Abstract
Background
Despite an expansive body of research on health and access to medical care among Mexican immigrants in the United States, research on return migrants focuses primarily on their labor market mobility and contributions to local development.
Objective
Motivated by recent scholarship that documents poor mental and physical health among Mexican return migrants, this study investigates return migrants' health insurance coverage and access to medical care.
Methods
I use descriptive and multivariate techniques to analyze data from the 2009 and 2014 rounds of Mexico's National Survey of Demographic Dynamics (ENADID, combined n=632,678).
Results
Analyses reveal a large and persistent gap between recent return migrants and non-migrants, despite rising overall health coverage in Mexico. Multivariate analyses suggest that unemployment among recent arrivals contributes to their lack of insurance. Relative to non-migrants, recently returned migrants rely disproportionately on private clinics, pharmacies, self-medication, or have no regular source of care. Mediation analysis suggests that returnees' high rate of uninsurance contributes to their inadequate access to care.
Conclusion
This study reveals limited access to medical care among the growing population of Mexican return migrants, highlighting the need for targeted policies to facilitate successful reintegration and ensure access to vital resources such as health care.
Keywords: Immigration/migration, return migrant, migration and health, Mexico, health, health insurance, access to care
1. Introduction
Mexican migrants constitute a vulnerable population. Separated from family and community, and often working in dangerous occupations and targeted by discrimination, immigrants face significant mental and physical health risks. Not surprisingly, scholars have devoted vast resources to documenting and understanding the health needs of Mexicans in the United States (Ana P Martinez-Donate, 2014; Diaz, Koning, & Martinez-Donate, 2016; Goldman et al., 2014; Torres & Waldinger, 2015; Wallace, Mendez-Luck, & Castañeda, 2009). Studies show that Mexican immigrants' mental and physical health decline with time spent abroad (Creighton, Goldman, Pebley, & Chung, 2012; Goldman et al., 2014; Potochnick & Perreira, 2010). Moreover, Mexican immigrants encounter substantial barriers to medical care in the United States (Torres & Waldinger, 2015). And yet, migration is not a one-way street.
Every year, hundreds thousands of Mexicans voluntarily return home to reunite with families or invest accumulated savings in new businesses (MATT, 2013; Ruiz-Tagle & Wong, 2009; Van Hook & Zhang, 2011). Many others are forcibly detained and repatriated for immigration violations (Amuedo-Dorantes, Puttitanum, & Martinez-Donate, 2013; Hagan, Rodriguez, & Castro, 2011). In recent years, driven by economic decline and rising interior enforcement, return migration to Mexico has grown dramatically. About 2.5 million Mexicans returned between 2005 and 2015, double the rate from a decade earlier (Gonzalez-Barrera, 2015; Passell, Cohn, & Gonzalez-Barrera, 2012). In response to heightened border patrol, recent return migrants are increasingly likely to settle permanently in Mexico, rather than return to the United States (Martinez, Aguayo-Tellez, & Rangel-Gonzalez, 2014; Schulthies & Ruiz Soto, 2017).
Several recent studies find that Mexican migrants return home in worse mental and physical health than when they first migrated (Familiar, Borges, Orozco, & Medina-Mora, 2011; Ullmann, Goldman, & Massey, 2011). Moreover, results from the Mexican Family Life Survey and other binational research on Mexican migrants indicate that return migrants are negatively selected on physical and self-rated health relative to those who remain in the United States (Arenas, Goldman, Pebley, & Teruel, 2015; Diaz et al., 2016), indicating a substantial level of health need among those returning home.
Despite the growing evidence of the health challenges that confront Mexican return migrants, very little is known about their access to health care upon return. International migrants, especially those without proper authorization, exist in a liminal space, often excluded from formal institutions such as health insurance while in the United States (López-Sanders, 2017; Torres & Waldinger, 2015; Vargas Bustamante et al., 2012). Indeed, barriers to receiving care in the United States are such that many Mexicans living near the border return home to obtain medical care (Su, Richardson, Wen, & Pagán, 2011; Wallace et al., 2009). The emergence of cross-border care utilization, combined with the growing population of voluntary and involuntary return migrants now settling in Mexico highlights the need for a clearer understanding of return migrants' access to health care in Mexico.
