Summary
Objective
This study examined changes in mental health symptoms and weight during weight loss treatment. It was hypothesized that worsening mental health would negatively impact weight loss.
Methods
Data were analyzed from a trial of 92 Hispanic women with overweight/obesity and prediabetes, who were randomized to receive intensive lifestyle intervention (ILI), metformin 1,700 mg daily, or standard care. Depression, anxiety and perceived stress were assessed at 0, 6 and 12 months. Six‐ and 12‐month weight change was compared among participants whose symptom scores worsened on any mental health measure (W) vs. improved or remained stable on all three (I/S).
Results
Among ILI participants, the 12‐month difference in weight loss between I/S and W groups was statistically significant: −5.1 kg (P = 0.001). From baseline to 6 months, ILI participants in I/S and W groups experienced comparable weight loss. However, from 6 to 12 months, W participants regained weight, whereas I/S participants experienced continued weight loss. In the metformin and standard care arms, there was no weight difference between I/S and W groups.
Conclusions
In ILI, 12‐month improvement or stability in mental health was significantly associated with weight loss. Weight trajectories between I/S and W groups diverged at 6 months.
Keywords: Anxiety, depression, perceived stress, weight loss
Introduction
A large body of research has demonstrated the association of common mental health problems, such as depression, anxiety and stress, with excess body weight 1, 2, 3, 4, 5, 6, 7. These same psychological concerns can impair individuals' ability to successfully complete weight loss interventions 8, 9. However, knowledge about the relationship between mental health and weight loss is limited for several reasons.
First, most weight loss trials have excluded those with comorbid mental health conditions 10. Second, mental health is most often operationalized as depressive symptoms or clinical depression, providing little information about other mental health concerns or multiple mental health comorbidities. Third, trials examining the relationship between mental health and weight loss have often only assessed baseline mental health status as a predictor, yielding inconsistent findings 10. Mental health symptoms likely change during weight loss treatments, necessitating evaluations that explore their trajectories over time 11. Such evaluations may promote understanding about how and when changes in mental health impact the success of weight loss efforts.
The landmark Diabetes Prevention Program (DPP) trial highlights challenges and opportunities for examining the association of mental health with weight loss. This trial of 3,234 adults with overweight/obesity and prediabetes studied an intensive lifestyle intervention (ILI) that produced clinically significant weight loss (6.8 kg at 12 months) and a 58% reduction in the risk of developing type 2 diabetes relative to placebo 12. DPP participants randomized to receive metformin, a common antidiabetic medicine, experienced comparatively less weight loss and a lower reduction in diabetes risk. In this trial, elevated symptoms of depression and anxiety at baseline did not impact weight outcomes 13. However, participants in this study had low levels of mental health symptoms, limiting the ability to examine associations with weight loss 14. Many subsequent translational studies have used less stringent exclusion criteria and may provide unique data to investigate changes in mental health and weight loss during active treatment.
The primary objective of this analysis was to examine the association between 12‐month changes in mental health symptoms and weight in a translational DPP trial of 92 Hispanic women (Latinas) with overweight/obesity and prediabetes. Trajectories of mental health symptoms and weight change during this trial were examined using data at 0, 6 and 12 months.
Methods
PREVENT‐DM was a comparative effectiveness trial of group‐based ILI (n = 33) vs. metformin 850 mg twice daily (n = 29) vs. standard care (n = 30) among 92 Latinas with prediabetes and overweight/obesity. The ILI delivered in this study was based on the Group Lifestyle Balance Program (copyright 2008, 2010, 2011, 2017; University of Pittsburgh), which is an evidence‐supported adaptation of the original NIH/National Institute of Diabetes and Digestive and Kidney Diseases‐funded DPP 15, 16. In the current study, this intervention was delivered weekly for the first 14 weeks, followed by 10 biweekly or monthly sessions during the remainder of the trial. The metformin participants attended brief monthly study visits, during which they returned unused medication doses from the previous month and received the next month's medication supply. Participants in the standard care arm had two study visits during the 12‐month intervention period when they received written educational materials about preventing type 2 diabetes. In the main effects from this trial, there was a significant difference in 12‐month weight loss among ILI participants relative to metformin (−3.1 kg, P = 0.013) and standard care (−4.8 kg, P < 0.001) 17. The weight change observed in the metformin and standard care arms was not significantly different 17. The protocol for this study was approved by the Northwestern University IRB. Detailed descriptions of the study population, interventions and primary findings were previously published 17, 18.
