Summary
Background
Radiation exposure due to computed tomography (CT) has become an important issue, as the number of CT examinations has been increasing worldwide. Radiation doses associated with CT are higher in comparison to other imaging procedures. CT-related radiation doses should be monitored and controlled in order to ensure reduction of radiation exposure and optimization of image quality. The aim of this study was to evaluate radiation doses in adult patient who underwent routine CT brain examinations, and to assess how CT scanning protocols affect patient doses in practice.
Material/Methods
A total of 118 patients underwent brain CT at two radiology departments equipped with 64-slice CT scanners, Khartoum, Sudan. Patient doses regarding weighted CT dose index (CTDIw) and dose length product (DLP) values were recorded. Quality control tests were performed for both scanners.
Results
The mean CTDIw values ranged from 62.9 to 65.8 mGy, DLP values ranged from 1003.7 to 1192.5 mGy, and the effective dose varied from 2.4 to 3.7 mSv.
Conclusions
Patient doses in this study was higher compared to previous research, suggesting that patients exposed to unnecessary radiation. Therefore, optimization of radiation doses with the use of specified imaging protocols, well-documented indications for CT, training of technicians, and quality control programs will reduce the necessary radiation doses. Establishment of the diagnostic reference level is recommended for further dose reduction.
Keywords: Multidetector Computed Tomography; Radiation Dosage; Tomography, X-Ray Computed
Background
The risk of cancer and radiation-related mortality that can be associated with computed tomography (CT) have been widely addressed. Huang et al. determined that radiation doses were up to 27.7 mSv, and the lifetime risk of cancer was up to 0.37%, in people over 50 years of age who underwent CT angiography (CTA) [1]. A study by Brenner et al. suggested that CT significantly increases the lifetime radiation risk in pediatric patients, as compared to adults [2]. Proper indications for CT and use of tailored CT protocols is important in order to decrease potential harms of radiation exposure [3]. The number of scans performed in the past years has increased, as compared to the previous decade; this is due to an improvement in speed of acquisition and image quality [4]. The use of multi-detector rows advanced very rapidly from 4 slices to even 640 slices, and dual-source multidetector CT (MDCT). Acquisition of a large number of thin slices in a single rotation enabled new applications, such as cardiac CT, whole-body CT, and CT colonography. It also improved patient throughput and workflow [5].
Management of radiation doses in CT is an urgent issue to all medical practitioners involved in CT. It has been estimated that the collective dose from CT procedure ranged between 60% up to 82% from all X-ray procedures [6,7]. Patients cumulative doses from CT procedures is increased due to higher effective doses per exam and introduction of new procedures. In CT imaging, there is no visible evidence that the patient has been overexposed since the quality of images might not be compromised. Several recent articles [5–8] stress that it is important to use the lowest radiation dose necessary to provide an image suitable for clinical purposes. Moreover, it is underscored that significant dose reductions can be achieved without compromising clinical efficacy.
Reducing radiation doses by optimizing scanning protocols and developing reference values is indicated. There is a wide variation in reported doses for similar procedures, as regards different and even the same scanner models [5]. The amount of radiation that the patient receives from CT depends on many parameters, including scanner design and acquisition protocol. Several methods have been described in the literature, as regards the assessment of efficient organ doses in CT examinations [9]. Two indexes, CTDIvol (computed tomography dose index volume) and DLP (dose length product) values are the two methods used to calculate the radiation exposure of patients who undergo CT [10].
CTDI (mGy) is derived from the dose delivery, along with a line which is parallel to the axis of rotation for the scanner (z-axis), and which is recorded for a single rotation of X-ray source. CTDI represents the average absorbed dose; CTDI is an equivalent of the dose value inside the irradiated slice (beam) that would result if the absorbed radiation dose profile was entirely concentrated to a rectangle of a width equal to the nominal beam width, with N being the number of independent (i.e. non-overlapping) slices that are acquired simultaneously. Accordingly, all dose contributions from outside the nominal beam width, i.e. the areas under the tails of the dose profile, are added to the area inside the slice [Nagel 2007]. In volume scans, CTDI estimates the average dose within the central region, which is known as multiple scan average dose (MSAD) [11].