Several studies conducted using the first two waves of the Mexican Health and Aging Survey (MHAS) documented a modest gap in coverage between older Mexican return migrants and non-migrants, between 5% and 10% in 2001(Aguila & Zissimopoulos, 2013; Polsky, Pagan, & Ross, 2006). Yet, a more recent paper published in the American Journal of Public Health found that 54% of migrants returned in the last five years were uninsured compared to just 35% of non-migrants according to the 2010 Mexican Census, (Wassink, 2016). Using data from a recent survey conducted in Tijuana, Mexico, Martinez-Donate (2017) found that Mexican migrants had significantly lower health coverage and access to care upon return, relative to their pre-migration levels, indicating that migration may be associated with a lapse in coverage. These findings suggest the need for further research on the causes of uninsurance among Mexican return migrants. In particular, while scholars have highlighted low coverage among recently returned migrants (Martinez-Donate et al., 2017; Wassink, 2016), they have not yet considered whether migrants' health coverage rises with time since return. Further investigation is also needed to assess the impact of uninsurance on Mexican return migrants' access to medical care.
This study uses data from two waves of Mexico's National Survey of Demographic Dynamics (ENADID) to evaluate health insurance coverage and access to a regular source of care among Mexican return migrants and non-migrants. To identify the importance of time since return to migrants' access to health care, I distinguish between those returned within one-year of the survey and those returned within five-years of the survey. My analysis is guided by major changes in Mexico's insurance system, specifically the implementation of a universal health care program, Seguro Popular, in 2003 (Knaul et al., 2012; Knaul & Frenk, 2005), and theories of international migration and the context of return (Massey & Espinosa, 1997; Villarreal & Blanchard, 2013; Wheatley, 2011).
2. Background
2.1 Institutional context: health insurance in Mexico
Since 1943, Mexico's social security program, Instituto Mexicano de Seguro Social (IMSS) and similar state run insurance programs have covered workers in formally registered Mexican businesses. Similar programs exist to insure state and federal government employees (Institute of Social Services for State Employees, ISSSTE) employees in Mexico's state-owned oil and gas company (Petroleos Mexicanos, PEMEX), and members of the armed services (Secretariat of National Defense, SEDENA). These insurance programs function similarly to U.S. Social Security. Employees are automatically enrolled by their employers in concert with the particular insurance program through which they are affiliated. However, as is the case throughout much of Latin America (Tornarolli, Battistón, Gasparini, & Gluzmann, 2014), the majority of Mexican laborers work in the informal sector of the economy, which includes small firms with between 1-5 employees that are not formally registered, regulated, or taxed by the government. Firms in the informal economy rarely provide health coverage, pensions, severance pay, or written contracts (Arias, Azuara, Bernal, Heckman, & Villarreal, 2010; Levy, 2008; Perry et al., 2007). Therefore, the majority of the Mexican population has historically relied on private clinics, pharmacies, and self-medication to obtain medical treatment (Knaul & Frenk, 2005).
In 2003, the Mexican government created Seguro Popular (the People's Insurance) because, according to then Secretary of Health, Julio Frenk, “more than half of Mexican households lack [ed] health insurance” (Knaul & Frenk, 2005). Seguro Popular has made health insurance coverage available to Mexico's family workers, agricultural laborers, small business owners, independent artisans or traders, and laborers in unregistered Mexican firms who lack access to employment-based coverage. These individuals and their dependents can voluntarily affiliate with Seguro Popular. Those who participate make financial contributions that are matched by the state and federal government, which take the place of a formally registered employer. Extensive research has documented significant improvements in health coverage under Seguro Popular. Some estimates suggest that as of 2012, Seguro Popular had enrolled upwards of fifty-million individuals, with disproportionate affiliation among poor and rural Mexicans (Knaul et al., 2012), who continue to be overrepresented among those migrating to the United States (Massey & Espinosa, 1997; Rendall & Parker, 2014).
