The National Lung Screening Trial (NLST) released its main findings in 2011,1 concluding that the use of low-dose computed tomography (CT) to screen for lung cancer reduced lung cancer deaths by 20% compared with chest radiography.1,2 The subsequent publication of new lung cancer screening (LCS) guidelines may raise the public’s awareness of the clinical application of low-dose CT in screening,3,4 leading to increased demand for screening not only by individuals who meet the eligibility criteria recommended for LCS but also by those who do not. The present study documents early experience of LCS in terms of both intended and unintended uptake of low-dose CT at the population level.
Methods
We used data from the 2010 and 2015 National Health Interview Survey (NHIS)Cancer Control Module (CCM) (https://healthcaredelivery.cancer.gov/nhis/) linked to the core questionnaire and limited our study cohort to individuals who were 40 years or older. Using smoking status and history from the CCM, we classified individuals into high-risk smokers (30 pack-years of smoking history, current smokers or those who quit smoking within the last 15 years), low-risk smokers (current or former smokers who did not meet the criteria of high-risk smokers), and never-smokers. Per the age eligibility criteria in the NLST, we defined LCS-eligible individuals as high-risk smokers aged 55 to 74 years. We identified LCS with CT using the survey question “Were any of the CAT scans of your chest area done to check for lung cancer, rather than for some other reason?” A similar question was used to identify LCS with chest radiography. Weighted analyses that accounted for the multistage survey design of the NHIS were performed to compare the utilization of CT in 2010 and 2015. This study was exempted from review and participant written informed consent by the institutional review board at The University of Texas MD Anderson Cancer Center.
Results
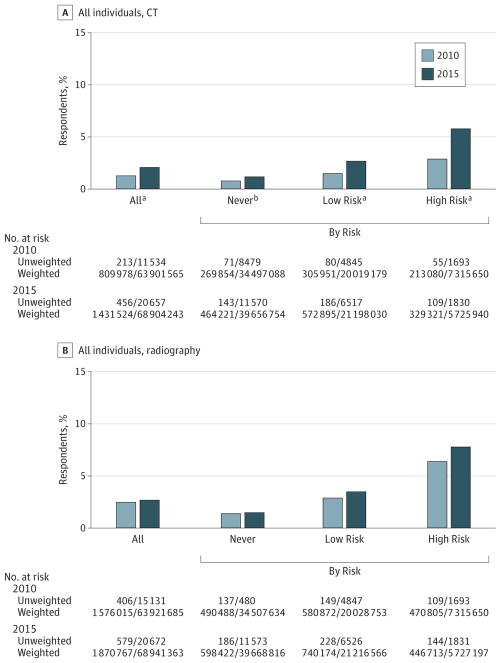
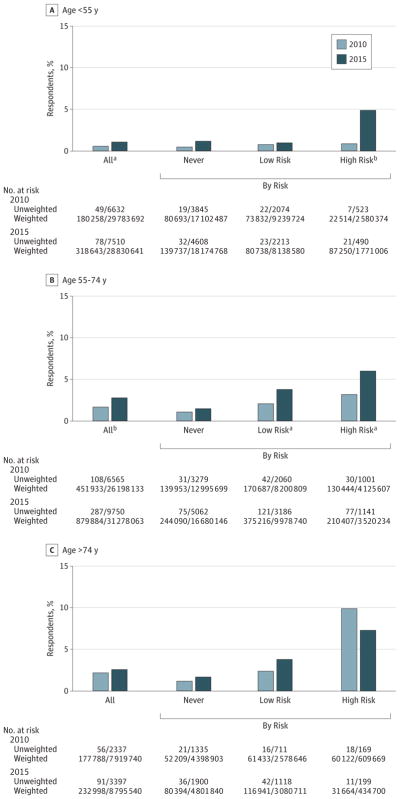
A total of 36 191 individuals responded to the question of CT for LCS, and 36 209 individuals responded to the chest radiography question. The percentage of individuals who received CT scans for LCS was more than 1.5 times higher in 2015 than in 2010 (2.1% vs 1.3%; P < .001) (Figure 1A), while the use of chest radiography for LCS was not significantly different (2.7% in 2015 vs 2.5% in 2010; P = .22) (Figure 1B). A similar trend in the use of CT was observed among many subgroups stratified by smoking or eligibility status. Figure 1A shows the rate of CT scans significantly increased for never-smokers (1.2% vs 0.8%; P = .03), low-risk smokers (2.7% vs 1.5%; P < .001), and high-risk smokers (5.8%vs 2.9%; P < .001). In addition, significant increases in the rate of CT were observed among high-risk smokers who did not meet the age eligibility criteria (Figure 2A) and those who met the age eligibility but were not heavy smokers (Figure 2B). No significant trend in the use of CT was observed for individuals older than 74 years (Figure 2C).