Eighty‐five PREVENT‐DM participants (92.4%) who completed data collection visits at 0, 6 and 12 months were included in the current analysis. The primary outcome of the current analysis was weight change from baseline to 12 months, and its association with changes in depression, anxiety and perceived stress was examined. The following widely used questionnaires were used to measure these mental health variables: Beck Depression Inventory II (BDI‐II), Generalized Anxiety Disorder 7‐item Scale (GAD‐7) and the Perceived Stress Scale (PSS), which measures levels of general stress. For each mental health measure, we characterized participants as improved/stable (lower or equivalent scores at 12 months) or worsened (higher scores at 12 months). Participants whose symptom scores worsened on any of the three measures were considered to have worsened mental health (W), and those who improved or remained stable on all three measures were considered to have improved/stable mental health (I/S). Among the 85 participants included in this analysis, none were missing data for weight or mental health measures at 12 months.
The mean 12‐month change in weight and mental health measures was assessed by treatment assignment and mental health status (Table 2). The significance of 12‐month weight differences between I/S vs. W participants was assessed using independent‐sample t‐tests (Table 3). The difference in weight change was further stratified according to the number of mental health measures that worsened at 12 months (Table 3). To explore timing of these effects, 6‐month changes in mental health symptoms and weight were explored in the same manner described previously (Figure 1). Key variables were assessed separately among participants in the ILI arm and in the combined metformin and standard care arms. These two study arms were combined in the analysis because: (1) neither metformin nor standard care is thought to impact mental health outcomes directly; and (2) the 12‐month weight change did not differ between these groups 17. In a sensitivity analysis, the same analyses were repeated in the metformin and standard care groups individually. The mean 12‐month weight change was also modeled using ANCOVA, adjusting for baseline weight and including an interaction term for treatment assignment x categorical change in mental health status (i.e. I/S and W). All analyses assumed a 5% level of significance and were conducted using SPSS, version 24.
Table 2.
12‐month changes in weight and mental health measures by treatment assignment and mental health status
| Characteristic | Treatment assignment | Mental health status | ||
|---|---|---|---|---|
| Intensive lifestyle intervention (n = 30) | Metformin + standard care (n = 55) | Improved or stable (n = 32) | Worsened (n = 53) | |
| Mean ± SDa | Mean ± SDa | Mean ± SDa | Mean ± SDa | |
| Change in weight, kg | −4.0 ± 4.4 | −0.1 ± 3.8 | −2.9 ± 4.7 | −0.6 ± 4.0 |
| Change in mental health measures | ||||
| Depression scoreb | −3.8 ± 9.1 | −0.6 ± 6.6 | −6.0 ± 5.6 | 0.9 ± 7.6 |
| Anxiety scorec | −1.0 ± 5.5 | −0.2 ± 3.6 | −2.7 ± 3.4 | 0.8 ± 4.4 |
| Perceived stress scored | −0.9 ± 7.1 | −0.6 ± 5.8 | −5.3 ± 4.3 | 2.0 ± 5.7 |
A negative sign before the observed mean change indicates weight loss and mental health improvement. No sign before the observed mean change indicates mental health worsening.
Beck Depression Inventory II is scored from 0 to 63, with higher numbers indicating more depressive symptoms.
GAD‐7 is scored from 0 to 21, with higher numbers indicating more anxiety symptoms.
Perceived Stress Scale is scored from 0 to 40, with higher numbers indicating higher levels of perceived stress.
Table 3.
12‐month weight change according to changes in mental health measures
| Change in mental health measures | Intensive lifestyle intervention (n = 30) | Metformin + standard care (n = 55) | ||
|---|---|---|---|---|
| n | Weight change, kg (95% CI)a | n | Weight change, kg (95% CI)a | |
| Improved or stable (I/S) | 13 | −6.9 (−9.4, −4.3) | 19 | −0.2 (−1.5, 1.2) |
| Worsened on any mental health measure (W) | 17 | −1.8 (−3.5, −0.1) | 36 | −0.1 (−1.5, 1.4) |
| Between group difference, P‐valueb | 30 | −5.1 (−2.3, −7.9), 0.001 | 57 | 0.1 (−2.1, 2.3), 0.919 |
| Worsened on 1 mental health measure | 10 | −3.0 (−4.8, −1.2) | 18 | −0.1 (−1.5, 1.3) |
| Worsened on 2 mental health measures | 2 | −0.4 (−16.9, 16.1) | 10 | −0.8 (−3.8, 2.2) |
| Worsened on 3 mental health measures | 5 | 0.3 (−5.1, 5.6) | 8 | 1.0 (−4.7, 6.6) |
A negative sign before the observed mean weight change or 95% CI indicates weight loss, and no sign indicates weight gain.
