Abstract
Objective
To validate the impact of HPV status, cancer stem cell (CSC) marker expression and tumour hypoxia status in patients with locally advanced head and neck squamous cell carcinoma (HNSCC), who received postoperative radiotherapy. The results of the exploration cohort have previously been reported by the German Cancer Consortium Radiation Oncology Group (DKTK-ROG; Lohaus et al., 2014; Linge et al., 2016).
Materials and methods
For 152 patients with locally advanced HNSCC the impact of HPV16 DNA status, CSC marker expression and hypoxia-associated gene signatures on outcome of postoperative radiotherapy were retrospectively analysed. Out of them, 40 patients received postoperative radiochemotherapy. Cox models presented in a previous study were validated using the concordance index as a performance measure. The primary endpoint of this study was loco-regional control. Results were compared to those previously reported by DKTK-ROG.
Results
Loco-regional control, freedom from distant metastases and overall survival were inferior to the previously reported cohort. Despite of this, the prognostic value of the combination of HPV infection status, CSC marker expression (SLC3A2) and tumour hypoxia status could be validated in univariate analyses using an independent validation cohort. For multivariate models, the concordance index was between 0.58 and 0.69 in validation, indicating a good prognostic performance of the models. The inclusion of CD44 and the 15-gene hypoxia signature moderately improved the performance compared to a baseline model without CSC markers or hypoxia classifiers.
Conclusions
The HPV status, CSC marker expression of CD44 and SLC3A2 as well as hypoxia status are potential prognostic biomarkers for patients with locally advanced HNSCC treated by postoperative radiotherapy.
Keywords: Biomarker, Cancer stem cells, HNSCC, HPV, Hypoxia, Postoperative radiochemotherapy, Validation
Introduction
The 5-year overall survival rate of patients with head and neck squamous cell carcinoma (HNSCC) is about 50%, although treatment efficacy has been therapeutically improved in the last decade [1], [2], [3]. Furthermore, the number of oropharyngeal cancers has increased worldwide over the last years [4], [5], [6]. For patients with resected locally advanced HNSCC it has been shown in three randomized clinical trials [7], [8], [9] that loco-regional control can be improved by postoperative radiochemotherapy (PORT-C) compared to postoperative radiotherapy (PORT) alone. However, due to their biological characteristics tumours are responding very heterogeneously to this treatment. In addition to established clinical parameters, novel biomarkers are needed to identify patient groups, which require escalated or de-escalated treatment schedules.
Independent of exogenous carcinogens, e.g. tobacco and alcohol consumption, infection with high-risk human papilloma virus (HPV) has become a major risk factor for the development of HNSCC over the past decade [10]. It has been shown that patients with HPV-related HNSCC are a distinct subgroup with better outcome of primary radiochemotherapy [11], [12], [13], [14]. Recently, in a multicentre retrospective trial conducted by the German Cancer Consortium Radiation Oncology Group (DKTK-ROG) it was shown, that patients with HPV16 DNA positive oropharyngeal tumours have a high rate of loco-regional tumour control and overall survival also after PORT-C compared to patients with HPV16 DNA negative tumours [15]. Furthermore, in a recent study it was shown that high expression of previously developed tumour hypoxia-associated gene signatures [16], [17] and cancer stem cell (CSC) markers within the surgically removed primary tumour were associated with impaired loco-regional tumour control after PORT-C in HNSCC [18]. These biomarkers were used to stratify patients with HPV16 DNA negative tumours into smaller subgroups with low and high probability of loco-regional recurrence. In order to apply this patient stratification scheme in future clinical trials regarding treatment de-escalation or intensification, these results have to be validated. Therefore, the present publication reports on the validation results of the Cox models presented in [18] on HPV16 DNA status, CSC marker expression and tumour hypoxia-associated gene signatures, using an independent validation cohort of HNSCC patients treated by PORT or PORT-C.
Material and methods
Patients
In this publication, two patient cohorts are being considered: a training cohort previously reported by DKTK-ROG and a monocentric validation cohort. For the training cohort, inclusion criteria, data collection, handling and analyses of biomaterial were previously described in detail [15], [18]. Briefly, 221 patients, who received PORT-C between 2004 and 2012 at nine partner sites of the DKTK-ROG, were included to identify potential prognosticators for loco-regional control after PORT-C, such as CSCs and tumour hypoxia [18]. In the retrospective validation cohort, patients treated at the Department of Radiation Oncology of the University Hospital Dresden meeting the following criteria were included: not included in the previous DKTK-ROG cohort, histologically proven squamous cell carcinoma arising from the oral cavity, oropharynx, hypopharynx or larynx; treatment between 1999 and 2006 with PORT or PORT-C in curative intention according to standard radiotherapy protocols (2 Gy/fraction, 5 fractions/week), covering the former tumour region and regional lymph nodes (50 Gy) and a boost (10–16 Gy) to the former tumour region and to the regions of involved lymph nodes. Before surgery, all patients had undergone staging (computed tomography or magnetic resonance imaging, chest X-ray and abdominal ultrasound), and only patients without evidence of distant metastases were included. Formalin-fixed paraffin-embedded (FFPE) tumour material as well as follow-up data of patients had to be available. Finally, 152 patients meeting all these criteria were included in the validation cohort. Follow-up data of patients were collected using the RadPlanBio Platform at the DKTK partner site Dresden [19]. Ethical approval for retrospective analyses of clinical and biological data was obtained from the local ethics committee.
Preparation of biomaterials for biomarker analyses
FFPE blocks of the primary tumour specimens (removed by surgery) were first subjected to haematoxylin and eosin staining to histologically confirm the presence of squamous cell carcinoma. Afterwards, they were processed under standardised procedures for biomarker investigations described below.
Immunohistochemical staining of p16 and CD44
Immunohistochemical (IHC) staining of p16 was performed using the CINtec Histology kit (Roche mtm laboratories AG, Basel, CH) according to the manufacturer’s instructions. Overexpression of p16 was defined as ⩾70% intense tumour staining. For p16 staining, 148 samples were evaluable. For CD44 protein expression, 145 patients of the validation cohort could be analysed. Immunohistochemical staining was performed as described in [18]. CD44 staining intensity was scored (0, +, ++, +++) and tumours with a minimum of 10% staining were considered as positive. Blinded samples were scored by two independent observers (AL and CK) with an inter-observer variability of <5%.
