ABSTRACT
OBJECTIVE
To compare cancer hospital morbidity among the local population and the immigrant population in Chile.
METHODS
This is a prevalence study based on the analysis of hospital discharges of all the health centers of Chile. Cancer hospital discharges were characterized in 2012 according to the migratory status. The crude and specific rates of hospital morbidity for this cause were estimated for the analysis of their association with migratory status using zero-inflated negative binomial regression, adjusted for sociodemographic variables.
RESULTS
The neoplasms were the third cause of hospital discharges for immigrants and the seventh one for Chileans. The adjusted rate of cancer hospital discharges was higher for Chileans than immigrants, and the latter had fewer days of hospitalization and greater proportion of surgical interventions. In the group of immigrants, cancer hospital discharges mainly corresponded to patients belonging to the private system (46%), and in the group of Chileans they mainly corresponded to patients in the public system (71.1%). We observed a large difference in the proportion of cancer hospital discharges for patients with no health insurance between the two populations (22.6%: immigrants, 1.0%: Chileans). In both populations, the three most frequent types of cancer were: (i) lymphoid tissue, hematopoietic organs, and related tissues, (ii) digestive organs, and (iii) breast cancer.
CONCLUSIONS
Models of differentiated care should be considered for immigrants, with the creation of specific programs of information, coverage, and protection against cancer. More information on this problem must be generated at the local and international level.
Keywords: Emigrants and Immigrants, Neoplasms, epidemiology; Hospitalization; Health Services Accessibility; Socioeconomic Factors; Health Inequalities; Latin America
RESUMEN
OBJETIVO
Comparar la morbilidad hospitalaria por cáncer entre población local e inmigrante en Chile.
MÉTODOS
Estudio de prevalencia basado en el análisis de egresos hospitalarios de todos los centros de Chile. Se caracterizaron los egresos hospitalarios por cáncer en 2012 según condición migratoria. Se estimaran las tasas brutas y específicas de morbilidad hospitalaria por esta causa, para finalmente analizar su asociación con el estatus migratorio mediante una regresión binomial negativa inflada por ceros ajustada por variables sociodemográficas.
RESULTADOS
Las neoplasias fueron la tercera causa de egresos hospitalarios en inmigrantes y la séptima en chilenos. La tasa ajustada de egresos hospitalarios por cáncer fue mayor en chilenos que en inmigrantes, y estos presentaron menor cantidad de días de hospitalización y mayor proporción de intervenciones quirúrgicas. En el grupo de inmigrantes, los egresos hospitalarios por cáncer corresponderán principalmente a pacientes pertenecientes al sistema privado (46%) y en chilenos a pacientes en el sistema público (71,1%). Se observó una amplia diferencia en la proporción de egresos hospitalarios por cáncer correspondientes a pacientes sin previsión de salud entre ambas poblaciones (22,6%: inmigrantes, 1,0%: chilenos). En ambas poblaciones, los tres cánceres que se presentaron con mayor frecuencia fueron: (i) tejidos linfáticos, órganos hematopoyéticos y tejidos afines, (ii) órganos digestivos y (iii) cáncer de mama.
CONCLUSIONES
Se deben considerar modelos de atención diferenciada en inmigrantes, creando programas específicos de información, cobertura y protección frente al cáncer. Es necesario generar más información sobre esta problemática a nivel local e internacional.
Keywords: Emigrantes e Inmigrantes; Neoplasias, epidemiología; Hospitalización; Accesibilidad a los Servicios de Salud; Factores Socioeconómicos; Desigualdades en la Salud; América Latina
INTRODUCTION
Globally, close to 200 million persons live in a place different from where they were born 1 . In Latin America, it was estimated that approximately 4.0% of the population lived in a country other than that of origin in 2011 2 . The immigrant population usually presents a population structure, in sex, age, and other factors, that is different from the local population 3 .
For all the changes that the migratory process implies both for the individuals, by modifying their conditions and lifestyles, and for the population, given the patterns of infectious and chronic diseases that individuals bring with them, international migration has the potential to generate high impact on public health 4 . In Chile 3 and in the world 5 international migration has been recognized as a valuable indicator of vulnerability and social inequality in health between and within countries3–5.
International migration itself does not necessarily pose a threat to mental and general health. Its association with factors such as cultural barriers, difficulty of access and use of health services, conditions of the country of origin, residence time, and social, economic, labor, and educational factors 6 , 7 , among others, determines the individual and family well-being of the immigrant. It is in relation to these factors that it becomes important to link the evidence on international migration, health, and social vulnerability. Similarly, it is important to analyze the health and use of services by this population for all levels of health care. Immigrants can report different expectations, problems, and needs related to health care 8 . The international literature shows that: (i) there is insufficient use of health services by immigrants compared to the local population in some countries, (ii) in general, most immigrants use public health services 9 , and (iii) secondary care services are used by immigrants in some countries, in some cases without even having used the primary level, with the problem that they have a limited role in the provision of services 7 .
It is thus that diseases, for which secondary prevention and adequate treatment can be determinant to reduce their incidence and mortality, become a focus of special care for immigrants. Cancer fulfills these characteristics 10 and is a global public health problem because of its high therapeutic cost and high burden as a disease 11 . In the Americas, 2.8 million new cases were registered in 2012, of which approximately 47% occurred in Latin America and the Caribbean 12 .
Cancer is a health priority in Chile, presenting high prevalence, mortality, and heterogeneity throughout the country 13 . Although it has been studied extensively for the local population 14 , the information on cancer in immigrants in the country is scarce 10 . The distribution of cancer prevalence, risk, and mortality differs between local and immigrant population and according to the characteristics of these populations in each country. In Italy, the risk of colorectal 15 or cervical cancer 16 is higher in the immigrant population compared to the local population. On the other hand, no differences have been observed in Denmark between the local and foreign population in cancer mortality 17 . In Spain, local women had higher rates of detection of cervical cancer than immigrants 10 , and the latter were less likely to undergo gynecological cancer screening 18 .
