Abstract
Introduction
Surgical readmissions are common, costly, and the focus of national quality improvement efforts. Given the relatively high readmission rates among vascular patients, pay-for-performance initiatives such as Medicare's Hospital Readmissions Reduction Program have targeted vascular surgery for increased scrutiny in the near future. Yet, the extent to which institutional case-mix influences hospital profiling remains unexplored. We sought to evaluate whether higher readmission rates in vascular surgery are a reflection of worse performance or of treating sicker patients.
Methods
This retrospective observational cohort study of the national Medicare population includes 479,047 beneficiaries undergoing lower extremity revascularization (LER) in 1,701 hospitals from 2005-2009. We employed hierarchical logistic regression to mimic CMS' methodology accounting for age, gender, pre-existing comorbidities, and differences in hospital operative volume. We estimated 30-day risk-standardized readmission rates (RSRR) for each hospital when including (1) all LER patients; (2) claudicants; or (3) high-risk patients (rest pain, ulceration or tissue loss). We stratified hospitals into quintiles based upon overall RSRR for all LERs and examined differences in RSRR for claudicants and high-risk patients between and within quintiles. Next, we evaluated differences in case-mix (the proportion of claudicants and high-risk patients treated) across quintiles. Finally, we simulated differences in the receipt of penalties before and after adjusting for hospital case-mix.
Results
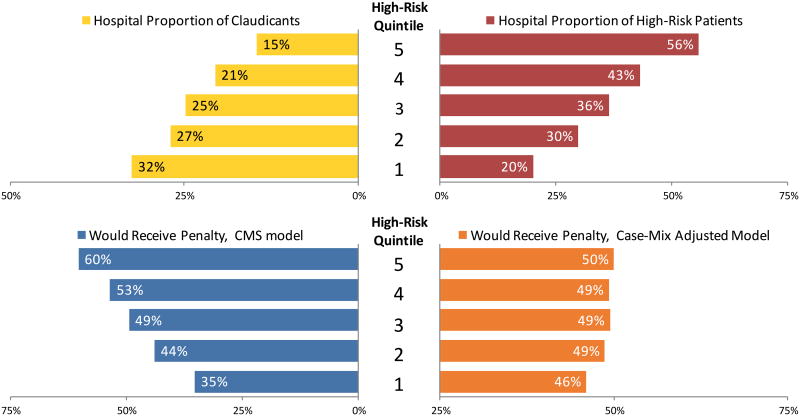
Readmission rates varied widely by indication – 7.3% (claudicants) versus 19.5% (high-risk). Even after adjusting for patient demographics, length of stay, and discharge destination, high-risk patients were significantly more likely to be readmitted (OR 1.76, 95% CI 1.71-1.81). The Best hospitals (top quintile) under the HRRP treated a much lower proportion of high-risk patients compared to the Worst hospitals (bottom quintile) (20% vs 56%, P <0.001). In the absence of case-mix adjustment, we observed a stepwise increase in the proportion of hospitals penalized as the proportion of high-risk patients treated increased (35% to 60%, P<0.001). However, after case-mix adjustment, there were no differences between quintiles in the proportion of hospitalized penalized (50% to 46%, P = 0.30).
Conclusions
Our findings suggest that the differences in readmission rates following lower extremity revascularization are largely driven by hospital case-mix rather than true differences in quality.
1 Introduction
In an effort to decrease cost and improve quality in health care, reducing readmissions has become a popular target of pay-for-performance programs. Currently, the largest pay-for-performance program aimed at reducing readmissions is the Center for Medicare and Medicaid Services' (CMS) Hospital Readmissions Reduction Program (HRRP).[1] While originally encompassing only three medical conditions, HRRP has recently been expanded to include hip and knee surgery.[2] Further, CMS has indicated that vascular procedures will be included in future rounds of expansion given the high readmission rate among vascular patients.[3]
The growing enthusiasm for using readmissions as a marker of hospital quality following vascular surgery has prompted efforts to better understand the reasons for readmission. However, the extent to which existing methodology, for profiling hospitals on medical readmissions, may be effectively applied to surgery is unknown. Since the same surgical procedure is often performed for a variety of indications, there is a significant risk of confounding by indication.[4] For example, Rutherford classification is a strong predictor of adverse outcomes following lower extremity revascularization (LER). Data from single institution studies and clinical trials have show that readmission rates increase as patients progress from intermittent claudication to tissue loss.[5,6] However, to date, the extent to which operative indication impacts hospital rankings remains unknown.