DNA extraction and PCR-array based analyses of HPV status
DNA extraction and PCR-array based analyses of HPV status were performed as described previously [15]. Briefly, genomic DNA was extracted from 5-μm FFPE sections using the QIAamp DNA FFPE tissue kit (Qiagen). HPV DNA analyses including genotyping were performed using the LCD-Array HPV 3.5 kit (CHIPRON GmbH, Berlin, DE) according to the instructions of the manufacturer. In total, 148 samples were evaluable for HPV DNA analyses.
nanoString RNA analyses
For the validation cohort, gene expression analyses have been performed using nanoString technology as described previously [18], including two hypoxia-associated gene signatures (see Supplementary Table 1) as well as potential CSC markers CD44, SLC3A2 and MET. Briefly, total RNA as well as reporter and capture probes specific to the genes of interest were mixed and incubated at 62 °C for 22 h. Samples were then kept at 4 °C for a maximum of 18 h and subjected to the nCounter system. Raw counts were logarithmised and then normalised to the mean of the internal level of reference genes ACTR3, B2M, GNB2L1, NDFIP1, POLR2A, RPL11, RPL37A, or to the reference genes of the corresponding hypoxia-gene signatures (Supplementary Table 1), respectively [16], [17]. Seven samples had to be omitted from nanoString analyses due to insufficient tumour material or due to too low RNA yield, thus 145 samples were evaluable. The CD44 probe design, which was incorrectly designed for the training cohort [18], has been corrected and included in the validation cohort.
Clinical endpoints and statistical analysis
The primary endpoint was loco-regional tumour control (LRC) and secondary endpoints were freedom from distant metastases (DM) and overall survival (OS). The endpoints were calculated from the first day of radiotherapy to the date of event or censoring and survival curves were estimated by the Kaplan-Meier method. To compare patient groups stratified by HPV16 DNA status, CSC marker expression and hypoxia classification, Log-rank tests were used. For the stratification of the validation cohort with respect to CSC marker expression, the cut-offs from the training cohort reported in [18] were applied. Hypoxia classification on the validation cohort was performed by k-means clustering (Euclidian distance) according to the cluster centres of the training cohort (Supplementary Table 2). The impact of potential prognostic variables on the endpoints was evaluated using univariate Cox-regression for both cohorts. To evaluate the prognostic performance of the multivariate Cox models presented in [18] for the validation cohort, the concordance index (ci) was calculated, which is equal to 0.5 for non-prognostic models and equals 1 for perfectly predicting models [20]. Bootstrap resampling with 10,000 samples was used to estimate the confidence intervals (CI) of the concordance index. From these bootstrap samples a p-value for the hypothesis ci = 0.5 was calculated. To evaluate differences between the two cohorts Mann-Whitney-U tests were used for continuous variables and chi-squared tests for categorical variables. The bootstrapping procedure and ci calculation were implemented in Python. For all of the other analyses, SPSS 23 software (IBM Corporation, Armonk, NY, USA) was used. In this study, two-sided tests were performed and p-values < 0.05 were considered statistically significant.
Results
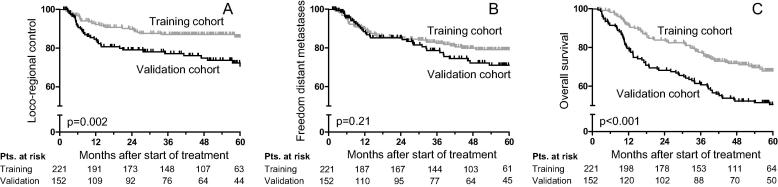
In this retrospective study, the prognostic value of HPV16 DNA status, CSC markers and hypoxia classifiers presented in [18] for 221 patients (training cohort) should be validated on an independent validation cohort of 152 patients. The patient data, treatment parameters and tumour characteristics of the training cohort have been described previously [15], [18]. They are summarised in Table 1 together with the values of the validation cohort and the comparison between both cohorts. Patients in the validation cohort were treated between 1999 and 2006 with PORT (N = 112) or PORT-C (N = 40), while all patients of the training cohort received PORT-C as the standard treatment (p < 0.001). Furthermore, patients in the retrospective validation cohort had a significantly lower age (p = 0.016), delivered dose (p = 0.001), N stage (p < 0.001), R status (p < 0.001), extracapsular extension (ECE) status (p < 0.001) and also showed a different distribution in their tumour localisations (p < 0.001). The fraction of oropharyngeal tumours and tumours of the oral cavity were almost reverse in training and validation cohort (oropharynx: 57% vs 30%, oral cavity: 27% vs 55%). In the validation cohort HPV infection occurred less frequently than in the (more recently treated) training cohort (HPV16 DNA positivity: 14% vs. 33%, p < 0.001). For the considered endpoints, patients in the validation cohort showed lower LRC and OS, while the occurrence of DM was not significantly different, see Fig. 1. Actuarial rates of LRC, freedom from DM and OS for the training and validation cohort were 90% vs 78% (p = 0.002), 85% vs 84% (p = 0.21) and 83% vs 68% (p < 0.001), after two years, respectively.
Table 1.
Comparison of the patient and tumour characteristics of the training and validation cohort.