In Italy, despite the total hospitalization rates being higher for the local population than the immigrant population, it was the latter one that presented a higher rate of cervical cancer and a lower rate of mastectomies 19 . Often, cancer is not the leading cause of death in international migrants. However, in countries such as Sweden, cancer is the third cause of death in this population 20 , highlighting the importance of studying this phenomenon globally and in countries with a high health burden for this disease.
The objective of this study was to compare cancer hospital morbidity among the local population and immigrant population in Chile. We aimed to contribute with current national and international knowledge on the health of the immigrant population, especially focusing on hospitalizations for cancer.
METHODS
This is a prevalence study based on the analysis of secondary data from hospital discharges of all public and private centers in Chile, compiled by the Department of Health Statistics and Information (DEIS) of the Ministry of Health of Chile, in 2012. This year was the first time when information on the nationality of the subject treated at the hospitals was registered. For the purposes of this study, we considered as synonyms the concepts of foreign population (nationality other than Chilean) and immigrants or international migrants. Cancer hospital discharges (CHD) were characterized in 2012 according to migratory status. We studied the crude and specific rates of hospital morbidity for this cause to analyze the association between them and migratory status (Chilean or immigrant). The analysis of hospital discharges provides information on both morbidity and health care services, according to the pathology explored 19 . The information obtained from them represents a strong indicator of morbidity of a country, even if we exclude the discharges for obstetric causes. Therefore, their analysis allows knowing and adjusting the health services to the needs of different subgroups of the population (in this case, the immigrant population) at the primary and secondary level 21 .
The database of hospital discharges in Chile in 2012 contains: (i) demographic characteristics (sex, age, nationality, place of residence), (ii) health insurance (public, private, none, others), and (iii) characteristics of the hospitalization, such as diagnosis (coded according to ICD-10), condition of the discharges (discharge or death), surgical intervention (yes, no), days of hospitalization, date, and information on the center where the hospital discharge occurred. We estimated the absolute numbers and those relative to migratory status from the characteristics mentioned above in hospital discharges, whose main diagnosis corresponded to the codes C00-D09 (in situ and malignant neoplasms) of ICD-10.
The specific rates of cancer hospital morbidity (CHM) were amplified by 100,000 and were calculated as the ratio between the number of hospital discharges per in situ and malignant neoplasms in the subgroups of: migratory status, age, sex, and type of health insurance, in 2012 (numerator), and total population in the same subgroup for the same period (denominator). The number of hospital discharges was obtained using its homonymous database and the denominators of the population database, that is, the total population by subgroup, from the average of the estimates of population obtained using the studies of national socioeconomic characterization (CASEN) in the 2011 and 2013 versions. Both versions of the research use a complex sampling, which was considered for the estimates and which are representative of the residents in private households in the fifteen regions of the country excluding areas of difficult access and institutionalized persons 22 .
The association between cancer hospital morbidity and migratory status was analyzed using an explanatory model of zero-inflated negative binomial regression (ZINB). In this model, the count values are generated from a negative binomial model and the excess zeros come from a binary model. It is suitable for situations that have excess zeros and dispersion, in addition to the assumption that the event is not impossible in any of the populations under study or in their subgroups 23 , as is the case with CHD.
The main dependent variable for this analysis was the specific rate of cancer hospital morbidity and the main independent variable was the migratory status. Based on the literature and availability, we considered the confounding variables: sex, age, health insurance, and the interaction between the variables of migratory status and health insurance, resulting in a model as: λ
log (λ) ~ log (p) + migratory status + sex + age + age2 + insurance + migratory status insurance
logit (π) = log (1/1-π) ~ migratory status + age + sex + health insurance
Where corresponds to the number of hospital discharges in the subgroup, corresponds to the logarithm of the total population of the country in the subgroup (offset), and corresponds to the probability of observing excess zero. The fit tests of the model were corroborated.
RESULTS
Approximately 74,282 CHD happened in Chile in 2012, which is equivalent to 4.5% of the total HD of the country in the period. Of these, 0.7% corresponded to the immigrant population. Neoplasms (C00-D48 of ICD-10) corresponded to the third most common cause of hospital discharges in immigrants; on the other hand, neoplasms corresponded to the seventh most common cause in the local population, according to the large chapters of causes of the ICD-10.
The three most common causes of CHD in both the local and immigrant population were malignant neoplasms of: (i) digestive organs (22.9% total: 18.5% immigrants, 22.9% Chileans, codes C15-C26 of ICD-10), (ii) lymphoid tissue, hematopoietic organs, and related tissues (17.4% total: 17.7% immigrants, 17.4% Chileans, codes C81-C96 of ICD-10), and (iii) breast (10.3% total: 16.7% immigrants, 10.3% Chileans, code C50 of ICD-10) (Table 1).
Table 1. Hospital profile of patients who were discharged because of cancer (C00-D09 of ICD-10), according to migratory status. Chile, 2012.
