The recent outbreak of Marburg virus disease in Kween District, eastern Uganda, reported in The Lancet Infectious Diseases,1 marks the 13th independent viral haemorrhagic fever outbreak identified and confirmed via laboratory test by the Uganda Virus Research Institute (UVRI)’s viral haemorrhagic fever surveillance and laboratory programme since 2010. This Marburg virus disease outbreak was followed closely by three independent confirmations of human Rift Valley fever virus infection in three districts in central Uganda, and now brings the total viral haemorrhagic fever outbreak detections to 16. This exceptional number of early detections and subsequent outbreak responses has led to a significant decrease in the overall intensity (p=0·001) and duration (p<0·0001) of viral haemorrhagic fever outbreaks in Uganda, and serves as a role model for detecting and responding to public health threats of international concern.
Uganda’s national viral haemorrhagic fever surveillance and laboratory programme was initiated in 2010 as a collaboration between UVRI, the Uganda Ministry of Health, and the US Centers for Disease Control (CDC)’s Viral Special Pathogens Branch. It was a first-of-its-kind national viral haemorrhagic fever sentinel surveillance system established to enhance Uganda’s IDSR surveillance to rapidly detect, diagnose, report, and respond to viral haemorrhagic fevers, as well as other emerging zoonotic infectious diseases. The programme also sought to expand and enhance laboratory diagnostic testing for viral haemorrhagic fevers in Uganda, improve incident case detection through better clinical recognition, and use the data generated to better inform decision making and disease control efforts at the national level.
This comprehensive programme was implemented through the creation of a series of sentinel surveillance sites directly linked to UVRI and the Ministry of Health. Training of regional hospital and district health office staff included epidemiological data collection, viral haemorrhagic fever surveillance, epidemiology and ecology, suspect patient identification, and infection control procedures. Key elements of the programme were development of a standardised three-tiered case definition and case reporting form specific for viral haemorrhagic fevers. Each site can now report a suspected case and safely collect and ship samples to be tested at UVRI and reported to the Ministry of Health. The programme initially had six directly supported sentinel surveillance sites, which has now grown to over 20 sites and counting.
UVRI serves as the national viral haemorrhagic fever reference laboratory and has the capacity to do confirmatory real-time testing for all major regional viral haemorrhagic fevers of public health concern. These include Ebola virus disease, Marburg virus disease, Rift Valley fever, and Crimean-Congo haemorrhagic fever. The diagnostic tests done are antigen-detection ELISA, IgM and IgG ELISA, and real-time RT-PCR. Suspected diagnostic specimens are tested in a state of the art, biosafety level 3, high-containment laboratory suite. All viral haemorrhagic fever laboratory confirmatory testing is done at UVRI and results are available within 24–48 h after sample reception. Since 2010, the viral haemorrhagic fever laboratory has tested over 11 000 clinical samples from serosurveys, surveillance programmes, and outbreaks. Suspected samples are submitted for testing from throughout Uganda and regionally from east Africa and central Africa. To date, this has led to confirmation of 16 independent viral haemorrhagic fever outbreaks, and includes three outbreaks of Ebola virus disease in 20112 and 2012, three outbreaks of Marburg virus disease in 2012,3 2014,4 and 2017, six outbreaks of Crimean-Congo haemorrhagic fever in 2013, 2015, and 2017, and four independent outbreaks of Rift Valley fever in 20165 and 2017. No human cases of Rift Valley fever have been detected between 1968 and the 2016 outbreak. The regional capacity for viral haemorrhagic fever testing also led to one outbreak confirmation of Ebola Bundibugyo in Isiro, Democratic Republic of the Congo, in 2012.
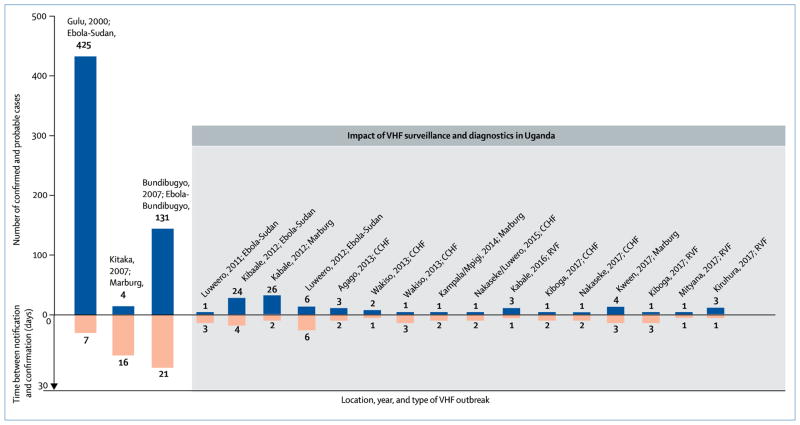
Uganda’s viral haemorrhagic fever surveillance system has contributed to a substantial improvement in time to response for viral haemorrhagic fever outbreaks. Earlier case detection and laboratory confirmation has led to faster public health responses, case patients being isolated with the use of infection control precautions,2–4 decreased secondary transmission in the communities (p=0·01),2–4,6,7 and ultimately shorter (p<0·0001) and less severe outbreaks (p=0·001; figure). Two large outbreaks, of Ebola Sudan (in 20007) and Ebola Bundibugyo (in 20076), occurred during an era of limited surveillance and outbreak detection capacity. Following implementation of enhanced surveillance (figure) the number of outbreak detections has increased five times from the previous 10 years. The size and scope of each outbreak has also been substantially reduced, with the time between initial clinical notification and laboratory confirmation being shortened from 2 weeks before 2010 to an average of just 2·5 days now (p<0·0001).
