol ≥240 mg/dL or current self-reported use of cholesterol-lowering medications. Borderline high cholesterol was defined as total cholesterol between 200 and 239 mg/dL. Consistent with the definition at the time of the analysis, hypertension was defined as an average systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg or current self-reported use of antihypertensive medication. Borderline hypertension was defined as an average blood pressure of 120–139 mmHg systolic or 80–89 mmHg diastolic. Because 56.9% of participants were missing fasting plasma glucose (FPG), both FPG and hemoglobin A1c (HbA1c) were used to identify individuals with diabetes and borderline diabetes. Type 1 or Type 2 diabetes was defined as FPG ≥126 mg/dL or HbA1c ≥6.5%, or self-reported use of insulin or oral agents. Borderline diabetes was defined as FPG 100–125 mg/dL or HbA1c 5.7%–6.5%. Missing total cholesterol, blood pressure measurements, and FPG or HbA1c accounted for 1,139 (10.3%), 946 (8.5%), and 1,069 (9.7%) of observations, respectively.
Participants were asked if they had ever been told by a doctor or health professional that their blood cholesterol level was high, that they had hypertension or high blood pressure, or that they had diabetes, prediabetes, impaired glucose tolerance, or borderline diabetes. Those responding affirmatively were categorized as being aware of having hypercholesterolemia, hypertension, and diabetes, respectively.
Several sociodemographic and clinical variables were examined including age, sex, race/ethnicity, poverty, insurance status, education, place of birth, usual source of care, and other cardiovascular risk factors, including hypercholesterolemia, hypertension, diabetes, BMI (healthy BMI [<25 kg/m2], overweight [25–29.9kg/m2] and obese [≥30kg/m2]), smoking status (never, past, and current), and family history of early cardiovascular disease. Poverty was defined as the ratio of family income to geographic poverty level <133%.31 Usual source of care was categorized as no usual source, hospital emergency room or outpatient department, and doctor’s office or clinic/health center. Family history of cardiovascular disease was defined as having a close family relative with a heart attack or angina aged <50 years.
Statistical Analysis
NHANES data were analyzed in 2017 using the survey procedures in SAS, version 9.4 to account for the complex survey design.32 The prevalence of hypercholesterolemia, hypertension, and diabetes and borderline levels of these risk factors were estimated in the U.S. young adult population. Awareness for these risk factors was calculated among those with high or borderline levels and compared across participant characteristics using Rao–Scott modified chi-square tests. Multivariable logistic regression analyses were used to identify covariates associated with hypercholesterolemia, hypertension, and diabetes awareness. Covariates were selected using a backwards elimination model and retained in the final model if they were associated with risk factor awareness at the p<0.05 level.
Missing covariate data were rare. There was missing data for ≅13% of participants on one variable, 10% of participants on two variables, and 1% of participants on three or more variables. Missing covariate data were imputed using a single imputation approach. Outcome data (i.e., awareness) were missing in 33.9%, 0%, and 0.3% of participants with high or borderline cholesterol, blood pressure, and blood glucose, respectively. Outcome data were not imputed. Participants with missing cholesterol awareness data were more likely to be younger, uninsured, and to lack a usual source of care. Consent for participation in NHANES was obtained during the initial screening visit. This analysis was deemed exempt under federal regulation 45 CFR §46.101(b).
RESULTS
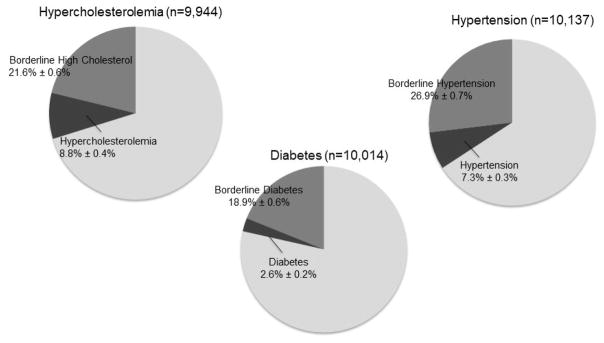
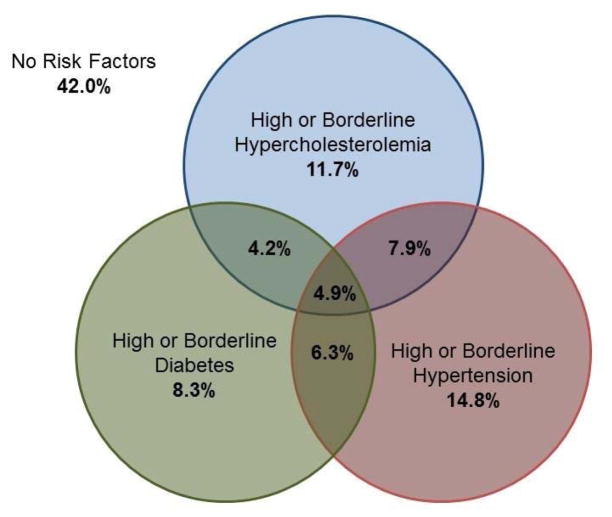
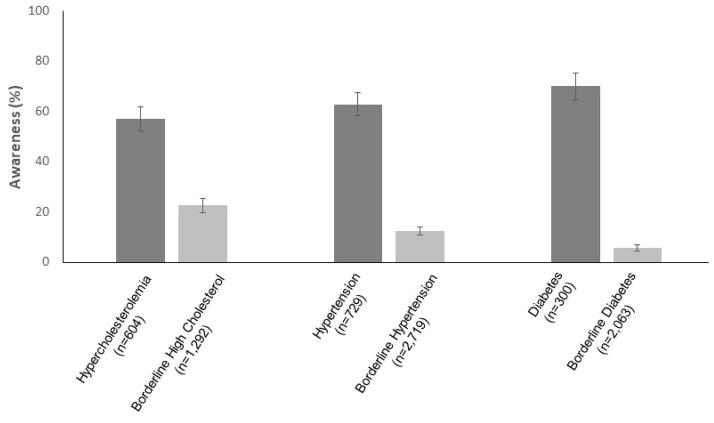
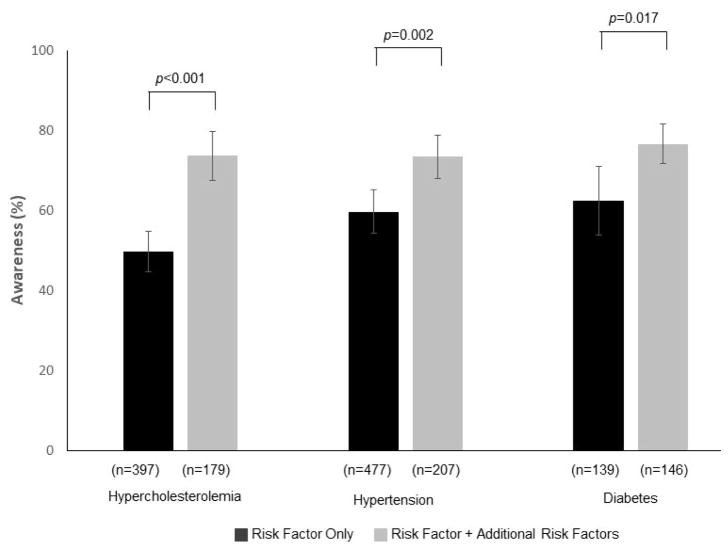
Among U.S. young adults aged 18 to 39 years, 8.8% (SE=0.4%) had hypercholesterolemia and 21.6% (SE=0.6%) had borderline high cholesterol (Figure 1). An estimated 7.3% (SE=0.3%) of young adults had hypertension and 26.9% (SE=0.7%) had borderline hypertension. There were 2.6% (SE=0.2%) of young adults that had Type 1 or Type 2 diabetes and 18.9% (SE=0.6%) had borderline diabetes. Approximately 18.9% (SE=1.6%) of adults with hypercholesterolemia, 43.9% (SE=2.3%) of adults with hypertension, and 53.4% (SE=3.1%) of adults with diabetes reported taking medications to treat these conditions. The prevalence of comorbid hypercholesterolemia, hypertension, and diabetes are provided in Appendix Figures 1 and 2. The majority of young adults with hypercholesterolemia, hypertension, or diabetes had only a single risk factor; however, there was significant overlap among individuals with borderline levels of these risk factors. Of those with hypercholesterolemia, 56.9% (SE=2.4%) were aware of their elevated cholesterol, whereas 62.7% (SE=2.4%) of young adults with hypertension were aware of having hypertension, and 70.0% (SE=2.7%) of those with diabetes knew of their diagnosis (Figure 2). Awareness among individuals with borderline high levels of cholesterol, blood pressure, and blood glucose was significantly lower (22.5% [SE=1.4%], 12.3% [SE=0.8%], and 5.7% [SE=0.7%], respectively). In general, awareness was higher in young adults with more than one risk factor compared with those with only one risk factor (Appendix Figure 3).