| Hospital characteristics | Chilean (n = 74,382) | Immigrant (n = 486) | Total (n = 74,868) | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n | % | n | % | n | % | |
| Type of cancer | ||||||
| Digestive organs | 17,042 | 22.9 | 90 | 18.5 | 17,132 | 22.9 |
| Lymphoid tissue, hematopoietic organs, and related tissues | 12,904 | 17.4 | 86 | 17.7 | 12,990 | 17.4 |
| Breast | 7,647 | 10.3 | 81 | 16.7 | 7,728 | 10.3 |
| Female genital organs | 6,289 | 8.5 | 36 | 7.4 | 6,325 | 8.4 |
| Ill-defined, other secondary, and unspecified sites | 3,655 | 4.9 | 35 | 7.2 | 3,690 | 4.9 |
| Respiratory and intrathoracic organs | 3,789 | 5.1 | 34 | 7.0 | 3,823 | 5.1 |
| In situ | 3,029 | 4.1 | 31 | 6.4 | 3,060 | 4.1 |
| Thyroid gland and other endocrine glands | 3,789 | 5.1 | 22 | 4.5 | 3,811 | 5.1 |
| Male genital organs | 5,694 | 7.7 | 17 | 3.5 | 5,711 | 7.6 |
| Lips, oral cavity, and pharynx | 995 | 1.3 | 16 | 3.3 | 1,011 | 1.4 |
| Melanoma and other malignant neoplasms of skin | 2,052 | 2.8 | 14 | 2.9 | 2,066 | 2.8 |
| Urinary tract | 3,068 | 4.1 | 12 | 2.5 | 3,080 | 4.1 |
| Eye, brain, and other parts of central nervous system | 2,049 | 2.8 | 8 | 1.6 | 2,057 | 2.7 |
| Mesothelial and soft tissue | 1,129 | 1.5 | 3 | 0.6 | 1,132 | 1.5 |
| Bone and articular cartilage | 1,005 | 1.4 | 1 | 0.2 | 1,006 | 1.3 |
| Malignant neoplasms of independent (primary) multiple sites | 146 | 0.2 | 0 | 0 | 146 | 0.2 |
| Discharge condition | ||||||
| Alive | 70,446 | 94.8 | 474 | 97.5 | 70,920 | 94.9 |
| Deceased | 3,836 | 5.2 | 12 | 2.5 | 3,848 | 5.1 |
| Surgical intervention | ||||||
| Yes | 30,022 | 40.4 | 210 | 43.2 | 30,232 | 40.4 |
| No | 44,260 | 59.6 | 276 | 56.8 | 44,536 | 59.6 |
| Days of hospitalization | ||||||
| 1 day | 19,202 | 25.8 | 183 | 37.7 | 19,385 | 25.9 |
| 2 days | 10,441 | 14.0 | 89 | 18.3 | 10,530 | 14.1 |
| 3 days | 7,473 | 10.0 | 55 | 11.3 | 7,528 | 10.1 |
| 4 or more days | 37,266 | 50.1 | 159 | 32.7 | 37,425 | 50.0 |
| Average (standard deviation) | 7.5 (12.3) | 5.9 (15.3) | 7.5 (12.4) | |||
| Minimum/Maximum | 1/349 | 1/235 | 1/349 | |||
The local population presented a cancer hospital mortality rate that was almost double that of immigrants (5.2% Chileans, 2.5% immigrants) (Table 1). The latter had a lower average age of death (60 years for immigrants versus 65 years for Chileans), increasing their years of potential life lost. No death was registered within the HD in older adults aged more than 75 years for immigrants. In contrast, we found 30% of the total CHD for this age range reported as deceased for Chileans.
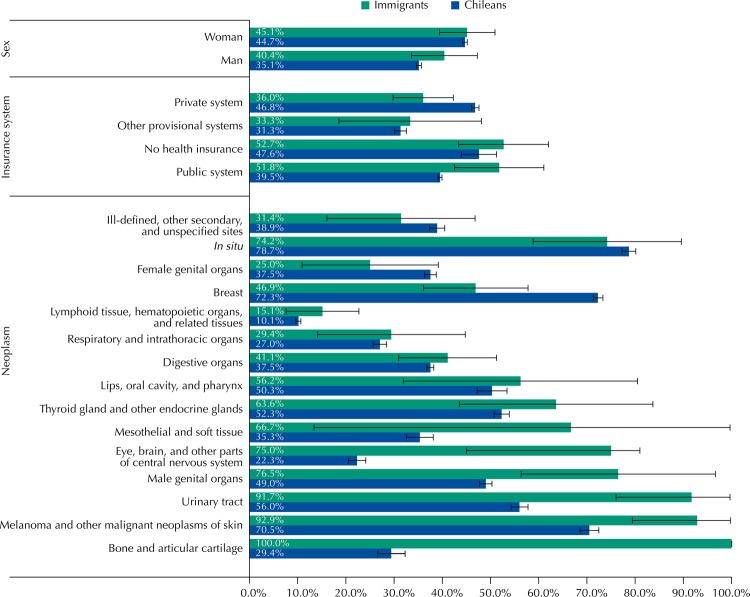
Chileans presented 50.1% of the CHD in patients with four or more days of stay, while this percentage was 32.7% for immigrants. Conversely, for surgical interventions (SI), the proportion is 0.3 percentage points higher in the immigrant population (Table 1). This situation was maintained for the different types of cancer, going from two to seventy-one percentage points of difference between Chileans and immigrants. The exceptions were the neoplasms of breast, female organs, in situ, and ill-defined sites, in which Chileans had a higher percentage of SI than immigrants. Breast cancer was the only type that presented a statistically significant difference in the local population (72.3% Chileans, 46.9% immigrants). We also observed differences in the proportion of surgical interventions, and only the private system (Institutions of Health Insurance [ISAPRE]) registered a higher percentage of SI in Chileans than in immigrants (46.8% Chileans, 46.9% immigrants, statistically significant difference) (Figure).
Figure. Percentage of surgical interventions in cancer patients (C00-D09 of the ICD-10) with the respective confidence intervals (95% confidence level), for Chileans and immigrants, according to the type of neoplasm, sex, and health insurance. Chile, 2012.
We observed the most evident differences between Chileans and immigrants for health insurance. For Chileans, the highest proportion of CHD, close to 70.0%, occurred in patients with National Health Fund (FONASA), even after stratifying by sex and age. In contrast, for immigrant population, the highest proportion occurred in patients with ISAPRE (46.3%), even after stratifying by sex. We highlight the high percentage of CHD for immigrants without health insurance, 22.6% (equivalent to 110 CHD), which is above the 1.0% of CHD (equivalent to 742 CHD) for Chileans in the same situation. For both populations, women had more CHD than men. However, this situation is not transversal for all age groups; for example, in children under 14 years of age, the proportion of CHD for men was higher (Table 2).