The DLP is directly related to the patient (stochastic) risk and may be used to set reference values for a given type of CT examination in order to help ensure patient CT doses are as low as reasonably achievable [12]. DLP is obtained by multiplying the CTDIvol value by the scan range; the value of DLP apparently does not provide a dose value, which is also evident from its measurement unit (mGy·cm). Nevertheless, it serves as a surrogate of patient dose. This is especially meaningful when comparing dose levels, and it became accepted through the establishment of diagnostic reference levels (DRL) [13].
Aldrich et al. conducted a study to compare the dose length product (DLP) and effective radiation doses of CT examinations [14]. That study focused on the need to optimize the effective dose and conduct more research to determine which additional efforts are needed to reduce patient exposure. Optimizing exposure factors can help maintain low radiation doses, thereby reducing risks. The aim of this study was to evaluate radiation doses in adult patients undergoing routine CT brain examinations and to assess how CT scanning protocols affect patient organ doses in practice.
Material and Methods
Patient population
Data for this study were acquired with multidetector CT scanners (MSCT); 64 slice CT scanners (Toshiba, Sensation Aquilion 64) installed in 2010, in two hospitals in Khartoum state, Sudan. The Amal Hospital will be indicated as H1 and Zaytona Hospital as H2, respectively.
The CT scanners included in this study undergo a planned and regular preventive maintenance and have an annual quality assurance certificate issued by a biomedical engineer and certified medical physicists. This study was approved by a research ethics committee, and all data were managed with respecting HIPPA.
The data were collected with a questionnaire filled by a research assistant. The patient population consisted of 118 adult patients (63 male and 55 female) who underwent brain CT scan examinations. The mean age of patients was 35.6±3.6 years. Exposure-related parameters, kilovoltage (kV), tube current (mA), exposure time, slices thickness, the number of slices are demonstrated in Table 1.
Table 1.
CT parameters for adult brain procedures.
| Hospital | n* | Tube output (kVp) | mAs | Total mAs | Slice thickness | Number of Slices | Scan range (cm) |
|---|---|---|---|---|---|---|---|
| H1 | 87 | 120 | 242.8±1.2 | 319 | 5.5±1.7 | 24.4±0.7 | 15.3±1.1 |
| H2 | 31 | 120 | 162.9±4.8 | 289 | 6.5±3.1 | 23.9±1.3 | 14.9±0.9 |
Organ dose and risk assessment
CT multi-detector scanners generate patient dose indexes, CT dose CTDIvol and DLP, at the end of each examination. Radiation doses were calculated with ImpaCT software to measure effective dose, based on the scanner model, manufacturer, and scanning parameters as input data. The mean CTDIw, CTDIvol, DLP, and efficient dose values were characterized according to the region and protocol used (brain CT protocol was used for this study)
Estimation of cancer risk (R) following routine CT examination was calculated with the following equation:
R=ΣTrT.HT
where Tr is the risk coefficient from the International Commission on Radiation Protection (ICRP) Publication 103(2007) (ICRP 2007), and the HT is the organ-specific equivalent dose in organ T. The effective dose (E) was multiplied by the risk factor (r) to calculate the lifetime mortality risk (R) per examination [15].
Results and Discussion
The information acquired from the CT scanning parameters (e.g., kVp, mAs, slice thickness, scan range, and a number of slices) was used with other parameters to calculate CTDIw, DLO, and effective doses. It was observed that CT protocols that were used for both hospitals were highly standardized, and were similar to protocols from other studies. Adjusting scan protocols according to patient size was not considered in this study, although it is practiced in some hospitals [16]. The use of the constant potential for all CT procedure (120 kVp) with different patient sizes means that some patients may expose to unnecessary dose (Table 1). This change would be acceptable because of the difference in focus to iso-center distance in scanners. In CT, patients are exposed to high radiation doses. Therefore, the use of average dose values (CTDI or DLP) will provide less information regarding the radiation risks. Effective dose is the unit of choice in this situation (partial exposure); furthermore, comparisons between different procedures are possible with different imaging modalities. Table 2 shows the data collected from two hospitals, with a small variation in CTDIw, DLP, and effective dose values. Values in H2 were higher in comparison to H1, CTDIw was 62.9±1.3 and 65.8±0.9, DLP 1003.7±183.4 and 1192.5±85.6, effective dose 2.4±1.5 and 3.7±0.9, respectively.