In this context, we sought to better understand the relationship between operative indication for lower extremity revascularization and readmission. Specifically, we addressed three questions. (1) At the patient-level, what is the association between operative indication and readmission? (2) Do hospitals with lower readmission rates perform better than other hospitals with high-risk patients or do they simply treat less high-risk patients? (3) What would be the impact on hospital profiling of adjusting for the mix of high versus low-risk patients?
2 Methods
2.1 Dataset and patient population
We used CMS' MEDPAR national analytic files capturing 100% fee-for-service beneficiaries for 2005-2009. We included all patients with the following International Classification of Disease Version 9 (ICD-9) procedural codes – 38.08, 38.18, 38.38, 38.48, 38.88, 39.25, 39.29, 39.35, 39.90. We excluded patients suffering in-hospital mortality because these patients did not have the opportunity to be readmitted. We also excluded patients who underwent surgery in hospitals performing less than 50 LER procedures per year. This approach mirrors CMS' exclusion of low-volume hospitals from HRRP penalties.[7]
2.2 Operative Indication
Our primary exposure variable was operative indication which served as our proxy for risk. Using ICD-9 codes, we created a three-level variable based ICD-9 diagnostic codes - low risk (ie claudication [440.21]), high-risk (rest pain [440.22], or tissue loss [440.23, 440.24]), and intermediate risk (patients undergoing LEAB who did not have a diagnostic code that specifically described their level of peripheral arterial occlusive disease).
2.3 Primary outcome measure
Our primary outcome measure was 30-day any-cause readmission to any acute care hospital.
2.4 Multilevel Modeling of Risk-Standardized Readmission Rates (RSRR)
To make comparisons between readmissions rates across hospitals, we employed multilevel modeling to adjust for (1) differences in pre-operative patient risk factors that may impact the likelihood of readmission, and (2) statistical noise generated by low case volumes at some hospitals. Failing to account for the former runs the risk of misclassifying hospitals as poor performers because they treat sicker or older patients. Failure to account for procedural volume runs the risk of erroneously concluding that a hospital performing 1,000 operations with 500 readmissions has similar performance to a hospital performing 10 operations with 5 readmissions. While the tabulated readmission rate for both hospitals is 50%, the high volume hospital more assuredly a poor performer. In contrast, the low volume hospital may be a poor performer or may have merely been unlucky 5 times; without a greater sample of patients from that hospital it is difficult to differentiate using only observed performance.
To estimate hospital RSRRs, we employed a two step process. First, we used multiple logistic regression to generate a predicted probability of readmission for each patient based upon variables included in the CMS model - age, gender, non-elective admission and comorbidities. Although available, we specifically excluded race and socioeconomic status to mirror the model used by CMS for the HRRP. This predicted probability was then used to generate the log odds of the patient's predicted probability of readmission. Conversion to log-odds is necessary when using a logistic link function to meet the requirement of linearity with respect to a dichotomous outcome (ie readmitted versus not readmitted).[8]
The second step in estimating hospital RSRR uses a multilevel mixed-effects model (STATA: xtmelogit) to account for age, gender and comorbidities (fixed-effect), as well as the differences in reliability due to hospital volume (random intercept). The random effect parameter from this equation is used to estimate RSRRs. This approach has been extensively described and validated in prior studies of hospital profiling.[9,10] Moreover, CMS' HRRP uses multilevel modeling to calculate RSRRs and penalties.[7] We used this two-step approach to estimate three readmission rates for each hospital - a rate based on hospital performance for all lower extremity revascularizations, a rate based on only claudicants, and a rate based on only high-risk patients.
2.5 Analytic Approach
To provide a more intuitive understanding of relative performance we divided hospitals into quintiles based upon this CMS-RSRR. We designated the 20% of hospitals with the lowest CMS-RSRR to be the “Best” hospitals and the 20% of hospitals with the highest CMS-RSRR to be the “Worst.”