Table 2. Sociodemographic profile (sex, age, health insurance) of patients who were discharged because of cancer (C00-D09 of ICD-10), according to migratory status. Chile, 2012.
| Migratory status/ sex/ health insuranced | Age (years)a | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| 0 to 14 (n = 6,370)b | 15 to 29 (n = 4,702) | 30 to 44 (n = 9,512) | 45 to 59 (n = 19,215) | 60 to 74 (n = 23,565) | 75 to 89 (n = 10,377) | 90 or more (n = 541) | Total (n = 74,282) | |||
| Chilean | Man | Public | 81.1% | 72.8% | 60.9% | 66.2% | 69.3% | 73.5% | 67.9% | 70.1% |
| Private | 11.3% | 19.6% | 30.6% | 25.7% | 20.5% | 13.2% | 10.7% | 20.2% | ||
| No insurance | 0.4% | 0.8% | 1.3% | 1.1% | 1.2% | 1.0% | 1.3% | 1.0% | ||
| Other | 7.2% | 6.9% | 7.2% | 7.1% | 9.0% | 12.3% | 20.1% | 8.7% | ||
| Total | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | ||
| % of menc | 56.3%c | 52.0% | 31.4% | 36.3% | 49.9% | 49.5% | 41.4% | 44.6% | ||
| Woman | Public | 75.1% | 71.0% | 67.4% | 68.8% | 73.8% | 78.7% | 78.2% | 71.9% | |
| Private | 13.5% | 20.0% | 26.7% | 24.4% | 18.6% | 10.1% | 4.4% | 20.2% | ||
| No insurance | 0.4% | 1.5% | 1.0% | 0.8% | 0.9% | 1.1% | 2.2% | 0.9% | ||
| Other | 11.1% | 7.5% | 5.0% | 6.1% | 6.6% | 10.1% | 15.1% | 7.1% | ||
| Total | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | ||
| Total | Public | 78.4% | 71.9% | 65.3% | 67.9% | 71.6% | 76.1% | 73.9% | 71.1% | |
| Private | 12.3% | 19.8% | 27.9% | 24.8% | 19.6% | 11.7% | 7.0% | 20.2% | ||
| No insurance | 0.4% | 1.1% | 1.1% | 0.9% | 1.1% | 1.1% | 1.8% | 1.0% | ||
| Other | 8.9% | 7.1% | 5.7% | 6.4% | 7.8% | 11.2% | 17.2% | 7.8% | ||
| Total | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | ||
| 0 to 14 | 15 to 29 | 30 to 44 | 45 to 59 | 60 to 74 | 75 to 89 | 90 or more | Total | |||
| (n = 18) | (n = 19) | (n = 78) | (n = 143) | (n = 154) | (n = 71) | (n = 3) | (n = 486) | |||
| Immigrant | Man | Public | 58.3% | 33.3% | 9.1% | 22.0% | 10.8% | 17.6% | 100.0% | 19.2% |
| Private | 16.7% | 0.0% | 36.4% | 52.0% | 37.3% | 47.1% | 0% | 39.9% | ||
| No insurance | 25.0% | 66.7% | 54.5% | 22.0% | 36.1% | 29.4% | 0% | 32.3% | ||
| Other | 0% | 0% | 0% | 4.0% | 15.7% | 5.9% | 0% | 8.6% | ||
| Total | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | ||
| % of menb | 66.7% | 31.6% | 14.1% | 35.0% | 53.9% | 47.9% | 66.7% | 40.7% | ||
| Woman | Public | 0% | 69.2% | 40.3% | 22.6% | 16.9% | 13.5% | 0% | 25.7% | |
| Private | 33.3% | 15.4% | 56.7% | 45.2% | 50.7% | 70.3% | 0% | 50.7% | ||
| No insurance | 66.7% | 7.7% | 3.0% | 21.5% | 19.7% | 10.8% | 100% | 16.0% | ||
| Other | 0% | 7.7% | 0% | 10.8% | 12.7% | 5.4% | 0% | 7.6% | ||
| Total | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | ||
| Total | Public | 38.9% | 57.9% | 35.9% | 22.4% | 13.6% | 15.5% | 66.7% | 23.0% | |
| Private | 22.2% | 10.5% | 53.8% | 47.6% | 43.5% | 59.2% | 0% | 46.3% | ||
| No insurance | 38.9% | 26.3% | 10.3% | 21.7% | 28.6% | 19.7% | 33.3% | 22.6% | ||
| Other | 0% | 5.3% | 0% | 8.4% | 14.3% | 5.6% | 0% | 8.0% | ||
| Total | 100% | 100% | 100% | 100% | 100% | 100% | 100% | 100% | ||
a Of the hospital discharges for Chileans, 8.6% were patients aged between 1 and 14 years, 6.3% between 15 and 29, 12.8% between 30 and 44, 25.9% between 45 and 59, 31.7% between 60 and 74, 14% between 75 and 89, and 0.7% were aged 90 years or more. Of the hospital discharges for immigrants, 3.7% were patients aged between 1 and 14 years, 3.9% between 15 and 29, 16% between 30 and 44, 29.4% between 45 and 59, 31.7% between 60 and 74, 14.6% between 75 and 89, and 0.6% were aged 90 years or more.
b “n” corresponds to the total of Chileans or immigrants, as appropriate, in the age group.
c Of the hospital discharges corresponding to Chilean patients aged between 0 and 14 years, 56.3% were men and, consequently, 43.7% were women. An analog reading can be carried out for all percentages present in this row of % of men.
d The National Health Fund (FONASA) corresponds to the Public System, and the Institutions of Health Insurance (ISAPRE) corresponds to the private health system.
The information provided up to this point shows the characteristics of hospitalization and the (absolute and relative) frequency of CHD in both populations and their subgroups. However, in order to understand the dynamics of the CHD, we need to analyze them also in terms of rates (crude and specific), especially if we wish to compare populations with different structures, as is the case of Chileans and immigrants.
The 486 CHD for immigrants suppose a rate of 162.4 discharges per 100,000 persons; the 74,282 CHD for Chileans suppose a rate of 446.6 discharges per 100,000 persons. Standardized by sex and age, immigrants had a rate of 249.3 CHD per 100,000 persons and the local population had a rate of 446 CHD per 100,000 persons. In both cases, Chileans presented a higher rate of CHD, but when we standardize it, the gap decreases between both populations.