| Characteristics | Training cohort (2004–2012) |
Validation cohort (1999–2006) |
p-Value | ||
|---|---|---|---|---|---|
| Median (range) | Median (range) | ||||
| Follow-up (months) | 46.2 (2.5–100.1) | 43.1 (1.8–153) | 0.29 | ||
| Age (years) | 57.0 (24.0–75.2) | 52.7 (36.3–71.0) | 0.016 | ||
| Dose (Gy) | 64 (56–68) | 64 (60–66) | 0.001 | ||
| Number of pts | (%) | Number of pts | (%) | ||
| Gender | |||||
| Male/Female | 180/41 | (81/19) | 127/25 | (84/16) | 0.60 |
| Clinical tumour (T) stage | |||||
| cT1/cT2/cT3/cT4 | 41/98/47/35 | (19/44/21/16) | 40/69/24/19 | (26/45/16/13) | 0.20 |
| Clinical nodal (N) stage | |||||
| cN0/cN1/cN2/cN3 | 22/31/138/30 | (10/14/62/14) | 15/31/104/2 | (10/20/68/1) | <0.001 |
| Stage (UICC 7th edition) | |||||
| I/II/III/IV | 0/8/33/180 | (0/4/15/81) | 2/3/34/113 | (1/2/23/74) | 0.069 |
| R status | |||||
| 0/1/unknown | 125/94/2 | (57/42/1) | 109/30/13 | (72/20/8) | <0.001 |
| ECE status | |||||
| 0/1/unknown | 103/118/0 | (47/53/0) | 104/47/1 | (68/31/1) | <0.001 |
| Localisation | |||||
| Oropharynx/oral cavity/hypopharynx/larynx | 126/60/35/0 | (57/27/16/0) | 46/83/15/8 | (30/55/10/5) | <0.001 |
| Grading | |||||
| 1/2/3/unknown | 5/123/89/4 | (2/56/40/2) | 3/78/71/0 | (2/51/47/0) | 0.55 |
| Chemotherapy | |||||
| yes/no | 221/0 | (100/0) | 40/112 | (26/74) | <0.001 |
| Smoking during therapy | |||||
| yes/no/unknown | 186/20/15 | (84/9/7) | 103/16/33 | (68/11/22) | 0.30 |
| Alcohol during therapy | |||||
| yes/no/unknown | 100/30/91 | (45/14/41) | 99/19/34 | (65/13/22) | 0.17 |
| p16 status | |||||
| negative/positive/unknown | 135/79/7 | (61/36/3) | 128/20/4 | (84/13/3) | <0.001 |
| HPV16 DNA status | |||||
| negative/positive/unknown | 143/72/6 | (65/33/2) | 126/22/4 | (83/14/3) | <0.001 |
| CD44 protein | |||||
| negative/positive/unknown | 44/151/26 | (20/68/12) | 15/130/7 | (10/85/5) | 0.003 |
| CD44 (log2-normalised expression) | |||||
| ⩽0.2 / > 0.2 / unknown | 78/118/25 | (35/54/11) | 55/90/7 | (36/59/5) | 0.73 |
| SLC3A2 (log2-normalised expression) | |||||
| ⩽−3.135 />−3.135 / unknown | 77/119/25 | (35/54/11) | 43/102/7 | (28/67/5) | 0.066 |
| MET (log2-normalised expression) | |||||
| ⩽−4.135 />−4.135 / unknown | 94/102/25 | (43/46/11) | 47/98/7 | (31/64/5) | <0.001 |
| 15-gene hypoxia signature | |||||
| low hypoxic/highly hypoxic/unknown | 79/117/25 | (36/53/11) | 41/104/7 | (27/68/5) | 0.021 |
| 26-gene hypoxia signature | |||||
| low hypoxic/highly hypoxic/unknown | 72/124/25 | (33/56/11) | 22/123/7 | (14/81/5) | <0.001 |
| Loco-regional recurrences | 29 | (13) | 38 | (25) | 0.003 |
| Distant metastases | 42 | (19) | 24 | (22) | 0.43 |
| Deaths | 70 | (32) | 86 | (57) | <0.001 |
Bold numbers indicate significant p-Values with p < 0.05.
Fig. 1.
(A–C) Kaplan-Meier estimates of (A) loco-regional control (LRC), (B) freedom of distant metastases (DM) and (C) overall survival (OS) for the training and validation cohort.
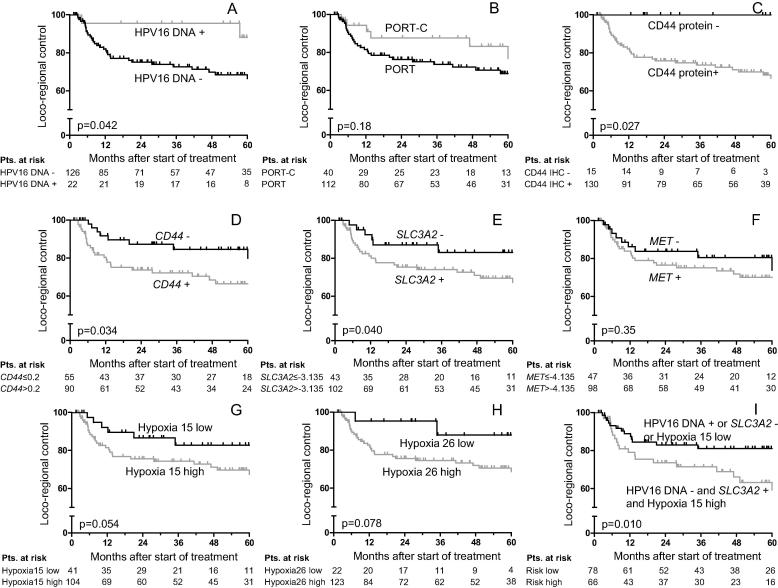
Table 2 shows the results of univariate Cox regression with clinical parameters and HPV status for the considered endpoints of the validation cohort. Significantly lower LRC and OS was found for higher T stage (LRC: HR 2.46, p = 0.008; OS: HR 2.14, p = 0.001) and tumours of the oral cavity (LRC: HR 2.68, p = 0.005; OS: HR 2.22, p < 0.001), while oropharyngeal tumours (LRC: HR 0.38, p = 0.020; OS: HR 0.40, p = 0.001) and HPV16 DNA positive tumours (LRC: HR 0.25, p = 0.060; OS: HR 0.35, p = 0.015) showed improved LRC and OS. These results are consistent with the findings of the training cohort [18]. Fig. 2 A-B shows Kaplan-Meier curves of the validation cohort stratified for HVP16 DNA status and use of chemotherapy. Patients with HPV16 DNA positive tumours showed significantly higher loco-regional control rates compared to patients with HPV16 DNA negative tumours using the Log-rank test; a statistical trend was obtained by Cox regression. The higher loco-regional control rates in the small patient group receiving PORT-C did not reach statistical significance.
Table 2.
