Summary
Objective
Most Americans spend an average of 8 hours per day in the workplace. Current understanding of eating behaviours in the workplace and their association with overweight, obesity and binge eating disorder (BED) is limited. Workplace eating behaviours and weight‐related self‐efficacy were examined in a sample of 98 individuals with overweight or obesity, with or without BED.
Design
Participants completed the Weight Efficacy Lifestyle Questionnaire, Work and Social Adjustment Scale, Worker's Perception of Environmental Factors, and a Workplace Questionnaire.
Results
Eating unplanned food occurred on average 2.43 times per week (SD = 3.37), and eating unplanned food even when meals were brought from home occurred on average 1.28 times per week (SD = 1.84). Individuals with BED purchased lunch even when they brought food from home significantly more frequently than did individuals without BED. Those with BED also reported significantly poorer work and social adjustment related to binge eating as compared with those without BED. The most significant barriers to healthy eating in the workplace were coworker influence, eating more food in general and more junk food in response to stress, eating unplanned food at work and time constraints.
Conclusions
These factors may be important to target in weight‐loss treatment to increase individuals' weight loss success. As individuals with BED may be the most vulnerable to eating unplanned foods, clinicians may want to focus on this potential barrier in BED treatment.
Keywords: Binge‐eating disorder, obesity, overweight, workplace eating
Obesity is a contributor to many health problems, and individuals with excess weight struggle to consistently eat a healthy diet 1. Public health experts propose the idea of an obesogenic environment, which suggests that biological variables, behavioural factors, and environmental influences are the driving forces of rising obesity levels 2. The workplace is one setting that may contribute to an obesogenic environment 1, and most employed Americans spend an average of 8 hours per day at their place of work 3. Thus, understanding the influence of the workplace environment on eating behaviours is essential for promoting healthier lifestyles. Research specifically examining eating behaviours in the workplace as they relate to obesity, however, is limited.
Food availability and stress may increase eating in the workplace. Many work environments foster an unhealthy diet by offering cheap foods of low nutritional value and easily accessible vending machine foods 4. Continually being exposed to food makes it more likely that individuals will consume more food 5, 6. Stress at work also may be an important variable in the relationship between work environment and weight. As stress and burnout increase, eating awareness 7 and intuitive eating decline, while uncontrolled and emotional eating increase 8, 9. For individuals of a healthy weight, work stress was related to increased risk of weight gain over 5 years 10. Individuals who are overweight tend to eat more in response to stress when compared with those of a healthy weight 11 and therefore may be even more vulnerable to the impact of work stress on weight. Among individuals with overweight or obesity, work stress has been linked to increased body mass index (BMI) 12, 13, 14, greater risk for central obesity 12, and high fat intake 13. The relationship between work stress and eating behaviour is an important one to examine, especially among individuals with overweight or obesity.
Another important factor to consider, as it confers increased overweight and obesity risk, is binge eating disorder (BED) 15. BED, a psychiatric disorder included in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5), is characterized by frequent binge eating (i.e. consuming large amounts of food in a relatively brief period of time) without the presence of regular compensatory behaviours, a subjective feeling of loss of control during binge eating and at least three associated factors (eating more rapidly; eating until uncomfortably full; eating large amounts despite not being hungry; eating alone due to embarrassment; or feeling disgusted, depressed, or guilty after eating) 16. BED is categorized by severity as follows: mild (1 to 3 episodes weekly), moderate (4 to 7 episodes weekly), severe (8 to 13 episodes weekly) and extreme (14 or more episodes weekly). Lifetime prevalence of BED in the United States is estimated at 2.6 % among the general population, however, lifetime prevalence is estimated at 30.70% and 36.20% among individuals with overweight or obesity, respectively, within individuals seeking weight‐loss treatment 15. In addition to being at greater risk for obesity, individuals diagnosed with BED, as compared with those without BED, are at greater risk for developing mood and anxiety disorders 17, 18, 19. BED also can cause functional impairment in the workplace. For example, binge eating predicts higher rates of absenteeism from work in men 20 and greater work productivity impairment in both sexes 21. Those with BED and overweight or obesity, therefore, may be particularly vulnerable to workplace stress and unhealthy eating patterns as compared with those without BED.
A factor that may impact the relationship between work‐related stress and excess weight is self‐efficacy. Self‐efficacy, defined as confidence in one's ability to enact behaviour change, may be instrumental to weight loss 22 and consistently predicts weight change in individuals with and without BED 23, 24, 25, 26. Thus, to enhance current understanding of how the workplace impacts eating behaviors, it is important to examine self‐efficacy, especially in the presence of stress and BED.
In summary, many Americans spend a large proportion of their time at work 3, an environment where unhealthy food frequently is available, and where stress levels often are high. Yet little is known about the relationships among workplace eating behaviours, stress, and self‐efficacy among those with overweight or obesity, and current understanding of these relationships among individuals with BED is even more limited. To address limitations in the literature, this study aimed to (i) examine eating behaviours and barriers to healthy eating in the workplace among individuals with overweight or obesity, (ii) compare those with and without BED, (iii) explore social, emotional, and environmental correlates of workplace eating behaviours including (iiia) factors that facilitate healthy eating and (iiib) those that serve as barriers. It was hypothesized that unhealthy workplace eating and influences would be prevalent within this sample and that individuals with BED would report poorer work‐related eating behaviours (e.g. higher intake of ‘junk food’, unplanned food, and larger amounts of food) compared with individuals without BED. Lower eating self‐efficacy was hypothesized to be associated with higher levels of unhealthy workplace eating behaviours.
