Abstract
Indigenous people worldwide suffer from higher rates of morbidity and mortality than neighboring populations. In addition to having limited access to public health infrastructure, indigenous people may also have priorities and health perceptions that deter them from seeking adequate modern healthcare. Here we propose that living in a harsh and unpredictable environment reduces motivation to pursue deliberate, costly action to improve health outcomes. We assess whether variation in Health Locus of Control (HLC), a psychological construct designed to capture self-efficacy with respect to health, explains variation in treatment uptake behavior among Tsimane Amerindians (N=690; age range: 40–89 years; 55.8% female; data collection: 2008–2012), a high mortality and morbidity indigenous population in the Bolivian Amazon, Beni Department. Comparisons with two industrialized populations in Japan (Miyagi prefecture; e0=76.6 years) and the United Kingdom (Caerphilly county borough; e0=81.2 years) confirm that Tsimane (e0=54.1 years) have a more externalized HLC. Multilevel level models were used to investigate whether HLC predicts treatment uptake, and mediates the relationship between modernization and treatment uptake. External HLC scores were predictive of treatment outcomes: Powerful others scores were positively associated with probability of receiving modern treatment (adjusted odds ratio [OR] =1.33), while Chance scores were negatively associated with probability of receiving modern treatment (adjusted OR=0.76). We found no effects, however, of Internal HLC or educational capital on treatment uptake. Overall, our findings indicate that health-related decision-making is influenced more by a psychological orientation affecting self-efficacy, shaped in part by perceptions of environmental unpredictability and harshness, than by limited knowledge, education or other indicators of modernization.
Keywords: locus of control, treatment, Tsimane, self-efficacy, modernization, healthcare
1. INTRODUCTION
Indigenous populations typically experience worse health outcomes than their non-indigenous neighbors, including malnutrition, stunted growth, infectious and chronic diseases, and thus lower life expectancy (King et al., 2009a). They face numerous obstacles to accessing quality health care (e.g. geographic isolation, lack of public health infrastructure, insufficient resources), which are often compounded by linguistic barriers, ethnic discrimination and mistrust of health care institutions (King et al., 2009b). Indigenous people may also prefer treatments that better reflect their own traditional beliefs of disease etiology, progression and transmission, and types of treatment perceived to be most effective. Greater exposure to and positive experience with modern treatments, perhaps through schooling or other means (e.g. town visits, social networks), may increase the likelihood of using modern healthcare, which may complement or substitute for traditional treatments. Preferences and decisions about treatments may also vary by illness type. For example, Chinese patients are more likely to use traditional treatments for respiratory infections, and modern treatments for traumas (Giordano et al., 2004). Treatment choice may not just reflect beliefs about disease etiology and preferences for efficacy (Huanca, 2006), but may also reflect constraints to obtaining preferred alternatives, e.g., if traditional treatments are readily available as fallback options (Lasker, 1981).
Here, we study the psychological underpinnings affecting treatment uptake and how they vary with modernization. We propose that preferences for and decisions to pursue treatments are affected by cues of environmental unpredictability, such as unsanitary living conditions, high rates of infectious disease, low socioeconomic status, natural disasters and displacement by governments or foreign entities (Ford et al., 2010). Cues of environments characterized by high mortality and morbidity have been linked to more present-oriented time preferences, as short-term fitness considerations may outweigh potential longer-term gains that may never be realized (Quinlan et al., 2016). A related literature on the psychology of poverty suggests that low income conditions affect decision-making by reducing self-efficacy and sense of personal control, increasing vigilance and impulsivity (Sheehy-Skeffington and Haushofer, 2014). Thus, a combination of resource limitation, harsh environment and uncertainty about the future may lead to undervaluing long-term health. Under such conditions of relative deprivation, one might expect under-utilization of available health care ( Nettle, 2010).
1.1. Health Locus of Control (HLC)
HLC describes the extent to which individuals believe their health is controllable and determined by their own actions, rather than by chance or deeds of other potent individuals (Wallston et al., 1978). HLC measures beliefs along three dimensions: i) Internal, ii) Powerful others and iii) Chance. Internal HLC is the extent to which individuals believe their health is due to their own actions. Powerful others HLC is the extent to which individuals believe their health is influenced by potent others (e.g. kin, friends, medical professionals). Chance HLC is the extent to which individuals believe their health is unpredictable and due to luck, fate, or other external factors over which they have no control. These three measures reflect underlying beliefs about the relative importance of self, others, and happenstance in determining one’s own health status (Wallston et al., 1978).
High Internal individuals believe that their health can be improved by their own actions, so they are more likely than others to seek treatment or engage in preventative health behaviors. High Chance individuals, on the other hand, believe they have relatively limited control over their health. They are thus less likely to pursue treatment or engage in preventive health behaviors. While considered an aspect of a more externalized locus of control, Powerful others HLC occupies a more ambiguous position. On one hand, individuals with high Powerful others may take fewer preventative health measures, believing that any health problems could be managed by others; on the other hand, for the same reason, they may be more likely to seek treatment and follow health recommendations provided by influential actors (Steptoe and Wardle, 2001).
In accordance with these general predictions, different HLC orientations are associated with a wide range of health behaviors and outcomes. Commitment to regular physical exercise (Duffy, 1997; Steptoe and Wardle, 2001), dental health behaviors (Macgregor et al., 1997; Steptoe and Wardle, 2001), frequency of cancer screening among women (Murray and McMillan, 1993), and reduced stress (Roddenberry and Renk, 2010) have been positively associated with Internal HLC and negatively with Chance and Powerful others. Self-reported poor health was negatively associated with both Internal and Chance HLC in the UK, but positively associated with Powerful others (Poortinga et al., 2008). Burker et al. (2005) found Internal HLC to be positively associated with the odds of surviving a lung transplant surgery, but null associations were found with Chance and Powerful others. However, associations with some health-related behaviors, including alcohol consumption and smoking, are inconsistent (Callaghan, 1998; Calnan, 1989). Explanations for these inconsistencies include small sample sizes, low statistical power, inappropriate statistical tests, inherent differences between risk-enhancing (e.g. smoking) and risk-reducing (e.g. regular exercise) behaviors and the multiple factors that affect them, as well as conceptual concerns with the HLC construct (reviewed in Steptoe and Wardle, 2001). The Chance HLC, for example, may be multidimensional reflecting not only beliefs in luck or fate, but also beliefs in other environmental factors over which individuals have some limited control (Steptoe and Wardle, 2001).
Although many HLC studies are correlational, experiments inducing a “poverty mindset” similarly show that experiences of poverty reduce self-efficacy (Sheehy-Skeffington and Haushofer, 2014; p.97–98). One observational study across seven countries showed that effects of socioeconomic status on health were mediated largely by perceived control over health (Bobak et al., 2000).
1.2. Life history theory and HLC
While individual differences in perceived control over one’s health could arise from differences in stable personality traits (Hampson and Friedman, 2008), we expect HLC variation to reflect a more flexible response to environmental uncertainty (Nettle, 2010). Life history theory posits that individuals face trade-offs between investing limited resources across fitness-relevant functions, including growth, somatic maintenance and reproduction, in ways that maximize fitness (Stearns, 1992). As many resources cannot be allocated to multiple functions simultaneously, the emphasis of life history theory on trade-offs has been instructive in illuminating why people often make decisions that knowingly compromise long-term health for short-term fitness benefits (e.g. Hill, 1993). Life history theory predicts that living in an unpredictable environment characterized by high morbidity and mortality should lead to more present-oriented time preferences promoting the valuation of short-term benefits despite long-term costs (e.g. cigarette smoking), while discounting short-term costs that yield long-term benefits (e.g. regular exercise). Cues of poverty similarly are expected to lead to greater preference for short-term gains (Liu et al., 2012). Development of a suite of relevant psychological traits guiding preferences and decision-making, such as self-efficacy, impulsivity, self-regulation and temporal discounting, may be shaped by exposures in early life (Gale et al., 2008), though additional changes over the life course are also important (Schneider et al., 2006).