The specific rates by sex and age groups were higher for Chileans than for immigrants. This situation was repeated for the different types of health insurance, with the exception of the subgroup that had no insurance (174.6 × 100,000 persons for Chileans, 335.2 × 100,000 persons for immigrants). Among men without health insurance, the rates of CHD were higher for immigrants than for the local population for all age subgroups; on the other hand, in the case of women without health insurance, this situation occurred only in those aged between zero and 14, 45 and 74, and older adults aged over 90 years. In immigrants younger than 15 years of age, although the amount of CHD corresponding to patients from FONASA and without insurance was the same (n = 8), the rate was higher in those without insurance with 98.9 CHD per 100,000 persons (Table 3).
Table 3. Specific rates of cancer hospital morbidity according to sex, age group, migratory status, and health insurance, amplified by 100,000. Chile, 2012.
| Variable | Chilean 446.6* | Immigrant 162.4* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| Public | Private | Other | None | Total | Public | Private | Other | None | Total | ||
|
|
|
|
|
|
|
|
|
|
|
|
|
| Sexo | Age (years) | 397.0 | 669.0 | 1279.0 | 174.6 | 446.6 | 56.0 | 411.8 | 629.3 | 335.2 | 162.4 |
| Man | 0 to 14 | 198.5 | 179.1 | 568.2 | 66.0 | 201.8 | 58.4 | 78.6 | 0.0 | 66.0 | 61.8 |
| 15 to 29 | 116.5 | 142.5 | 267.1 | 22.9 | 118.8 | 7.2 | 0.0 | 0.0 | 68.9 | 13.5 | |
| 30 to 44 | 176.1 | 331.2 | 538.6 | 55.5 | 205.7 | 3.9 | 48.9 | 0.0 | 137.3 | 27.0 | |
| 45 to 59 | 417.3 | 808.4 | 1072.1 | 127.9 | 478.6 | 101.5 | 436.5 | 585.7 | 796.2 | 263.1 | |
| 60 to 74 | 1162.4 | 3058.9 | 3598.1 | 870.1 | 1407.8 | 200.6 | 2080.5 | 4788.2 | 3236.2 | 1138.1 | |
| 75 to 89 | 1448.6 | 4790.9 | 4508.7 | 2312.4 | 1746.8 | 319.5 | 2608.0 | 1126.8 | 8368.2 | 1186.9 | |
| 90 or more | 885.9 | 1390.9 | 3440.4 | 707.5 | 1072.4 | 489.6 | 0 | - | - | 455.6 | |
| Total | 379.7 | 580.2 | 1200.6 | 136.6 | 419.4 | 45.7 | 300.4 | 473.1 | 373.3 | 147.6 | |
| Woman | 0 to 14 | 146.0 | 165.4 | 794.0 | 45.4 | 159.8 | 0.0 | 61.9 | 0.0 | 157.8 | 28.2 |
| 15 to 29 | 95.9 | 158.4 | 385.0 | 59.8 | 108.3 | 23.9 | 26.6 | 159.5 | 14.8 | 24.6 | |
| 30 to 44 | 332.4 | 702.5 | 1056.4 | 203.8 | 396.3 | 70.7 | 354.7 | 0.0 | 60.4 | 125.0 | |
| 45 to 59 | 599.2 | 1320.8 | 1712.0 | 278.1 | 710.2 | 127.6 | 851.6 | 2285.7 | 958.1 | 386.1 | |
| 60 to 74 | 944.7 | 2753.7 | 2329.4 | 1146.4 | 1121.2 | 185.7 | 2138.4 | 4109.6 | 2737.0 | 799.0 | |
| 75 to 89 | 1045.2 | 2682.8 | 2915.2 | 1290.8 | 1184.4 | 194.9 | 9647.5 | 784.3 | 1027.0 | 1059.6 | |
| 90 or more | 612.8 | 1400.0 | 1196.1 | 958.9 | 676.4 | 0 | - | 0 | 1550.4 | 120.9 | |
| Total | 411.8 | 763.4 | 1367.2 | 235.0 | 471.2 | 63.3 | 515.2 | 844.9 | 293.5 | 174.4 | |
| Total | 0 to 14 | 172.6 | 172.2 | 672.0 | 55.1 | 181.0 | 26.2 | 69.3 | 0.0 | 98.9 | 44.2 |
| 15 to 29 | 105.8 | 149.8 | 315.4 | 37.9 | 113.5 | 16.8 | 13.3 | 39.7 | 39.8 | 19.5 | |
| 30 to 44 | 263.8 | 506.9 | 763.4 | 99.5 | 306.9 | 43.9 | 222.2 | 0.0 | 104.1 | 82.7 | |
| 45 to 59 | 519.0 | 1067.2 | 1383.6 | 183.7 | 604.1 | 117.2 | 624.5 | 1540.4 | 893.6 | 331.8 | |
| 60 to 74 | 1038.8 | 2905.3 | 2923.3 | 970.6 | 1248.1 | 191.8 | 2111.2 | 4485.2 | 3058.7 | 951.8 | |
| 75 to 89 | 1205.7 | 3565.1 | 3609.2 | 1643.9 | 1409.2 | 247.6 | 4756.5 | 924.9 | 2750.5 | 1117.0 | |
| 90 or more | 694.1 | 1394.2 | 1747.8 | 866.6 | 798.5 | 173.0 | 0 | 0 | 1550.4 | 237.0 | |
| Total | 397.0 | 669.0 | 1279.0 | 174.6 | 446.6 | 56.0 | 411.8 | 629.3 | 335.2 | 162.4 | |
* The standardized rate of cancer hospital morbidity for Chileans is 446 (95%CI 404.7–487.3) and the standardized rate of hospital cancer morbidity for immigrants is 249.3 (95%CI 218.4–280.2). The rates were standardized using the total population of Chile as the reference structure.