Table 2.
CTDIw, DLP, and effective dose values from two hospitals in Khartoum state.
| Hospital | CTDIw (mGy) | DLP (mGy·cm) | Effective dose (mSv) | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| H1 | 62.9 | 1.3 | 1003.7 | 183.4 | 2.4 | 1.5 |
| H2 | 65.8 | 0.9 | 1192.5 | 85.6 | 3.7 | 0.9 |
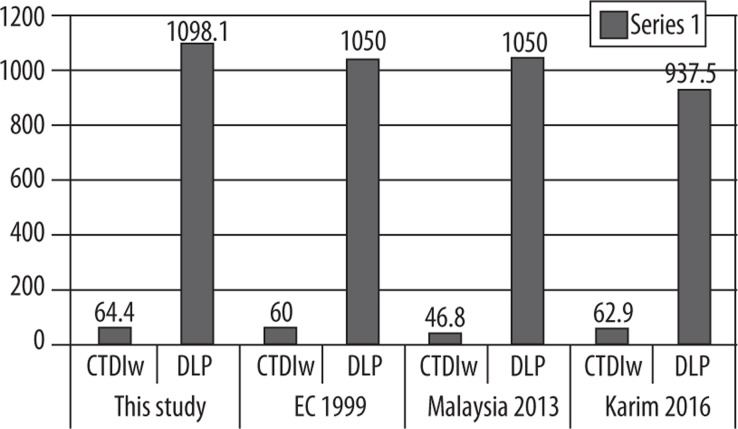
The mean effective dose reported in this study was 3.5±1.4 mSv, and it was comparable to others studies that used the same scanner type and similar scanning protocols. The mean values of CTDIw and DLP, compared to the diagnostic reference levels (DRL) of the European Commissioner (EC) [17], Malaysia, Ministry of Health 2013 [18], and [19], are presented in Figure 1.
Figure 1.
Comparison between CTDIw and DLP values in various studies
CTDIw values that were observed in this study were slightly higher than those observed in other studies (EC1999, by 0.9%), (Karim 2016, by 1%), and (Malaysia 2013, by almost 7.2%). All other readings in Table 2 and DLP values observed in this study are higher than those observed in other studies (EC1999 by 0.9%), (Malaysia 2013 and Karim 2016 by 0.8%). CT examinations contributed significantly to diagnosing different diseases; however, radiation exposure is significantly higher, as compared with other radiological examinations. Dose monitoring during CT procedures and re-evaluation of equipment and techniques are mandatory to keep the radiation risk as low as reasonably achievable. Justification of CT scan examinations, when sensitive organs are involved, is highly recommended, especially in children and patients with chronic diseases who need continuous follow-up. If the clinical situation and disease of the patient permit, one can increase the pitch of examination. CT requests must be generated only by qualified medical practitioners and justified by both the referring doctor and the radiologist. CT scanner quality assurance and quality control programs are critical to maintaining radiation doses as low as possible. Careful optimization of imaging protocols must is essential to ensure that they are designed to according to the clinical need and patient size [22].
Conclusions
In this study, we assessed radiation doses of routine CT brain examinations performed with two new multi-detectors 64 scanners installed in the Khartoum state, Sudan. Although both hospitals used the same scanner type and protocol, there was a variation in dose measurement; patient and organ factors can be considered as a variable that justifies this difference. The obtained radiation values were slightly higher than the values observed in the literature. Our data should be used for further improvement of standardized protocols, considering tube current, scan range, and patient size factors. It is necessary to establish the minimum exposure threshold that will deliver adequate image quality in all applications; preferably, this threshold should be expressed in terms of clinical effectiveness. It is recommended to establish reference dose levels (RDL) in Sudan and optimize examinations in order to improve quality and ensure patient safety.