Method
Participants
Participants were 98 adults (75 women and 23 men) with overweight or obesity (BMI ≥ 25 kg/m2) recruited through primary care provider referrals and flyers placed in waiting/patient rooms for a behavioural weight‐loss treatment study being performed in primary care centres in a large urban university‐based medical healthcare centre. Exclusion criteria included BMI ≥ 55 kg/m2 (individuals with a BMI above 55 kg/m2 were referred for more intensive weight‐loss treatments); under 18 years of age; over 65 years of age; current/planned pregnancy; breastfeeding; serious mental illness (e.g. schizophrenia and bipolar disorder); or uncontrolled liver disease, hypertension (blood pressure > 160/95 mmHg), thyroid disease (thyroid‐stimulating hormone > 6.75 mIU/L) or diabetes (hemoglobin A1c > 8.0). Of the 98 participants who completed questionnaires, 74 (57 women and 17 men) worked outside of the home and were included in further analyses. Mean age was 46.51 years (SD = 10.18). Participants identified as the following race and ethnicity: White, not Hispanic (n = 53, 71.62%); Black (n = 15, 20.27%); White, Hispanic (n = 2; 2.70%); and other (n = 4; 5.41%). Most participants were married (n = 46, 62.16%) and had at least some college education (n = 69, 93.24%). Mean BMI was 35.23 kg/m2 (SD = 7.09). Participants fell within the following BMI categories: 25.68% (n = 19) overweight (BMI of 25 to <30 kg/m2), 28.38% (n = 21) Class 1 obesity (BMI of 30 to <35 kg/m2), 22.97% (n = 17) Class 2 obesity (BMI of 35 to <40 kg/m2) and 22.97% (n = 17) Class 3 obesity (BMI of 40 kg/m2 or higher). Twenty (27.00%) participants met DSM‐5 BED criteria.
Measures
Beck Depression Inventory
The Beck Depression Inventory (BDI) 27 is a 21‐item self‐report measure that assesses current depression level. Higher scores indicate increased depression. A total score of 21 or above suggests presence of depression. The BDI has excellent validity and reliability, with internal consistency ranging from 0.81 to 0.86 28. In this sample, Cronbach's α was 0.87.
Eating Disorder Examination
The Eating Disorder Examination (EDE) is a semi‐structured interview for assessing eating disorders and diagnosing BED (29; edited to correspond with DSM‐5). The EDE includes an overall score (EDE‐Global) and four subscales: restraint, eating concern, shape concern, and weight concern. The EDE has demonstrated good inter‐rater (0.65 to 0.96) and test–retest reliability (0.50 to 0.88) 30. The EDE‐Global score provides an index of eating disorder symptomatology, with higher scores reflecting greater severity. Cronbach's α for EDE‐Global with the current sample was 0.87.
Weight Efficacy Lifestyle Questionnaire
The Weight Efficacy Lifestyle Questionnaire (WELQ) 31 is a 20‐item measure that evaluates self‐efficacy and includes five situational factor subscales: negative emotions, availability, social pressure, physical discomfort, and positive activities. Items were rated between 0 (Not Confident) and 9 (Very Confident). Cronbach's α for each scale ranges from 0.70 to 0.90 31. In this sample, Cronbach's α for scales were as follows: WELQ‐Negative Emotions 0.90, WELQ‐Availability 0.76, WELQ‐Social Pressure 0.87, WELQ‐Physical Discomfort 0.87, and WELQ Positive Activities 0.74.
Work and Social Adjustment Scale
The Work Social Adjustment Scale (WSAS) 32 is a self‐report, 5‐item scale that measures functional impairment related to work and social activities with good internal consistency (Cronbach's α across multiple time points ranges from 0.79 to 0.94); test–retest reliability is 0.73 32. For this study, the measure was adapted to binge eating as the specified problem. For example, ‘because of my binge eating, my ability to work is impaired.’ Items were scored between 0 (Not at all) and 8 (Extremely), and an average impairment score was used for data analysis. Cronbach's α for WSAS in this sample was 0.81.
Worker's Perception of Environmental Factors
The Worker's Perception of Environmental Factors (WPEF) 33 is a self‐report measure, consisting of eight multiple choice items examining factors at work that influence decisions to eat healthy or junk food and to exercise. Only the items pertaining to food choice were analysed in this study (i.e. items 3, 4, 6, and 8). For example, ‘Does stress at your worksite influence you to: eat larger amounts of food, eat less food, eat more junk food, eat healthier food’. Item responses were examined, as scoring is not available for the WPEF.
Workplace Questionnaire
To examine eating behaviours in the workplace, a self‐report questionnaire was created that included the following four questions: ‘1. How many times a week do coworkers bring food in to share?’, ‘2. On average, how many times a week (can be more than once a day) do you eat this food?’, ‘3. How many times a week do you eat food at work that was not planned?’ (i.e. unplanned food), and ‘4. How many times a week do you buy food for lunch even though you brought your meal from home?’ Participants responded with the number of times/days for each item.
Procedures
Participants provided informed consent. Master‐level or doctoral‐level psychology clinicians trained in eating and weight disorders assessed participants for BED via gold standard semi‐structured interviews edited for DSM‐5 criteria (i.e. edited Eating Disorder Examination and the Structured Clinical Interview for DSM‐IV Axis 1 Disorders; 29, 34). These psychology clinicians received extensive and ongoing interview training and supervision, including initial in‐person supervision during interviews and eventual review of taped interviews. The psychology clinicians also participated in weekly supervision where any questions regarding BED diagnosis were discussed. The clinicians were blinded to the hypotheses of the current study. Trained clinicians measured participants' height using a wall measure and weight with a large capacity digital scale. Participants then completed study questionnaires. Study procedures were reviewed and approved by the university's Institutional Review Board.
Data analyses
Descriptive statistics were computed to examine participant characteristics. Group differences were examined using independent samples t‐tests for continuous variables and chi‐square for categorical variables. Correlations among the various measures were examined using Pearson's r for continuous variables and Kendall's Tau b for dichotomous variables. Because there were few significant differences between the groups with and without BED, correlations for the entire sample were examined.
Results
The groups with and without BED did not significantly differ on age, sex, race/ethnicity, marital status, level of education, sexual orientation or BDI. Three (4.20%) participants met criteria for depression based on BDI score. Participants with BED had a significantly higher average BMI than those without BED (t (72) = −3.01, p = 0.004). Table 1 shows the descriptive statistics for workplace eating (Workplace Questionnaire (WQ)), work and social adjustment (WSAS), weight self‐efficacy (WELQ), depression (BDI) and eating disorder symptomology (EDE), along with t‐tests examining differences on these measures between individuals with and without BED. Figure 1 shows how many times coworkers brought food to work, and Figure 2 shows how often participants ate that food. On average, participants ate unplanned food 2.43 times per week (SD = 3.37; Figure 3) and purchased lunch even when they brought food from home 1.28 times per week (SD = 1.84; Figure 4). The group with BED reported a statistically significant higher frequency of purchasing lunch even when food was brought from home and reported significantly poorer adjustment on the WSAS. Figure 5 shows the percentage of time participants ate food specifically brought by coworkers. More than half of the participants reported weekly exposure to food brought in by coworkers (46 participants of 74, 62.16%). Of these 46 participants, over half reported eating this food 100% of the time (27 participants of 46, 58.70%).