Among the variables considered for the model of excess zeros, “other insurance” and age were significant. Thus, the chance of presenting excess zero was 9.4 times (95%CI 1.57–55.92) higher in patients with other health insurance (other than the public or private system) in relation to those without insurance. In relation to age, as it increased in one year, the chance to present excess zero decreased by 5.0% (OR = 0.95, 95%CI 0.92–0.98) (Table 4).
Table 4. Analysis of the zero-inflated negative binomial model for the relationship between cancer rate and migratory status, adjusted for sociodemographic variables, including additive and interaction effects. Chile, 2012.
| Variable | Coefficient | PR | 95%CI | p | |
|---|---|---|---|---|---|
| Negative binomial model (counting) | |||||
|
| |||||
| Migratory status | Immigrant | 0.969 | 2,6 | 1.77–3.93 | 0.000 |
| Chilean | 1 | ||||
| Age | Age | 0.033 | 1.0 | 1.02–1.05 | 0.000 |
| Age | 0.0001 | 1.0 | 0.99–1.00 | 0.343 | |
| Sex | Woman | 0.095 | 1.1 | 0.92–1.32 | 0.308 |
| Man | 1 | ||||
| Health insurance | FONASA | 0.388 | 1.5 | 1.08–2.01 | 0.014 |
| ISAPRE | 1.071 | 2.9 | 2.15–3.96 | 0.000 | |
| Other | 1.568 | 4.8 | 3.51–6.56 | 0.000 | |
| No insurance | |||||
| Intersection | Immigrant-FONASA | -2.547 | 0.8 | 0.05–0.14 | 0.000 |
| Immigrant-ISAPRE | -1.073 | 0.3 | 0.20–0.59 | 0.000 | |
| Immigrant-other | -1.055 | 0.3 | 0.17–0.72 | 0.005 | |
| Constant | -7.633 | 0.001 | 0.0003–0.0007 | 0.000 | |
|
| |||||
| Logistic model (excess zeros) | |||||
|
| |||||
| Migratory status | Immigrant | 20.92 | 1.22x109 | 0 | 0.995 |
| Chilean | 1 | ||||
| Age | Age | -0.05 | 0.9 | 0.91–0.98 | 0.004 |
| Sex | Woman | 0.2 | 1.2 | 0.39–3.80 | 0.73 |
| Man | 1 | ||||
| Health insurance | Public | -0.13 | 0.9 | 0.14–5.47 | 0.889 |
| Private | 0.4 | 1.5 | 0.31–7.24 | 0.619 | |
| Other | 2.24 | 9.4 | 1.58–55.92 | 0.014 | |
| No insurance | 1 | ||||
| Constant | -20.82 | 0.0 | 0 | 0.995 | |
PRR: Prevalence Rate Ratio
In(α) = -0.882 (IC95% -1.120 – -0.644), p = 0.000
Log pseudolikelihood: p = 0.000
Test Vuong: z = 1.70; p = 0.0442
The adjusted ZINB model reaffirms some of the observed results at the level of specific rates. Immigrants without health insurance were 2.6 times (95%CI 1.77–3.93) more likely to leave the hospital because of cancer compared to Chileans without insurance. Other types of insurance had a different situation. Sex was the only variable that had no significant effect on the count model. The adjusted models showed adequate adjustment, supporting the validity of these results (Table 4).
DISCUSSION
Neoplasms were the third cause of hospital discharges for immigrants (n = 700) and the seventh for the local population (n = 115,406) in Chile in 2012. In the group of immigrants, the CHD mainly corresponded to patients belonging to the private system (46.0%), and in the group of Chileans they mainly corresponded to patients in the public system (71.1%). We observed a large difference in the proportion of CHD for patients with no health insurance between the two populations (22.6%: immigrants, 1.0%: Chileans). In both populations, the three most frequent types of cancer were: (i) lymphoid tissue, hematopoietic organs, and related tissues, (ii) digestive organs, and (iii) breast cancer.
Similar to the results found in Italy for hospital discharges in general 19 , the rate of CHD differs between the local (446.0 CHD per 100,000 persons) and immigrant population (249.3 CHD per 100,000 persons), being it lower for immigrants. Similar to that found in Spain on the total number of hospital discharges 7 , the local population in Chile has longer hospitalization stay for cancer than immigrants. Paradoxically, with some exceptions, for the different types of cancer, sex, and health insurance, immigrants have a higher proportion of surgical interventions for cancer (Figure). All of the above suggests inequalities in the quality, use, and access to secondary health care between both populations.
Similarly to what is happening around the world, changes in breast cancer rates have been observed among working women who migrated to industrialized regions 24 , which highlights the importance of analyzing this pathology in immigrants. In Chile, based on hospital discharges, breast cancer also appears as a focus of special attention in this population. For 2012, the percentage of discharges for cancer within the total HD was higher in immigrants than in Chileans in the same situation. This is one of the only four cancers in which immigrants have a lower proportion of surgical interventions. This reality is similar to that observed in Italy, where immigrants had lower rates of mastectomies than the local population 19 .
This study has strengths, such as: (i) it is the first of its kind in the country 25 , (ii) it can count on the universe of CHD for the local and immigrant population in the period, (iii) it analyzes the exposed problem considering demographic, hospital, and health insurance variables, and (iv) it uses an appropriate analysis methodology 23 , by recognizing the distribution of the studied phenomenon (CHD, their dispersion, and the large number of subgroups in which no CHD is observed) and the difference in the population structures between Chileans and immigrants 3 (according to phenomena such as the “feminization of migration” and “effect of the health migrant”). This is not only applied at the theoretical level, but it is also proved in practice by the Vuong test, which was significant at a level of 0.05 for the proposed ZINB model. This indicates that this model is a significant improvement to explain the situation of a standard negative binomial model 23 .
