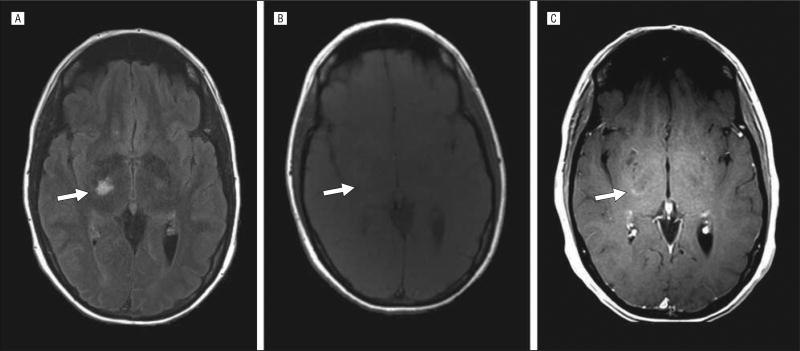
A previously healthy 40-year-old woman presented with subacute onset of a left homonymous hemianopia. Contrast-enhanced magnetic resonance imaging of the brain revealed a T2-hyperintense lesion in the right thalamus, with associated subtle gadolinium enhancement (Figure 1), and a small periventricular lesion. Although her visual symptoms were improving, a new left-sided hemiparesis developed 3 weeks later. Additional magnetic resonance imaging of the brain showed extension of the original thalamic lesion into the right internal capsule, with persistent contrast enhancement. Her visual and motor symptoms gradually improved over 3 months.
Figure 1.
A, Axial fluid-attenuated inversion recovery sequence on magnetic resonance imaging showing a hyperintense lesion (arrow) in the right lateral thalamus. The T1-weighted sequence before (B) and after (C) the administration of gadolinium contrast medium shows corresponding subtle contrast enhancement within the lesion (arrows).
The differential diagnosis included multiple sclerosis, malignancy, and stroke. The patient underwent an extensive examination, including magnetic resonance angiography, echocardiography, and a hypercoagulable and autoimmune workup. All of the results were unremarkable, with the exception that the patient had positive cerebrospinal fluid–specific oligoclonal bands and an elevated cerebrospinal fluid IgG index. Six months after presentation, she developed tingling in the fingertips bilaterally and visual blurring with vertical gaze. Additional magnetic resonance imaging of the brain revealed a new enhancing lesion in the juxtacortical white matter of the right frontal lobe, and magnetic resonance imaging of the cervical spine showed 3 small non-enhancing lesions, suggesting the diagnosis of relapsing-remitting multiple sclerosis. Glatiramer acetate therapy was initiated, and the patient remains clinically and radiologically stable 9 months later.
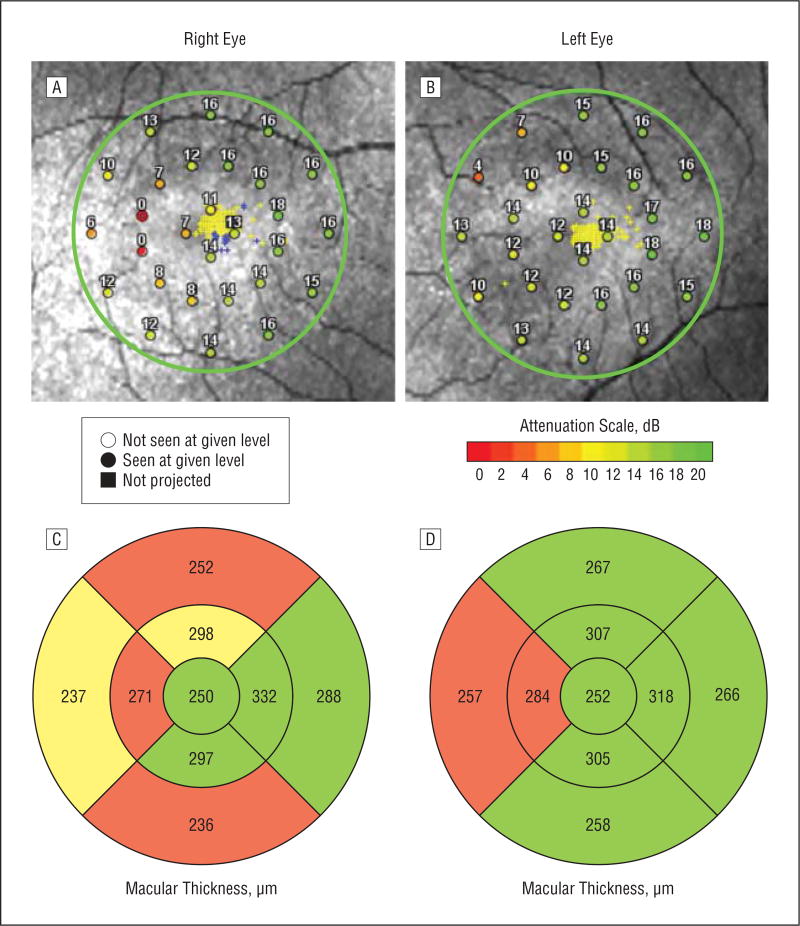
Serial spectral-domain optical coherence tomography showed progressive macular thinning in the temporal hemimacula of the right eye and nasal hemimacula of the left eye, corresponding precisely with the patient’s presenting clinical deficit of a left homonymous hemianopia (Figure 2). Retinal segmentation demonstrated that this thinning was confined to the ganglion cell and inner plexiform layer composite (these 2 layers cannot be visually discriminated on optical coherence tomographic scans), with sparing of the deeper nuclear layers. The combination of clinical and radiological findings suggest that the observed pattern of macular thinning on optical coherence tomographic scans most likely reflects retrograde transsynaptic degeneration due to lateral geniculate nucleus involvement from her documented thalamic lesion, rather than a primary retinal process.