We propose that HLC, reflecting an adaptive psychological attribute affecting motivation to deliberate and pursue action to improve one’s health, will co-vary with cues of environmental unpredictability. “Exogenous” sources of morbidity and mortality reflect those that are difficult to reduce with changes in resource allocation, and are thus often viewed as unavoidable. To some extent, all causes of mortality have “endogenous” and “exogenous” components (Carnes et al., 2006; p.184), but the utility of invoking the “exogenous” quality of environmental unpredictability focuses attention on the perceived difficulty of lowering morbidity and mortality, and the great efforts necessary to reduce associated risks. For example, living in a neighborhood with a high rate of violent crime may foster perceptions of environmental harshness, even though one could relocate to a safer neighborhood. Environmental cues of unpredictability, resource shortfalls and high mortality serve to discount potential benefits of carefully planned behaviors that have long-term consequences, whereas they may enhance appeal of behaviors producing short-term rewards (e.g. risky sexual behaviors, criminal behavior) ( Pepper and Nettle, 2014). Conversely, other activities that provide longer-term benefits but that have immediate costs (e.g. adherence to a healthy diet, safe sex practices) are associated with living in a relatively stable environment (Huston and Finke, 2003).
Evidence from psychology and behavioral economics supports the notion that HLC internalization is more costly than externalization, given the greater time and effort associated with conscious planning and forethought (reviewed in Rucas and Miller, 2013). Similarly, stressors associated with poverty and a reduced sense of power may be associated with greater susceptibility to misleading cognitive biases and poor decision-making (Sheehy-Skeffington and Haushofer, 2014). A “deficit” approach to cognition views these cognitive biases as errors, whereas an evolutionary-minded interpretation suggests instead that early exposure to sustained adversity induces adaptive shifts in cognition that help individuals cope in those hostile environments (Ellis et al., 2017; p.561–562). Consistent with this “adaptive resilience” approach, individuals in high stress contexts outperform others in abilities that would likely be beneficial in a hostile environment, including vigilance, tracking, memory retention for negative events, and attention shifting (Ellis et al., 2017; p. 566). A relatively predictable environment with lower mortality risk should favor greater internalized HLC due to greater perceived longer-term payoffs from investing in health. Such investment requires greater sense of control and ability to self-regulate in ways that realize delayed gains at short-term cost. In contrast, a more unpredictable environment should favor greater externalized HLC and greater temporal discounting of investing in health. Experiments show that low levels of control predict reduced ability to focus on concrete goals (Keltner et al., 2003), greater belief that goals are unattainable (Anderson and Galinsky, 2006), reduced motivation to realize goals (Galinsky et al., 2003), and greater future discounting (Joshi and Fast, 2013). Thus, we expect patterned variability in HLC, and we expect this variability to influence treatment seeking and acquisition.
1.3. Study goals and predictions
We explore determinants of treatment uptake among Tsimane Amerindians, an indigenous population of the Bolivian Amazon. Tsimane are forager-farmers experiencing high mortality (life expectancy at birth [1990–2002]=54.1), high fertility (total fertility rate=9), and varying degrees of modernization. First, we compare Tsimane HLC to two age-matched samples from industrialized populations experiencing lower morbidity and mortality. We then examine whether HLC among Tsimane is associated with use of modern and traditional treatment, independently of modernization (operationalized by educational capital and residential distance from the closest market town). Lastly, we assess whether the effect of modernization on treatment uptake is mediated by differences in HLC. We hypothesize that the perceived controllability of health behaviors and outcomes, and therefore treatment uptake, will vary in response to local cues of environmental unpredictability. Using between- and within-population comparisons, we test the following six predictions of variation in HLC (P1–P2) and treatment uptake (P3–P6):
P1: Relative to industrialized populations, Tsimane scores on Internal HLC are lower, and their scores on Chance and Powerful others HLC are higher.
P2: Access to modern healthcare and exposure to biomedical models of health may lead some individuals to develop an internalized HLC. Thus, within Tsimane, we predict that living farther from town is associated with lower Internal and greater Chance HLC. Conversely, we predict educational attainment is associated with greater Internal and lower Chance and Spirits HLC. Traditional Tsimane beliefs about illness etiology can invoke forest spirits, sorcery or poisoning (Gurven et al., 2007). Thus, we also predict Spirits HLC to be positively associated with residential distance from town and negatively associated with educational attainment. To the extent that Powerful others HLC pertains to physicians, we predict that Powerful others will be negatively associated with residential distance from town and positively associated with educational attainment.
P3: Treatment uptake (modern and/or traditional) is positively associated with Internal, and negatively associated with Chance HLC.
P4: Due to the growing influence of Christian missionaries among Tsimane since the 1950s (Gurven et al., 2007), Tsimane seem to increasingly endorse the belief that “Supreme Beings” such as God are responsible for health. We thus predict that modern treatment uptake is negatively associated with Chance, God and Spirits HLC, and positively associated with Internal and Powerful others HLC. We also predict that modern treatment uptake is negatively associated with distance from town and positively associated with educational attainment.
P5: Traditional treatment uptake is positively associated with Internal and Spirits HLC and residential distance from town, and negatively associated with Powerful others and God HLC, and with educational attainment.
P6: The effect of modernization on modern treatment uptake is at least partially mediated by HLC.
2. METHODS
2.1. Study population
Tsimane forager-horticulturalists reside in lowland Bolivia, Beni Department, in >90 villages ranging in size from ~50–500 residents. Compared to other local indigenous populations, Tsimane are less exposed to Bolivian nationals, despite intermittent contact with Jesuit missionaries in the late 17th and early 18th century. Tsimane experience a high pathogen burden and have little access to modern medical care. They are regularly co-infected with bacteria, viruses and intestinal parasites. Indicators of immune activation, usually in response to infection, are positively associated with depressive symptomology (Stieglitz et al., 2015). Despite improvements in life expectancy over the last two decades, there was only a relatively small decrease in infant mortality rates from the period 1950–89 to 1990–2002 (Gurven et al. 2007). Infectious diseases are the major cause of death, while chronic degenerative diseases are still rare (Kaplan et al., 2017).
Villages vary in degree of modernization; modern healthcare is largely limited to a small municipal hospital and pharmacies in the nearest market town of San Borja, a Catholic-run health post in the central Maniqui river region, and a health clinic originally organized by evangelical missionaries a few kilometers outside of San Borja. The San Borja hospital is rated “Level 1”, providing basic attention and routine surgeries by general practitioners. Attention from specialists requires transportation to larger cities, including Trinidad (~6–8 hours from San Borja by road).
This study was conducted as part of the Tsimane Health and Life History Project (THLHP; http://www.unm.edu/~tsimane). Since 2002 the THLHP has collected demographic, biomedical and socioeconomic data, while providing medical assistance to Tsimane (see Gurven et al., 2017). Data was collected between 2008 and 2012. All study procedures were approved by the IRB at the University of California-Santa Barbara, the Tsimane governing council (Gran Consejo Tsimane), village leaders in community meetings, and study participants.