Table 1.
T‐test analyses between participants with and without binge‐eating disorder (BED) for the Beck Depression Inventory (BDI), Eating Disorder Examination (EDE), Weight Lifestyle Efficacy Questionnaire (WELQ), Work and Social Adjustment Scale (WSAS), and Workplace Questionnaire (WQ)
| Total Sample | BED | Non‐BED | t‐test analysis | ||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Range | Mean (SD) | Range | Mean (SD) | Range | ||
| BDI (N = 74) | 7.93 (6.73) | 10.30 (8.03) | 7.06 (6.04) | t(72) = −1.87, p = 0.07 | |||
| EDE‐global (N = 74) | 1.78 (.94) | 2.12 (.88) | 1.66 (.93) | t(72) = −1.93, p = 0.06 | |||
| EDE‐restraint | 1.32 (.95) | 1.46 (.72) | 1.27 (1.03) | t(72) = −0.76, p = 0.45 | |||
| EDE‐eating concern | .82 (1.06) | 1.25 (1.13) | 0.66 (1.00) | t(72) = −2.16, p = 0.03 | |||
| EDE‐shape concern | 2.58 (1.39) | 3.14 (1.31) | 2.38 (1.38) | t(72) = −2.13, p = 0.04 | |||
| EDE‐weight concern | 2.40 (1.25) | 2.64 (1.25) | 2.31 (1.25) | t(72) = −1.00, p = 0.32 | |||
| WELQ (N = 74) | |||||||
| Negative emotions | 19.88 (10.91) | 18.15 (12.94) | 20.52 (10.11) | t(71) = 0.82, p = 0.41 | |||
| Availability | 17.03 (8.58) | 14.20 (9.10) | 18.07 (8.22) | t(71) = 1.68, p = 0.10 | |||
| Social pressure | 21.76 (10.01) | 19.55 (10.47) | 22.00 (9.81) | t(71) = 1.14, p = 0.26 | |||
| Physical discomfort | 26.18 (8.73) | 23.95 (9.39) | 27.00 (8.42) | t(72) = 1.34, p = 0.18 | |||
| Positive activities | 23.95 (8.96) | 21.00 (8.83) | 25.04 (8.56) | t(72) = 1.79, p = 0.08 | |||
| WSAS (N = 74) | |||||||
| Total | 7.72 (8.31) | 12.50 (9.34) | 5.94 (7.21) | t(71) = −3.42, p = 0.002 | |||
| WQ (n = 68–71) | |||||||
| Times per week coworkers bring food | 1.62 (1.76) | 0–5 | 1.44 (1.76) | 0–5 | 1.67 (1.77) | 0–5 | t(65) = 0.47, p = 0.64 |
| Times per week this food is eaten | 1.34 (2.13) | 0–8 | 1.73 (3.39) | 0–8 | 1.15 (1.26) | 0–5 | t(63) = 0.19, p = 0.85 |
| Times per week unplanned food is eaten | 2.43 (3.37) | 0–20 | 2.53 (3.36) | 0–14 | 2.64 (3.43) | 0–20 | t(67) = 0.12, p = 0.90 |
| Times per week lunch is purchased even when food is brought from home | 1.28 (1.84) | 0–10 | 2.00 (2.47) | 0–10 | 0.91 (1.37) | 0–5 | t(68) = −2.20, p = 0.03 |
Figure 1.
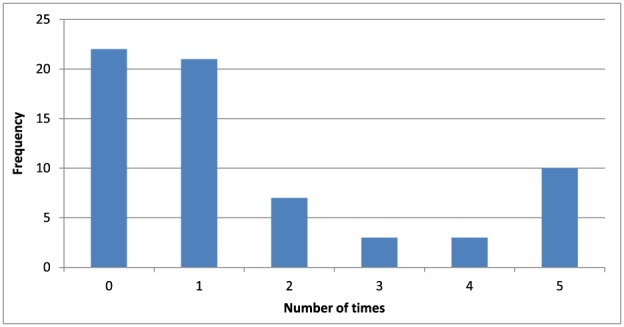
Frequency: times per week coworkers brought food to work.
Figure 2.
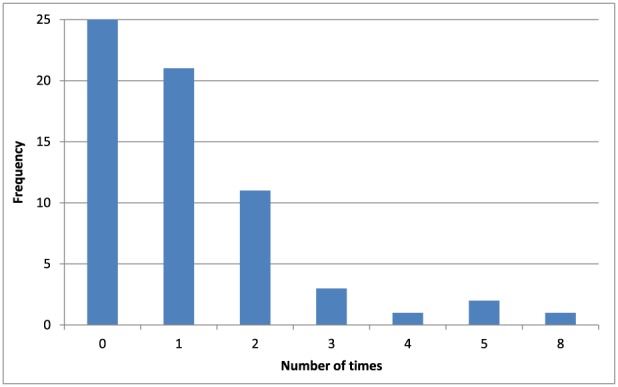
Frequency: times per week participants ate food brought by coworkers.
Figure 3.
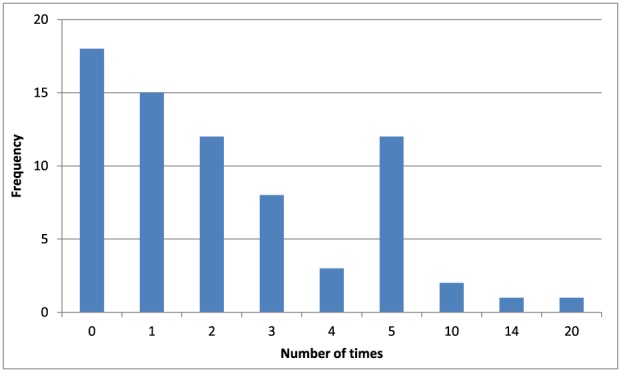
Frequency: times per week any unplanned food was eaten.
Figure 4.