Acknowledgement
The authors would like to thank the hospitals CT scan technologists who helped in data collection and the hospital administration and colleagues who give full support to this study
References
- 1.Huang B, Li J, Law MWM, et al. Radiation dose and cancer risk in retrospectively and prospectively ECG-gated coronary angiography using 64-slice multidetector CT. Br J Radiol. 2010;83(986):152–58. doi: 10.1259/bjr/29879495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brenner DJ, Elliston CD, Hall EJ, Berdon WE. Estimated risks of radiation-induced fatal cancer from pediatric CT. Am J Roentgenol. 2001;176(2):289–96. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 3.Brenner DJ, Hall EJ. Computed tomography – an increasing source of radiation exposure. N Engl J Med. 2007;357(22):2277–84. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 4.Krille L, Dreger S, Schindel R, et al. Risk of cancer incidence before the age of 15 years after exposure to ionising radiation from computed tomography: Results from a German cohort study. Radiat Environ Biophys. 2015;54(1):1–12. doi: 10.1007/s00411-014-0580-3. [DOI] [PubMed] [Google Scholar]
- 5.Dougeni E, Faulkner K, Panayiotakis G. A review of patient dose and optimisation methods in adult and paediatric CT scanning. Eur J Radiol. 2012;81(4):e665–83. doi: 10.1016/j.ejrad.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 6.Huda W, Ogden KM, Khorasani MR. Converting dose-length product to effective dose at CT. Radiology. 2008;248(3):995–1003. doi: 10.1148/radiol.2483071964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valentin J. International Commission on Radiation Protection: Managing patient dose in multi-detector computed tomography(MDCT). ICRP Publication 102. Ann ICRP. 2007;37(1):1–79, iii. doi: 10.1016/j.icrp.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 8.McCollough C, Cody D, Edyvean S, Geise R. The measurement, reporting, and management of radiation dose in CT. Report of AAPM Task Group. 2008:1–34. [Google Scholar]
- 9.Damilakis J. How to measure the performance. Esr. 2006 Apr;:2010. [Google Scholar]
- 10.Chatzoglou V, Kottou S, Nikolopoulos D, et al. Management and optimisation of the dose in computed tomography via a dose tracking software. OMICJ Journal of Radiology. 2016:5(July). [Google Scholar]
- 11.Shope TB, Gagne RM, Johnson GC. A method for describing the doses delivered by transmission x-ray computed tomography. Med Phys. 1981;8(1981):488–95. doi: 10.1118/1.594995. [DOI] [PubMed] [Google Scholar]
- 12.Dunn M. National survey of doses from CT in the UK. National survey of doses from CT in the UK. 2003;2016 doi: 10.1259/bjr/93277434. January 2007. [DOI] [PubMed] [Google Scholar]
- 13.Kalender WA. X-ray computed tomography. Phys Med Biol. 2006;51(13):R29–43. doi: 10.1088/0031-9155/51/13/R03. [DOI] [PubMed] [Google Scholar]
- 14.Aldrich JE, Bilawich A-M, Mayo JR. Radiation doses to patients receiving computed tomography examinations in British Columbia. Can Assoc Radiol J. 2006;57(2):79–85. [PubMed] [Google Scholar]
- 15.Karim MKA, Hashim S, Bradley DA, et al. Radiation doses from computed tomography practice in Johor Bahru, Malaysia. Radiat Phys Chem. 2016;121:69–74. [Google Scholar]
- 16.Brady SL, Mirro AE, Moore BM, Kaufman RA. How to appropriately calculate effective dose for CT using either size-specific dose estimates or dose-length product. Am J Roentgenol. 2015;204(5):953–58. doi: 10.2214/AJR.14.13317. [DOI] [PubMed] [Google Scholar]
- 17.Menzel H, Schibilla H, Teunen D. European guidelines on quality criteria for computed tomography – Guidelines on radiation dose to the patient. European Commision. 2000:Appendix 1. [Google Scholar]
- 18.Kementerian Kesihatan Malaysia . 2013. Malaysian Diagnostic Reference Levels in Medical Imaging (Radiology) [Google Scholar]
- 19.Karim MKA, Hashim S, Sabarudin A, et al. Evaluating organ dose and radiation risk of routine CT examinations in Johor Malaysia. Sains Malaysiana. 2016;45(4):567–73. [Google Scholar]