2.2. Health locus of control (HLC)
Tsimane HLC was assessed using a previously used HLC scale (Wallston et al., 1978) that was translated from Spanish into Tsimane, and then back-translated to ensure consistency. It contains 18 items classified into three sub-scales assessing Internal HLC (e.g. “If you are sick, do you think that the things that you do will quickly return you to health?”), Chance HLC (e.g. “You think that luck is important in whether you quickly recuperate from illness.”) and Powerful others HLC (e.g. “You think that frequently visiting doctors is the best way to avoid being sick.”) dimensions on a six point Likert scale (1=fully disagree to 6=fully agree) which has been successfully used in past Tsimane research (Gurven et al., 2013; Stieglitz et al., 2015) (see Electronic Supplementary Materials [ESM] section 1[INSERT LINK TO ONLINE FILE]). The sample consists of 957 participants (age range: 40–89 years; 52% female). To control for possible response biases, we eliminated from our sample participants who consistently gave highly positive or highly negative answers across all HLC sub-scales (ESM section 2) resulting in a final sample of 690 participants. 95% of the 153 participants who consistently gave highly positive answers were men, whereas all participants who consistently gave highly negative answers (N=114) were women. Participants who gave highly valenced answers (N=267) also had, on average, a lower level of educational attainment relative to the remainder of the sample suggesting they may have had more difficulty understanding the questions or response scale. They did not significantly differ from the remainder of the sample with regards to socio-demographics (ESM section 2). Apart from the Internal HLC subscale, which had a relatively low Cronbach α of 0.51, α for Chance and Powerful others HLC was 0.61 and 0.73, respectively (ESM section 2), which is comparable to those in Wallston’s original HLC data (0.67–0.77). To consider whether Tsimane health beliefs and decision-making are influenced by forest spirits or the Judeo-Christian God, God HLC (e.g. “If my health worsens, it is up to God if I get better again.”) and Spirits HLC (e.g. “If my health worsens it’s the spirits who can make me feel better again.”) were assessed with four additional questions. In total, the Tsimane HLC questionnaire contained 22 items; sub-scale items were summed to create HLC scores along five dimensions: Internal, Chance, Powerful others, God, and Spirits HLC (ESM section 1[INSERT LINK TO ONLINE FILE]).
An exhaustive search using the keyword “health locus of control” on Google Scholar and PubMed was conducted to find studies using a comparable HLC questionnaire and age-matched comparative samples. The search rendered only two studies, from Japan and the UK, hereby respectively: the “Miyagi study” (Kuwahara et al., 2004), and the “the Caerphilly study” (Poortinga et al., 2008). Gurven et al. (2007) estimated a Tsimane life expectancy at birth of 54.1 years in for the period 1990–2002 compared to 76.6 years during the same time period for the Caerphilly sample, and 81.2 years for the Miyagi sample. Other factors including standard of living, residential environment, rates and types of disease, vulnerability to natural disasters, and access to healthcare vary greatly among these populations. Caerphilly is a largely rural county in South Wales, UK, and is home to at least six hospitals and numerous health care facilities. One study estimated that the median drive-time was 12.3 minutes (range= 0–24 minutes) from 559 census output areas defined by the 2001 Census to the nearest hospital in the area (Fone et al., 2006). Caerphilly residents experience lower levels of literacy relative to other UK regions (National Assembly for Wales, 2003), but according to government statistics for the years 2008–09, only 1.4% of 15 year-old pupils leave full-time education without a degree or qualification (National Assembly for Wales, 2010). Miyagi residents are also from a largely rural area in Japan, which has 115 hospitals, 1,616 clinics and 5,149 practicing physicians (Statistics Japan, 2017). The basic education level in Japan is higher overall than in Europe and the USA, and less strongly associated with income (Anzai et al., 2000). Even though earthquakes and tsunamis are frequent and have a considerable impact, Japan is highly prepared. The impact and significance of natural disasters such as floods and landslides are greater in developing countries such as Bolivia (Alcantara-Ayala, 2002).
We used a sub-sample of Tsimane data including participants aged 45–74 years (n=645) to match the age range of the samples in these comparative UK and Japanese studies; we compared weighted averages by age of HLC scores using the Tsimane sample as a baseline (ESM section 3).
2.3. Treatment uptake
As part of the THLHP’s focus on age-related change in adult health, including clinical diagnoses and treatment, adult participants (n=1,624 observations for 812 individuals; age range: 40 – 90 years) were queried in 2008–2012 about illnesses they experienced in the month prior to annual THLHP community visits. To aid with recall, participants were prompted with a list of common illnesses, and for each one the participant experienced, the participant described illness severity and type of treatment used (if any). An illness was considered “very minimal” if it did not prevent the participant from performing daily tasks, and if he/she stated that the illness did not require treatment because it would quickly resolve itself. These very minimal ailments (n=329 observations) were excluded from analysis, resulting in a final sample of 1,295 observations for 665 individuals (age range: 40 – 90 years; 54% female) which were then matched to the HLC data.
Illnesses were grouped into four categories: respiratory infection (42.8%), trauma (11.7% of cases), diarrhea and other gastrointestinal problems (20.8%), and other illnesses (24.7%). Two general treatment modalities were considered: modern (i.e. care received at a hospital or clinic, or receipt of drugs from a pharmacy or itinerant merchant) and traditional (i.e. medicinal plants or care received from a traditional healer). Tsimane have a rich ethno-pharmacological inventory of over 230 plants and animal parts with reported medicinal applications (Reyes-García et al., 2005). While shamans (cocojsi) are currently rare, Tsimane often seek out elders for advice or treatment regarding a wide range of illnesses. Though ‘evil eye’ and other forms of sorcery are still invoked emically as causes of sickness, beliefs about whether modern treatment is effective against illnesses of presumed supernatural origin are variable. Tsimane often report travel costs as constraints affecting decisions to utilize modern treatment in town.
2.4. Indicators of modernization
Modernization is proxied by residential distance from town and educational capital. Distance from town was measured in kilometers from the village center to San Borja as the crow flies. This measure is strongly positively correlated (Pearson r=0.87; p<0.001) with another measure of distance based on actual travel routes along rivers or roads between villages and San Borja, which was not used in analysis (ESM section 4). Educational capital (range: 0–6) is a three-item composite summing the participant’s Spanish fluency (0=none, 1=some, 2=fluent), literacy (0=none, 1=some, 2=literate) and years of schooling (0= none, 1= 1–5 years, 2= >5 years) (ESM section 5).
2.5. Data analysis
Analyses were conducted using R version 3.4.1. We used Welch’s t-test to compare mean HLC scores across populations (P1). We performed linear mixed model regressions ( lme4 R package) and conducted separate regressions for each of the nine outcomes (five HLC scales and four treatment types), including individual ID as a random effect for robust standard errors. We used the linear mixed effects model function ( lmer) for the continuous HLC outcomes (P2), and the generalized linear mixed effects model function ( glmer) for the binary treatment uptake outcomes (P3–P6). Summed HLC scales were transformed into z-scores, and we control for age, sex (0=female, 1=male), and whether individuals self-identify as Christian in all models of HLC. For models of treatment uptake, we compare models based on AIC, starting with baseline models predicting the probability of receiving treatment (controlling for age and illness type). We then tested for effects of HLC and modernization proxies on treatment uptake, first separately, and then together in final models comprising all variables (P3–P6). We repeat the same procedure with all treatment modalities: any treatment, specifically modern or traditional treatment, or both modern and traditional treatments (see ESM section 6 for further details).
3. RESULTS
3.1. Descriptives
Mean and SD scores on the HLC scales are shown in Table 1. Mean Chance HLC, Powerful others and God HLC are higher (respectively 16%, 37%, and 50%) than the Internal HLC. Mean Spirits HLC is lower (53%) than Internal HLC. Women, on average, score lower than men in Internal, Chance, Powerful Others and God HLC (respectively 10%, 7%, 6% and 5% lower), but higher (3%) on Spirits HLC.