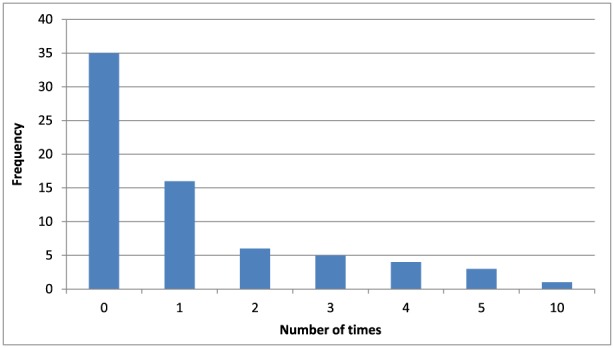
Frequency: times per week participants purchased lunch even when food was brought from home.
Figure 5.
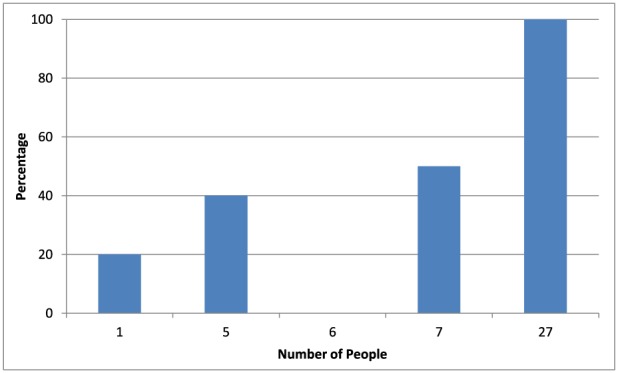
Percentage of time food was consumed when brought by coworkers.
Table 2 shows the descriptive statistics for workplace environment (WPEF). Eating junk food in response to stress at work was the most frequently reported factor influencing eating behaviour, with 48.65% of the sample reporting this behaviour. Eating more food overall in response to stress at work was the second highest reported behaviour at 40.54% from the whole sample. Chi‐square analyses revealed no significant differences between individuals with and without BED on any of these items.
Table 2.
Chi‐square comparisons between participants with and without binge eating disorder (BED) on the Worker's Perception of Environmental Factors items
| Total Sample | BED | Non‐BED | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | Chi‐square analysis | |
| 1. Time constraints prevent healthy eating at worksite | 24 | 32.43% | 8 | 40.00% | 16 | 29.63% | x 2(1) = 0.72, p = 0.40 |
| 2. Cost of food prevents healthy eating at worksite | 9 | 12.16% | 4 | 20.00% | 5 | 9.26% | x 2(1) = 1.58, p = 0.21 |
| 3. Quality of food prevents healthy eating at worksite | 18 | 24.32% | 5 | 25.00% | 13 | 24.07% | x 2(1) < 0.01, p = 0.93 |
| 4. Eat more food in response to stress at the worksite | 30 | 40.54% | 9 | 45.00% | 21 | 38.89% | x 2(1) = 0.23, p = 0.63 |
| 5. Eat less food in response to stress at the worksite | 4 | 5.41% | 1 | 5.00% | 3 | 5.56% | x 2(1) < 0.01, p = 0.93 |
| 6. Eat healthy food in response to stress at the worksite | 0 | 0.00% | 0 | 0.00% | 0 | 0.00% | N/A |
| 7. Eat junk food in response to stress at the worksite | 36 | 48.65% | 11 | 55.00% | 25 | 46.30% | x 2(1) = 0.44, p = 0.51 |
| 8. Coworkers influence increased food intake | 6 | 8.11% | 2 | 10.00% | 4 | 7.41% | x 2(2) = 0.51, p = 0.78 |
| 9. Coworkers influence decreased food intake | 1 | 1.35% | 0 | 0.00% | 1 | 1.85% | x 2(2) = 0.74, p = 0.69 |
| 10. Coworkers influence increased junk food intake | 21 | 28.38% | 6 | 30.00% | 15 | 27.78% | x 2(2) = 0.41, p = 0.81 |
| 11. Coworkers influence increased healthy food intake | 5 | 6.76% | 3 | 15.00% | 2 | 3.70% | x 2(2) = 3.42, p = 0.18 |
The results of the correlation analyses between the workplace measures and measures of depression, eating disorder symptomology, workplace impairment, and weight efficacy can be seen in Table 3. Eating food brought in by coworkers (WQ) was significantly negatively correlated with WELQ‐Negative Emotions, WELQ‐Availability, and WELQ Social Pressure. Unplanned eating was significantly positively correlated with the WSAS. Buying food when already brought from home (WQ) was significantly positively correlated with EDE‐Global, EDE‐Shape Concern, EDE‐Weight Concern and the WSAS. Cost of food as a barrier to healthy eating (WPEF) was significantly positively correlated with the WSAS. Stress resulting in eating larger amounts of food (WPEF) was significantly positively correlated with the WSAS and significantly negatively correlated with all WELQ scales. Stress resulting in eating larger amounts of junk food (WPEF) was significantly negatively correlated with WELQ‐Negative Emotions. Coworkers influencing eating larger amounts of food (WPEF) was significantly negatively correlated with BMI, WELQ‐Availability and WELQ‐Social Pressure and positively with EDE‐Eating Concern.
Table 3.