This research has limitations, such as: (i) the impossibility of determining in which stage of the disease the HD occurred and if the disease was present before the migratory process, (ii) the difficulty in elucidating whether the results obtained are the product of prevalence of cancer in both populations or whether they were a reflection of the way in which both populations use the health services 26 , (iii) the selection bias, because of the difference in the definition of immigrants in the record of HD (nationality of the patient) and CASEN (“lifetime migration”, mother’s residence at the moment of the person’s birth), and (iv) the information bias when collecting the variable of migratory status in both databases, since it is carried out using different questions (“what is your nationality?”, for hospital discharges, versus “in which country did your mother live when you were born?”, for the CASEN database).
This study needs some relevant variables for research. The length of stay in the recipient country is one of the variables that recurrently appears in the literature as fundamental to analyze the different health phenomena in the international migrant population 6 , especially in studies on cancer and more specifically on breast cancer 24 , 27 , 28 . The study by John et al. carried out in the United States in 2005, has indicated that the incidence rate of breast cancer is directly proportional to the time lived in the country, especially in women who had arrived before the age of 20 years 28 . Given the absence of this variable in official records, we could not consider it in the analysis in this research. Similarly, we did not have the variables of socioeconomic status, degree of cultural assimilation, age of arrival in the country, and other variables related to the disease. These variables could be considered in the future for a better understanding of this phenomenon and its implications for public health.
We can identify some implications of this research and public health study. Hospital discharges are a valuable source of information and are usually used to determine morbidity in the population 29 . Similarly, studies on the immigrant population are of great utility for public health and epidemiology, as they compare populations with genetic and ethnic differences that begin to share the social, cultural, and environmental conditions at some point in their life 27 . Along with these premises, the results of this study emphasize the importance of studying cancer in this community, in general, and cancers of interest such as breast cancer. At the same time, studies need to stratify by ethnicity and/or origin, examining the modifiable behavior and environmental determinants before and after the migration process.
This research opens the door for future research in the country for the generation of hypothesis regarding the access and use of tests for the early detection and timely treatment of cancer by immigrants. Cancer is a disease in which survival tends to be worse when factors such as social vulnerability, late diagnosis, and access limitations are combined, which fits the profile of some immigrant groups in Chile and Latin America.
Acknowledgments
The authors would like to thank the department of health statistics and information (DEIS) of the Ministry of Health of Chile for delivering the database of hospital discharges of 2012.
Footnotes
Funding: Comissão Nacional de Pesquisa Científica e Tecnológica (CONICYT – Projeto Fondecyt de Iniciação 11130042).
REFERENCES
- 1.United Nations, Department of Economic and Social Affairs, Population Division . Trends in total migrant stock: the 2005 revision. New York: 2006. [cited 2017 Sep 30]. http://www.un.org/esa/population/publications/migration/UN_Migrant_Stock_Documentation_2005.pdf. [Google Scholar]
- 2.International Organization for Migration . World migration report: communicating effectively about migration. Geneva: IOM; 2012. [cited 2017 Feb 1]. http://publications.iom.int/system/files/pdf/wmr2011_english.pdf. [Google Scholar]
- 3.Cabieses B, Pickett KE, Tunstall H. Comparing sociodemographic factors associated with disability between immigrants and the Chilean-born: are there different stories to tell. Int J Environ Res Public Health. 2012;9(12):4403–4432. doi: 10.3390/ijerph9124403. https://doi.org/10.3390/ijerph9124403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azerkan F, Zendehdel K, Tillgren P, Faxelid E. Risk of cervical cancer among immigrants by age at immigration and follow-up time in Sweden, from 1968 to 2004. Int J Cancer. 2008;123(11):2664–2670. doi: 10.1002/ijc.23843. https://doi.org/10.1002/ijc.23843. [DOI] [PubMed] [Google Scholar]
- 5.Davies A, Mosca D, Frattini C. Migration and health service delivery. World Hosp Health Serv. 2010;46(3):5–7. [PubMed] [Google Scholar]
- 6.Cabieses B, Tunstall H, Pickett KE, Gideon J. Understanding differences in access and use of healthcare between international immigrants to Chile and the Chilean-born : a repeated cross-sectional population-based study in Chile. Int J Equity Health. 2012;11:68. doi: 10.1186/1475-9276-11-68. https://doi.org/10.1186/1475-9276-11-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanz B, Torres AM, Schumacher TR. Características sociodemográficas y utilización de servícios sanitarios por la población inmigrante residente en un área de la Comunidad de Madrid. Aten Primaria. 2000;26(5):314–318. doi: 10.1016/S0212-6567(00)78671-9. https://doi.org/10.1016/S0212-6567(00)78671-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harmsen JAM, Bernsen RMD, Bruijnzeels MA, Meeuwesen L. Patients’ evaluation of quality of care in general practice: what are the cultural and linguistic barriers? Patient Educ Couns. 2016;72(1):155–162. doi: 10.1016/j.pec.2008.03.018. https://.doi.org/10.1016/j.pec.2008.03.018. [DOI] [PubMed] [Google Scholar]