Table 1.
Mean (SD) Tsimane HLC by sex and age
| HLC scale | Internal (range 6–36) | Chance (range 6–36) | Powerful others (range 6–36) | God (range 6–36) | Spirits (range 6–36) |
|---|---|---|---|---|---|
|
| |||||
| All (n=690) | 19.29 (4.77) | 22.38 (4.89) | 26.74 (4.18) | 28.99 (7.26) | 9.10 (4.79) |
| Sex | |||||
| Female(n=367) | 18.33 (4.71) | 21.57 (4.71) | 25.92 (4.41) | 28.34 (8.00) | 9.21 (4.73) |
| Male (n=323) | 20.37 (4.6) | 23.3 (4.93) | 27.68 (3.69) | 29.72 (6.24) | 8.98 (4.86) |
| Age | |||||
| 40–49 (n=340) | 19.63 (4.81) | 22.45 (4.77) | 26.67 (4.14) | 28.73 (7.18) | 9.34 (5.21) |
| 50–59 (n=164) | 18.93 (4.84) | 21.51 (4.81) | 26.67 (4.25) | 29.60 (6.85) | 9.22 (4.67) |
| 60–69 (n=122) | 19.25 (4.57) | 23.53 (5.07) | 27.06 (3.83) | 29.16 (7.12) | 8.45 (3.95) |
| 70–79 (n=48) | 18.17 (4.67) | 21.75 (5.17) | 26.48 (4.96) | 28.12 (8.54) | 8.68 (4.02) |
| 80–89 (n=16) | 19.31 (4.74) | 22.62 (4.44) | 27.50 (4.77) | 29.44 (9.87) | 9.20 (4.87) |
Slightly more men (37.5%) than women (33.0%) seek modern treatment, whereas traditional treatment seeking is similar across the sexes (women: 38.1%, men: 36.8%). Participants residing >70 km from town receive traditional treatment for 55.2% of illnesses and modern treatment for 14.7% of illnesses, while those living near town (<30 km) receive traditional and modern treatment for 37.9% and 39.1% of illnesses, respectively (see ESM section 7 for further details on socio-demographic covariates of treatment uptake and treatment by illness type). Fully adjusted models, however, show no sex or age-related differences in treatment uptake, whereas living farther from town is associated with reduced likelihood of receiving modern treatment (Table 2).
Table 2. Predictors of modern treatment uptake.
Effects are given as odds ratios, and models adjust for age, sex, and illness type. See ESM section 12 for complete model summaries.
| HLC (z-scores) | Modernization | |||||||
|---|---|---|---|---|---|---|---|---|
| Internal | Chance | Powerful Others | God | Spirits | Distance from town (km) | Educational Capital (z-score) | ||
| Model 2: Baseline +HLC | Exp(β) (p-value) | 0.994 (0.935) | 0.837 (0.013) | 1.306 (0.000) | 1.072 (0.339) | 1.017 (0.801) | ||
| Model 3: Baseline+Modernization | Exp(β) (p-value) | 0.989 (0.001) | 1.029 (0.734) | |||||
| Model 4: Full | Exp(β) (p-value) | 1.047 (0.576) | 0.761 (0.001) | 1.332 (0.000) | 1.095 (0.317) | 1.024 (0.737) | 0.928 (0.003) | 1.058 (0.521) |
3.2. Tsimane have less internalized and more externalized HLC than industrialized populations (P1)
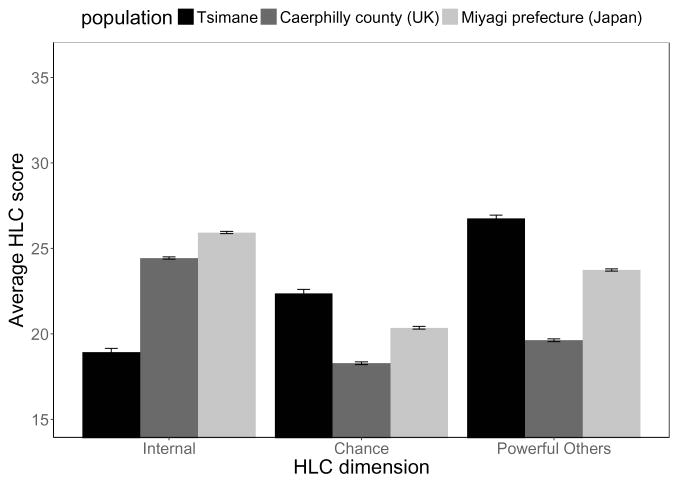
Mean Internal HLC score for Tsimane (18.93; n=645) is 23% lower (p<0.001) than the Caerphilly score (24.44; n=6,177) and 27% lower (p<0.001) than the Miyagi score (25.93; n=4,030). Conversely, for Chance HLC, average Tsimane score (22.37) is 18% higher (p<0.001) than the Caerphilly score (18.29), and 10% higher (p<0.001) than the Miyagi score (20.36). Powerful others HLC is 36% higher (p<0.001) and 13% (p<0.001) higher among Tsimane (26.76) than among Caerphilly (19.63) and Miyagi (23.74) samples (Figure 1; ESM section 3).
Figure 1. Mean (+SE) HLC across three populations (HLC range: 6–36).
Note: comparisons only exist for Internal, Chance and Powerful others HLC.
N=645 Tsimane (e0=54.1 in 2000); N=6,177 for the UK sample (e0=76.6 in 2000) from Poortinga et al. (2008); and N=4,030 for the Japanese sample (e0=81.2 in 2000) from Kuwahara et al. (2004).
3.3. Within Tsimane effects of modernization on HLC are mixed (P2)
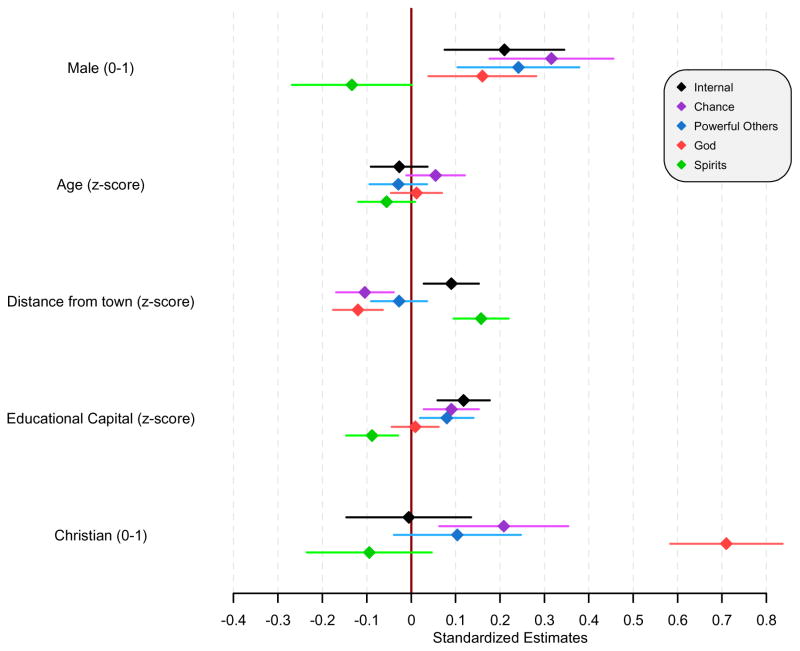
3.3.1. Distance from town
Contrary to P2, participants living farther from town have higher Internal and lower Chance HLC (Figure 2, table ESM section 8). Effect sizes, however, are small: the Internal HLC of adults from the most remote village (82 km from town) is higher than that of adults from the closest village (5 km) by only 0.21 SDs (β=0.002); their Chance HLC is lower by only 0.19 SDs (β=−0.003). Adults living farther from town have lower God and Powerful others HLC, and higher Spirits HLC (Figure 2, table ESM section 8). Effects sizes, however, are also small: 0.16 SDs (β=−0.002) for the Powerful others HLC contrasting individuals living in the farthest vs. closest villages, 0.19 SDs (β=−0.002), for God HLC and 0.07 SDs (β=0.001) for Spirits HLC (Figure 2; ESM section 8).