Pearson product–moment and Kendall's Tau b correlation coefficients
| BMI | BDI | EDE‐global | EDE‐restraint | EDE‐eating concern | EDE‐shape concern | EDE‐weight concern | WSAS total | WELQ‐ negative emotions | WELQ‐ availability | WELQ‐ social pressure | WELQ‐ physical discomfort | WELQ‐ positive activities | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Workplace Questionnaire | |||||||||||||
| On average, how many times a week (can be more than once a day) do you eat this food? | −0.03 p = 0.80 | 0.14 p = 0.25 | 0.02 p = 0.86 | −0.03 p = 0.80 | −0.05 p = 0.67 | 0.12 p = 0.36 | 0.01 p = 0.94 | 0.09 p = 0.47 | −0.27* p = 0.03 | −0.25* p = 0.04 | −0.26* p = 0.04 | −0.07 p = 0.58 | −0.16 p = 0.21 |
| On average, how many times a week (can be more than once a day) do you eat food at work that was unplanned? | 0.09 p = 0.47 | 0.04 p = 0.72 | 0.08 p = 0.54 | −0.12 p = 0.35 | 0.11 p = 0.37 | 0.11 p = 0.35 | 0.09 p = 0.47 | 0.27* p = 0.03 | −0.15 p = 0.21 | −0.13 p = 0.27 | −0.14 p = 0.25 | −0.16 p = 0.20 | −0.14 p = 0.27 |
| On average how many times a week do you buy food even when a meal was brought from home? | 0.09 p = 0.46 | 0.14 p = 0.25 | 0.28* p = 0.02 | 0.14 p = 0.24 | 0.17 p = 0.16 | 0.29* p = 0.02 | 0.26* p = 0.03 | 0.39** p < 0.0005 | 0.04 p = 0.75 | −0.01 p = 0.91 | −0.05 p = 0.66 | −0.03 p = 0.82 | −0.18 p = 0.14 |
| WPEFa | |||||||||||||
| Do you feel that time constraints at your worksite prevent you from eating healthy? | 0.11 p = 0.26 | 0.03 p = 0.75 | −0.09 p = 0.37 | −0.04 p = 0.72 | −0.10 p = 0.34 | −0.05 p = 0.61 | −0.06 p = 0.57 | 0.01 p = 0.94 | −0.04 p = 0.67 | 0.09 p = 0.35 | −0.04 p = 0.65 | −0.02 p = 0.81 | 0.06 p = 0.60 |
| Cost of food prevents healthy eating | 0.05 p = 0.63 | −0.02 p = 0.87 | 0.08 p = 0.41 | −0.07 p = 0.47 | 0.15 p = 0.14 | 0.14 p = 0.15 | 0.05 p = 0.60 | 0.22* p = 0.03 | −0.05 p = 0.64 | −0.11 p = 0.26 | −0.09 p = 0.38 | −0.05 p = 0.61 | −0.16 p = 0.17 |
| Quality of food prevents healthy eating | −0.12 p = 0.22 | −0.08 p = 0.45 | 0.02 p = 0.84 | 0.02 p = 0.88 | −0.08 p = 0.43 | 0.04 p = 0.67 | 0.04 p = 0.69 | 0.04 p = 0.73 | 0.06 p = 0.56 | 0.07 p = 0.45 | 0.16 p = 0.10 | 0.08 p = 0.43 | 0.16 p = 0.16 |
| Stress causes consumption larger amounts of food | 0.06 p = 0.54 | 0.18 p = 0.07 | 0.12 p = 0.23 | −0.05 p = 0.63 | 0.18 p = 0.08 | 0.14 p = 0.16 | 0.13 p = 0.18 | 0.23* p = 0.02 | −0.29** p = 0.03 | −0.35** p = 0.003 | −0.22* p = 0.03 | −0.20* p = 0.04 | −0.35*, * p = 0.002 |
| Stress causes consumption of more junk food | −0.18 p = 0.06 | 0.05 p = 0.61 | −0.01 p = 0.88 | −0.07 p = 0.50 | 0.15 p = 0.16 | 0.01 p = 0.95 | 0.02 p = 0.85 | 0.10 p = 0.30 | −0.26** p = 0.008 | −0.15 p = 0.14 | −0.12 p = 0.24 | −0.15 p = 0.14 | −0.14 p = 0.22 |
| Coworkers influence consumption of larger amounts of food | −0.26** p = 0.007 | 0.05 p = 0.63 | 0.14 p = 0.15 | 0.06 p = 0.55 | 0.24* p = 0.02 | 0.07 p = 0.47 | 0.18 p = 0.07 | 0.07 p = 0.49 | −0.08 p = 0.42 | −0.20* p = 0.04 | −0.28** p = 0.005 | −0.03 p = 0.77 | 0.01 p = 0.91 |
| Coworkers influence consumption of more junk food | 0.16 p = 0.10 | −0.12 p = 0.22 | 0.10 p = 0.31 | 0.05 p = 0.65 | 0.05 p = 0.60 | 0.08 p = 0.43 | 0.13 p = 0.19 | −0.05 p = 0.61 | −0.08 p = 0.41 | −0.06 p = 0.55 | −0.10 p = 0.34 | −0.01 p = 0.96 | 0.004 p = 0.98 |
Pearson's r was used for all correlations except for the items of the WPEF for which Kendall's Tau b was used.
Correlation is significant at the 0.01 level (two‐tailed).
Correlation is significant at the 0.05 level (two‐tailed).
BMI, body mass index; BDI, Beck Depression Inventory; EDE, Disorder Examination; WSAS, Work and Social Adjustment Scale; WELQ, Weight Efficacy Lifestyle Questionnaire; WPEF, Worker's Perception of Environmental Factors.
Body mass index was investigated as a potential moderator of the relationships among variables. Overall, BMI was unrelated to the workplace eating outcomes. Only 1 of the 10 examined items was significantly correlated with BMI. Therefore, no further analyses were conducted.
Discussion
This study examined eating behaviours in the workplace in a sample of individuals with overweight or obesity, both with and without BED. Results support the theory that the workplace is an important component of the obesogenic environment. Eating behaviours were influenced by workplace factors in the social, emotional, and practical domains. In comparison with those without BED, individuals with BED were significantly more likely to buy lunch at work even when they already brought food from home. Coworker behaviours, consumption of unplanned food, time constraints, and participants' stress appeared to be the most significant barriers to healthy workplace eating for participants with and without BED. Finally, lower weight‐related self‐efficacy and higher work and social impairment due to binge eating were associated with unhealthy eating behaviours at work.
While individuals with BED reported buying lunch (even when they brought food from home) twice weekly, participants with excess weight but no BED still reported purchasing food (despite bringing it from home) on average once weekly. The reported ranges, however, indicated that some participants with and without BED reported purchasing such food daily. This recurrent pattern is important for those who are seeking to lose weight because a long‐term, consistent pattern of purchasing food away from home may lead to increased intake of calorie‐dense/less nutrient‐rich food, which is typical for foods prepared outside the home 35. Individuals with BED also reported higher impairments in work and social settings due to binge eating than those without BED; this is not surprising given the fact that functional impairment due to binge eating is part of the diagnostic criteria for BED. While individuals with BED had significantly higher average BMIs than individuals without BED, BMI generally was unrelated to workplace eating behaviours. Perhaps the lack of significant correlations is due to ceiling effects or restricted range as all participants had a BMI over 25 kg/m2.