2.5.1 Operative Indication and Readmission
First, we sought to determine if, at the patient level, operative indication is independently associated with readmission. Specifically, we employed multiple logistic regression models determine the impact of operative indication on readmission after sequentially adjusting for selected patient demographics (CMS' model), the occurrence of a major complication during the index hospitalization, length of stay (LOS), and the patient's discharge destination (home, home with home health, skilled nursing facility, nursing home).
2.5.2 Proportion of High-Risk Patients Treated and Readmission
For the first part of this analysis, we quantified the variation in the proportion of claudicants versus high-risk patients treated by the Best and Worst hospitals (case-mix). We used t-tests to determine if these differences were statistically significant.
The second part of this investigation examined the relative difference in RSRR between the claudicants and high-risk patients treated in the same hospital. We hypothesized that the Best and Worst hospitals would have similar differences in the RSRR. In other words, the Best hospitals do not have improved success at preventing readmissions in high-risk patients. We used t-tests to assess whether differences were statistically significant. We also used multiple logistic regression to determine odds ratios for readmission comparing high-risk patients to claudicants. This model adjusted for patient factors (age, gender, comorbidities) and hospital factors (percent of Black patients treated, index hospitalization length-of-stay, percent of major complications, hospital procedural volume, within hospital Delta, teaching status, and safety-net hospital status).
2.5.3 Impact on HRRP Performance of Adjusting for Indication
To evaluate the effect of adjusting for case-mix on HRRP performance, we conducted tests to evaluate the proportion of hospitals projected to receive a penalty under CMS' model and under a case-mix adjusted model. Receipt of penalties under HRRP is based on the hospital's O:E ratio and the size of any penalties is proportionate to its O:E ratio. If this O:E ratio was greater than 1, then the hospital would receive a penalty. Second, we used t-tests to compare the number of hospitals projected to receive lower penalties under case mix adjusted model. If the O:E ratio was lower after case-mix adjustment compared to CMS' model, then that hospital would receive a lower penalty.[7]
2.6 Results
We evaluated 479,047 procedures performed in 1,701 hospitals. Demographic characteristics are detailed in Table I. The overall unadjusted hospital 30-day readmission rate was 15.0% (standard deviation [SD] 4.74%, range 2.2% - 40.3%). Readmission rates varied by operation with open bypass patients having higher readmission rates. Table II. The Best performing hospitals under the HRRP had a readmission rate of 11.7% (observed-to-expected [O:E] ratio 0.81) while the Worst performers had a readmission rate of 17.2% (O:E ratio 1.27).
Table 1. Patient Demographics by Risk-Classification.
| Characteristic | Risk-Classification Based on Operative Indication | ||
|---|---|---|---|
|
| |||
| Claudication | High-Risk | Unspecified | |
| Number of Patients | 130,841 | 171,251 | 176,955 |
| Age, mean ± SD | 74.6 ± 6.4 | 76.4 ± 8.1 | 75.8 ± 7.5 |
| Female Gender (%) | 44% | 48% | 48% |
| Black Race (%) | 9% | 16% | 11% |
| >3 Comorbidities (%) | 37% | 52% | 48% |
| non-Elective admission (%) | 21% | 45% | 44% |
| Endovascular (%) | 64% | 51% | 56% |
All differences are statistically significant at the p < 0.05 level.
Table 2. Unadjusted Readmission Rates and Odds Ratios for Readmission Stratified by Operation.