Figure 2. Predictors of HLC.
Standardized estimates from linear mixed models of the relationship between modernization proxies and the five HLC dimensions, indicated by the diamonds; bars denote 95% CIs. See ESM section 8 for parameter estimates.
3.3.2. Educational capital
The effect of educational capital is positive and significant for Internal (β=0.113) and Powerful others HLC (β=0.087), negative and significant for Spirits HLC (β=−0.086), but not significantly associated with either Chance or God HLC (Figure 2; ESM section 8). We also tested for a distance to town-by-educational capital interaction effect but it was not significant.
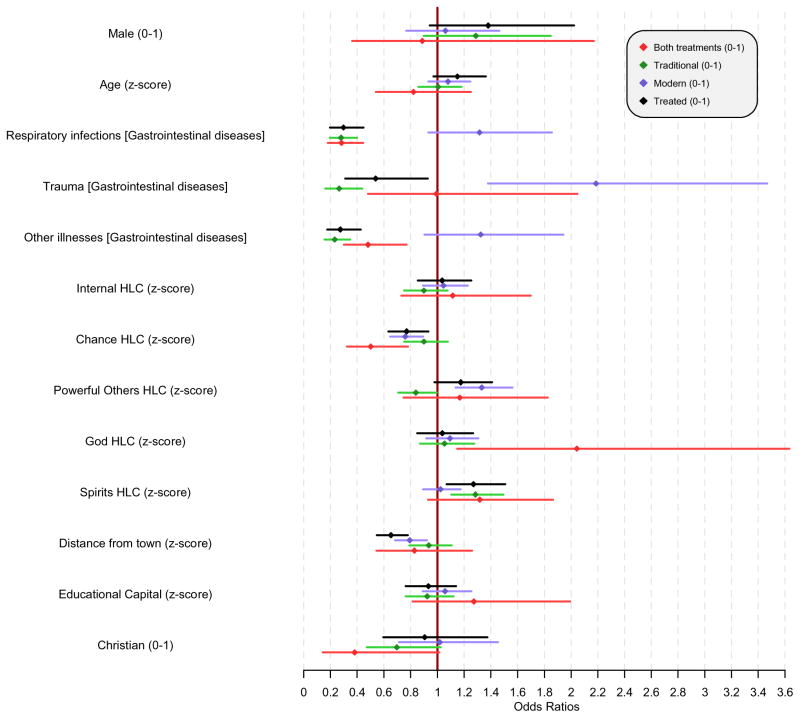
3.4. Chance but not Internal HLC is associated with treatment uptake (P3)
Figure 3 summarizes results of models estimating effects of Chance and Internal HLC on treatment uptake. Each SD unit increase in Chance HLC is associated with 23% lower odds of receiving any treatment, 24% lower odds of receiving modern treatment, and 50% lower odds of receiving both modern and traditional treatments. The association between all types of treatment uptake and Internal HLC is positive but not significant in any model (Figure 3; ESM sections 9–13).
Figure 3. Best fit models for treatment uptake.
Odds ratios for the association between modernization proxies, the five HLC dimensions, and treatment uptake; bars denote 95% CIs. See ESM section 10 for parameter estimates.
3.5. Greater Powerful others HLC, reduced Chance HLC, and town proximity are each associated with modern treatment uptake (P4)
Each SD unit increase in Powerful others HLC is associated with 33% higher odds of modern treatment uptake; odds of modern treatment use are 17% lower for each additional 10 km one lives from town (2% per km)(Figure 3; Table 2: Model 4). In addition, a SD unit increase in Chance HLC is associated with 24% lower odds of modern treatment uptake. Internal, God and Spirits HLC, and modernization proxies, show no significant associations with modern treatment uptake (Figure 3; Table 2: Model 4; ESM section 11).
3.6. Reduced Powerful others and greater Spirits HLC are associated with traditional treatment uptake (P5)
Each SD unit increase in Powerful others HLC is associated with 16% lower odds of traditional treatment uptake, whereas each SD unit increase in Spirits HLC is associated with 29% higher odds. No other HLC score is associated with traditional treatment uptake, and its association with modernization proxies is in the expected direction but not significant (Figure 3, ESM section 12).
3.7. Effect of modernization on modern treatment uptake is not mediated by HLC (P6)
The effect of distance from town on modern treatment uptake does not diminish with inclusion of Powerful others and other HLC scales (Table 2: Models 3, 4), indicating that HLC does not mediate this effect. In fact, the effect of distance to town is stronger after adjusting for HLC scales (OR=0.989 to OR=0.794). It is noteworthy that educational capital is not associated with modern treatment uptake in any of the models. Similarly, there is no mediation effect of HLC on any other treatment outcome (ESM sections 10–13).
4. DISCUSSION
We assessed whether variation in HLC, a psychological construct aimed to capture control with respect to health, explains variation in treatment uptake among Tsimane Amerindians. Given the Tsimane ecological context of high mortality and morbidity, we first explored whether Tsimane HLC perceptions differ from those living in two industrialized settings characterized by low morbidity and mortality. We then investigated whether, among Tsimane, HLC predicts treatment uptake, and whether it mediates the relationship between modernization and treatment uptake. A guiding motivation of this study was to test whether the decision to treat common illnesses when multiple traditional and modern treatments are available is affected not just by treatment access and familiarity, but also by a psychological orientation shaped by living in a harsh, unpredictable environment. Rather than rely on a binary contrast between “internal” and “external” locus, we employed a locus of control measure specifically oriented toward health behaviors, including HLC sub-scales decomposing external others in meaningful ways. We found that multiple external HLC sub-scales – including Chance, Powerful others, God and Spirits – independently predicted different treatment outcomes. Importantly, best fit models for treatment uptake summarized in the ESM (section 9) included all HLC scales measured, suggesting that a dichotomous score would have been inadequate. Several HLC sub-scales are weakly positively correlated with each other (ESM section 1), further supporting the notion that HLC may not fall neatly on a spectrum from “highly internal” to “highly external”. Instead, our results are consistent with other findings where individuals simultaneously hold beliefs suggestive of both internal and external HLC (Poortinga et al., 2008).
Consistent with P1, we found that Tsimane show lower Internal HLC, and higher Chance and Powerful others HLC than age-matched samples from Japan and the UK. Despite this being a limited comparison, this result is consistent with the notion that an externalized locus is a response to living in an unpredictable environment whereby responsibility for health outcomes is attributed to external forces such as luck or fate, and that more stable environments favor a more internalized locus. In the early 2000s, Tsimane life expectancy was 22.5 years lower than in Caerphilly (UK) and 27.1 years lower than in Miyagi (Japan). Compared to these industrialized populations, Tsimane have much less access to healthcare and lower levels of schooling. Tsimane also lack access to health-related information (e.g. disease etiology, recommended hygienic practices independent of modern technology) that can inform health psychology and decision-making, largely due to geographical, linguistic and cultural barriers, financial limitations, and lower levels of formal schooling, especially among older adults (Gurven et al., 2017, 2007). In addition, to the extent that Tsimane are able to access medical care in town, they also face discrimination by Bolivian nationals, including medical professionals, who often do not provide them with the same level of care and information that other non-Tsimane Bolivian patients receive. Even in the absence of discrimination, available modern medical care for Tsimane is less comprehensive than that found in the UK and Japan. As a result, Tsimane appear to be less likely to ascribe fluctuations in their health to variation in their own preventative or curative behavior (e.g. boiling river water before drinking, cleaning and dressing wounds), and instead appear to be more likely to ascribe such fluctuations to external entities, including happenstance, supernatural beings, or professional medical interventions.