Figure 2.
A and B, Scanning laser ophthalmoscope microperimetry map (OPKO Health Inc) demonstrating a homonymous hemianopic visual field deficit. The color-coded visual attenuation scale provides the mean retinal sensitivity to a standardized visual stimulus (range, 0–20 dB; with 0 representing the absence of retinal sensitivity and 20 representing maximum retinal sensitivity). C and D, Cirrus high-definition–optical coherence tomographic macular thickness maps (in units of micrometers) demonstrate hemimacular thinning, which corresponds to the demonstrated visual field deficit (green = 5%–95%, yellow = 1%–5%, and red = less than 1% for age-matched controls).
COMMENT
Homonymous visual field deficits are an atypical manifestation of multiple sclerosis and have rarely been reported as a presenting feature.1 Optical coherence tomography is a non-invasive imaging technique that uses near-infrared light to produce cross-sectional or 3-dimensional images of the retina.2 Optical coherence tomography has the ability to objectively quantify measurements of the peripapillary retinal nerve fiber layer and retinal macular thickness, and it is emerging as a useful clinical tool in multiple sclerosis.3 For our patient, optical coherence tomographic measurements enabled the confirmation of retrograde transsynaptic homonymous hemimacular degeneration of the retinal ganglion cells, which was attributable to a lesion affecting the right lateral geniculate nucleus, with appropriately corresponding visual symptomatology and perimetry deficits.
Acknowledgments
Conflict of Interest Disclosures: Dr Saidha has received consulting fees from MedicalLogix for the development of continuing medical education programs in neurology and educational grant support from Teva Neuroscience. Dr Calabresi has provided consultation services to Novartis, EMD-Serono, Teva, Biogen-Idec, Vertex, Vaccinex, Genzyme, Genentech.
Funding/Support: This work was supported by the National Multiple Sclerosis Society (grant TR 3760-A-3 to Dr Calabresi); the Braxton Debbie Angela Dillon and Skip Donor Advisor Fund (to Dr Calabresi); and the Multiple Sclerosis Society of Canada Postdoctoral Fellowship Award (to Dr Oh).
Role of the Sponsors: The study sponsors did not participate in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr Oh had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Oh and Calabresi. Acquisition of data: Oh, Sotirchos, Sepah, and Nguyen. Analysis and interpretation of data: Oh, Sotirchos, Saidha, Ibrahim, Sepah, Nguyen, and Calabresi. Drafting of the manuscript: Oh and Sotirchos. Critical revision of the manuscript for important intellectual content: Oh, Saidha, Sotirchos, Ibrahim, Sepah, Nguyen, and Calabresi. Obtained funding: Calabresi. Administrative, technical, and material support: Ibrahim. Study supervision: Calabresi.
References
- 1.Gündüz K, Cansu K, Bulduklar S, Saatçi I. Homonymous hemianopsia as the initial manifestation of multiple sclerosis. Ophthalmologica. 1998;212(3):215–220. doi: 10.1159/000027283. [DOI] [PubMed] [Google Scholar]
- 2.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254(5035):1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frohman EM, Fujimoto JG, Frohman TC, Calabresi PA, Cutter G, Balcer LJ. Optical coherence tomography. Nat Clin Pract Neurol. 2008;4(12):664–675. doi: 10.1038/ncpneuro0950. [DOI] [PMC free article] [PubMed] [Google Scholar]