Figure 1.
Prevalence of cardiovascular risk factors in U.S young adults aged 18–39 years from the National Health and Nutrition Examination Survey 2005–2014.
aBorderline high cholesterol was defined as total cholesterol (fasting or nonfasting [2.2%]) 200–239mg/dL and high cholesterol was defined as total cholesterol ≥240mg/dL or self-reported use of cholesterol-lowering agent. Hypertension was defined as blood pressure ≥140/90mmHg averaged over three measurements or self-reported use of blood pressure lowering agent. Borderline hypertension was defined as average blood pressure 120–139/80–89mmgHg. Diabetes was defined as fasting blood glucose ≥126mg/dL or hemoglobin A1c ≥6.5%. Or self-reported use of insulin or oral agents. Borderline diabetes was defined as fasting blood glucose 100–125mg/dL or hemoglobin A1c 5.7–6.4%.
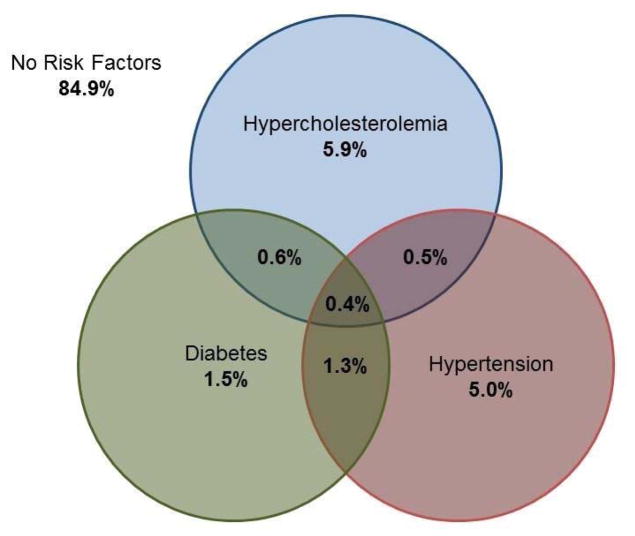
Appendix Figure 1.
Overlap of hypercholesterolemia, hypertension, and diabetes in U.S. young adults aged 18–39 years.
Appendix Figure 2.
Overlap of high and borderline hypercholesterolemia, hypertension, and diabetes in U.S. young adults aged 18–39 years.
Figure 2.
Percentage of young adults (aged 18 to 30 years) with high or borderline levels of cholesterol, blood pressure, and blood glucose reporting awareness of their risk factor from the National Health and Nutrition Examination Survey 2005–2014.
Appendix Figure 3.
Percentage of young adults with a single or multiple risk factors reporting awareness of hypercholesterolemia, hypertension, or diabetes.
Factors associated with hypercholesterolemia, hypertension, and diabetes awareness are provided in Table 1. After multivariable adjustment, insurance status and having a usual source of care were independent correlates of hypercholesterolemia, hypertension, and diabetes awareness (Table 2). Other correlates of hypercholesterolemia awareness included older age and concurrent diabetes. Similarly, older age, female gender, U.S. origin, concurrent diabetes, and current smoking were significantly associated with hypertension awareness, and non-Hispanic white race/ethnicity was associated with diabetes awareness. Relative to non-Hispanic white adults, non-Hispanic black adults and Hispanic adults were significantly less likely to be aware of their diabetes.
Table 1.
Percentage of U.S. Young Adults (Aged 18 to 39 Years) With Hypercholesterolemia, Hypertension, and Diabetes Reporting Awareness of Their Risk Factor by Participant Characteristics From NHANES 2005–2014a
| Characteristic | Awareness of hypercholesterolemia (n=604) | Awareness of hypertension (n=729) | Awareness of diabetes (n=300) | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Overall N | Weighted % ± SE | p-value | Overall N | Weighted % ± SE | p-value | Overall N | Weighted % ± SE | p-value | |
| Age | <0.001 | <0.001 | 0.759 | ||||||
| 18–29 years | 151 | 40.6 ± 3.8 | 200 | 46.1 ± 4.5 | 89 | 68.7 ± 4.5 | |||
| 30–39 years | 453 | 62.9 ± 2.7 | 529 | 69.4 ± 2.3 | 211 | 70.4 ± 3.3 | |||
| Gender | 0.167 | <0.001 | <0.001 | ||||||
| Male | 347 | 54.2 ± 3.1 | 463 | 53.4 ± 2.8 | 165 | 59.8 ± 4.1 | |||
| Female | 257 | 60.6 ± 3.5 | 266 | 80.2 ± 2.9 | 135 | 81.1 ± 3.6 | |||
| Race/Ethnicity | 0.077 | 0.121 | <0.001 | ||||||
| Non-Hispanic white | 301 | 60.0 ± 3.2 | 295 | 63.4 ± 3.5 | 101 | 81.8 ± 3.6 | |||
| Non-Hispanic black | 101 | 57.8 ± 4.0 | 248 | 68.3 ± 2.9 | 75 | 69.2 ± 5.6 | |||
| Mexican American or other Hispanic | 138 | 47.5 ± 4.5 | 123 | 54.7 ± 5.0 | 89 | 50.3 ± 5.6 | |||
| Other race/ethnicity | 64 | 49.6 ± 8.1 | 63 | 55.0 ± 7.5 | 35 | 60.0 ± 9.5 | |||
| Education | 0.344 | 0.782 | 0.004 | ||||||
| Less than high school | 108 | 50.1 ± 5.2 | 141 | 60.9 ± 4.7 | 72 | 56.6 ± 6.8 | |||
| High school graduate | 125 | 61.6 ± 5.1 | 188 | 65.3 ± 3.9 | 79 | 63.5 ± 5.2 | |||
| College graduate | 364 | 57.3 ± 3.1 | 367 | 62.9 ± 3.2 | 133 | 77.2 ± 3.4 | |||
| Missing | 7 | – | 33 | – | 16 | – | |||
| Poverty | 0.106 | 0.841 | 0.001 | ||||||
| No | 370 | 58.9 ± 3.0 | 431 | 62.9 ± 2.9 | 148 | 75.9 ± 2.9 | |||
| Yes | 185 | 49.4 ± 4.8 | 251 | 62.1 ± 3.2 | 123 | 59.4 ± 5.1 | |||
| Missing | 49 | – | 29 | – | |||||
| Insured | <0.001 | <0.001 | <0.001 | ||||||
| No | 165 | 38.0 ± 5.5 | 206 | 47.2 ± 4.1 | 117 | 53.1 ± 4.0 | |||
| Yes | 439 | 62.0 ± 2.7 | 523 | 67.7 ± 2.5 | 183 | 78.8 ± 3.4 | |||
| Foreign born | 0.085 | <0.001 | 0.001 | ||||||
| No | 460 | 58.5 ± 2.5 | 614 | 65.1 ± 2.6 | 226 | 74.8 ± 2.9 | |||
| Yes | 144 | 49.8 ± 4.9 | 115 | 46.3 ± 4.4 | 74 | 48.3 ± 7.4 | |||
| Usual source of care | <0.001 | <0.001 | <0.001 | ||||||
| None | 132 | 34.7 ± 4.7 | 171 | 35.6 ± 4.6 | 66 | 42.6 ± 5.6 | |||
| Hospital or health center | 120 | 55.9 ± 5.5 | 142 | 67.8 ± 4.9 | 77 | 68.3 ± 7.0 | |||
| Private clinic or doctor’s office | 352 | 64.4 ± 2.8 | 416 | 70.9 ± 2.9 | 157 | 80.0 ± 3.4 | |||
| Cholesterol | – | 0.091 | 0.011 | ||||||
| Normal | – | – | 351 | 61.9 ± 3.1 | 131 | 70.3 ± 4.6 | |||