Univariate Cox regression with clinical variables as well as HPV status for the endpoints loco-regional control, freedom of distant metastases and overall survival for the validation cohort. Shown is the hazard ratio (HR) with 95% confidence interval (CI) and the p-value testing the hypothesis HR = 1.
| Loco-regional control |
Distant metastases |
Overall survival |
||||
|---|---|---|---|---|---|---|
| Variable | HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value |
| Age (years) | 0.97 (0.94–1.01) | 0.16⁎ | 0.99 (0.95–1.03) | 0.56 | 1.01 (0.99–1.04) | 0.31 |
| Dose (Gy) | 1.07 (0.94–1.24) | 0.31 | 1.21 (1.02–1.42) | 0.022 | 1.07 (0.98–1.18) | 0.15 |
| Gender | 0.36 (0.11–1.16) | 0.087 | 0.04 (0.00–1.33) | 0.071 | 0.59 (0.31–1.15) | 0.12 |
| T stage (1,2 vs 3,4) | 2.46 (1.26–4.79) | 0.008⁎ | 2.50 (1.24–5.05) | 0.010⁎ | 2.14 (1.35–3.38) | 0.001⁎ |
| N stage (0,1 vs 2,3) | 0.87 (0.44–1.74) | 0.69 | 0.99 (0.47–2.09) | 0.98⁎ | 0.85 (0.54–1.34) | 0.48 |
| UICC stage (I–III vs IV) | 1.13 (0.53–2.40) | 0.75 | 1.03 (0.48–2.21) | 0.95 | 0.99 (0.62–1.60) | 0.97 |
| R status | 0.86 (0.39–1.89) | 0.71 | 1.38 (0.64–3.00) | 0.41 | 1.29 (0.78–2.11) | 0.32 |
| ECE status | 1.60 (0.82–3.11) | 0.17 | 1.75 (0.87–3.49) | 0.11⁎ | 1.41 (0.90–2.21) | 0.13⁎ |
| Oropharynx | 0.38 (0.17–0.86) | 0.020⁎ | 0.41 (0.18–0.94) | 0.034⁎ | 0.40 (0.23–0.68) | 0.001⁎ |
| Oral cavity | 2.68 (1.35–5.33) | 0.005⁎ | 1.55 (0.78–3.08) | 0.21⁎ | 2.22 (1.43–3.46) | <0.001⁎ |
| Hypopharynx | 0.91 (0.32–2.60) | 0.86 | 1.87 (0.77–4.53) | 0.17 | 0.89 (0.43–1.84) | 0.74 |
| Larynx | 0.40 (0.05–2.89) | 0.36 | 1.05 (0.31–3.59) | 0.94 | 1.02 (0.44–2.35) | 0.96 |
| Grading (1,2 vs 3) | 0.97 (0.50–1.86) | 0.92 | 1.81 (0.91–3.61) | 0.094 | 1.12 (0.74–1.72) | 0.59 |
| Chemotherapy | 0.55 (0.23–1.32) | 0.18 | 1.42 (0.69–2.93) | 0.34 | 0.77 (0.45–1.31) | 0.33 |
| Smoking | 1.19 (0.36–3.98) | 0.78 | 2.20 (0.52–9.30) | 0.28 | 1.22 (0.55–2.68) | 0.63 |
| Alcohol | 0.87 (0.33–2.31) | 0.78 | 2.83 (0.67–12.0) | 0.16 | 1.26 (0.62–2.55) | 0.53 |
| p16 | 0.46 (0.14–1.49) | 0.19⁎ | 0.46 (0.14–1.50) | 0.20⁎ | 0.40 (0.17–0.92) | 0.031⁎ |
| HPV16 DNA | 0.25 (0.06–1.06) | 0.060⁎ | 0.40 (0.12–1.33) | 0.13⁎ | 0.35 (0.15–0.82) | 0.015⁎ |
Bold numbers indicate significant p-Values with p < 0.05.
p < 0.05 in published training cohort.
Fig. 2.
(A–I) Kaplan-Maier estimates of loco-regional control (LRC) for the validation cohort stratified for (A) HPV16 DNA status, (B) chemotherapy, (C–F) cancer stem cell (CSC) marker expression, (G and H) hypoxia-related gene classification and (I) combined risk. Gene names are indicated using italics.
In [18] a significant impact of the cancer stem-cell markers CD44, SLC3A2 and MET on LRC was found using their expression values dichotomised at the cut-offs 0.2, −3.135 and −4.135, respectively. These cut-offs were used for patient stratification of the validation cohort. The resulting Kaplan-Meier curves are depicted in Fig. 2D–F. In univariate analyses, the impact of CD44 (HR 2.14, p = 0.049) and SLC3A2 (HR 2.45, p = 0.047) on LRC could be confirmed with lower hazard ratios, while MET expression showed no correlation with LRC (Table 3). Also the significant impact of CD44 protein on LRC could be confirmed (p = 0.027, Fig. 2C). For the secondary endpoints only CD44 showed a significant correlation with freedom of DM. The prognostic value of MET and SLC3A2 for OS and DM could not be confirmed.
Table 3.
Training (cohort 1) and validation (cohort 2) of univariate Cox models containing cancer stem cell marker expression or hypoxia classifiers for the endpoints loco-regional control, freedom of distant metastases and overall survival. Shown is the hazard ratio (HR) with 95% confidence interval (CI) and the p-value testing the hypothesis HR = 1.