Contrary to P2, living farther from town is associated with higher Internal HLC and lower Chance HLC, suggesting that adults residing farther away from town are more likely to believe in their own ability to affect their health. One possible explanation is that living near non-Tsimane Bolivians in town may promote perceptions of inequality and lower relative wealth, and possibly lower sense of control and self-efficacy, despite objectively greater access and health status. Tsimane often face ethnic discrimination in town hospitals and pharmacies, although even in the absence of discrimination, they are severely resource-limited and may not be able to afford the same level of healthcare received by other Bolivians. Greater interactions with Bolivians combined with ethnic discrimination may reduce feelings of self-control over health outcomes, and perhaps exacerbate perceptions of poor health. Consistent with this view, a study in the Peruvian Amazon revealed that self-reported health and well-being declined substantially over a period of several decades among Matsigenka Amerindians despite objective health improvements (Izquierdo, 2005). This discrepancy was attributed to negative experiences with greater modernization, more permanent settlement, and greater interaction with outsiders. Whether a similar pattern exists among Tsimane when comparing subjective and objective measures of health in relation to modernization is currently under investigation.
As expected, God HLC is higher among adults living closer to town (P2), likely reflecting the greater influence of evangelical missionaries and mainstream religious culture near town. The evangelical missionaries had a long-term presence in several villages near town, and their domain of influence is strongest among nearby villages. On the other hand, Spirits HLC was higher among participants living in more remote villages, where traditional spiritual and religious beliefs are more common, and less sanctioned by Protestant or Catholic presence. We note, however, that even in villages close to town, many Tsimane still hold traditional beliefs about sorcery and forest spirits.
Educational capital was associated with higher Powerful Others and Internal HLC (Figure 2; ESM section 8). Effects of education on HLC may be two-fold. First, education confers economic advantage which may buffer against unhealthy lifestyle choices and their harmful effects on health directly. Second, formal education may facilitate acquisition of positive attitudes about health, familiarity with the modern healthcare system and institutions, exposure to biomedical models of health hazards, and easier communication with healthcare professionals. This, in turn, may confer a higher sense of control over health outcomes and better quality of care, resulting in different decision-making patterns with regards to treatment uptake or preventative behaviors (Cutler and Lleras-Muney, 2006). Together, these explanations may shed light on why more educated Tsimane place greater faith in their ability to affect their own health.
Our results do not indicate that Internal HLC is associated with treatment uptake (P3). Instead, those displaying high Powerful others HLC and low Chance HLC are more likely to report modern treatment uptake (Table 2; Figure 3; ESM sections 9,11), while those scoring higher for Powerful others and Spirits HLC are more likely to report traditional treatment uptake (Figure 3, ESM sections 9,12). Consistent with findings by Pepper and Nettle (2014) who find that only extrinsic mortality risk perceptions are associated with health effort, these results suggest that the lack of motivation to pursue treatment for high Chance HLC individuals may be a result of high levels of perceived uncontrollable mortality (i.e. extrinsic), which can alter the payoff to investing in health even where it is controllable. These results also highlight that Internal HLC is not necessarily the best predictor of treatment uptake. Among the Tsimane, a belief in the importance of physicians and nurses (reflected in Powerful others HLC) may be more important than a belief in one’s own ability to affect one’s health when deciding whether and how to treat illness. It is also plausible that experience of receiving treatment itself can increase one’s Powerful others HLC, since this sub-scale is based on questions related to physician efficacy.
Consistent with P3, higher Chance HLC is associated with reduced modern treatment uptake. Thus, while Tsimane as a population have higher Chance HLC than two industrialized populations, even among Tsimane, those scoring higher may be even more sensitive to living in an unpredictable environment, and therefore less willing to expend resources to improve their own health. Tsimane with a higher Spirits HLC are more likely to receive traditional treatment, likely reflecting their faith in traditional beliefs more generally.
Aside from HLC, the variable most strongly associated with modern treatment uptake was residential distance from town (P4), which serves as a proxy for access to the market and modern medical facilities. Tsimane from distant communities incur significant financial and other costs (e.g. opportunity costs linked to reduced subsistence effort) to reach town for modern treatment.
Despite the effects of educational capital on HLC, we did not find any evidence that educational capital was associated with treatment uptake (modern or traditional), or that educational capital interacts with town proximity to affect uptake. Knowledge alone therefore does not lead to treatment uptake, whereas other factors such as limited treatment access and psychological orientation related to self-efficacy are more important. Our study was limited to adults aged 40+ years who would have had relatively low levels of exposure to formal schooling, and so perhaps including a broader range of educational exposures might have yielded different results. Nonetheless, the limited range of schooling we do find is associated with the Powerful Others and Internal HLC (P2). While limited access to town is generally expected to reduce motivation for modern treatment uptake, our finding that educational capital is less important than HLC is striking and merits further study.
Residential distance from town is not associated with traditional treatment uptake (P5). Although knowledge of some traditional remedies appears to be greater in more remote communities (Reyes-García et al., 2005), our results do not indicate that this affects patterns of traditional treatment uptake (Figure 3; ESM section 12). Our results also suggest that Tsimane do not consider modern treatment to substitute for traditional treatment, but instead consider the former to complement the latter. Similar mixing of traditional and modern treatments have been reported in other populations (Giordano et al., 2004).
Despite our prediction that HLC would at least partially mediate the relationship between modernization and treatment uptake (P6), we found no evidence of mediation (Table 3; ESM sections 10–13); HLC and modernization instead exerted independent effects on treatment uptake.
4.1. Study limitations
First, the cross-sectional design prevents strong casual inference, and does not preclude reverse causality. We found that Powerful others HLC is significantly associated with modern treatment uptake. It is not clear whether this means that HLC beliefs affect treatment uptake or vice versa; most likely the relationship operates in both directions. Future research on changes in Powerful others HLC and other HLC sub-scales following treatment could help shed light on this question. Second, the current HLC is based on a number of established scales with reasonable internal validity, but a greater set of similar instruments assessing self-efficacy could add robustness to our HLC measurements. Second, we have excluded a relatively large number of participants from our study (N=267) to avoid response bias in the HLC results. The excluded participants had, on average, a lower level of educational attainment relative to the remainder of the sample suggesting they may have had more difficulty understanding the questions or response scale. Third, the decision to treat an illness may not always be made by the focal individual whose traits we link to having received a particular course of treatment. Instead, others (e.g. a spouse, children) may offer to procure medicinal plants, or offer to obtain assistance at a clinic, pharmacy or hospital in town. Given our focus on adults aged 40+ years, the opinions of focal adults are likely taken into consideration even when decisions may be influenced by others. Fourth, our cross-cultural comparison was based on only two other samples representative of industrialized populations, due to the unavailability of additional comparable data. Population-level comparisons of this sort are subject to the usual caveats with comparative work, as one cannot be sure that participants from different cultural backgrounds employ the same goalposts in their subjective evaluations using Likert-type scales. Lastly, our study is limited by not having systematically studied beliefs and perceptions of the effectiveness of different treatments for the common debilitating illnesses assessed here. Our proxy measures of modernization may also not fully capture the extent to which modernization buffers against environmental unpredictability. Future research should also more directly assess perceptions of environmental harshness and stochasticity, such as perceived disease risk, material wealth, and access to clean water, in relation to health behaviors.