Figure. Impact of enhanced viral haemorrhagic fever surveillance in Uganda on outbreak detections and their magnitude and scope relative to the reduction in time from notification to laboratory confirmation.
VHF=viral haemorrhagic fever. CCHF=Crimean-Congo haemorrhagic fever. RVF=Rift Valley fever.
In addition to the success of the viral haemorrhagic fever programme in Uganda, direct technical assistance and support for response to viral haemorrhagic fever outbreaks throughout Africa has been provided, including for the west Africa Ebola outbreak in 2014–16.8 Materials developed for the Uganda viral haemorrhagic fever programme, including standardised case reporting forms, case definitions, health education and risk communication materials, and the Epi-Info viral haemorrhagic fever application,9 were used in 2014 to the three west African countries affected by Ebola virus disease to aid in outbreak management and control since the region had no previous experience with filovirus outbreaks. The programme continues to serve as an Africa-wide resource providing technical assistance, expert training, and capacity building for Ministries of Health, UN agencies, and international public health organisations as well as serving as a pioneer and role model for the Global Health Security Agenda.10
The UVRI viral haemorrhagic fever programme highlights the importance of continued support and investment for dedicated public health surveillance and response programmes for emerging zoonotic diseases and how these can significantly reduce morbidity (p=0·001) and mortality (p=0·01) from continued viral haemorrhagic fever outbreaks.
Footnotes
The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention. We declare no competing interests.
References
- 1.Zwizwai R. Infectious disease surveillance update. Lancet Infect Dis. 17:1244. doi: 10.1016/S1473-3099(16)00023-2. [DOI] [PubMed] [Google Scholar]
- 2.Shoemaker T, MacNeil A, Balinandi S, et al. Reemerging Sudan Ebola virus disease in Uganda, 2011. Emerg Infect Dis. 2012;18:1480–83. doi: 10.3201/eid1809.111536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knust B, Schafer IJ, Wamala J, et al. Multidistrict outbreak of Marburg virus disease-Uganda, 2012. J Infect Dis. 2015;212(suppl 2):S119–28. doi: 10.1093/infdis/jiv351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nyakarahuka L, Ojwang J, Tumusiime A, et al. Isolated case of Marburg virus disease, Kampala, Uganda, 2014. Emerg Infect Dis. 2017;23:1001–04. doi: 10.3201/eid2306.170047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de St Maurice A, Nyakarahuka L, Purpura L, et al. Notes from the field: Rift valley fever response—Kabale District, Uganda, March 2016. MMWR Morb Mortal Wkly Rep. 2016;65:1200–01. doi: 10.15585/mmwr.mm6543a5. [DOI] [PubMed] [Google Scholar]
- 6.Wamala JF, Lukwago L, Malimbo M, et al. Ebola hemorrhagic fever associated with novel virus strain, Uganda, 2007–2008. Emerg Infect Dis. 2010;16:1087–92. doi: 10.3201/eid1607.091525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Okware SI, Omaswa FG, Zaramba S, et al. An outbreak of Ebola in Uganda. Trop Med Int Health. 2002;7:1068–75. doi: 10.1046/j.1365-3156.2002.00944.x. [DOI] [PubMed] [Google Scholar]
- 8.Bagcchi S. Ebola haemorrhagic fever in west Africa. Lancet Infect Dis. 2014;14:375. doi: 10.1016/s1473-3099(14)70034-9. [DOI] [PubMed] [Google Scholar]
- 9.Schafer IJ, Knudsen E, McNamara LA, Agnihotri S, Rollin PE, Islam A. The Epi Info Viral hemorrhagic fever (VHF) application: a resource for outbreak data management and contact tracing in the 2014–2016 West Africa Ebola epidemic. J Infect Dis. 2016;214(suppl 3):S122–36. doi: 10.1093/infdis/jiw272. [DOI] [PubMed] [Google Scholar]
- 10.Borchert JN, Tappero JW, Downing R, et al. Rapidly building global health security capacity—Uganda demonstration project, 2013. MMWR Morb Mortal Wkly Rep. 2014;63:73–76. [PMC free article] [PubMed] [Google Scholar]