2.2 Migration and health insurance coverage
In this study, I consider two factors that may contribute to migrants' low levels of health insurance coverage. First, migration could reduce health coverage due to absence during key enrollment periods or a lapse in coverage due to migration. Seguro Popular was rolled out in stages with communities systematically targeted for enrollment (King et al., 2009; Knaul et al., 2012). When individuals migrate, they run the risk of severing social and institutional ties in their home communities, which may include loss of insurance coverage. For those migrants who have most recently returned, health insurance is likely one of many items requiring attention. Thus, to the extent that absence during enrollment or migration following enrollment contributes to uninsurance, one might expect migrants' coverage to increase with time following return, as former migrants gain information and check off higher priority agenda items such as securing employment. Some returnees may expect to gain coverage through IMSS following a successful formal sector job search. Others may delay enrolling in Seguro Popular until they successfully re-enter the informal labor market or get a new business venture off the ground (Hagan & Wassink, 2016; Lindstrom, 2013). Prior studies of health coverage among return migrants have not categorized migrants by duration of residence since return (Aguila & Zissimopoulos, 2013; Polsky et al., 2006; Wassink, 2016). In-doing-so, they emphasize the disparity between non-migrants and return migrants, but obscure variations among return migrants at different stages of the reintegration process. I overcome this limitation by separating those migrants back between 1-12 months and those back between 1-5 years.
Second, migrants' uninsurance may also stem from disproportionate employment in the informal sector. Informal sector employment in Mexico is associated with an increased risk of U.S. migration (Villarreal & Blanchard, 2013). In particular, Villarreal (2013) argues that the lack of benefits and employment protections associated with informal sector employment reduce migrants' incentives to remain in Mexico. Research on return migrants reveals a persistently high rate of informal sector employment upon return, with returnees significantly more likely than non-migrants to work in or operate small, unregistered businesses (Sheehan & Riosmena, 2013). If labor market status is the primary driver of uninsurance among return migrants, one would expect adjustment for regular employment to reduce the negative association between migration experience and health insurance coverage. One might also expect the level of health insurance coverage among return migrants to increase over time, as Seguro Popular continues to incorporate previously uninsured informal sector workers, both migrants and non-migrants alike. However, such improvement would not necessarily attenuate the disparity between recently returned and non-migrants.
Employment status may also affect health insurance coverage by diverting return migrants' energies into ongoing job searches. For most return migrants, securing employment represents an immediate and pressing concern (Cassarino, 2004; Lindstrom, 2013; Wassink & Hagan, Forthcoming). Whereas among non-migrants labor market inactivity is most commonly associated with school enrollment or homemaker-status among return migrants it likely represents an on-going job search (Lindstrom, 2013). Return migrants planning a return trip to the United States, who have limited incentive to enroll in health insurance, may also opt not to re-enter the labor market. In either case, labor market inactivity would likely be associated with a greater risk of uninsurance among return migrants than non-migrants. To distinguish between the two sources of uninsurance, one could compare the most recently returned migrants against those back in Mexico for a longer period. As time since return increases, the odds of a return trip decline and returnees' ability to voluntarily forgo employment will decline. Thus, if inactivity is more strongly associated with uninsurance among the most recently returned migrants it would lend support to a planned return trip as the causal factor. But, as time since return increases, inactivity more likely reveals the consequences of a failed economic reintegration and associated marginalization among returnees.
2.3 Uninsurance and access to care among Mexican return migrants
An important aspect of Mexico's health care system is that each insurance program corresponds to its own affiliated clinics. Formal employees covered through IMSS can receive care at IMSS hospitals, state and federal workers visit ISSSTE clinics, Seguro Popular enrollees visit Seguro Popular facilities, and the uninsured can visit private clinics, pharmacies, self-medicate, or go without care. High levels of uninsurance among return migrants likely result in a disproportionate reliance on private clinics, pharmacies, and self-medication within an already vulnerable population. Moreover, reliance on private clinics and pharmacies would place return migrants at increased risk of incurring catastrophic medical expenses and going without medical care, especially preventative treatment (Galárraga, Sosa-Rubí, Salinas-Rodríguez, & Sesma-Vázquez, 2010; King et al., 2009). Recent cross-border research shows that Mexican immigrants in the United States who return home expressly to seek medical care are heavily dependent on private clinics, rather than those affiliated with IMSS, ISSSTE, or Seguro Popular (González-Block, Bustamante, Sierra, & Cardoso, 2014; González-Block & Sierra-de la Vega, 2011). Research using Mexico's National Survey of Migration on the Northern Frontier shows that deported migrants have especially low access to care, which is exacerbated by poor self-rated health (Fernández-Niño, Ramírez-Valdés, Cerecero-Garcia, & Bojorquez-Chapela, 2014). Yet, no nationally representative studies have investigated access to a regular source of care among Mexican return migrants.