P‐value for the difference in weight loss between I/S and W groups was generated using the independent samples t‐test.
Figure 1.
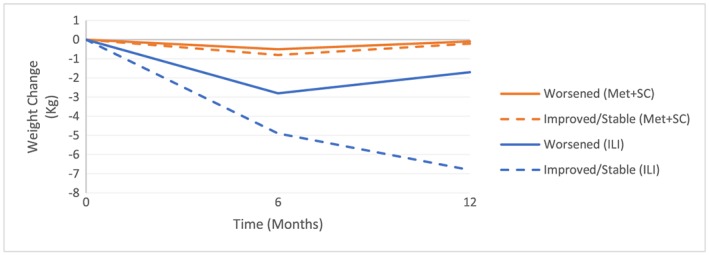
Change in weight at 6 and 12 months by changes in mental health (improved/stable vs. worsened) Legend: ILI = Intensive Lifestyle Intervention; Met = Metformin; SC = Standard Care.
Results
Table 1 presents the baseline characteristics of the participants by treatment assignment. The overall mean BMI was 33.3 kg/m2 (data not shown) 18. Demographic and other cardiometabolic data have been presented in‐depth elsewhere 17, 18. In the ILI group, mean baseline scores for the BDI, GAD‐7, and PSS were 13.5 ± 9.9, 4.7 ± 4.6, and 23.9 ± 7.7, respectively. The corresponding values in the combined metformin and standard care groups were 11.2 ± 9.0, 4.3 ± 4.4, and 22.0 ± 7.0. There were no meaningful differences in baseline characteristics between those whose mental health was improved or stable (I/S) vs. worsened (W), except for higher levels of perceived stress in the I/S group (24.4 ± 7.6) vs. 21.6 ± 6.8 in the W group (data not shown).
Table 1.
Baseline characteristics of study participants by treatment assignment
| Characteristica | Intensive lifestyle intervention (n = 33) | Metformin + standard care (n = 59) | P‐value |
|---|---|---|---|
| Age, years | 45.5 ± 12.3 | 44.9 ± 12.6 | 0.81 |
| Education, years | 10.2 ± 3.5 | 9.4 ± 3.7 | 0.32 |
| Household income, $ | 14,905 ± 7,518 | 15,875 ± 11,088 | 0.62 |
| Foreign born, n (%) | 30 (90.9) | 56 (94.9) | 0.66 |
| Weight, kg | 85.4 ± 23.0 | 78.9 ± 13.9 | 0.15 |
| BMI, kg/m2 | 34.4 ± 7.9 | 32.7 ± 5.6 | 0.23 |
| Depression scoreb | 13.5 ± 9.9 | 11.2 ± 9.0 | 0.26 |
| Anxiety scorec | 4.7 ± 4.6 | 4.3 ± 4.4 | 0.65 |
| Perceived stress scored | 23.9 ± 7.7 | 22.0 ± 7.3 | 0.22 |
Data are presented as means ± SD except otherwise noted.
Beck Depression Inventory II is scored from 0 to 63, with higher numbers indicating more depressive symptoms.
GAD‐7 is scored from 0 to 21, with higher numbers indicating more anxiety symptoms.
Perceived Stress Scale is scored from 0 to 40, with higher numbers indicating higher levels of perceived stress.
There was greater mean weight loss and larger mental health improvements among ILI participants than those who received metformin and standard care. (Table 2) Twelve‐month mean changes in weight and mental health measures were also greater among those whose mental health status improved or remained stable vs. worsened. (Table 2).