There were no other significant differences between the participants with and without BED on any of the other workplace eating behaviours. This lack of more widespread differences in workplace eating may be because BED often involves eating alone (along with embarrassment, guilt and shame about amount of food eaten), and workplace eating may be more social in nature 36, 37. Secretive eating behaviour was not assessed in this study, however, so it is unknown if this factor accounts for the lack of differences. Additionally, the study included participants with both overweight and obesity who were seeking weight‐loss treatment. Individuals with obesity, as compared with those without, tend to experience lower eating‐related self‐efficacy in all domains 38; therefore, this influence may have obscured the relationship between BED and unhealthy eating behaviours.
The sample reported that coworkers brought food to the office an average of 1.62 times per week, but there was a great deal of variability, ranging from 0 to 5 times weekly. Participants more often ate the food brought by coworkers, with a range of 0 to 8 times weekly. Individuals who were exposed to food brought by coworkers consumed these foods most of the time. Taken by itself, this continual exposure to food creates concern for unhealthy eating behaviours. The sample also reported eating unplanned foods with an average of 2.43 times per week (range of 0 to 20 times per week). When magnified over a 48‐week work year, this frequent unplanned eating can have a significant impact on individuals' weight and health, particularly at workplaces that may have food available more frequently. Individuals with lower self‐efficacy in response to social pressure, availability of food, and negative emotions were the most likely to eat more food in response to coworkers, including the food that coworkers brought to work. Furthermore, poorer work and social adjustment (due to binge eating) were related to purchasing food even when meals were already brought to work, suggesting that the risks of poorer eating may be compounded when personal factors interact with workplace environmental factors and may be greater for those who binge eat.
In addition to unplanned eating, participants reported that coworkers influenced them to eat more junk food, but not more food in general, and existing literature demonstrating that intake increases in the presence of others 39, 40, 41. It is possible that the overall amount of food eaten when brought in by coworkers is naturally limited by social norms (i.e. sharing and ensuring there is enough for everyone), which may not be present in other social situations with large numbers of people (e.g. ordering at a restaurant or a party). Personal factors may also impact this finding. Coworker influence to eat more food was particularly strong for those with low eating self‐efficacy in situations where food is highly available and in situations where they perceive strong social influence; therefore, there may be a subset of individuals at risk for eating more food under these circumstances.
Few to no participants reported their coworkers influenced them to eat healthier or to consume less food. It is possible that the unplanned foods, including those brought in by coworkers, are more likely to be unhealthy food, although this was not measured directly. Research shows that the macronutrient content of foods eaten in social settings tends towards foods with more fat and protein 42.
As hypothesized, stress in the workplace was related to eating both more food in general and more junk food specifically. Additionally, participants with low weight self‐efficacy were more likely to report eating in response to stress, which makes sense in light of past research showing that individuals with higher levels of stress or work‐related burnout tend to eat less intuitively and with less control 8, 9. With respect to work performance, higher levels of self‐rated work impairment due to binge eating were also related to eating in response to stress. Because this study used cross‐sectional data, it is difficult to determine the direction of these relationships; therefore, the precise causality cannot be ascertained from this research. These factors are important to examine in future research.
In addition to the opportunities to eat unplanned foods and the impact of stress, several practical factors were identified as barriers to healthy eating. Time constraints in the workplace were the biggest practical barrier to healthy eating, identified by about one‐third of the participants as a barrier, which is consistent with other research indicating time restrictions as a barrier to healthy eating at work 43, 44. Quality of food available and cost of food also were identified by a subset of the participants as barriers, consistent with research indicating that employees desire inexpensive, healthy food options at work to meet their nutritional goals 45.
This study had several limitations. First, the sample size was small, and less than a third of the participants met criteria for BED, therefore, the findings need to be interpreted with caution. This study utilized cross‐sectional data, which limits the ability to interpret the data. Additionally, the sample itself may not generalize to the larger population of individuals with overweight/obesity and BED because the study participants were primarily women, Caucasian, educated and treatment seeking.
Despite these limitations, the study's findings are relevant for intervening on both the public health and individual levels. More workplaces may wish to consider broad‐based empirically supported health promoting interventions 7, 46, 47, 48, 49, 50. Coworker behaviour and work stress influenced eating behaviour negatively, and this was particularly true for individuals with low weight‐related self‐efficacy and greater work impairment due to binge eating. Together, these findings suggest that interventions designed to target self‐efficacy in the face of stress and social influence may help individuals make healthier choices at work. Furthermore, these findings support the need to explicitly address workplace eating in treatment for BED and for interventions for weight management in general. Teaching stress management that includes strategies to help balance work responsibility with the time it takes to choose healthy food options could also be beneficial. For example, individuals who underwent guided self‐help cognitive‐behavioural therapy for recurrent binge eating, as compared with those who received treatment as usual, took fewer days off work for reasons related to eating disorder impairment 51.
There are several ways in which future research may expand upon the present study. A larger and more demographically diverse sample size would increase power and generalizability. A larger subsample of participants with BED would also increase power for comparison analyses. Validation studies of workplace eating measures are needed. Assessment of secretive eating, estimates of caloric consumption and more details regarding the nature of the unplanned food consumed would also shed light on the specifics of workplace eating behaviours. Repeated measures may also allow for more interpretation of directionality between work impairment and stress‐related eating. As BMI appeared mostly unrelated to work variables in this study, further examination of potential moderators may elucidate the interaction between BED and eating at work.
Conclusions
Since people spend much of their time at work, understanding workplace influences on eating behaviour is essential for the treatment of overweight/obesity and BED. The present results raise several areas that may be targeted in weight‐loss treatment to increase patients' success such as responding to unplanned foods in the workplace, resisting coworkers' influence, managing time and coping with work‐related stress. In particular, individuals with impairment related to binge eating may be most vulnerable to eating unplanned foods, clinicians may want to address such experiences directly in treatment.
Role of funding sources
This study was supported, in part, by a National Institutes of Health career development grant (Dr. Rachel Barnes: K23 DK092279). The National Institutes of Health were not involved in study design, collection, analysis, interpretation of data, the writing of the report or in the decision to submit this article for publication. The article does not represent the views of the NIH. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government. No additional funding was obtained for submitting this article.