| Borderline hypercholesterolemia | – | – | 175 | 60.2 ± 4.1 | 71 | 55.4 ± 6.7 | |||
| Hypercholesterolemia | – | – | 157 | 71.8 ± 4.1 | 96 | 79.6 ± 3.8 | |||
| Missing | – | – | 46 | – | 2 | – | |||
| Blood pressure | <0.001 | – | 0.027 | ||||||
| Normal | 276 | 53.4 ± 3.0 | – | – | 101 | 66.7 ± 5.4 | |||
| Borderline hypertension | 164 | 48.1 ± 4.3 | – | – | 93 | 60.7 ± 4.8 | |||
| Hypertension | 135 | 73.1 ± 5.2 | – | – | 86 | 79.7 ± 4.6 | |||
| Missing | 29 | – | – | – | 20 | – | |||
| Glucose intolerance | 0.003 | <0.001 | – | ||||||
| Normal | 342 | 53.5 ± 3.2 | 368 | 57.1 ± 3.3 | – | – | |||
| Borderline diabetes | 178 | 53.3 ± 5.4 | 235 | 68.4 ± 3.0 | – | – | |||
| Diabetes | 75 | 81.8 ± 4.7 | 86 | 82.7 ± 4.1 | – | – | |||
| Missing | 9 | – | 40 | – | – | – | |||
| BMI (kg/m2) | 0.124 | 0.001 | 0.503 | ||||||
| Healthy BMI (<25kg/m2) | 137 | 51.8 ± 4.6 | 107 | 53.9 ± 5.3 | 44 | 74.1 ± 8.2 | |||
| Overweight (25–30kg/m2) | 185 | 53.9 ± 4.4 | 156 | 52.9 ± 4.5 | 65 | 75.2 ± 5.6 | |||
| Obese (>30kg/m2) | 282 | 62.1 ± 3.3 | 466 | 68.8 ± 2.6 | 191 | 67.3 ± 3.6 | |||
| Smoking | 0.287 | 0.047 | 0.112 | ||||||
| Never | 333 | 58.0 ± 3.0 | 400 | 57.8 ± 3.2 | 164 | 70.2 ± 4.1 | |||
| Past | 90 | 62.9 ± 5.4 | 94 | 72.5 ± 6.2 | 35 | 81.7 ± 5.4 | |||
| Current | 180 | 51.5 ± 5.2 | 204 | 68.1 ± 4.1 | 86 | 62.6 ± 5.6 | |||
| Missing | 1 | – | 31 | – | 15 | ||||
| Family history of cardiovascular disease | 0.916 | 0.081 | 0.043 | ||||||
| No | 487 | 56.9 ± 2.8 | 566 | 61.4 ± 2.7 | 230 | 66.9 ± 3.0 | |||
| Yes | 91 | 57.8 ± 7.5 | 115 | 70.9 ± 4.5 | 44 | 81.4 ± 5.8 | |||
| Missing | 26 | – | 48 | – | 26 | ||||
All percentages are row percentages. Boldface indicates statistical significant (p<0.05).
NHANES, National Health and Nutrition Examination Survey
Table 2.
Sociodemographic and Clinical Correlates of Cardiovascular Risk Factor Awareness in U.S. Young Adults (Aged 18 to 30 Years) From NHANES 2005–2014
| Characteristic | Awareness of hypercholesterolemia (n=604) | Awareness of hypertension (n=729) | Awareness of diabetes (n=300) | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Unadjusted Weighted OR (95% CI) | Adjusted Weighted OR (95% CI)a | Unadjusted Weighted OR (95% CI) | Adjusted Weighted OR (95% CI)a | Unadjusted Weighted OR (95% CI) | Adjusted Weighted OR (95% CI)a | |
| Age | ||||||
| 18–29 years | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| 30–39 years | 2.48 (1.68, 3.65) | 2.35 (1.53, 3.61) | 2.65 (1.83, 3.84) | 2.05 (1.36, 3.09) | 1.08 (0.64, 1.84) | |
| Gender | ||||||
| Male | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Female | 1.30 (0.89, 1.90) | 3.53 (2.37, 5.24) | 2.89 (1.80, 4.66) | 2.89 (1.57, 5.31) | ||
| Race/Ethnicity | ||||||
| Non-Hispanic white | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Non-Hispanic black | 0.91 (0.61, 1.38) | 1.24 (0.88, 1.76) | 0.50 (0.24, 1.04) | 0.51 (0.24, 1.07) | ||
| Mexican American or other Hispanic | 0.60 (0.40, 0.92) | 0.69 (0.42, 1.16) | 0.23 (0.12, 0.44) | 0.35 (0.16, 0.76) | ||
| Other race/ethnicity | 0.66 (0.32, 1.33) | 0.71 (0.36, 1.38) | 0.33 (0.14, 0.81) | 0.41 (0.15, 1.10) | ||
| Education | ||||||
| Less than high school | 1.00 | 1.00 | 1.00 | |||
| High school graduate | 1.27 (0.76, 2.13) | 1.45 (0.92, 2.28) | 1.82 (0.94, 0.35) | |||
| College graduate | 1.62 (0.98, 2.69) | 0.97 (0.54, 1.39) | 1.89 (0.91, 3.92) | |||
| Poverty | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 0.73 (0.45, 1.17) | 0.98 (0.70, 1.37) | 0.52 (0.32, 0.84) | |||
| Insured | ||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 2.66 (1.57, 4.51) | 2.14 (1.25, 3.65) | 2.35 (1.61, 3.43) | 1.93 (1.23, 3.00) | 3.29 (1.89, 5.74) | 1.99 (1.01, 3.89) |
| Foreign born | ||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Yes | 0.71 (0.47, 1.05) | 0.46 (0.31, 0.69) | 0.51 (0.32, 0.82) | 0.32 (0.16, 0.63) | ||
| Usual source of care | ||||||
| None | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Hospital or health center | 2.38 (1.35, 4.20) | 1.62 (0.92, 2.85) | 3.81 (1.98, 7.31) | 3.09 (1.56, 6.09) | 2.91 (1.27, 6.66) | 1.91 (0.87, 4.22) |
| Private clinic or doctor’s office | 3.40 (2.13, 5.44) | 2.09 (1.24, 3.53) | 4.41 (2.78, 6.99) | 2.60 (1.56, 4.33) | 5.40 (3.07, 9.51) | 2.72 (1.26, 5.89) |
| Cholesterol | ||||||
| Normal | – | 1.00 | 1.00 | |||
| Borderline hypercholesterolemia | – | 0.94 (0.62, 1.44) | 0.52 (0.25, 1.06) | |||
| Hypercholesterolemia | – | 1.67 (1.05, 2.67) | 1.62 (0.84, 3.14) | |||
| Blood pressure | ||||||
| Normal | 1.00 | – | 1.00 | |||
| Borderline hypertension | 0.85 (0.58, 1.25) | – | 0.81 (0.43, 1.52) | |||
| Hypertension | 2.33 (1.29, 4.22) | – | 1.61 (0.85, 3.07) | |||
| Glucose intolerance | ||||||
| Normal | 1.00 | 1.00 | 1.00 | 1.00 | – | |
| Borderline diabetes | 1.03 (0.61, 1.75) | 1.11 (0.62, 1.99) | 1.56 (1.10, 2.21) | 1.68 (1.16, 2.45) | – | |
| Diabetes | 3.92 (1.88, 8.14) | 3.90 (1.86, 8.17) | 3.84 (2.16, 6.80) | 3.94 (2.05, 7.57) | – | |
| BMI (kg/m2) | ||||||