Table 3 presents the mean 12‐month weight change by treatment arm among participants who worsened on any of the mental health measures (W) vs. those who improved or remained stable on all three (I/S). Among the 30 ILI participants who completed follow‐up, 17 experienced worsening in mental health status and 13 demonstrated stable or improved mental health status. A significant difference in weight loss was observed between the I/S and W groups of −5.1 kg (95% CI: −7.9, −2.3; P = 0.001). Among ILI participants in the W group, those who worsened on only one mental health measure still experienced significant, yet diminished weight loss (−3.0 kg, 95% CI: −4.8, −1.2). However, those who worsened on two or three measures experienced non‐significant weight loss or weight gain. For metformin and standard care participants, there were no significant 12‐month weight changes in any of the groups defined by mental health status. The same null findings were observed in a sensitivity analysis examining the metformin and standard care arms separately. When modeling 12‐month weight change, the interaction term for treatment assignment × categorical mental health status was significant (P = 0.01).
Figure 1 displays the mean weight change at 6 and 12 months among improved/stable (I/S) and worsened (W) groups by treatment arm. Among ILI participants, the difference in weight loss between these groups was not significant at 6 months (data not shown). However, from 6 to 12 months, the W group regained weight, whereas the I/S group continued to lose weight.
Discussion
Among ILI participants in PREVENT‐DM, those whose three mental health measures were either improved or stable (I/S) over 12 months experienced significantly greater weight loss than those who worsened on any mental health measure (W). Mean weight loss was comparable among both I/S and W groups from baseline to 6 months. Weight loss trajectories diverged between 6 and 12 months, with W participants regaining weight and I/S participants continuing to lose weight. None of these relationships were found in the metformin and standard care arms.
Strengths of this study include its unique population of socioeconomically disadvantaged Latinas with prediabetes and overweight/obesity. Clinical trials including such vulnerable populations are few, especially among those with mental health comorbidities 19. In addition, prior research examining the relationship between mental health status and weight loss has included few Latinas, leaving practitioners with limited insight into effective weight loss treatments in this group 20, 21. Studying mental health in Latinas is especially important given differences in their presentation of mental health problems relative to other racial/ethnic and gender subgroups 22. In addition, self‐reported data for three mental health indicators are presented here, expanding on similar weight loss trials that have focused primarily on depression. Furthermore, longitudinal changes were explored in the current study, whereas most trials have analyzed mental health measures only as baseline predictors of weight loss.
This analysis has several limitations. Most importantly, the observed association between mental health improvement and weight loss does not imply a direction of causality. Improvement or stability in mental health may cause weight loss, or weight loss may lead to improvement in mental health, or improvements in both indicators may be mutually reinforcing. Second, the infrequency of antidepressant medication use among ILI participants (n = 3, 9.1%) precluded examination of its association with weight change. This represents a lower rate of antidepressant medication use than that reported in similar studies 23, which may reflect limited healthcare access among mostly foreign born Latinas with low socioeconomic status in the current study. Third, generalizability of the findings may be limited in other racial/ethnic groups and among men. Fourth, the study used validated scales to measure symptoms of depression, anxiety and perceived stress, rather than using a clinician interview, which is considered the gold standard for diagnosing mental health conditions. Finally, the small sample size and wide variation in mental health changes observed in this cohort limited statistical power and precluded drawing definitive conclusions about the relationships described here.
The significant association between mental health changes and weight loss observed in this analysis may be partly related to higher baseline levels of psychological distress relative to the original DPP trial 14, 24. Specifically, only 10% of DPP participants had a BDI score ≥ 11, the threshold used to define mild depression in that trial, compared to 53.2% of participants in PREVENT‐DM. The pragmatic consideration to not exclude participants with clinical levels of depression and anxiety in PREVENT‐DM may better reflect the mental health status of adults participating in community‐based ILI programs. On average, baseline depression and anxiety scores among participants in the current analysis were higher than the general population, but below clinical cutoffs used to define mild depression 14, 15, 16, 17, 18, 19 and anxiety 5, 6, 7, 8, 9, 10 on the same scales 25, 26. However, the number of participants with baseline depression and anxiety scores above these clinical cutoffs was 35 and 37, respectively (data not shown). The current sample had substantially higher levels of baseline perceived stress than a national sample of Hispanics 27. Examining the association between reliable and clinically significant mental health changes with weight loss was not possible due to the small numbers of participants who met relevant clinical thresholds. This should be explored in future research including larger samples, where such analyses are feasible.
One other translational trial of ILI delivered by telephone reported similar baseline levels of depressive symptoms and stress to those observed here. In that study, high levels of depressive symptoms and perceived stress at baseline were associated with less subsequent weight loss 23. That trial, however, did not report longitudinal changes in mental health measures. Some evidence on successful maintenance of weight loss suggests that lower levels of depression may be associated with greater odds of success 28, 29, 30; however, a clear consensus remains elusive. Few data examining the impact of anxiety and perceived stress on weight loss or maintenance exist.