| Loco-regional control |
Distant metastases |
Overall survival |
|||||
|---|---|---|---|---|---|---|---|
| HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value | ||
| Cohort | |||||||
| All patients | |||||||
| CD44 protein | 1 | 9.09 (1.24–66.8) | 0.030 | 2.29 (0.90–5.86) | 0.084 | 1.78 (0.91–3.50) | 0.093 |
| 2 | ⁎ | 1.80 (0.43–7.54) | 0.42 | 1.16 (0.53–2.53) | 0.71 | ||
| CD44 > 0.2 | 1 | 3.56 (1.36–9.35) | 0.010 | 1.69 (0.83–3.43) | 0.15 | 1.57 (0.92–2.67) | 0.098 |
| 2 | 2.14 (1.00–4.56) | 0.049 | 2.30 (1.04–5.08) | 0.040 | 1.20 (0.76–1.89) | 0.44 | |
| SLC3A2 > −3.135 | 1 | 6.54 (1.97–21.7) | 0.002 | 4.17 (1.74–10.0) | 0.001 | 2.37 (1.36–4.13) | 0.002 |
| 2 | 2.45 (1.01–5.91) | 0.047 | 1.78 (0.77–4.10) | 0.18 | 1.19 (0.73–1.93) | 0.48 | |
| MET > −4.135 | 1 | 5.19 (1.97–13.7) | 0.001 | 3.41 (1.61–7.23) | 0.001 | 2.74 (1.60–4.70) | <0.001 |
| 2 | 1.43 (0.67–3.07) | 0.35 | 1.18 (0.56–2.47) | 0.67 | 0.93 (0.58–1.47) | 0.74 | |
| 15-gene signature | 1 | 3.55 (1.35–9.35) | 0.010 | 1.27 (0.65–2.46) | 0.49 | 1.47 (0.88–2.47) | 0.14 |
| 2 | 2.32 (0.96–5.59) | 0.061 | 1.06 (0.50–2.22) | 0.89 | 1.20 (0.74–1.96) | 0.46 | |
| 26-gene signature | 1 | 9.37 (2.22–39.5) | 0.002 | 2.15 (1.01–4.55) | 0.046 | 2.48 (1.39–4.42) | 0.002 |
| 2 | 3.36 (0.81–14.0) | 0.097 | 2.16 (0.66–7.07) | 0.21 | 1.26 (0.66–2.38) | 0.48 | |
| Patients with HPV16 DNA-negative tumours | |||||||
| CD44 protein | 1 | ⁎ | 2.20 (0.53–9.18) | 0.28 | 1.45 (0.58–3.64) | 0.43 | |
| 2 | ⁎ | 0.79 (0.19–3.35) | 0.75 | 0.68 (0.29–1.57) | 0.36 | ||
| CD44 > 0.2 | 1 | 4.15 (1.25–13.8) | 0.020 | 1.69 (0.72–3.94) | 0.23 | 1.40 (0.76–2.58) | 0.28 |
| 2 | 1.85 (0.86–3.96) | 0.11 | 2.54 (1.04–6.22) | 0.041 | 1.17 (0.72–1.90) | 0.52 | |
| SLC3A2 > −3.135 | 1 | 9.23 (1.25–68.1) | 0.029 | 3.56 (1.08–11.7) | 0.037 | 1.53 (0.79–2.98) | 0.21 |
| 2 | 1.87 (0.77–4.55) | 0.17 | 1.80 (0.69–4.73) | 0.23 | 1.13 (0.67–1.93) | 0.64 | |
| MET > −4.135 | 1 | 3.74 (1.29–10.9) | 0.015 | 2.82 (1.16–6.87) | 0.023 | 2.42 (1.27–4.61) | 0.007 |
| 2 | 0.97 (0.45–2.08) | 0.94 | 0.75 (0.34–1.66) | 0.48 | 0.71 (0.43–1.16) | 0.17 | |
| 15-gene signature | 1 | 4.66 (1.60–13.5) | 0.005 | 1.54 (0.73–3.21) | 0.26 | 1.88 (1.06–3.34) | 0.031 |
| 2 | 2.13 (0.88–5.15) | 0.093 | 1.37 (0.59–3.21) | 0.47 | 1.38 (0.80–2.37) | 0.25 | |
| 26-gene signature | 1 | 11.3 (1.53–83.7) | 0.017 | 1.51 (0.65–3.51) | 0.34 | 2.05 (1.03–4.08) | 0.040 |
| 2 | 1.62 (0.39–6.78) | 0.51 | 1.36 (0.32–5.73) | 0.68 | 0.91 (0.42–1.99) | 0.81 | |
Bold numbers indicate significant p-Values with p < 0.05.
No convergence due to no events in the CD44 protein negative group.
For hypoxia-related gene classification based on the 15- and 26-gene signature [16], [17], k-means clustering was used in [18]. Both classifiers were able to stratify patients into a group with high hypoxia-related gene expression and low LRC and a group with low hypoxia-related gene expression and better LRC. For the validation cohort, the hypoxia classification was performed using the cluster centres of the training cohort. Based on this classification, Fig. 2G and 2H present Kaplan-Meier curves of tumours with low and high hypoxia-related gene expression for the validation cohort. A statistical trend for differences in LRC between both groups was obtained for both signatures (15-gene signature: HR 2.32, p = 0.061; 26-gene signature: HR 3.36, p = 0.097; Table 3). Considering only patients with HPV16 DNA negative tumours, this trend remained for the 15-gene signature (HR 2.13, p = 0.093) but not for the 26-gene signature. In [18] low-risk patients (HPV16 DNA positive or SLC3A2 negative or low hypoxia) showed favourable LRC compared to the remaining high-risk patients. Here, this classification also yields a significant difference in LRC (p = 0.010, Fig. 2I).
In [18] several multivariate Cox models were presented, which included HPV16 DNA status, one CSC marker and one hypoxia-associated gene classifier as well as the clinical parameters ECE status, tumour localisation oropharynx and hypopharynx. For the primary endpoint LRC, these models were applied to the validation cohort without adapting the model parameters. The prognostic performance of these models was then evaluated by the concordance index (ci). To reveal an additional impact of the CSC markers or hypoxia classifiers, the model performance was compared to a baseline model, which did not contain any CSC marker or hypoxia classifier. In Table 4 the results of the training cohort and the validation cohort are presented for all patients and for patients with HPV16 DNA negative tumours. For the training cohort, the baseline model showed a ci of 0.76 for all patients and of 0.66 for patients with HPV16 DNA negative tumours. Using additional CSC markers and hypoxia classifiers improved the ci up to 0.81 and 0.76, respectively, revealing their significant impact. For the validation cohort the baseline model showed ci = 0.66 for all patients and ci = 0.63 for patients with HVP16 DNA negative tumours. Including additional CSC markers or hypoxia classifiers improved these models only for CD44 and the 15-gene hypoxia classifier up to ci = 0.69 and ci = 0.65, respectively. Validation on the patient subgroup which received PORT-C led to higher ci values for all CSC markers and hypoxia classifiers, however, due to the low patient number with large confidence intervals.
Table 4.