| Healthy BMI (<25kg/m2) | 1.00 | 1.00 | 1.00 | |||
| Overweight (25–30kg/m2) | 1.09 (0.64, 1.84) | 0.96 (0.63, 1.47) | 1.06 (0.38, 2.96) | |||
| Obese (>30kg/m2) | 1.52 (1.01, 2.30) | 1.89 (1.19, 3.01) | 0.72 (0.28, 1.87) | |||
| Smoking | ||||||
| Never | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Past | 1.23 (0.75, 2.02) | 1.80 (0.92, 3.49) | 1.83 (0.91, 3.68) | 1.93 (0.79, 4.75) | ||
| Current | 0.77 (0.48, 1.26) | 1.56 (0.99, 2.47) | 1.81 (1.06, 3.08) | 0.69 (0.37, 1.27) | ||
| Family history of cardiovascular disease | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 1.06 (0.54, 2.07) | 1.55 (0.94, 2.55) | 1.83 (0.86, 3.87) | |||
Multivariate models used a backwards elimination approach evaluating changes in likelihood ratios. Final model included only those variables associated (p<0.10) with risk factor awareness. Variables that were not included in the multivariate model are left blank.
NHANES, National Health and Nutrition Examination Survey
When analyses were repeated in young adults with borderline risk factors, associations between sociodemographic and clinical factors with risk factor awareness were generally weaker (Appendix Table 1). Among young adults with borderline high cholesterol, correlates of awareness included higher education and family history of cardiovascular disease (Appendix Table 2). Correlates of awareness in individuals with borderline high blood pressure included older age, race/ethnicity, U.S. origin and overweight or obesity, and correlates of awareness in individuals with borderline diabetes included older age, race/ethnicity, and family history of cardiovascular disease.
Appendix Table 1.
Percentage of Young Adults With Borderline Hypercholesterolemia, Hypertension, and Diabetes Reporting Awareness of Their Risk Factor by Participant Characteristicsa
| Characteristic | Awareness of borderline hypercholesterolemia (n=1,292) | Awareness of borderline hypertension (n=2,719) | Awareness of borderline diabetes (n=2,063) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall N | Weighted % ± SE | p-value | Overall N | Weighted % ± SE | p-value | Overall N | Weighted % ± SE | p-value | |
| Age | 0.177 | 0.001 | <0.001 | ||||||
| 18–29 years | 438 | 20.3 ± 1.8 | 1,501 | 9.9 ± 0.9 | 933 | 3.1 ± 0.8 | |||
| 30–39 years | 854 | 23.7 ± 1.9 | 1,218 | 15.1 ± 1.2 | 1,130 | 7.6 ± 1.0 | |||
| Gender | 0.824 | 0.305 | <0.001 | ||||||
| Male | 680 | 22.2 ± 1.8 | 1,970 | 11.8 ± 0.9 | 1,273 | 3.7 ± 0.7 | |||
| Female | 612 | 22.8 ± 2.3 | 749 | 13.7 ± 1.5 | 790 | 9.1 ± 1.2 | |||
| Race/Ethnicity | 0.845 | 0.128 | 0.023 | ||||||
| Non-Hispanic white | 537 | 22.7 ± 2.1 | 1,041 | 12.6 ± 1.2 | 637 | 5.1 ± 1.0 | |||
| Non-Hispanic black | 267 | 21.6 ± 2.7 | 737 | 13.2 ± 1.3 | 559 | 6.0 ± 0.9 | |||
| Hispanic | 299 | 20.9 ± 2.6 | 707 | 9.2 ± 1.3 | 643 | 4.1 ± 0.8 | |||
| Other race/ethnicity | 189 | 25.1 ± 4.2 | 234 | 16.6 ± 3.4 | 224 | 12.2 ± 3.3 | |||
| Education | 0.758 | 0.081 | 0.144 | ||||||
| Less than high school | 221 | 20.8 ± 3.2 | 520 | 11.2 ± 1.6 | 460 | 4.5 ± 1.1 | |||
| High school graduate | 235 | 22.2 ± 2.9 | 563 | 10.6 ± 1.4 | 453 | 4.6 ± 1.4 | |||
| College graduate | 809 | 23.3 ± 1.7 | 1,234 | 14.1 ± 1.1 | 899 | 7.1 ± 1.1 | |||
| Missing | 27 | – | 402 | – | 251 | – | |||
| Poverty | 0.585 | 0.505 | 0.763 | ||||||
| No | 802 | 23.4 ± 1.7 | 1,540 | 12.1 ± 1.1 | 1,094 | 5.5 ± 1.0 | |||
| Yes | 417 | 21.8 ± 2.6 | 995 | 13.3 ± 1.2 | 817 | 6.0 ± 0.9 | |||
| Missing | 73 | – | 184 | – | 152 | – | |||
| Insured | 0.012 | 0.157 | 0.730 | ||||||
| No | 375 | 17.8 ± 2.2 | 1,012 | 11.0 ± 1.0 | 802 | 5.3 ± 1.0 | |||
| Yes | 915 | 24.0 ± 1.6 | 1,700 | 12.8 ± 0.9 | 1,257 | 5.8 ± 0.9 | |||
| Missing | 2 | – | 7 | – | 4 | – | |||
| Foreign born | 0.930 | <0.001 | 0.526 | ||||||
| No | 943 | 22.4 ±1.7 | 2,110 | 13.4 ± 0.9 | 1,441 | 5.4 ± 0.7 | |||
| Yes | 349 | 22.7 ± 2.6 | 609 | 7.5 ± 1.3 | 622 | 6.4 ± 1.4 | |||
| Usual source of care | 0.066 | 0.659 | 0.116 | ||||||
| None | 343 | 17.3 ± 2.7 | 957 | 11.8 ± 1.2 | 710 | 3.9 ± 1.2 | |||
| Hospital or health center | 249 | 26.1 ± 3.3 | 534 | 13.8 ± 1.8 | 438 | 5.7 ± 1.1 | |||
| Private clinic or doctor’s office | 700 | 23.7 ± 1.9 | 1,228 | 12.2 ± 1.2 | 915 | 6.8 ± 1.0 | |||
| Cholesterol | – | 0.188 | 0.734 | ||||||
| Normal | – | – | 1,654 | 11.5 ± 0.9 | 1,316 | 5.3 ± 0.8 | |||
| Borderline hypercholesterolemia | – | – | 647 | 12.6 ± 1.6 | 510 | 6.2 ± 1.3 | |||
| Hypercholesterolemia | – | – | 235 | 16.0 ± 2.4 | 227 | 6.6 ± 1.7 | |||
| Missing | – | – | 183 | – | 10 | – | |||
| Blood pressure | 0.141 | – | 0.035 | ||||||
| Normal | 702 | 21.4 ± 1.9 | – | – | 1,080 | 5.8 ± 1.0 | |||
| Borderline hypertension | 398 | 22.1 ± 2.5 | – | – | 651 | 4.1 ± 0.9 | |||
| Hypertension | 130 | 31.5 ± 4.9 | – | – | 235 | 10.6 ± 2.5 | |||
| Missing | 62 | – | – | – | 97 | – | |||
| Glucose intolerance | 0.434 | 0.069 | – | ||||||
| Normal | 908 | 22.4 ± 1.7 | 1,806 | 11.4 ± 0.9 | – | – | |||