| Type of Lower Extremity Arterial Intervention | Unadjusted Readmission Rates %, [SD] | Odds Ratio for Readmission within 30-Days, Comparison of High-Risk to Claudication | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Adjusted for Patient Demographics Alone (CMS Model) | Adjusted for Patient Demographics, and Length-of-Stay | Adjusted for Patient Demographics, Length-of-Stay, and Discharge Destination | ||||||||||
|
|
|
|
|
|||||||||
| Claudicants | Unspecified | High-Risk | OR | 95% CI | OR | 95% CI | OR | 95% CI | ||||
| Any Revascularization | 7.3% | [26.0%] | 13.8% | [34.8%] | 19.5% | [39.6%] | 2.46 | [2.39 - 2.53] | 2.03 | [1.97 - 2.09] | 1.76 | [1.71 - 1.81] |
| Open Arterial Bypass | 9.1% | [28.7%] | 15.9% | [36.6%] | 20.3% | [40.2%] | 2.07 | [1.99 - 2.16] | 1.78 | [1.71 - 1.86] | 1.57 | [1.50 - 1.63] |
| Angioplasty +/- Stent | 6.3% | [24.2%] | 12.2% | [32.7%] | 18.7% | [39.0%] | 2.67 | [2.57 - 2.77] | 2.20 | [2.11 - 2.29] | 1.92 | [1.84 - 2.00] |
2.6.1 Odds of Readmission by Indication
After adjusting for age, gender, and comorbidities (CMS' model), patients with high-risk operative indications were significantly more likely to be readmitted compared to claudicants (Odds Ratio [OR] 2.46, 95% confidence interval [CI] 2.39-2.53). Even in the fully adjusted model (demographics, LOS, and discharge destination), high-risk patients still had a 1.76 greater odds of readmission compared to claudicants. This held true when operations were analyzed individually. Table II. Compared to CMS' model, addition of a variable for operative indication increased the proportion of variance explained for both open aterial bypass recipients (36.5% vs 23.0%) and for endovascular recipients (44.4% vs 65.2%).
2.6.2 Within Hospital Difference in Readmission Rates Between Claudicants and High-Risk Patients (delta-RSRR)
On average, readmission rates for high-risk patients were 12.2±2.1 percentage points higher than claudicants. When stratified by hospital quintile of performance under the HRRP, there was no statistically significant difference in the odds ratio for readmission comparing high-risk patients to claudicants (Best Hospitals, OR = 2.07 [95% CI 1.89-2.27]; Worst Hospitals, OR = 2.14 [95% CI 1.95-2.34]). Table III.
Table 3. Within Hospital Difference in Readmission Rates by Operative Indication Stratified by Procedure type and Readmission Quintile.
| Hospital Readmission Quintile Based on CMS Model | Open Arterial Bypass | Angioplasty +/- Stent | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Hospital Unadjusted Readmission Rates (%) | Odds Ratio for Readmission, High-Risk vs Claudication within the same hospital | Hospital Unadjusted Readmission Rates (%) | Odds Ratio for Readmission, High-Risk vs Claudication within the same hospital | |||||||
|
|
|
|
|
|||||||
| Claudicants | Unspecified | High-Risk | OR | 95% CI | Claudicants | Unspecified | High-Risk | OR | 95% CI | |
| Lowest (Best) | 6.8% | 12.2% | 15.5% | 2.07 | [1.89 - 2.27] | 5.1% | 9.2% | 14.3% | 2.39 | [2.19 - 2.61] |
| Low | 8.7% | 13.6% | 17.4% | 1.78 | [1.64 - 1.94] | 6.0% | 11.0% | 17.4% | 2.54 | [2.33 - 2.77] |
| Median | 9.2% | 15.5% | 20.0% | 1.99 | [1.82 - 2.17] | 6.6% | 12.2% | 18.3% | 2.44 | [2.25 - 2.64] |
| High | 10.1% | 17.7% | 21.6% | 1.96 | [1.80 - 2.13] | 7.0% | 13.5% | 21.0% | 2.74 | [2.50 - 3.00] |
| Highest (Worst) | 12.3% | 20.8% | 26.7% | 2.14 | [1.95 - 2.34] | 8.5% | 16.1% | 24.3% | 2.67 | [2.48 - 2.89] |
2.6.3 Case-Mix Adjustment and HRRP Penalties
Overall, 853 of the 1701 hospitals (50.1%) would receive lower penalties under a model that adjusts for case-mix based upon operative indication. Of the 823 hospitals projected to receive a penalty under HRRP's extension to LER, 73 hospitals would receive no penalty if CMS adjusted for case-mix. After adjusting for operative indication, hospitals treating the greatest proportion of high risk patient (top quintile) were significantly more likely to receive a penalty reduction compared to those treating the lowest proportion of high-risk patients (76.5% vs 28.7%, P <0.001).
Under CMS' model, hospitals in the top quintile of high-risk patients treated were dramatically more likely to receive readmission penalties compared to non-high risk treating hospitals (60% vs 35%, P <0.001). Figure 1. Under a case-mix adjusted model, there was no statistically significant difference in the receipt of penalties between high-risk treating and non-high risk treating hospitals (50.0% vs 46.0%, P = 0.30). Figure 1.