Training and validation of multivariate Cox models for the endpoint loco-regional control containing cancer stem cell marker expression and hypoxia classifiers in addition to HPV16 DNA status and the clinical parameters ECE status, localisation oropharynx and hypopharynx. Shown is the concordance index (ci) with 95% confidence interval (CI) and the p-value testing the hypothesis ci = 0.5. Validation was also performed for the subgroup of patients who received radiochemotherapy (RCT).
| Training cohort |
Validation cohort |
Validation cohort, RCT only |
||||
|---|---|---|---|---|---|---|
| Included variables | ci (95% CI) | p-Value | ci (95% CI) | p-Value | ci (95% CI) | p-Value |
| All patients | ||||||
| Baseline (clinical parameters, HPV16 DNA status) | 0.76 (0.67–0.83) | <0.01 | 0.66 (0.58–0.75) | <0.01 | 0.69 (0.40–0.91) | 0.15 |
| CD44 > 0.2 | 0.76 (0.68–0.83) | <0.01 | 0.69 (0.60–0.77) | <0.01 | 0.77 (0.55–0.93) | 0.02 |
| SLC3A2 > −3.135 | 0.77 (0.68–0.84) | <0.01 | 0.66 (0.56–0.76) | <0.01 | 0.72 (0.44–0.92) | 0.10 |
| MET > −4.135 | 0.78 (0.69–0.85) | <0.01 | 0.64 (0.54–0.74) | 0.01 | 0.75 (0.50–0.92) | 0.04 |
| 15-gene signature | 0.80 (0.73–0.87) | <0.01 | 0.68 (0.58–0.77) | <0.01 | 0.74 (0.44–0.93) | 0.10 |
| 26-gene signature | 0.79 (0.71–0.85) | <0.01 | 0.67 (0.58–0.75) | <0.01 | 0.71 (0.43–0.91) | 0.11 |
| CD44 > 0.2, 15-gene signature | 0.80 (0.72–0.87) | <0.01 | 0.69 (0.60–0.78) | <0.01 | 0.78 (0.53–0.94) | 0.04 |
| SLC3A2 > −3.135, 15-gene signature | 0.81 (0.73–0.87) | <0.01 | 0.67 (0.58–0.75) | <0.01 | 0.76 (0.48–0.95) | 0.07 |
| MET > −4.135, 15-gene signature | 0.81 (0.74–0.88) | <0.01 | 0.66 (0.56–0.75) | <0.01 | 0.75 (0.47–0.93) | 0.07 |
| Patients with HPV16 DNA negative tumours | ||||||
| Baseline (clinical parameters) | 0.66 (0.55–0.77) | 0.01 | 0.63 (0.54–0.71) | 0.01 | 0.60 (0.21–0.87) | 0.49 |
| CD44 > 0.2 | 0.68 (0.58–0.77) | <0.01 | 0.63 (0.53–0.73) | 0.01 | 0.70 (0.41–0.90) | 0.13 |
| SLC3A2 > −3.135 | 0.69 (0.58–0.79) | <0.01 | 0.62 (0.51–0.71) | 0.03 | 0.63 (0.26–0.89) | 0.38 |
| MET > −4.135 | 0.71 (0.60–0.81) | <0.01 | 0.58 (0.47–0.70) | 0.16 | 0.66 (0.31–0.90) | 0.25 |
| 15-gene signature | 0.74 (0.65–0.82) | <0.01 | 0.64 (0.54–0.74) | 0.01 | 0.64 (0.25–0.91) | 0.36 |
| 26-gene signature | 0.71 (0.62–0.80) | <0.01 | 0.62 (0.53–0.71) | 0.01 | 0.61 (0.26–0.88) | 0.42 |
| CD44 > 0.2, 15-gene signature | 0.74 (0.65–0.82) | <0.01 | 0.65 (0.54–0.74) | 0.01 | 0.69 (0.36–0.91) | 0.19 |
| SLC3A2 > −3.135, 15-gene signature | 0.76 (0.68–0.84) | <0.01 | 0.62 (0.52–0.72) | 0.03 | 0.68 (0.33–0.92) | 0.24 |
| MET > −4.135, 15-gene signature | 0.76 (0.68–0.84) | <0.01 | 0.61 (0.50–0.71) | 0.05 | 0.66 (0.29–0.91) | 0.29 |
Discussion
In our previous multicentre retrospective study, we showed that HPV status, tumour expression of CSC markers and hypoxia-related genes play a prognostic role in patients with locally advanced HNSCC, who were treated by PORT-C [15], [18]. In the current study, these results were validated on an earlier, independent cohort with patients who received PORT or PORT-C between 1999 and 2006. Despite significant differences in patient characteristics and treatment outcome between the two cohorts, the prognostic ability of the CSC markers CD44 protein, CD44 and SLC3A2 could be confirmed in univariate analyses; for the 15-gene hypoxia classifier a statistical trend was obtained. This underlines the robustness of the evaluated marker set. Furthermore, it could be shown that CD44 and the 15-gene hypoxia classifier moderately improved the ci of the published multivariate Cox models. However, this improvement did not reach statistical significance.
The validation cohort consisted of patients treated between 1999 and 2006. These patients showed favourable clinical parameters with less R1-resected tumours and less lymphnodes showing extracapsular extension. However, LRC and OS were significantly lower compared to the later treated training cohort [15]. This may be explained by the lower number of oropharyngeal cancers in this validation cohort, which show a significantly improved outcome due to a high radiosensitivity associated with positive HPV infection status [21], [22] and the higher number of tumours in the oral cavity that generally show poorer outcome. From the literature, there is also conflicting data on the value of HPV as a prognostic factor for non-oropharyngeal cancers. Lassen et al. showed that the radiotherapy outcome in the subgroup of non-oropharyngeal tumours does not differ by their p16 status [12]. In contrast, Chung et al. demonstrated, that HPV infection may also play a role in a subset of non-oropharyngeal cancers [23], suggesting that this needs further exploration. Furthermore, only 40 of the 152 patients received simultaneous radiochemotherapy since this had not been a standard treatment at that time. Technological advances in radiotherapy [3] and diagnostics may also have contributed to a better outcome of the patients in the training cohort. Despite these significant differences a statistical trend for improved LRC for patients with HPV16 DNA positive tumours could be obtained, which is in agreement with our previous study [15].