| Borderline diabetes | 334 | 23.7 ± 2.7 | 655 | 13.1 ± 1.6 | – | – | |||
| Diabetes | 50 | 14.9 ± 4.7 | 93 | 24.1 ± 6.3 | – | – | |||
| Missing | 0 | – | 165 | – | – | – | |||
| BMI (kg/m2) | 0.240 | <0.001 | 0.001 | ||||||
| Healthy BMI (<25kg/m2) | 349 | 19.8 ± 2.6 | 842 | 7.3 ± 1.0 | 504 | 5.2 ± 1.5 | |||
| Overweight (25–30kg/m2) | 395 | 21.5 ± 2.4 | 826 | 12.1 ± 1.5 | 600 | 2.5 ± 0.7 | |||
| Obese (>30kg/m2) | 548 | 25.0 ± 2.1 | 1,051 | 16.3 ± 1.6 | 959 | 7.8 ± 1.0 | |||
| Smoking | 0.278 | 0.225 | 0.916 | ||||||
| Never | 812 | 21.0 ± 1.5 | 1,382 | 11.4 ± 1.1 | 1,109 | 6.2 ± 1.0 | |||
| Past | 172 | 26.6 ± 3.4 | 320 | 13.9 ± 2.3 | 241 | 5.6 ± 1.9 | |||
| Current | 308 | 23.7 ± 3.2 | 675 | 14.8 ± 1.6 | 500 | 5.6 ± 1.1 | |||
| Missing | 0 | – | 342 | – | 213 | – | |||
| Family history of cardiovascular disease | 0.017 | 0.062 | 0.022 | ||||||
| No | 1,114 | 21.6 ± 1.5 | 2,030 | 12.2 ± 0.9 | 1,581 | 5.1 ± 0.7 | |||
| Yes | 131 | 32.2 ± 4.2 | 236 | 17.9 ± 2.8 | 187 | 12.1 ± 2.9 | |||
| Missing | 47 | – | 453 | – | 295 | – | |||
All percentages are row percentages.
Appendix Table 2.
Sociodemographic and Clinical Correlates of Cardiovascular Risk Factor Awareness
| Characteristic | Awareness of borderline hypercholesterolemia (n=1,292) | Awareness of borderline hypertension (n=2,719) | Awareness of borderline diabetes (n=2,063) | |||
|---|---|---|---|---|---|---|
| Unadjusted weighted OR (95% CI) | Adjusted weighted OR (95% CI) | Unadjusted weighted OR (95% CI) | Adjusted weighted OR (95% CI) | Unadjusted weighted OR (95% CI) | Adjusted weighted OR (95% CI) | |
| Age | ||||||
| 18–29 years | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| 30–39 years | 1.22 (0.91, 1.64) | 1.63 (1.23, 2.15) | 1.59 (1.19, 2.11) | 2.60 (1.46, 4.63) | 2.53 (1.43, 4.47) | |
| Gender | ||||||
| Male | 1.00 | 1.00 | 1.00 | |||
| Female | 1.04 (0.74, 1.46) | 1.18 (0.86, 1.62) | 2.58 (1.67, 3.98) | |||
| Race/Ethnicity | ||||||
| Non-Hispanic white | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Non-Hispanic black | 0.94 (0.63, 1.41) | 1.06 (0.76, 1.48) | 1.09 (0.78, 1.54) | 1.19 (0.71, 1.99) | 1.27 (0.74, 2.16) | |
| Hispanic | 0.90 (0.59, 1.36) | 0.70 (0.48, 1.04) | 0.91 (0.57, 1.45) | 0.80 (0.44, 1.43) | 0.84 (0.47, 1.53) | |
| Other race/ethnicity | 1.14 (0.69, 1.89) | 1.38 (0.80, 2.38) | 1.89 (1.07, 3.35) | 2.58 (1.26, 5.27) | 2.47 (1.20, 5.11) | |
| Education | ||||||
| Less than high school | 1.00 | 1.00 | 1.00 | 1.00 | ||
| High school graduate | 0.94 (0.61, 1.44) | 0.97 (0.64, 1.47) | 1.38 (0.94, 2.04) | 1.18 (0.68, 2.06) | ||
| College graduate | 1.48 (0.99, 2.19) | 1.53 (1.05, 2.24) | 1.24 (0.86, 1.79) | 193 (1.02, 3.65) | ||
| Poverty | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 0.90 (0.64, 1.26) | 1.03 (0.75, 1.41) | 1.12 (0.66, 1.91) | |||
| Insured | ||||||
| No | 1.00 | 1.00 | 1.00 | |||
| Yes | 1.45 (1.07, 1.99) | 1.16 (0.91, 1.48) | 1.12 (0.67, 1.88) | |||
| Foreign born | ||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Yes | 1.02 (0.70, 1.48) | 0.53 (0.35, 0.79) | 0.49 (0.30, 0.81) | 1.19 (0.70, 2.01) | ||
| Usual source of care | ||||||
| None | 1.00 | 1.00 | 1.00 | |||
| Hospital or health center | 1.68 (1.00, 2.84) | 1.20 (0.81, 1.79) | 1.49 (0.69, 3.24) | |||
| Private clinic or doctor’s office | 1.48 (1.02, 2.15) | 1.04 (0.76, 1.42) | 1.81 (0.89, 3.68) | |||
| Cholesterol | ||||||
| Normal | – | 1.00 | 1.00 | |||
| Borderline hypercholesterolemia | – | 1.08 (0.79, 1.49) | 1.17 (0.67, 2.03) | |||
| Hypercholesterolemia | – | 1.55 (1.05, 2.29) | 1.27 (0.67, 2.39) | |||
| Blood pressure | ||||||
| Normal | 1.00 | – | 1.00 | |||
| Borderline hypertension | 1.09 (0.76, 1.59) | – | 0.69 (0.39, 1.24) | |||
| Hypertension | 1.71 (1.04, 2.83) | – | 1.93 (1.02, 3.66) | |||
| Glucose intolerance | ||||||
| Normal | 1.00 | 1.00 | – | |||
| Borderline diabetes | 1.08 (0.78, 1.48) | 1.10 (0.81, 1.49) | – | |||
| Diabetes | 0.60 (0.27, 1.33) | 2.28 (1.14, 4.56) | – | |||
| BMI (kg/m2) | ||||||
| Healthy BMI (<25kg/m2) | 1.00 | 1.00 | 1.00 | 1.00 | ||
| Overweight (25–30kg/m2) | 1.11 (0.73, 1.69) | 1.75 (1.19, 2.58) | 1.73 (1.17, 2.55) | 0.47 (0.21, 1.08) | ||
| Obese (>30kg/m2) | 1.35 (0.94, 1.95) | 2.47 (1.63, 3.74) | 2.34 (1.53, 3.58) | 1.54 (0.79, 3.02) | ||
| Smoking | ||||||
| Never | 1.00 | 1.00 | 1.00 | |||
| Past | 1.36 (0.94, 1.98) | 1.24 (0.81, 1.90) | 0.89 (0.39, 2.01) | |||
| Current | 1.17 (0.80, 1.70) | 1.31 (0.91, 1.88) | 0.88 (0.52, 1.48) | |||
| Family history of cardiovascular disease | ||||||
| No | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Yes | 1.69 (1.12, 2.55) | 1.74 (1.15, 2.62) | 1.51 (1.01, 2.28) | 2.42 (1.31, 4.46) | 2.31 (1.26, 4.23) | |
Notes: Multivariate models used a backwards elimination approach evaluating changes in likelihood ratios. Final model included only those variables associated (p<0.10) with risk factor awareness. Variables that were not included in the multivariate model are left blank.