Figure 1. Weighted Analysis of the Rate of Lung Cancer Screening in the National Health Interview Survey by Screening Technology and Risk for Lung Cancer.
Individuals in the “All” category could not be classified by risk owing to missing responses to 1 or more questions used in risk classification. Virgule construction represents No./total No.
aP < .001.
bP < .05.
Figure 2. Weighted Analysis of the Rate of Computed Tomography for Lung Cancer Screening in the National Health Interview Survey by Risk for Lung Cancer and Age Eligibility.
Individuals in the “All” category could not be classified by risk owing to missing responses to 1 or more questions used in risk classification. Virgule construction represents No./total No.
aP < .05.
bP < .001.
Discussion
Our analysis of LCS-related survey questions in national survey data showed 3 interesting patterns when comparing the screening rate between 2001 and 2015. First, we found a significant but small increase in the use of CT among individuals who met the eligibility criteria of LCS. This pattern of intended use of CT scans exhibits a slow uptake and under use of a screening technology with established effectiveness. Second, a temporal rise in the use of CT for LCS was also found among individuals who did not meet the eligibility criteria; this unintended spillover raises concerns about overuse. To what extent the increasing use of CT for LCS was driven by recently released guidelines or simply reflected a rising trend of CT use in general needs to be explored in future research.5 Finally, the use of chest radiography remained stable despite its lack of effectiveness in LCS, which may reflect primary care physicians’ knowledge gap regarding the latest scientific discovery in LCS.6
Acknowledgments
Funding/Support: This work was supported by the Duncan Family Institute, a fellowship from The University of Texas MD Anderson Cancer Center’s Halliburton Employees Foundation (Huo), and the National Cancer Institute (Shih; R01 CA207216).
Additional Contributions: The authors thank Gary Deyter, technical writer from the Department of Health Services Research at The University of Texas MD Anderson Cancer Center, for his editorial assistance. He received no compensation for his contributions beyond that provided in the normal course of employment.
Footnotes
Conflict of Interest Disclosures: None reported.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author Contributions: Dr Shih had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Huo, Shen, Shih.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Huo, Shen.
Critical revision of the manuscript for important intellectual content: Huo, Volk, Shih.
Statistical analysis: Huo, Shen.
Obtained funding: Huo, Shih.
Administrative, technical, or material support: Huo, Shih.
Supervision: Volk, Shih.
References
- 1.Aberle DR, Adams AM, Berg CD, et al. National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365(5):395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pinsky PF, Church TR, Izmirlian G, Kramer BS. The National Lung Screening Trial: results stratified by demographics, smoking history, and lung cancer histology. Cancer. 2013;119(22):3976–3983. doi: 10.1002/cncr.28326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moyer VA U.S. Preventive Services Task Force. Screening for lung cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(5):330–338. doi: 10.7326/M13-2771. [DOI] [PubMed] [Google Scholar]
- 4.Wender R, Fontham ETH, Barrera E, Jr, et al. American Cancer Society lung cancer screening guidelines. CA Cancer J Clin. 2013;63(2):107–117. doi: 10.3322/caac.21172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith-Bindman R, Miglioretti DL, Johnson E, et al. Use of diagnostic imaging studies and associated radiation exposure for patients enrolled in large integrated health care systems, 1996–2010. JAMA. 2012;307(22):2400–2409. doi: 10.1001/jama.2012.5960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lewis JA, Petty WJ, Tooze JA, et al. Low-Dose CT Lung Cancer Screening Practices and Attitudes among Primary Care Providers at an Academic Medical Center. Cancer Epidemiol Biomarkers Prev. 2015;24(4):664–670. doi: 10.1158/1055-9965.EPI-14-1241. [DOI] [PMC free article] [PubMed] [Google Scholar]