While the timing of changes in mental health status and weight loss cannot be definitively determined here, the current study provides preliminary evidence about when mental health changes may impact weight loss during behavioral treatment. Among ILI participants, 16 experienced worsening mental health status from baseline to 6 months (data not shown), and 17 met the same criteria at 12‐month follow‐up. These findings suggest that even with initial weight loss, participants whose mental health worsens may begin to regain weight after 6 months, while others continue to lose weight. A previous weight loss trial of women reported a similar pattern for changes in depressive symptoms and weight at 6 months 31. One explanation for these findings is the reduced frequency of contact between 6 and 12 months, which likely provides less psychosocial support for those with worsening symptoms.
The divergence of weight trajectories at 6 months among those with improved or stable vs. worsened mental health may partly explain why weight loss generally plateaus in behavioral treatment at this same time 32. To support ongoing weight loss or weight maintenance beyond 6 months, programs might consider monitoring mental health outcomes longitudinally and providing more intensive psychosocial support for participants whose mental health is worsening. Future research may consider the extent to which mental health improvements are related to the frequency of intervention contacts. In addition, future studies should replicate our findings in larger samples and develop psychosocial enhancements to existing lifestyle interventions that can be tested in diverse populations.
Clinical trial registration
The PREVENT‐DM trial was recorded in the National Clinical Trials Registry (NCT02088034): http://www.clinicaltrials.gov. The current study represents a secondary analysis of data from this trial.
Funding
Support for the PREVENT‐DM trial was provided by K23DK095981. For the current analysis, Dr. O'Brien was supported by R03DK109243, and Dr. Schueller was supported by K08MH102336. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institute of Mental Health. No sponsor or funding source had a role in the design or conduct of the study; collection, management, analysis or interpretation of the data; or preparation, review or approval of the manuscript.
Conflict of Interest Statement
The authors declared no conflict of interest.
Alhalel, N. , Schueller, S. M. , and O'Brien, M. J. (2018) Association of changes in mental health with weight loss during intensive lifestyle intervention: does the timing matter?. Obesity Science & Practice, 4: 153–158. doi: 10.1002/osp4.157.
References
- 1. Simon GE, Von Korff M, Saunders K, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry 2006; 63: 824–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Allison DB, Newcomer JW, Dunn AL, et al. Obesity among those with mental disorders: a National Institute of Mental Health meeting report. Am J Prev Med 2009; 36: 341–350. [DOI] [PubMed] [Google Scholar]
- 3. Gerlach G, Loeber S, Herpertz S. Personality disorders and obesity: a systematic review. Obes Rev 2016; 17: 691–723. [DOI] [PubMed] [Google Scholar]
- 4. Husky MM, Mazure CM, Ruffault A, Flahault C, Kovess‐Masfety V. Differential associations between excess body weight and psychiatric disorders in men and women. J Womens Health 2017: 17. (Epub ahead of print Jul 7). [DOI] [PubMed] [Google Scholar]
- 5. Jagielski AC, Brown A, Hosseini‐Araghi M, Thomas GN, Taheri S. The association between adiposity, mental well‐being, and quality of life in extreme obesity. PLoS One 2014; 9: e92859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marmorstein NR, Iacono WG. Associations between depression and obesity in parents and their late‐adolescent offspring: a community‐based study. Psychosom Med 2016; 78: 861–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Marmorstein NR, Iacono WG, Legrand L. Obesity and depression in adolescence and beyond: reciprocal risks. Int J Obes (Lond) 2014; 38: 906–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fabricatore AN, Wadden TA, Moore RH, et al. Predictors of attrition and weight loss success: results from a randomized controlled trial. Behav Res Ther 2009; 47: 685–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Somerset SM, Graham L, Markwell K. Depression scores predict adherence in a dietary weight loss intervention trial. Clin Nutr 2011; 30: 593–598. [DOI] [PubMed] [Google Scholar]
- 10. Teixeira PJ, Going SB, Sardinha LB, Lohman TG. A review of psychosocial pre‐treatment predictors of weight control. Obes Rev 2005; 6: 43–65. [DOI] [PubMed] [Google Scholar]