Figure 1.
Variation in Hospital Case-Mix and HRRP Penalties. Quintiles are based on the proportion of high-risk patients treated by each hospital with Quintile 5 treating the most high-risk patients and Quintile 1 treating the least high risk patients.
2.7 Discussion
This study evaluates the relationship between operative indication and 30-day readmissions following LER. Our primary findings were: (1) patients with ulceration, tissue loss or rest pain (high-risk) have a 3-fold increased risk of readmission compared to claudicants; (2) the Worst hospitals under then HRRP treat a significantly greater proportion of high-risk patients compared to other hospitals; (3) including operative indication based on ICD-9 codes in risk-modeling of 30-day readmissions would essentially eliminate the differences in receipt of penalties based high-risk case-mix.
Gaining a better understanding of readmissions in vascular surgery is particularly timely given the planned expansion of CMS' HRRP to vascular procedures. While numerous prior studies have sought to identify patient-level risk factors for readmission, there remains a sizable knowledge gap regarding the impact of various patient factors on hospital profiling. Our study builds on that existing literature by evaluating the impact of surgical case-mix on hospital profiling of readmissions under the HRRP. In this context, our findings have several important implications for policymakers.
2.7.1 Operative Indication is Predictive of Readmission
Despite the recent nationwide conversion to electronic medical records and dramatic improvements in natural language processing, many national quality improvement initiatives continue to rely on billing data to evaluate large numbers of hospitals.[11] The use of administrative data in public reporting programs has long been criticized for an inability to adequately adjust for important clinical risk factors such as TransAtlantic InterSociety Consensus (TASC) classification. While multiple clinical studies demonstrate TASC to be strongly predictive of important clinical outcomes (e.g. restenosis, reintervention, amputation) there does not currently exist a cost-effective method of coding this TASC classification for all patients treated in the nearly 2,000 American hospitals performing LER.[12] It is unlikely that such granular clinical data will be usable in the future because this would require either manual entry into a national database (eg the National Surgical Quality Improvement Program), or creation of billing codes that parallel clinical severity markers. Current registries, such as the SVS VQI, have been trying to combine the strength of a manually abstracted database with the long-term outcomes available in Medicare, but these efforts have not yet come to fruition.
Our study identifies operative indication, based on icd-9 codes, as a robust predictor of a patient's risk of readmission independent of other common risk factors (age, comorbidities, and LOS). More importantly, from a policy standpoint, we demonstrate that adjusting for operative indication would in fact change penalties to hospitals under the HRRP.
2.7.2 Disparity Between High-Risk Patients and Claudicants - Implications for Policymakers
At the extremes, there are two commonly employed policy strategies used to improve outcomes among high-risk subsets of patients. The first is to guide these patients to centers that are better able to handle complex care (i.e. selective referral).[13] This option works best when there are disproportionately bad outcomes in high-risk patients. For instance, patients severe trauma are better cared for level 1 trauma centers compared to local community hospitals. This is the rationale for the policy of temporarily stabilizing these patients at community centers and then rapidly transferring them to regional level 1 trauma facilities. Selective referral is attractive because, while potentially challenging to implement, it is a simple policy solution to enact by governmental fiat.
The second commonly employed strategy for improving outcomes is to attempt to raise the bar of performance across the board by disseminating best-practices of high performers to poor performs. This approach poses several challenges. At the outset, it requires the identification and implementation of specific behaviors leading to better outcomes. This step often requires conducting large, multi-institutional trials which may have opposing conclusions depending upon practice setting. More recently, regional collaboratives have been used to help identify high performing and low-performing hospitals. Best practices are generated from these evaluations of hospitals at a regional level and regional efforts are then employed to improve care (Cite MSQC and VSGNE- protamine and CEA).
We found that the Best and Worse HRRP hospitals have similar disparities in readmission rates between high-risk and claudicant patients. This implies that poor performing hospitals have a global performance problem not a problem with disproportionately worse outcomes in complex patients. Thus, a policy of selective referrals based on the publically available CMS readmission rates will not necessarily solve the problem of high readmission rates in high-risk patients. Rather, a comprehensive national strategy should attempt to raise the bar of performance for all hospitals. This might be achieved through either disease specific national or regional collaboratives and benchmarking. Alternatively, CMS could also incentivize innovation on a hospital-by-hospital basis to address the specific challenges at a tactical level that lead to high readmission rates.