- 9.Hernando Arizaleta L, Palomar Rodríguez J, Márquez Cid M, Monteagudo Piqueras O. Impacto de la inmigración sobre la asistencia hospitalaria: frecuentación, casuística y repercusión económica. [cited 2017 Sep 30];Gac Sanit. 2009 23(3):208–215. doi: 10.1016/j.gaceta.2008.06.006. http://scielo.isciii.es/pdf/gs/v23n3/original6.pdf. [DOI] [PubMed] [Google Scholar]
- 10.Rodríguez-Salés V, Ortiz-Barreda G, Sanjosé S. Revisión bibliográfica sobre la prevención del cáncer en personas inmigrantes residentes en España. Rev Esp Salud Publica. 2014;88(6):735–743. doi: 10.4321/S1135-57272014000600006. https://doi.org/10.4321/S1135-57272014000600006. [DOI] [PubMed] [Google Scholar]
- 11.López-Gómez M, Malmierca E, Górgolas M, Casado E. Cancer in developing countries : the next most preventable pandemic . the global problem of cancer. Crit Rev Oncol Hematol. 2013;88(1):117–122. doi: 10.1016/j.critrevonc.2013.03.011. https://doi.org/10.1016/j.critrevonc.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Organización Panamericana de la Salud . El cáncer en la región de las Américas. Washington (DC): 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Icasa-N M, Nuñez-F ML, Torres-A FJ, Díaz-S NL, Varela-G DE. Distribución geográfica de mortalidad por tumores malignos de estómago, tráquea, bronquios y pulmón, Chile 1997-2004. Rev Med Chile. 2007;135(11):1397–1405. https://doi.org/10.4067/S0034-98872007001100005. [PubMed] [Google Scholar]
- 14.Medina-L E, Kaempffer-R AM. Mortalidade por cáncer en Chile: consideraciones epidemiológicas. Rev Med Chile. 2001;129(10):1195–1202. https://doi.org/10.4067/S0034-98872001001000014. [PubMed] [Google Scholar]
- 15.Turrin A, Zorzi M, Giorgi Rossi P, Senore C, Campari C, Fedato C, et al. Colorectal cancer screening of immigrants to Italy. Figures from the 2013 National Survey. Prev Med. 2015;81:132–137. doi: 10.1016/j.ypmed.2015.08.016. https://doi.org/10.1016/j.ypmed.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 16.Tornesello ML. Rossi PG. Buonaguro L. Buonaguro FM. HPV Prevalence Italian Working Group Human papillomavirus infection and cervical neoplasia among migrant women living in Italy. 31Front Oncol. 2014;4 doi: 10.3389/fonc.2014.00031. https://doi.org/10.3389/fonc.2014.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Norredam M, Olsbjerg M, Petersen JH, Hutchings M, Krasnik A. Cancer mortality does not differ between migrants and Danish-born patients. A4848Dan Med J. 2014;61(6) [PubMed] [Google Scholar]
- 18.Sanz-Barbero B, Regidor E, Galindo S. Influencia del lugar de origen en la utilización de pruebas de cribado de cáncer ginecológico en España. Rev Saude Publica. 2011;45(6):1019–1026. doi: 10.1590/s0034-89102011000600003. https://doi.org/10.1590/S0034-89102011000600003. [DOI] [PubMed] [Google Scholar]
- 19.Waure C, Bruno S, Furia G, Di Sciullo L, Carovillano S, Specchia ML, et al. Health inequalities: an analysis of hospitalizations with respect to migrant status, gender and geographical area. 2BMC Int Health Hum Rights. 2015;15 doi: 10.1186/s12914-014-0032-9. https://doi.org/10.1186/s12914-014-0032-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wahlberg A, Kallestai C, Lundgren AC, Essén B. Causes of death among undocumented migrants in Sweden, 1997-2010. Glob Health Action. 2014;7:24464. doi: 10.3402/gha.v7.24464. https://doi.org/10.3402/gha.v7.24464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Superintendencia de Salud (CHL) Departamento de Estudios y Desarrollo . Analisis general de los egresos hospitalarios, año 2005. Santiago: 2006. [Google Scholar]
- 22.Ministerio del Desarrollo Social(CHL) Metodología de Diseño Muestral Encuesta de Caracterización Socioeconómica Nacional 2013. Santiago: Observatorio Social; 2015. [cited 2017 Sep 30]. Documentos Metodológicos, 30. http://observatorio.ministeriodesarrollosocial.gob.cl/documentos/Metodologia_Diseno_Muestral_Casen_2013.pdf. [Google Scholar]
- 23.Long JS. Regression models for categorical and limited dependent variables. Thousand Oaks: SAGE Publications; pp. 242–249. 1997. 1997. Social Sciences Series. Advanced Quantitative Techniques, 7. [Google Scholar]
- 24.Ziegler RG, Hoover RN, Pike MC, Hildesheim A, Nomura AM, West DW, et al. Migration patterns and breast cancer risk in Asian-American women. J Natl Cancer Inst. 1993;85(22):1819–1827. doi: 10.1093/jnci/85.22.1819. [DOI] [PubMed] [Google Scholar]
- 25.Cabieses B, Pickett KE, Tunstall H. What are the living conditions and health status of those who don’t report their migration status? A population-based study in Chile. 1013BMC Public Health. 2012;12 doi: 10.1186/1471-2458-12-1013. https://doi.org/10.1186/1471-2458-12-1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.López Lázaro L. Inmigración, estado de salud y uso de servicios de atención primaria. Aten Primaria. 2008;40(5):232–233. doi: 10.1157/13120589. https://doi.org/10.1157/13120589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parkin DM, Khlat M. Studies of cancer in migrants: rationale and methodology. Eur J Cancer. 1996;32A(5):761–771. doi: 10.1016/0959-8049(96)00062-7. [DOI] [PubMed] [Google Scholar]
- 28.John EM, Phipps AI, Davis A, Koo J. Migration history, acculturation, and breast cancer risk in Hispanic women. Cancer Epidemiol Biomarkers Prev. 2005;14(12):2905–2913. doi: 10.1158/1055-9965.EPI-05-0483. https://doi.org/10.1158/1055-9965.EPI-05-0483. [DOI] [PubMed] [Google Scholar]
- 29.North Carolina Department of Human Resources, Division of Health Services, State Center For Health Statistics . Use of hospital discharge data for estimating morbidity in North Carolina. Raleigh: 1981. [cited 2017 Sep 30]. SCHS Studies, 20. http://digital.ncdcr.gov/cdm/ref/collection/p249901coll22/id/160426. [Google Scholar]
- 30.Herrera Riquelme CA, Kuhn-Barrientos L, Rosso Astorga R, Jiménez de la Jara J. Tendencia de la mortalidad por cáncer en Chile según diferencias por nivel educacional, 2000-2010. [cited 2017 Sep 30];Rev Panam Salud Publica. 2015 37(1):44–51. http://www.scielosp.org/pdf/rpsp/v37n1/a06v37n1.pdf. [PubMed] [Google Scholar]