4.2. Conclusion
One reason indigenous populations like the Tsimane suffer higher morbidity and mortality rates than neighboring non-indigenous populations is the limited access to public health infrastructure. It is often believed that greater education is a powerful tool to equip and empower indigenous peoples to take better advantage of existing resources. While we show that greater schooling and language competence are associated with several HLC scales, they are not by themselves associated with treatment uptake. Instead, our results are consistent with a life history theoretical framework which proposes that environmental harshness and unpredictability promotes a psychology favoring temporal discounting that reduces motivation to invest in health. We find that Powerful others and Chance HLC are strongly predictive of treatment uptake. In particular, higher Powerful others HLC is associated with modern treatment uptake, while higher Chance HLC is inversely associated with modern treatment. Internal HLC, an important predictor of motivation to pursue treatment in industrialized populations, does not predict treatment uptake among Tsimane. It is possible that Internal HLC may not be the most relevant aspect of HLC cross-culturally, especially in populations where medical care is perceived as esoteric and/or where supernatural and more traditional factors are believed to contribute to health above and beyond individual behavior. The fact that a high Chance HLC is strongly associated with reduced modern treatment uptake suggests that individuals who believe their health is influenced by factors beyond their personal control might be less motivated to invest in health. This study also indicates that while physical access to healthcare, in the form of reduced distance from modern healthcare facilities, does play an important role in predicting treatment uptake, HLC appears to play an independent role. Notably, individuals with high Chance HLC and low Powerful others HLC are less likely to seek treatment. Facilitating access, improving familiarity with the modern healthcare system, and increasing trust in physicians may help motivate Tsimane to visit modern healthcare facilities. After the THLHP helped employ a bilingual Tsimane health promoter fluent in Spanish in the San Borja hospital, Tsimane visits to the hospital increased, and many have since reported to us that they now feel more comfortable at hospital.
At the population level, Tsimane scored higher in Chance and Powerful others HLC, and lower in Internal HLC than age-matched UK and Japanese samples. This supports the notion that a more externalized locus is a response to living in an unpredictable environment where mortality and morbidity are affected by factors beyond individual control, whereas stable environments favor an internalized locus as they provide more opportunities for attributing positive health to one’s own doing. Though preliminary, these findings are consistent with experimental and other evidence in industrialized populations showing the effects of unpredictability and environmental harshness on different aspects of cognition and psychological motivation.
Supplementary Material
Research highlights.
HLC is a strong predictor of treatment uptake for high morbidity-mortality Tsimane.
External but not Internal HLC associates with healthcare treatment uptake.
An externalized locus may be a rational response to environmental unpredictability.
Education is positively associated with HLC but does not predict treatment uptake.
Modern treatment is complementary to traditional options, not a substitute.
Acknowledgments
We would like to thank the Tsimane for their hospitality and collaboration; the Gran Consejo Tsimane; the members of the Tsimane Health and Life History Project; Edmond Seabright and three anonymous reviewers for their helpful comments.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alcantara-Ayala I. Geomorphology, natural hazards, vulnerability and prevention of natural disasters in developing countries. Geomorphology. 2002;47(2):107–124. [Google Scholar]
- Anderson C, Galinsky AD. Power, optimism, and risk-taking. European Journal of Social Psychology. 2006;36:511–536. [Google Scholar]
- Anzai Y, Ohkubo T, Nishino Y, Tsuji I, Hisamichi S. Relationship between health practices and education level in the rural Japanese population. Journal of epidemiology. 2000;10(3):149–156. doi: 10.2188/jea.10.149. [DOI] [PubMed] [Google Scholar]
- Bobak M, Pikhart H, Rose R, Hertzman C, Marmot M. Socioeconomic factors, material inequalities, and perceived control in self-rated health: cross-sectional data from seven post-communist countries. Social Science & Medicine. 2000;51:1343–1350. doi: 10.1016/s0277-9536(00)00096-4. [DOI] [PubMed] [Google Scholar]
- Burker EJ, Evon DM, Galanko J, Egan T. Health Locus of Control Predicts Survival after Lung Transplant. Journal of Health Psychology. 2005;10:695–704. doi: 10.1177/1359105305055326. [DOI] [PubMed] [Google Scholar]
- Callaghan P. Social support and locus of control as correlates of UK nurses’ health-related behaviours. Journal of Advanced Nursing. 1998;28(5):1127–1133. doi: 10.1046/j.1365-2648.1998.00811.x. [DOI] [PubMed] [Google Scholar]
- Calnan M. Control over health and patterns of health-related behaviour. Social Science & Medicine. 1989;29(2):131–136. doi: 10.1016/0277-9536(89)90161-5. [DOI] [PubMed] [Google Scholar]
- Carnes BA, Holden LR, Olshansky SJ, Witten MT, Siegel JS. Mortality Partitions and their Relevance to Research on Senescence. Biogerontology. 2006;7:183–198. doi: 10.1007/s10522-006-9020-3. [DOI] [PubMed] [Google Scholar]
- Cutler D, Lleras-Muney A. Education and Health: Evaluating Theories and Evidence. Cambridge, MA: 2006. [Google Scholar]
- Duffy ME. Determinants of reported health promotion behaviors in employed Mexican American women. Health Care for Women International. 1997;18:149–163. doi: 10.1080/07399339709516270. [DOI] [PubMed] [Google Scholar]
- Ellis BJ, Bianchi J, Griskevicius V, Frankenhuis WE. Beyond Risk and Protective Factors: An Adaptation-Based Approach to Resilience. Perspectives on Psychological Science. 2017 doi: 10.1177/1745691617693054. [DOI] [PubMed] [Google Scholar]
- Fone DL, Stephen C, Lester N. Comparison of perceived and modelled geographical access to accident and emergency departments: a cross-sectional analysis from the Caerphilly Health and Social Needs Study. International Journal of Health Geographics. 2006;119:738–742. doi: 10.1186/1476-072X-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford JD, Berrang-Ford L, King M, Furgal C. Vulnerability of Aboriginal health systems in Canada to climate change. Global Environmental Change. 2010;20:668–680. doi: 10.1016/j.gloenvcha.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale CR, Batty GD, Deary IJ. Locus of Control at Age 10 Years and Health Outcomes and Behaviors at Age 30 Years: The 1970 British Cohort Study. Psychosomatic Medicine. 2008;70:397–403. doi: 10.1097/PSY.0b013e31816a719e. [DOI] [PubMed] [Google Scholar]
- Galinsky AD, Gruenfeld DH, Magee JC. From Power to Action. Journal of Personality and Social Psychology. 2003;85:453–466. doi: 10.1037/0022-3514.85.3.453. [DOI] [PubMed] [Google Scholar]
- Giordano J, Garcia MK, Strickland G, Chen YC, Chou LF, Chen FJ, Hwang SJ, Anderson R. Integrating Chinese Traditional Medicine into a U.S. Public Health Paradigm. The Journal of Alternative and Complementary Medicine. 2004;10:706–710. doi: 10.1089/acm.2004.10.706. [DOI] [PubMed] [Google Scholar]