DISCUSSION
Despite the high prevalence of cardiovascular risk factors in this nationally representative sample of U.S. young adults, risk factor awareness remained less than ideal. Approximately 30% of young adults with diabetes, 37% with hypertension, and 43% with hypercholesterolemia were unaware of their condition. Awareness was substantially lower in young adults with borderline levels of these risk factors; more than 75% of young adults with borderline hypercholesterolemia, hypertension, and diabetes were unaware that they were at risk. Although predictors of awareness varied across risk factors, young adults with younger age, no insurance, or without a usual source of care were, in general, less likely to be aware of their risk factors. These findings suggest that targeting interventions to screen and raise awareness among these individuals may facilitate achieving treatment goals in this young adult population.
These findings are consistent with prior NHANES studies in older adult populations demonstrating suboptimal hypercholesterolemia, hypertension, and diabetes awareness. These studies have reported the prevalence of undiagnosed hypercholesterolemia, hypertension, and diabetes to be as high as 65%, 28%–31%, and 30%, respectively.19,23,24,33 Estimates of hypercholesterolemia awareness in this study were comparable to those in prior studies,33 but the prevalence of hypertension and diabetes awareness was higher possibly due to the use of more contemporary data or greater insurance coverage under the Affordable Care Act.19,33 Other studies using NHANES data have also explored predictors of risk factor awareness in older populations but only examined a few demographic characteristics.22,26 The current study extends these findings to a contemporary population of U.S. young adults, for whom risk factor awareness is critical to the prevention of future CHD, and examines a wide range of both sociodemographic and clinical correlates of awareness among individuals with both borderline and high levels of cardiovascular risk factors.
Individuals without insurance and without a usual source of care were more likely to be unaware of their risk factors. In fact, these variables were more consistent predictors of unawareness than most of the clinical variables examined. This observation is particularly concerning given prior reports showing higher cardiovascular morbidity and mortality in poor and less educated patients34–36 and lower treatment rates for coronary artery disease among the uninsured.37,38 Not surprisingly, prior studies have also found lower rates of treatment and control for hypercholesterolemia, hypertension, and diabetes among poor and uninsured patients.39 Despite racial/ethnic differences in the prevalence of cardiovascular risk factors in the general population, there were no differences in awareness of hypercholesterolemia or hypertension by race/ethnicity in multivariable analyses. The absence of an association is likely because of the inclusion of other variables, such as healthcare access and insurance, in the models. Only diabetes awareness differed by race/ethnicity with lower awareness among non-Hispanic and Hispanic adults. These data demonstrate the need for increased risk factor screening and education efforts among low-income and underinsured young adults and the urgency of such efforts in a time of healthcare reform.
Interestingly, the presence of multiple cardiovascular risk factors augmented awareness only moderately. Among young adults with more than one risk factor, 26%, 27%, and 23% were unaware of having hypercholesterolemia, hypertension, and diabetes, respectively. In multivariable models, comorbid diabetes was a significant correlate of both hypercholesterolemia and hypertension awareness possibly because the American Diabetes Association has been advising clinicians to identify and treat additional cardiovascular risk factors in patients with diabetes for decades.40 Neither hypercholesterolemia, hypertension, obesity, nor family history of early cardiovascular disease emerged as significant predictors of awareness for any risk factor, and smoking was only associated with hypertension awareness. This observation may be because of the fact that greater cardiovascular risk factor clustering tends to occur in Americans with low SES, which may prevent many individuals from obtaining screening or counseling for these risk factors.41 The association of smoking with increased hypertension awareness may be because of more targeted screening and education of smokers by clinicians given their elevated risk of cardiovascular disease.
This study also found very low awareness in individuals with borderline levels of these risk factors. Only 22%, 12%, and 6% of young adults with borderline hypercholesterolemia, hypertension, and diabetes, respectively, recalled having ever been told that they were at risk of these conditions. This low prevalence is especially concerning given the high prevalence of borderline risk factors in the young adult population and the likelihood that these individuals will go on to develop hypercholesterolemia, hypertension, and diabetes in the future if no intervention occurs. As the prevalence of cardiovascular disease continues to climb, there is an even greater imperative to focus on prevention earlier in life, particularly among those with borderline risk factors. Data from the Coronary Artery Risk Development in Young Adults study demonstrated that individuals with risk factors above optimal levels were two- to three-fold more likely to have subclinical atherosclerosis,4 and individuals who develop cardiovascular risk factors early in life are more likely to have a persistence of these factors into older adulthood.6–8 Early education and lifestyle modifications have been shown to reduce the development of these risk factors42–46; however, these interventions are contingent upon effectively screening and diagnosing these at-risk populations. Young adults with borderline risk factor levels are precisely the population who might benefit from simple inexpensive interventions to prevent the development of these risk factors and their sequelae.
Taken together, this study’s findings suggest that targeting educational and screening interventions at young adults with barriers to care may lower the prevalence of undiagnosed cardiovascular risk factors and improve treatment goals in this population. Unrecognized cardiovascular risk factors place individuals at risk for developing CHD and stroke later in life, in addition to being costly and disabling diseases in and of themselves. These findings are particularly timely given recent changes in the hypertension guidelines now defining hypertension as blood pressure greater than 130/80 mmHg, which is estimated to expand the percentage of young adults with hypertension from 11% to 30% in men and 10% to 19% in women.47
Recent guidelines recommend universal screening for cholesterol and blood pressure in all children between the ages of 17–21 years, which may improve diagnosis and identification of at risk youth.13,14 However, adherence to these guidelines amongst pediatricians is low,48 and many youth are lost to follow-up as they transition from pediatric to adult-centered care.49 Therefore, these guidelines are not likely to benefit adolescents or young adults with limited access to care who are most likely to be unaware of their risk factors. At present, the U.S. Preventive Services Task Force recommends selective cholesterol and diabetes screening for men and women at increased risk of CHD but does not advise routine cholesterol screening until age 35 years in men and age 45 years in women. Given the high prevalence of borderline and high cholesterol in young adults coupled with the low awareness of these risk factors observed in this study, more liberal screening of cholesterol may be warranted particularly in adults with interrupted access to care who may have infrequent opportunities for screening. Although the U.S. Preventive Services Task Force does recommend routine screening for hypertension in young adults, individuals with limited access to care are unlikely to benefit from these recommendations. As such, this study highlights the importance of community outreach efforts, such as mobile screening units.