Conflicts of interest
The authors have no conflicts to disclose.
Contributors
All authors contributed equally to the literature review and manuscript preparation.
Leung, S. L. , Barber, J. A. , Burger, A. , and Barnes, R. D. (2018) Factors associated with healthy and unhealthy workplace eating behaviours in individuals with overweight/obesity with and without binge eating disorder. Obesity Science & Practice, 4: 109–118. doi: 10.1002/osp4.151.
References
- 1. Swinburn BA, Caterson I, Seidell J, James W. Diet, nutrition and the prevention of excess weight gain and obesity. Public Health Nutr 2004; 7: 123–146. [DOI] [PubMed] [Google Scholar]
- 2. Lake A, Townshend T. Obesogenic environments: exploring the built and food environments. J R Soc Promot Health 2006; 126: 262–267. [DOI] [PubMed] [Google Scholar]
- 3. Bureau of Labor Statistics . (2017). American Time Use Survey News Release. Retrieved from https://www.bls.gov/news.release/archives/atus_06272017.htm
- 4. Story M, Kaphingst K, Robinson‐O'Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health 2008; 29: 253–272. [DOI] [PubMed] [Google Scholar]
- 5. Painter JE, Wansink B. How visibility and convenience influence candy consumption. Appetite 2002; 38: 237–238. [DOI] [PubMed] [Google Scholar]
- 6. Wansink B, Painter JE, Lee Y‐K. The office candy dish: proximity's influence on estimated and actual consumption. Int J Obes (Lond) 2006; 30: 871–875. https://doi.org/10.1038/sj.ijo.0803217. [DOI] [PubMed] [Google Scholar]
- 7. Barrington WE, Ceballos RM, Bishop SK, McGregor BA, Beresford SAA. Perceived stress, behavior, and body mass index among adults participating in a worksite obesity prevention program, Seattle, 2005–2007. Prev Chronic Dis 2012; 9 https://doi.org/10.5888/pcd9.120001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Järvelä‐Reijonen E, Karhunen L, Sairanen E, et al. High perceived stress is associated with unfavorable eating behavior in overweight and obese Finns of working age. Appetite 2016; 103: 249–258. https://doi.org/10.1016/j.appet.2016.04.023. [DOI] [PubMed] [Google Scholar]
- 9. Nevanperä NJ, Hopsu L, Kuosma E, Ukkola O, Uitti J, Laitinen JH. Occupational burnout, eating behavior, and weight among working women. Am J Clin Nutr 2012; 95: 934–943. https://doi.org/10.3945/ajcn.111.014191. [DOI] [PubMed] [Google Scholar]
- 10. Kivimäki M, Head J, Ferrie JE, et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. Int J Obes (Lond) 2006; 30: 982–987. [DOI] [PubMed] [Google Scholar]
- 11. Lemmens SG, Rutters F, Born JM, Westerterp‐Plantenga MS. Stress augments food ‘wanting’ and energy intake in visceral overweight subjects in the absence of hunger. Physiol Behav 2011; 103: 157–163. https://doi.org/10.1016/j.physbeh.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 12. Brunner EJ, Chandola T, Marmot MG. Prospective effect of job strain on general and central obesity in the Whitehall II Study. Am J Epidemiol 2007; 165: 828–837. https://doi.org/10.1093/aje/kwk058. [DOI] [PubMed] [Google Scholar]
- 13. Hellerstedt WL, Jeffery RW. The association of job strain and health behaviours in men and women. Int J Epidemiol 1997; 26: 575–583. https://doi.org/10.1093/ije/26.3.575. [DOI] [PubMed] [Google Scholar]
- 14. Kouvonen A, Kivimäki M, Cox SJ, Cox T, Vahtera J. Relationship between work stress and body mass index among 45,810 female and male employees. Psychosom Med 2005; 67: 577–583. [DOI] [PubMed] [Google Scholar]
- 15. Kessler RC, Berglund PA, Chiu WT, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry 2013; 73: 904–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. American Psychiatric Association . Diagnostic and statistical manual of mental disorders, 5th edn. Washington: DC, 2013. [Google Scholar]
- 17. Johnson JG, Spitzer RL, Williams JBW. Health problems, impairment and illnesses associated with bulimia nervosa and binge eating disorder among primary care and obstetric gynaecology patients. Psychol Med 2001; 31: 1455–1466. https://doi.org/10.1017/S0033291701004640. [DOI] [PubMed] [Google Scholar]
- 18. Telch CF, Stice E. Psychiatric comorbidity in women with binge eating disorder: prevalence rates from a non‐treatment‐seeking sample. J Consult Clin Psychol 1998; 66: 768–776. https://doi.org/10.1037/0022-006X.66.5.768. [DOI] [PubMed] [Google Scholar]
- 19. Wilfley DE, Wilson GT, Agras WS. The clinical significance of binge eating disorder. Int J Eat Disord 2003; 34: S96–S106. https://doi.org/10.1002/eat.10209. [DOI] [PubMed] [Google Scholar]
- 20. Mond J, Hay P. Functional impairment associated with bulimic behaviors in a community sample of men and women. Int J Eat Disord 2007; 40: 391–398. [DOI] [PubMed] [Google Scholar]
- 21. Striegel RH, Bedrosian R, Wang C, Schwartz S. Why men should be included in research on binge eating: results from a comparison of psychosocial impairment in men and women. Int J Eat Disord 2012; 45: 233–240. https://doi.org/10.1002/eat.20962. [DOI] [PubMed] [Google Scholar]
- 22. Glynn SM, Ruderman AJ. The development and validation of an Eating Self‐Efficacy Scale. Cognit Ther Res 1986; 10: 403–420. https://doi.org/10.1007/BF01173294. [Google Scholar]
- 23. Bernier M, Avard J. Self‐efficacy, outcome, and attrition in a weight‐reduction program. Cognit Ther Res 1986; 10: 319–338. https://doi.org/10.1007/BF01173469. [Google Scholar]
- 24. Linde JA, Jeffery RW, Levy RL, et al. Binge eating disorder, weight control self‐efficacy, and depression in overweight men and women. Int J Obes (Lond) 2004; 28: 418–425. https://doi.org/10.1038/sj.ijo.0802570. [DOI] [PubMed] [Google Scholar]