- Gurven M, Kaplan H, Supa AZ. Mortality experience of Tsimane Amerindians of Bolivia: Regional variation and temporal trends. American Journal of Human Biology. 2007;19:376–398. doi: 10.1002/ajhb.20600. [DOI] [PubMed] [Google Scholar]
- Gurven M, Stieglitz J, Trumble B, Blackwell AD, Beheim B, Davis H, Hooper P, Kaplan H. The Tsimane Health and Life History Project: Integrating anthropology and biomedicine. Evolutionary Anthropology: Issues, News, and Reviews. 2017;26:54–73. doi: 10.1002/evan.21515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurven M, von Rueden C, Massenkoff M, Kaplan H, Lero Vie M. How Universal Is the Big Five? Testing the five-factor Model of Personality Variation Among Forager–Farmers in the Bolivian Amazon. Journal of Personality and Social Psychology. 2013;104:354–370. doi: 10.1037/a0030841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampson SE, Friedman HS. Handbook o, editor. Personality and health: A lifespan perspective. Guilford Press; New York: 2008. [Google Scholar]
- Hill K. Life history theory and evolutionary anthropology. Evolutionary Anthropology: Issues, News, and Reviews. 1993;2:78–88. [Google Scholar]
- Huanca T. Landscape, and Identity in Tropical Forest. 2006. Tsimane’Oral Tradition. [Google Scholar]
- Huston SJ, Finke MS. Diet Choice and the Role of Time Preference. Journal of Consumer Affairs. 2003;37:143–160. [Google Scholar]
- Izquierdo C. When “health” is not enough: societal, individual and biomedical assessments of well-being among the Matsigenka of the Peruvian Amazon. Social Science & Medicine. 2005;61:767–783. doi: 10.1016/j.socscimed.2004.08.045. [DOI] [PubMed] [Google Scholar]
- Joshi PD, Fast NJ. Power and Reduced Temporal Discounting. Psychological Science. 2013;24:432–438. doi: 10.1177/0956797612457950. [DOI] [PubMed] [Google Scholar]
- Kaplan H, Thompson RC, Trumble BC, Wann LS, Allam AH, Beheim B, Frohlich B, Sutherland ML, Sutherland JD, Stieglitz J, Rodriguez DE, Michalik DE, Rowan CJ, Lombardi GP, Bedi R, Garcia AR, Min JK, Narula J, Finch CE, Gurven M, Thomas GS. Coronary atherosclerosis in indigenous South American Tsimane: a cross-sectional cohort study. The Lancet. 2017;389:1730–1739. doi: 10.1016/S0140-6736(17)30752-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keltner D, Gruenfeld DH, Anderson C. Power, approach, and inhibition. Psychological Review. 2003;110:265–284. doi: 10.1037/0033-295x.110.2.265. [DOI] [PubMed] [Google Scholar]
- King M, Smith A, Gracey M. Indigenous health part 2: the underlying causes of the health gap. The Lancet. 2009a;374:76–85. doi: 10.1016/S0140-6736(09)60827-8. [DOI] [PubMed] [Google Scholar]
- King M, Smith A, Gracey M. Indigenous health part 2: the underlying causes of the health gap. The Lancet. 2009b;374:76–85. doi: 10.1016/S0140-6736(09)60827-8. [DOI] [PubMed] [Google Scholar]
- Kuwahara A, Nishino Y, Ohkubo T, Tsuji I, Hisamichi S, Hosokawa T. Reliability and validity of the Multidimensional Health Locus of Control Scale in Japan: relationship with demographic factors and health-related behavior. The Tohoku journal of experimental medicine. 2004;203:37–45. doi: 10.1620/tjem.203.37. [DOI] [PubMed] [Google Scholar]
- Lasker JN. Choosing among therapies: Illness behavior in the Ivory Coast. Social Science & Medicine Part A: Medical Psychology & Medical Sociology. 1981;15:157–168. doi: 10.1016/0271-7123(81)90035-3. [DOI] [PubMed] [Google Scholar]
- Liu L, Feng T, Suo T, Lee K, Li H. Adapting to the destitute situations: Poverty cues lead to short-term choice. PloS one. 2012;7:e33950. doi: 10.1371/journal.pone.0033950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macgregor IDM, Regis D, Balding J. Self-concept and dental health behaviours in adolescents. Journal of Clinical Periodontology. 1997;24(5):335–339. doi: 10.1111/j.1600-051x.1997.tb00766.x. [DOI] [PubMed] [Google Scholar]
- Murray M, McMillan C. Health beliefs, locus of control, emotional control and women’s cancer screening behaviour. The British journal of clinical psychology. 1993;32:87–100. doi: 10.1111/j.2044-8260.1993.tb01032.x. [DOI] [PubMed] [Google Scholar]
- National Assembly for Wales. 2001 Census of Population:Key Statistics for Assembly Constituencies. 2003. [Google Scholar]
- National Assembly for Wales. Key Statistics for Caerphilly. 2010. [Google Scholar]
- Nettle D. Why Are There Social Gradients in Preventative Health Behavior? A Perspective from Behavioral Ecology. PLoS ONE. 2010;5:e13371. doi: 10.1371/journal.pone.0013371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pepper GV, Nettle D. Out of control mortality matters: the effect of perceived uncontrollable mortality risk on a health-related decision. PeerJ. 2014;2:e459. doi: 10.7717/peerj.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poortinga W, Dunstan FD, Fone DL. Health locus of control beliefs and socioeconomic differences in self-rated health. Preventive Medicine. 2008;46:374–380. doi: 10.1016/j.ypmed.2007.11.015. [DOI] [PubMed] [Google Scholar]
- Quinlan RJ, Dira SJ, Caudell M, Quinlan MB. Culture and Psychological Responses to Environmental Shocks: Cultural Ecology of Sidama Impulsivity and Niche Construction in Southwest Ethiopia. Current Anthropology. 2016;57:632–652. [Google Scholar]
- Reyes-García V, Vadez V, Huanca T, Leonard W. Knowledge and Consumption of Wild Plants: A comparative study in two Tsimane’ villages in the Bolivian Amazon. Ethnobotany Research & Applications. 2005;3:201–207. [Google Scholar]
- Roddenberry A, Renk K. Locus of control and self-efficacy: Potential mediators of stress, illness, and utilization of health services in college students. Child Psychiatry and Human Development. 2010;41:353–370. doi: 10.1007/s10578-010-0173-6. [DOI] [PubMed] [Google Scholar]
- Rucas SL, Miller AA. Locus of control and sleep in evolutionary perspective. Journal of Social, Evolutionary, and Cultural Psychology. 2013;7:79–96. [Google Scholar]
- Schneider A, Körner T, Mehring M, Wensing M, Elwyn G, Szecsenyi J. Impact of age, health locus of control and psychological co-morbidity on patients’ preferences for shared decision making in general practice. Patient Education and Counseling. 2006;61:292–298. doi: 10.1016/j.pec.2005.04.008. [DOI] [PubMed] [Google Scholar]
- Sheehy-Skeffington J, Haushofer J. The behavioural economics of poverty”. Barriers to and opportunities for poverty reduction. UNDP barriers to and opportunities for poverty reduction. 2014:96–112. [Google Scholar]
- Statistics Japan: Prefecture Comparisons. 2017 Retrieved from www.stats-japan.com.
- Stearns SC. The evolution of life histories. Oxford: Oxford University Press; 1992. [Google Scholar]
- Steptoe A, Wardle J. Locus of control and health behaviour revisited: A multivariate analysis of young adults from 18 countries. British Journal of Psychology. 2001;92:659–672. doi: 10.1348/000712601162400. [DOI] [PubMed] [Google Scholar]
- Stieglitz J, Trumble BC, Thompson ME, Blackwell AD, Kaplan H, Gurven M. Depression as sickness behavior? A test of the host defense hypothesis in a high pathogen population. Brain, Behavior, and Immunity. 2015;49:130–139. doi: 10.1016/j.bbi.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallston KA, Wallston BS, DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health education monographs. 1978;6:160–170. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.