2.7.3 Perverse Incentives to Avoid of High-Risk Patients
Our findings support the notion that the Best HRRP hospitals have lower readmission rates because they are treating fewer high-risk patients. Our simulation found that this difference in hospital case-mix has ramifications for HRRP penalties. In the absence of including a variable for operative indication, hospitals treating the greatest proportion of high-risk patients were significantly more likely to receive a HRRP penalty. After adjusting for indication, these differences based on case-mix were eliminated. In fact, more than 75% of high-risk serving hospitals would receive lower penalties after adjusting for operative indication.
Policies that do not adequately adjust for case-mix run the risk of creating perverse incentives for hospitals to avoid high-risk patients. Perhaps the best known example occurred in New York State after the initiation of a public reporting program for coronary artery bypass grafting (CABG). Following the 1989 release of hospital and surgeon specific mortality report cards, there is evidence demonstrating selective referrals of high-risk patients patients out of state. One study by Omoigui et al, examined compared characteristics of patients referred to the Cleveland Clinic for CABG from New York versus other states.[14] Prior to 1989, patients from New York had similar demographic characteristics compared to both patients from Ohio and other states. After dissemination of CABG report cards, compared to patients from other states, referrals New York had a much higher rate of risk factors for poor outcomes such as prior open heart surgery (21.5% vs 37.4%, P = .008) and New York Heart Association functional class III or IV (41.2% vs 47.6% P = .011). This resulted in significantly higher observed mortality in New York referrals compared to other referrals (5.2% vs 3.1%, P = .028).[14] However, this avoidance behavior becomes even more vexing in the context of a national initiatives such as the HRRP because the is no option for transferring patients to out-of-state hospitals not covered by the program. Rather the choice becomes operating (and accepting a penalty) or not operating on high-risk patients.
2.7.4 Limitations
This study is not without limitations. First, as with any evaluation relying on administrative data based upon billing codes and this lacks a significant amount of clinical data. In our case, there were a large number of people who underwent LER who either had codes indicating they had peripheral vascular disease “not otherwise specified” or but did not have codes indicating peripheral vascular disease. While some of these patients may certainly have undergone a revascularization procedure for other reasons such as trauma, it is also likely that many more had PVD that was not included due to suboptimal billing codes. However, this is the same data that CMS will use in evaluating vascular surgery for penalties. An analysis using a registry, although likely more robust, would not answer the same questions or have the same policy implications. Additionally, our finding that high-risk patients were approximately twice as likely as claudicants to be readmitted is similar to studies using clinical data.[5,6]
Secondly, while our study can inform readers as to whether or not a hospital would receive a penalty and whether the penalty would be more or less after adjusting for operative indication, it is difficult to provide estimates for actual dollar amounts of penalties. Each hospital's penalties under HRRP are assessed for a bundle of conditions – congestive heart failure, pneumonia, acute myocardial infarction, chronic obstructive pulmonary disease, and hip and knee replacements.[7]
“Finally, it is difficult to determine the extent to which the recent change to ICD-10 will exaggerate or attenuate our findings. Further multi-institutional studies linking clinical data to ICD-10 administrative data will be required to evaluate whether the updated coding library provides more accurate assessments of illness severity versus more opportunities to game the system.”
2.8 Conclusion
This study is the first to evaluate the impact of operative indication on hospital profiling under a national policy penalizing post-operative readmissions. We found that patients with rest pain, tissue loss, and ulcers, have dramatically higher readmission rates even after adjusting for patient demographics, comorbidities, and post-operative complications. We also found that extension of the HRRP to lower extremity revascularizations would largely penalized hospitals with the greatest burden of care for high-risk patients despite the fact they are not disproportionately worse at taking care of those patients.
Acknowledgments
Funding: This study was supported by grants R01 AG039434-03 (Dr. Osborne) from the National Institute on Aging; K08 HS017765-04 (Dr. Osborne) from the Agency for Healthcare Research and Quality; and Ruth L. Kirschstein National Research Service Awards T32 HL076123-09 from the National Heart Lung and Blood Institute (Dr. Gonzalez).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Medicare & Medicaid Services. Readmissions Reduction Program [Internet] 2012 Available from: http://go.cms.gov/1eUTfaO.