- 25. Nezami BT, Lang W, Jakicic JM, et al. The effect of self‐efficacy on behavior and weight in a behavioral weight‐loss intervention. Health Psychol 2016; 35: 714–722. https://doi.org/10.1037/hea0000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Roach JB, Yadrick MK, Johnson JT, Boudreaux LJ, Forsythe WA, Billon W. Using self‐efficacy to predict weight loss among young adults. J Am Diet Assoc 2003; 103: 1357–1359. https://doi.org/10.1016/S0002-8223(03)01072-1. [DOI] [PubMed] [Google Scholar]
- 27. Beck AT, Steer RA. Manual for the revised Beck Depression Inventory. Psychological Corporation: San Antonio, TX, 1987. [Google Scholar]
- 28. Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: twenty‐five years of evaluation. Clin Psychol Rev 1988; 8: 77–100. [Google Scholar]
- 29. Fairburn CG, Cooper Z. The Eating Disorders Examination In: Fairburn CG, Wilson GT. (eds). Binge eating: nature, assessment and treatment. Guilford Press: New York, 1993. [Google Scholar]
- 30. Grilo CM, Masheb RM, Lozano‐Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. Int J Eat Disord 2004; 35: 80–85. [DOI] [PubMed] [Google Scholar]
- 31. Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self‐efficacy in weight management. J Consult Clin Psychol 1991; 59: 739–744. https://doi.org/10.1037/0022-006X.59.5.739. [DOI] [PubMed] [Google Scholar]
- 32. Mundt JC, Marks IM, Shear MK, Greist JM. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. Br J Psychiatry 2002; 180: 461–464. https://doi.org/10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- 33. Watkins C, Golla V, Lartey G, Khubchandani J. Worker's perception: environmental factors influencing obesity at the workplace. Am J Health Stud 2008; 23: 74–80. [Google Scholar]
- 34. First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM‐IV‐TR Axis I Disorders, Research Version, Patient edn. Biometrics Research, New York State Psychiatric Institute: New York, 2002. [Google Scholar]
- 35. Guthrie JF, Lin B‐H, Frazao E. Role of food prepared away from home in the American diet, 1977‐78 versus 1994‐96: changes and consequences. J Nutr Educ Behav 2002; 34: 140–150. https://doi.org/10.1016/S1499-4046(06)60083-3. [DOI] [PubMed] [Google Scholar]
- 36. Greeno CG, Wing RR, Shiffman S. Binge antecedents in obese women with and without binge eating disorder. J Consult Clin Psychol 2000; 68: 95–102. [PubMed] [Google Scholar]
- 37. Tanofsky‐Kraff M, Goossens L, Eddy KT, et al. A multisite investigation of binge eating behaviors in children and adolescents. J Consult Clin Psychol 2007; 75: 901–913. https://doi.org/10.1037/0022-006X.75.6.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Richman RM, Loughnan GT, Droulers AM, Steinbeck KS, Caterson ID. Self‐efficacy in relation to eating behaviour among obese and non‐obese women. Int J Obes Relat Metab Disord 2001; 25: 907–913. https://doi.org/10.1038/sj.ijo.0801606. [DOI] [PubMed] [Google Scholar]
- 39. Herman CP. The social facilitation of eating. A review. Appetite 2015; 86: 61–73. https://doi.org/10.1016/j.appet.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 40. Herman CP, Polivy J. Normative influences on food intake. Physiol Behav 2005; 86: 762–772. https://doi.org/10.1016/j.physbeh.2005.08.064. [DOI] [PubMed] [Google Scholar]
- 41. Herman CP, Roth DA, Polivy J. Effects of the presence of others on food intake: a normative interpretation. Psychol Bull 2003; 129: 873–886. https://doi.org/10.1037/0033-2909.129.6.873. [DOI] [PubMed] [Google Scholar]
- 42. Patel KA, Schlundt DG. Impact of moods and social context on eating behavior. Appetite 2001; 36: 111–118. [DOI] [PubMed] [Google Scholar]
- 43. Symonds CR, Martins AC, Hartwell HJ. Foodscapes and wellbeing in the workplace: a university setting. Nutr Food Sci 2013; 43: 356–364. https://doi.org/10.1108/NFS-10-2012-0109. [Google Scholar]
- 44. Wandel M, Roos G. Work, food and physical activity. A qualitative study of coping strategies among men in three occupations. Appetite 2005; 44: 93–102. https://doi.org/10.1016/j.appet.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 45. Devine CM, Nelson JA, Chin N, Dozier A, Fernandez ID. “Pizza is cheaper than salad”: assessing workers' views for an environmental food intervention. Obesity 2007; 15: 57S–68S. https://doi.org/10.1038/oby.2007.388. [DOI] [PubMed] [Google Scholar]
- 46. Beresford SA, Bishop SK, Brunner NL, et al. Environmental assessment at worksites following a multilevel intervention to promote activity and changes in eating: The PACE Project. J Occup Environ Med 2010; 52: S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cash SW, Duncan GE, Beresford SA, McTiernan A, Patrick DL. Increases in physical activity may affect quality of life differently in men and women: the PACE project. Qual Life Res 2013; 22: 2381–2388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hannon PA, Hammerback K, Garson G, Harris JR, Sopher CJ. Stakeholder perspectives on workplace health promotion: a qualitative study of midsized employers in low‐wage industries. Am J Health Promot 2012; 27: 103–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mache S, Jensen S, Linnig S, et al. Do overweight workers profit by workplace health promotion, more than their normal‐weight peers? Evaluation of a worksite intervention. J Occupational Med Toxicol 2015; 10: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ryu H, Jung J, Cho J, Chin DL. Program development and effectiveness of workplace health promotion program for preventing metabolic syndrome among office workers. Int J Environ Res Public Health 2017; 14: 878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lynch FL, Striegel‐Moore RH, Dickerson JF, et al. Cost‐effectiveness of guided self‐help treatment for recurrent binge eating. J Consult Clin Psychol 2010; 78: 322–333. https://doi.org/10.1037/a0018982. [DOI] [PMC free article] [PubMed] [Google Scholar]