Validation of the multivariate Cox models published in [18] showed a generally lower prognostic performance for the validation cohort than for the training cohort (training: ci 0.66–0.81, validation: ci 0.58–0.69). This difference is expected, as the models were adjusted to the training data. Furthermore, cut-offs for the continuous CSC marker expressions as well as the clustering procedure for hypoxia classification were optimised for the training cohort. However, with an average ci of 0.67 for the total validation cohort and of 0.62 for patients with HPV16 DNA negative tumours, the multivariate models were still prognostic with an acceptable performance. The large difference in ci between all patients and those patients with HPV16 DNA negative tumours shows that the HPV16 DNA status is a strong prognosticator for LRC. Still, CD44 and the 15-gene hypoxia classifier were able to further improve the models, also in the validation cohort. At first glance, it is surprising that tumour hypoxia-associated gene expression of the resected tumour is associated with the outcome of postoperative radiotherapy. As discussed before [18], it is very unlikely that the low number of any remaining tumour cells after surgery differs in their hypoxia status. However, this suggests that hypoxia may have the potential to impact the outcome after postoperative radiotherapy also by other radiobiological mechanisms than by direct biochemical or radiobiological effects. In previous data from our laboratory, it was shown that pre-treatment hypoxia has an impact on local tumour control after radiotherapy also when radiotherapy was applied under homogenous anoxic conditions [24].
The prognostic ability of the putative CSC marker MET could not be confirmed by the validation cohort. However, the inclusion of MET resulted in multivariate models with higher ci values if only patients of the validation cohort who received PORT-C were considered. These models were not significant, which could be due to (1) the lower incidence of HPV positive tumours, which has shown to be associated with a lower CSC frequency [25] and (2) the low number of patients receiving PORT-C in the validation cohort. Furthermore, in the validation cohort, patients only received PORT-C within clinical trials, i.e. a selection of patients with more favourable clinical characteristics is likely, leading to a more homogeneous patient group compared to the total cohort. In addition, diagnostics and radiotherapy treatment have been technologically improved over the last years, such that the consideration of biological aspects might become even more important.
It should be noted that in the previously reported DKTK-ROG cohort [18] CD44 expression was determined by real-time PCR (RT-PCR) analysis because the nanoString CD44 probe design was invalid. In the present validation cohort, CD44 expression was measured by valid nanoString probes. Therefore, the validation of CD44 is challenging, as its expression in the two cohorts was determined by different methods and the cut-off value 0.2 obtained for RT-PCR might be different for nanoString. In general, many genes of the validation cohort showed significantly different mean expression values between the cohorts, i.e. an average shift. This is problematic if the expressions are dichotomized at cut-off values, as these cut-offs may lead to imbalanced patient groups for the validation cohort. The same holds for the hypoxia classifiers built by k-means clustering. In the validation cohort, this shift in gene expressions caused the hypoxia classifiers to identify significantly more hypoxic tumours compared to the training cohort. Renormalizing the validation data to the training data, as described in [26], gives the same fraction of more and less hypoxic tumours for both cohorts and even leads to a significant impact of hypoxia status on LRC, in contrast to the statistical trend shown in Table 3. However, this method is not applicable for individual patient prognosis, as required in clinical trials on treatment adaptation, and may warrant the inclusion of reference samples in future analyses.
The model validation showed a better performance for the subgroup of patients, which received PORT-C than for all patients. This indicates that the prognostic ability of CSC markers and hypoxia classifiers might be stronger for a patient cohort, which is more similar to the cohort originally used in [18]. However, at the time of treatment of the validation cohort simultaneous radiochemotherapy was applied only within clinical studies [7], [8], [9]. This potentially led to a higher homogeneity with better clinical performance of the patient subgroup treated with PORT-C, which is important for the interpretation of the biological heterogeneity of the tumours. Currently, a homogeneous patient cohort with locally advanced HNSCC treated with PORT-C is being recruited within a prospective clinical trial of the DKTK-ROG, which will allow for further validation of the models.
Taken together, this validation study confirmed the prognostic value of the HPV infection status, CSC marker expression of CD44 protein, CD44 and SLC3A2 and tumour hypoxia status presented in [18] for patients with locally advanced HNSCC receiving postoperative radiotherapy or radiochemotherapy. While a lower performance of the prognostic models is expected due to the older validation dataset and several differences between the cohorts, the significant validation results indicate the robustness of these biomarkers. After further validation on a currently recruiting prospective clinical trial of the DKTK-ROG these models may help to stratify patients for individualised treatment de-escalation or intensification strategies.
Conflict of interest
The authors declare no conflict of interest regarding the present manuscript.
Acknowledgements
The authors gratefully acknowledge the excellent technical assistance by Mrs. Liane Stolz-Kieslich, Mrs. Sigrid Balschukat and Mrs. Daniela Friede. FFPE specimens were kindly provided by the Tumour- and Normal Tissue Bank (TNTB; Dr. Daniela E. Aust) of the University Cancer Center (UCC) of the University Hospital Dresden.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.ctro.2016.10.002.