- 2.Suter LG, Grady JN, Lin Z, Parzynski CS, Potteiger J, Keenan M, et al. 2013 Measure Updates and Specifications : Elective Primary Total Hip Arthroplasty (THA) And / Or Total Knee Arthroplasty (TKA) All-Cause Unplanned 30-Day Risk-Standardized Readmission Measure [Internet] New Haven. 2013 Available from: http://bit.ly/Pnuj2o.
- 3.Medicare Payment Advisory Commission (MedPAC) Report to Congress: Promoting Greater Efficiency in Medicare [Internet] 2007;Chapter 5 Available from: http://1.usa.gov/1lp2gJ9. [Google Scholar]
- 4.Bosco JLF, Silliman Ra, Thwin SS, Geiger AM, Buist DSM, Prout MN, et al. J Clin Epidemiol [Internet] 1. Vol. 63. Elsevier Inc; 2010. A most stubborn bias: no adjustment method fully resolves confounding by indication in observational studies; pp. 64–74. Available from: http://dx.doi.org/10.1016/j.jclinepi.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McPhee JT, Barshes NR, Ho KJ, Madenci A, Ozaki CK, Nguyen LL, et al. Predictive factors of 30-day unplanned readmission after lower extremity bypass. J Vasc Surg. 2013 Apr;57(4):955–62. doi: 10.1016/j.jvs.2012.09.077. [DOI] [PubMed] [Google Scholar]
- 6.McPhee JT, Nguyen LL, Ho KJ, Ozaki CK, Conte MS, Belkin M. Risk prediction of 30-day readmission after infrainguinal bypass for critical limb ischemia. J Vasc Surg Society for Vascular Surgery. 2013 Jun;57(6):1481–8. doi: 10.1016/j.jvs.2012.11.074. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Medicare & Medicaid Services. Frequently Asked Questions: CMS Publicly Reported Risk-Standardized Outcome Measures [Internet] 2013 Available from: http://bit.ly/1hrSC9s.
- 8.Gonzalez AA, Girotti ME, Shih T, Wakefield TW, Dimick JB. Reliability of hospital readmission rates in vascular surgery. J Vasc Surg. 2014;59(6):1638–43. doi: 10.1016/j.jvs.2013.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Osborne NH, Ko CY, Upchurch GR, Dimick JB. The impact of adjusting for reliability on hospital quality rankings in vascular surgery. J Vasc Surg. 2011;53(1):1–5. doi: 10.1016/j.jvs.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 10.Kuhan G, Marshall EC, Abidia AF, Chetter IC, McCollum PT. A Bayesian Hierarchical Approach to Comparative Audit for Carotid Surgery. Eur J Vasc Endovasc Surg. 2002 Dec;24(6):505–10. doi: 10.1053/ejvs.2002.1763. [DOI] [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services. Fact Sheet- Hospital Value-Based Purchasing Program [Internet] Available from: http://www.cms.gov/Hospital-Value-Based-Purchasing.
- 12.Giles Ka, Pomposelli FB, Hamdan AD, Blattman SB, Panossian H, Schermerhorn ML. Infrapopliteal angioplasty for critical limb ischemia: Relation of TransAtlantic InterSociety Consensus class to outcome in 176 limbs. J Vasc Surg. 2008;48(1):128–36. doi: 10.1016/j.jvs.2008.02.027. [DOI] [PubMed] [Google Scholar]
- 13.Birkmeyer JD, Dudley RA, Phibbs C. Evidence-based Hospital Referral Fact Sheet [Internet] The Leapfrog Group Website. 2008:1–3. Available from: http://bit.ly/14yWb5u.
- 14.Omoigui NA, Miller DP, Brown KJ, Annan K, Cosgrove D, 3rd, Lytle B, Loop F, Topol EJ. Outmigration for coronary bypass surgery in an era of public dissemination of clinical outcomes. Circulation. 1996;93(1):27–33. doi: 10.1161/01.cir.93.1.27. [DOI] [PubMed] [Google Scholar]