Limitations
This study has its limitations. First, as with any self-reported questionnaire, participant answers may be subject to imperfect recall or social desirability bias. Second, data on cholesterol awareness was missing in approximately 34% of participants with high or borderline cholesterol. Compared with participants with recorded awareness data, participants with missing data were younger and more likely to be uninsured and lack a usual source of care. Therefore, cholesterol awareness may be even lower than those reported in this study. Third, NHANES uses three repeated measures on a single day (rather than multiple days) to diagnose hypertension. Although this is not the standard in clinical practice, the Centers for Disease Control and Prevention and multiple other studies have used these data to estimate the prevalence of hypertension.19,22 Similarly, the use of a single fasting glucose test and HbA1c to diagnose diabetes is not typically used in clinical practice; however, this method has also been used to estimate the population prevalence of both Type 1 and Type 2 diabetes.23,26 Fourth, information on health literacy or knowledge of cardiovascular disease was not available and may be important contributors to risk factor awareness. Fifth, participant access to care was evaluated at a single timepoint, when, in fact, many people routinely cycle in and out of coverage or between providers. Sixth, it was not possible to differentiate between Type 1 and Type 2 diabetes given the absence of laboratory data such as C-peptide levels or insulin antibody testing; however, both Type 1 and Type 2 diabetes confer an elevated risk of cardiovascular disease and mortality. Finally, lack of awareness could be a result of not having been screened, or alternatively, not receiving, or not understanding abnormal results. Because clinicians often use a risk score approach to evaluate patient risk, some participants may be aware that they are at increased risk of cardiovascular disease but unaware of individual cardiovascular risk factors.
CONCLUSIONS
Awareness of hypercholesterolemia, hypertension, and diabetes is suboptimal in U.S. young adults. Young adults with barriers to health care such as lack of insurance and no usual source of care were more likely to be unaware of their CHD risk factors. Future studies are needed to better understand impediments to awareness about CHD risk factors among young adults, and to develop and evaluate interventions that target screening in young adults with limited access to care. In the meantime, clinicians should continue to improve patient education around the risks and consequences of borderline and elevated levels of cardiovascular risk factors.
Acknowledgments
Dr. Emily Bucholz conceived of the study including the design, drafted the manuscript, had full access to all the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Gooding made substantive contributions to the interpretation of data, revised it critically for important intellectual content, and gave final approval of the manuscript. Dr. de Ferranti made substantive contributions to the conception, design, and interpretation of data; revised it critically for important intellectual content; and gave final approval of the manuscript.
HCG is supported by the National Heart, Lung, and Blood Institute of NIH (K23HL122361-01A1). SDD receives royalties from UpToDate for topics related to pediatric and adolescent preventive cardiology, and research funding from the Pediatric Heart Network. No other financial disclosures were reported by the authors of this paper.
References
- 1.Berenson GS, Srinivasan SR, Bao W, Newman WP, 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. N Engl J Med. 1998;338(23):1650–1656. doi: 10.1056/NEJM199806043382302. https://doi.org/10.1056/NEJM199806043382302. [DOI] [PubMed] [Google Scholar]
- 2.Berenson GS, Wattigney WA, Tracy RE, et al. Atherosclerosis of the aorta and coronary arteries and cardiovascular risk factors in persons aged 6 to 30 years and studied at necropsy (The Bogalusa Heart Study) Am J Cardiol. 1992;70(9):851–858. doi: 10.1016/0002-9149(92)90726-f. https://doi.org/10.1016/0002-9149(92)90726-F. [DOI] [PubMed] [Google Scholar]
- 3.Li S, Chen W, Srinivasan SR, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa Heart Study. JAMA. 2003;290(17):2271–2276. doi: 10.1001/jama.290.17.2271. https://doi.org/10.1001/jama.290.17.2271. [DOI] [PubMed] [Google Scholar]
- 4.Loria CM, Liu K, Lewis CE, et al. Early adult risk factor levels and subsequent coronary artery calcification: the CARDIA Study. J Am Coll Cardiol. 2007;49(20):2013–2020. doi: 10.1016/j.jacc.2007.03.009. https://doi.org/10.1016/j.jacc.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 5.McGill HC, Jr, McMahan CA, Gidding SS. Preventing heart disease in the 21st century: implications of the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study. Circulation. 2008;117(9):1216–1227. doi: 10.1161/CIRCULATIONAHA.107.717033. https://doi.org/10.1161/CIRCULATIONAHA.107.717033. [DOI] [PubMed] [Google Scholar]
- 6.Navar-Boggan AM, Peterson ED, D’Agostino RB, Sr, Neely B, Sniderman AD, Pencina MJ. Hyperlipidemia in early adulthood increases long-term risk of coronary heart disease. Circulation. 2015;131(5):451–458. doi: 10.1161/CIRCULATIONAHA.114.012477. https://doi.org/10.1161/CIRCULATIONAHA.114.012477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pletcher MJ, Bibbins-Domingo K, Liu K, et al. Nonoptimal lipids commonly present in young adults and coronary calcium later in life: the CARDIA study. Ann Intern Med. 2010;153(3):137–146. doi: 10.1059/0003-4819-153-3-201008030-00004. https://doi.org/10.7326/0003-4819-153-3-201008030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pletcher MJ, Vittinghoff E, Thanataveerat A, Bibbins-Domingo K, Moran AE. Young adult exposure to cardiovascular risk factors and risk of events later in life: the Framingham Offspring Study. PloS One. 2016;11:e0154288. doi: 10.1371/journal.pone.0154288. https://doi.org/10.1371/journal.pone.0154288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raynor LA, Schreiner PJ, Loria CM, Carr JJ, Pletcher MJ, Shikany JM. Associations of retrospective and concurrent lipid levels with subclinical atherosclerosis prediction after 20 years of follow-up: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Ann Epidemiol. 2013;23(8):492–497. doi: 10.1016/j.annepidem.2013.06.003. https://doi.org/10.1016/j.annepidem.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stamler J, Stamler R, Neaton JD, et al. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA. 1999;282(21):2012–2018. doi: 10.1001/jama.282.21.2012. https://doi.org/10.1001/jama.282.21.2012. [DOI] [PubMed] [Google Scholar]
- 11.Stamler J, Dyer AR, Shekelle RB, Neaton J, Stamler R. Relationship of baseline major risk factors to coronary and all-cause mortality, and to longevity: findings from long-term follow-up of Chicago cohorts. Cardiology. 1993;82(2–3):191–222. doi: 10.1159/000175868. https://doi.org/10.1159/000175868. [DOI] [PubMed] [Google Scholar]
- 12.Burke GL, Arnold AM, Bild DE, et al. Factors associated with healthy aging: the cardiovascular health study. J Am Geriatr Soc. 2001;49(3):254–262. doi: 10.1046/j.1532-5415.2001.4930254.x. https://doi.org/10.1046/j.1532-5415.2001.4930254.x. [DOI] [PubMed] [Google Scholar]
- 13.Integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Bethesda, MD: National Heart, Lung, and Blood Institute; 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(suppl 5):S213–256. doi: 10.1542/peds.2009-2107C. https://doi.org/10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin KW, Brown TR. Screening for lipid disorders in adults. Am Fam Physician. 2009;80(11):1281–1282. [PubMed] [Google Scholar]
- 16.U.S. Preventive Services Task Force. Final update summary: lipid disorders in adults (cholesterol, dyslipidemia): screening. Published 2008. [Google Scholar]