Appendix A. Supplementary material
References
- 1.Leemans C.R., Braakhuis B.J.M., Brakenhoff R.H. The molecular biology of head and neck cancer. Nat Rev Cancer. 2011;11:9–22. doi: 10.1038/nrc2982. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J., Soerjomataram I., Dikshit R., Eser S., Mathers C., Rebelo M. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 3.Baumann M., Krause M., Overgaard J., Debus J., Bentzen S.M., Daartz J. Radiation oncology in the era of precision medicine. Nat Rev Cancer. 2016;16:234–249. doi: 10.1038/nrc.2016.18. [DOI] [PubMed] [Google Scholar]
- 4.Chaturvedi A.K., Anderson W.F., Lortet-Tieulent J., Curado M.P., Ferlay J., Franceschi S. Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31:4550–4559. doi: 10.1200/JCO.2013.50.3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sturgis E.M., Cinciripini P.M. Trends in head and neck cancer incidence in relation to smoking prevalence: an emerging epidemic of human papillomavirus-associated cancers? Cancer. 2007;110:1429–1435. doi: 10.1002/cncr.22963. [DOI] [PubMed] [Google Scholar]
- 6.Habbous S., Chu K.P., Qiu X., La Delfa A., Harland L.T.G., Fadhel E. The changing incidence of human papillomavirus-associated oropharyngeal cancer using multiple imputation from 2000 to 2010 at a Comprehensive Cancer Centre. Cancer Epidemiol. 2013;37:820–829. doi: 10.1016/j.canep.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 7.Bernier J., Domenge C., Ozsahin M., Matuszewska K., Lefèbvre J.-L., Greiner R.H. Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med. 2004;350:1945–1952. doi: 10.1056/NEJMoa032641. [DOI] [PubMed] [Google Scholar]
- 8.Cooper J.S., Pajak T.F., Forastiere A.A., Jacobs J., Campbell B.H., Saxman S.B. Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med. 2004;350:1937–1944. doi: 10.1056/NEJMoa032646. [DOI] [PubMed] [Google Scholar]
- 9.Fietkau R., Lautenschläger C., Sauer R., Dunst J., Becker A., Baumann M. Postoperative concurrent radiochemotherapy versus radiotherapy in high-risk SCCA of the head and neck: Results of the German phase III trial ARO 96-3. J Clin Oncol. 2006;24:5507. [Google Scholar]
- 10.Fakhry C., Gillison M.L. Clinical implications of human papillomavirus in head and neck cancers. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24:2606–2611. doi: 10.1200/JCO.2006.06.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ang K.K., Harris J., Wheeler R., Weber R., Rosenthal D.I., Nguyen-Tân P.F. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med. 2010;363:24–35. doi: 10.1056/NEJMoa0912217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lassen P., Primdahl H., Johansen J., Kristensen C.A., Andersen E., Andersen L.J. Impact of HPV-associated p16-expression on radiotherapy outcome in advanced oropharynx and non-oropharynx cancer. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2014;113:310–316. doi: 10.1016/j.radonc.2014.11.032. [DOI] [PubMed] [Google Scholar]
- 13.Swick A.D., Chatterjee A., Costa A.-M.A., Kimple R.J. Modulation of therapeutic sensitivity by human papillomavirus. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2015;116:342–345. doi: 10.1016/j.radonc.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong A., Zhang X., Jones D., Veillard A.-S., Zhang M., Martin A. Relationships between p53 mutation, HPV status and outcome in oropharyngeal squamous cell carcinoma. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2016;118:342–349. doi: 10.1016/j.radonc.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 15.Lohaus F., Linge A., Tinhofer I., Budach V., Gkika E., Stuschke M. HPV16 DNA status is a strong prognosticator of loco-regional control after postoperative radiochemotherapy of locally advanced oropharyngeal carcinoma: results from a multicentre explorative study of the German Cancer Consortium Radiation Oncology Group (DKTK-ROG) Radiother Oncol J Eur Soc Ther Radiol Oncol. 2014;113:317–323. doi: 10.1016/j.radonc.2014.11.011. [DOI] [PubMed] [Google Scholar]
- 16.Toustrup K., Sørensen B.S., Nordsmark M., Busk M., Wiuf C., Alsner J. Development of a hypoxia gene expression classifier with predictive impact for hypoxic modification of radiotherapy in head and neck cancer. Cancer Res. 2011;71:5923–5931. doi: 10.1158/0008-5472.CAN-11-1182. [DOI] [PubMed] [Google Scholar]
- 17.Eustace A., Mani N., Span P.N., Irlam J.J., Taylor J., Betts G.N.J. A 26-gene hypoxia signature predicts benefit from hypoxia-modifying therapy in laryngeal cancer but not bladder cancer. Clin Cancer Res An Off J Am Assoc Cancer Res. 2013;19:4879–4888. doi: 10.1158/1078-0432.CCR-13-0542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Linge A., Löck S., Gudziol V., Nowak A., Lohaus F., von Neubeck C. Low cancer stem cell marker expression and low hypoxia identify good prognosis subgroups in HPV(-) HNSCC after Postoperative radiochemotherapy: a multicenter study of the DKTK-ROG. Clin Cancer Res An Off J Am Assoc Cancer Res. 2016;22:2639–2649. doi: 10.1158/1078-0432.CCR-15-1990. [DOI] [PubMed] [Google Scholar]
- 19.Skripcak T., Belka C., Bosch W., Brink C., Brunner T., Budach V. Creating a data exchange strategy for radiotherapy research: towards federated databases and anonymised public datasets. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2014;113:303–309. doi: 10.1016/j.radonc.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Harrell F. Springer; 2001. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. [Google Scholar]
- 21.Kawakami H., Okamoto I., Terao K., Sakai K., Suzuki M., Ueda S. Human papillomavirus DNA and p16 expression in Japanese patients with oropharyngeal squamous cell carcinoma. Cancer Med. 2013;2:933–941. doi: 10.1002/cam4.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salazar C.R., Smith R.V., Garg M.K., Haigentz M., Schiff B.A., Kawachi N. Human papillomavirus-associated head and neck squamous cell carcinoma survival: a comparison by tumor site and initial treatment. Head Neck Pathol. 2014;8:77–87. doi: 10.1007/s12105-013-0486-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chung C.H., Zhang Q., Kong C.S., Harris J., Fertig E.J., Harari P.M. P16 protein expression and human papillomavirus status as prognostic biomarkers of nonoropharyngeal head and neck squamous cell carcinoma. J Clin Oncol Off J Am Soc Clin Oncol. 2014;32:3930–3938. doi: 10.1200/JCO.2013.54.5228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yaromina A., Thames H., Zhou X., Hering S., Eicheler W., Dörfler A. Radiobiological hypoxia, histological parameters of tumour microenvironment and local tumour control after fractionated irradiation. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2010;96:116–122. doi: 10.1016/j.radonc.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 25.Vlashi E., Chen A.M., Boyrie S., Yu G., Nguyen A., Brower P.A. Radiation-induced dedifferentiation of head and neck cancer cells into cancer stem cells depends on human papillomavirus status. Int J Radiat Oncol Biol Phys. 2016;94:1198–1206. doi: 10.1016/j.ijrobp.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Toustrup K., Sørensen B.S., Metwally M.A.H., Tramm T., Mortensen L.S., Overgaard J. Validation of a 15-gene hypoxia classifier in head and neck cancer for prospective use in clinical trials. Acta Oncol. 2016:1–8. doi: 10.3109/0284186X.2016.1167959. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.