- 11. Stubbs J, Whybrow S, Teixeira P, et al. Problems in identifying predictors and correlates of weight loss and maintenance: implications for weight control therapies based on behaviour change. Obes Rev 2011; 12: 688–708. [DOI] [PubMed] [Google Scholar]
- 12. Knowler W, Barrett‐Connor E, Fowler S, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Delahanty LM, Peyrot M, Shrader PJ, et al. Pretreatment, psychological, and behavioral predictors of weight outcomes among lifestyle intervention participants in the Diabetes Prevention Program (DPP). Diabetes Care 2013; 36: 34–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Delahanty LM, Conroy MB, Nathan DM, Group DPPR . Psychological predictors of physical activity in the diabetes prevention program. J Acad Nutr Diet 2006; 106: 698–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Diabetes Prevention Program Research Group . The Diabetes Prevention Program (DPP) description of lifestyle intervention. Diabetes Care 2002; 25: 2165–2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kramer MK, Kriska AM, Venditti EM, et al. Translating the Diabetes Prevention Program: a comprehensive model for prevention training and program delivery. Am J Prev Med 2009; 37: 505–511. [DOI] [PubMed] [Google Scholar]
- 17. O'Brien MJ, Perez A, Scanlan AB, et al. PREVENT‐DM comparative effectiveness trial of lifestyle intervention and metformin. Am J Prev Med 2017; 52: 788–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Perez A, Alos VA, Scanlan A, et al. The rationale, design, and baseline characteristics of PREVENT‐DM: a community‐based comparative effectiveness trial of lifestyle intervention and metformin among Latinas with prediabetes. Contemp Clin Trials 2015; 45: 320–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. UyBico SJ, Pavel S, Gross CP. Recruiting vulnerable populations into research: a systematic review of recruitment interventions. J Gen Intern Med 2007; 22: 852–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Linde JA, Simon GE, Ludman EJ, et al. A randomized controlled trial of behavioral weight loss treatment versus combined weight loss/depression treatment among women with comorbid obesity and depression. Ann Behav Med 2011; 41: 119–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pagoto S, Schneider KL, Whited MC, et al. Randomized controlled trial of behavioral treatment for comorbid obesity and depression in women: the Be Active Trial. Int J Obes (Lond) 2013; 37: 1427–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shavitt S, Cho YI, Johnson TP, et al. Culture moderates the relation between perceived stress, social support, and mental and physical health. J Cross Cult Psychol 2016; 47: 956–980. [Google Scholar]
- 23. Trief PM, Cibula D, Delahanty LM, Weinstock RS. Depression, stress, and weight loss in individuals with metabolic syndrome in SHINE, a DPP translation study. Obesity (Silver Spring) 2014; 22: 2532–2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rubin RR, Knowler WC, Ma Y, et al. Depression symptoms and antidepressant medicine use in diabetes prevention program participants. Diabetes Care 2005; 28: 830–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Spitzer R, Kroenke K, Williams J, Lowe B. A brief measure for assessing generalized anxiety disorder – the GAD‐7. Arch Intern Med 2006; 166: 1092–1097. [DOI] [PubMed] [Google Scholar]
- 26. Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories‐IA and ‐II in psychiatric outpatients. J Pers Assess 1996; 67: 588–597. [DOI] [PubMed] [Google Scholar]
- 27. Cohen S, Williamson G. Perceived stress in a probability sample of the United States In: Spacapan S, Oskamp S. (eds). The Social Psychology of Health. Sage: Newbury Park, CA, 1988. [Google Scholar]
- 28. Wing RR, Phelan S. Long‐term weight loss maintenance. Am J Clin Nutr 2005; 82: 222 s–225 s. [DOI] [PubMed] [Google Scholar]
- 29. Elfhag K, Rössner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev 2005; 6: 67–85. [DOI] [PubMed] [Google Scholar]
- 30. Price DW, Ma Y, Rubin RR, et al. Depression as a predictor of weight regain among successful weight losers in the diabetes prevention program. Diabetes Care 2013; 36: 216–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Simon GE, Rohde P, Ludman EJ, et al. Association between change in depression and change in weight among women enrolled in weight loss treatment. Gen Hosp Psychiatry 2010; 32: 583–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Look AHEAD Research Group . The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring, Md) 2006; 14: 737–752. [DOI] [PMC free article] [PubMed] [Google Scholar]