- 17.Casagrande SS, Menke A, Cowie CC. Cardiovascular risk factors of adults age 20–49 years in the United States, 1971–2012: a series of cross-sectional studies. PloS One. 2016;11:e0161770. doi: 10.1371/journal.pone.0161770. https://doi.org/10.1371/journal.pone.0161770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheung BM, Ong KL, Man YB, Lam KS, Lau CP. Prevalence, awareness, treatment, and control of hypertension: United States National Health and Nutrition Examination Survey 2001–2002. J Clin Hypertension. 2006;8(2):93–98. doi: 10.1111/j.1524-6175.2006.04895.x. https://doi.org/10.1111/j.1524-6175.2006.04895.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52(5):818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. https://doi.org/10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 20.Kuklina EV, Yoon PW, Keenan NL. Prevalence of coronary heart disease risk factors and screening for high cholesterol levels among young adults, United States, 1999–2006. Ann Fam Med. 2010;8(4):327–333. doi: 10.1370/afm.1137. https://doi.org/10.1370/afm.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49(1):69–75. doi: 10.1161/01.HYP.0000252676.46043.18. https://doi.org/10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 22.Ayanian JZ, Zaslavsky AM, Weissman JS, Schneider EC, Ginsburg JA. Undiagnosed hypertension and hypercholesterolemia among uninsured and insured adults in the Third National Health and Nutrition Examination Survey. Am J Public Health. 2003;93(12):2051–2054. doi: 10.2105/ajph.93.12.2051. https://doi.org/10.2105/AJPH.93.12.2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999–2002. Diabetes Care. 2006;29(6):1263–1268. doi: 10.2337/dc06-0062. https://doi.org/10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 24.Ford ES, Mokdad AH, Giles WH, Mensah GA. Serum total cholesterol concentrations and awareness, treatment, and control of hypercholesterolemia among U.S. adults: findings from the National Health and Nutrition Examination Survey, 1999 to 2000. Circulation. 2003;107(17):2185–2189. doi: 10.1161/01.CIR.0000066320.27195.B4. https://doi.org/10.1161/01.CIR.0000066320.27195.B4. [DOI] [PubMed] [Google Scholar]
- 25.Gooding HC, McGinty S, Richmond TK, Gillman MW, Field AE. Hypertension awareness and control among young adults in the national longitudinal study of adolescent health. J Gen Intern Med. 2014;29(8):1098–1104. doi: 10.1007/s11606-014-2809-x. https://doi.org/10.1007/s11606-014-2809-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McDonald M, Hertz RP, Unger AN, Lustik MB. Prevalence, awareness, and management of hypertension, dyslipidemia, and diabetes among United States adults aged 65 and older. J Gerontol. 2009;64(2):256–263. doi: 10.1093/gerona/gln016. https://doi.org/10.1093/gerona/gln016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Muntner P, Levitan EB, Brown TM, et al. Trends in the prevalence, awareness, treatment and control of high low density lipoprotein-cholesterol among United States adults from 1999–2000 through 2009–2010. Am J Cardiol. 2013;112(5):664–670. doi: 10.1016/j.amjcard.2013.04.041. https://doi.org/10.1016/j.amjcard.2013.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(25 suppl 2):S1–45. doi: 10.1161/01.cir.0000437738.63853.7a. https://doi.org/10.1161/01.cir.0000437738.63853.7a. [DOI] [PubMed] [Google Scholar]
- 29.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. https://doi.org/10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown TM, Tanner RM, Carson AP, et al. Awareness, treatment, and control of LDL cholesterol are lower among U.S. adults with undiagnosed diabetes versus diagnosed diabetes. Diabetes Care. 2013;36(9):2734–2740. doi: 10.2337/dc12-2318. https://doi.org/10.2337/dc12-2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Medicaid and CHIP eligibility levels. [Accessed February 24, 2017];Medicaid.gov. www.medicaid.gov/medicaid/program-information/medicaid-and-chip-eligibility-levels/index.html. Published 2016.
- 32.Johnson CL, Paulose-Ram R, Ogden CL, et al. National Health and Nutrition Examination Survey: analytic guidelines, 1999–2010. Vital Health Stat 2. 2013;161:1–24. [PubMed] [Google Scholar]
- 33.Christian JB, Bourgeois NE, Lowe KA. Cholesterol screening in U.S. adults and awareness of high cholesterol among individuals with severe hypertriglyceridemia: National Health and Nutrition Examination Survey 2001–2008. J Cardiovasc Nurs. 2015;30(1):26–34. doi: 10.1097/JCN.0000000000000101. https://doi.org/10.1097/JCN.0000000000000101. [DOI] [PubMed] [Google Scholar]
- 34.Fowler-Brown A, Corbie-Smith G, Garrett J, Lurie N. Risk of cardiovascular events and death–does insurance matter? J Gen Intern Med. 2007;22(4):502–507. doi: 10.1007/s11606-007-0127-2. https://doi.org/10.1007/s11606-007-0127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4):1973–1998. doi: 10.1161/01.cir.88.4.1973. https://doi.org/10.1161/01.CIR.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 36.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. https://doi.org/10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 37.Arnold SV, Spertus JA, Tang F, et al. Statin use in outpatients with obstructive coronary artery disease. Circulation. 2011;124(22):2405–2410. doi: 10.1161/CIRCULATIONAHA.111.038265. https://doi.org/10.1161/CIRCULATIONAHA.111.038265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Smolderen KG, Spertus JA, Tang F, et al. Treatment differences by health insurance among outpatients with coronary artery disease: insights from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2013;61(10):1069–1075. doi: 10.1016/j.jacc.2012.11.058. https://doi.org/10.1016/j.jacc.2012.11.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brooks EL, Preis SR, Hwang SJ, et al. Health insurance and cardiovascular disease risk factors. Am J Med. 2010;123(8):741–747. doi: 10.1016/j.amjmed.2010.02.013. https://doi.org/10.1016/j.amjmed.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.American Diabetes Association. 8. Cardiovascular disease and risk management. Diabetes Care. 2015;38(suppl 1):S49–57. doi: 10.2337/dc15-S011. https://doi.org/10.2337/dc15-S011. [DOI] [PubMed] [Google Scholar]
- 41.Sharma S, Malarcher AM, Giles WH, Myers G. Racial, ethnic, and socioeconomic disparities in the clustering of cardiovascular risk factors. Ethn Dis. 2004;14(1):43–48. [PubMed] [Google Scholar]
- 42.Elmer PJ, Grimm R, Jr, Laing B, et al. Lifestyle intervention: results of the Treatment of Mild Hypertension Study (TOMHS) Prev Med. 1995;24(4):378–388. doi: 10.1006/pmed.1995.1062. https://doi.org/10.1006/pmed.1995.1062. [DOI] [PubMed] [Google Scholar]
- 43.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. https://doi.org/10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344(1):3–10. doi: 10.1056/NEJM200101043440101. https://doi.org/10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 45.Tuomilehto J, Lindstrom J, Eriksson JG, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344(18):1343–1350. doi: 10.1056/NEJM200105033441801. https://doi.org/10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 46.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136(7):493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. https://doi.org/10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 47.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Hypertension. 2018;71(1):1–481. https://doi.org/10.1161/HYP.0000000000000065. [Google Scholar]
- 48.Vinci SR, Rifas-Shiman SL, Cheng JK, Mannix RC, Gillman MW, de Ferranti SD. Cholesterol testing among children and adolescents during health visits. JAMA. 2014;311(17):1804–1807. doi: 10.1001/jama.2014.2410. https://doi.org/10.1001/jama.2014.2410. [DOI] [PubMed] [Google Scholar]
- 49.Fortuna RJ, Robbins BW, Halterman JS. Ambulatory care among young adults in the United States. Ann Intern Med. 2009;151(6):379–385. doi: 10.7326/0003-4819-151-6-200909150-00002. https://doi.org/10.7326/0003-4819-151-6-200909150-00002. [DOI] [PubMed] [Google Scholar]