2.4 Hypotheses
My analysis is guided by three sets of hypotheses. 1) The gap in health coverage between return migrants and non-migrants will decline from 2009 to 2014 as overall knowledge of and affiliation with Seguro Popular expands (H1a). Health insurance coverage will be higher among migrants with a longer duration of residence since return as they gradually reintegrate into Mexican society (H1b). 2) Labor market status will partially explain the disparity in health insurance coverage between return migrants and non-migrants (H2a). Labor market status will moderate the association between migration and health insurance coverage as inactive return migrants are disproportionately underinsured while they focus on active job searches or prepare to return to the United States (H2b).3) Migrants will be more likely than non-migrants to rely on private clinics, pharmacies, and self-medication for medical care (H3a). Migrants' high rate of uninsurance will explain their reliance on private clinics, pharmacies, and self-medication (H3b).
3. Data, measures, and methods
3.1 Data Source
This study employs data from the 2009 and 2014 waves of the ENADID. The ENADID is based on a multi-stage probability sample that was designed to yield nationally representative estimates across geographic regions and community-sizes. It has been widely used to study Mexico-U.S. migration (e.g. Massey & Zenteno, 2000; Riosmena & Massey, 2012). The 2009 ENADID had 314,123 respondents more than five-years-old and the 2014 iteration contained 318,555 individuals more than five-years-old. The ENADID is a repeated cross-section. So, while I was able to assess changes in coverage across time, I was unable to adopt a longitudinal approach and assess changes in coverage within persons. I restricted the sample to respondents older than five because one of the two indicators of migration in the ENADID identifies place of residence five years prior to the census, i.e., before five-year-old children were born. In the multivariate analyses, I excluded an additional 5,197 cases (0.8%) with missing information on control variables.
Drawing on the two waves of data, I assessed potential improvements over time as Seguro Popular continues to expand access to medical care throughout Mexico. I restricted my analysis of access to a regular source of care to the 2014 wave because the 2009 survey did not solicit respondents' regular sources of care. I used the survey's weights throughout to provide nationally representative estimates.
3.2 U.S. migration
The ENADID asks respondents where they lived five-years and one-year prior to the survey. Thus, the data allows me to assess return migrants' health insurance coverage as a factor of time since return to Mexico. In cases where respondents lived in the United States both one and five years prior, I classified them as one-year migrants to reflect their most recent status. Therefore, all five-year migrants have been back in Mexico between one and five years and all one-year migrants have been back in Mexico between zero and 12-months. Because the survey is administered in June and July, it likely includes very few seasonal migrants, as annual temporary migrants (documented and undocumented) tend to work in the United States during the agricultural season and then return for a few months in the winter. Thus, especially given the decline in undocumented Mexican migration to the United States in recent years (Chishti & Hipsman, 2015; Schulthies & Ruiz Soto, 2017), I expect the majority of one- and especially five-year migrants to remain in Mexico rather than returning to the United States.
3.3 Health insurance coverage
I created two distinct measures of insurance coverage. The first, which I use for descriptive purposes, separates health insurance coverage into four categories: none (uninsured), employment-based (IMSS, ISSSTE, PEMEX, SEDENA, or SEMAR), social program (Seguro Popular), other (private and other). For regression analysis, I dichotomize health coverage as insured and uninsured to assess the odds of being insured and the impact of coverage on access to a regular source of care among migrants and non-migrants.
3.4 Regular source of care
Respondents were given options for their regular sources of care that correspond to the different health insurance coverage programs. Thus, I used a similar categorization scheme. For descriptive comparison, I created a four-category variable that included: employment-based clinics (IMSS, ISSSTE, PEMEX, SEDENA, or SEMAR), public clinics (Seguro Popular), non-insurance based options (private clinics, pharmacies, ornone), and other. For regression analysis, I dichotomized the variable to indicate those respondents who reported private clinics, pharmacies, or none as their regular source of care.
3.5 Labor market status
The two most commonly used measures of formal sector employment in Mexico are receipt of benefits through employment and employment in a firm of five or more workers (Arias et al., 2010; Perry et al., 2007; Villarreal & Blanchard, 2013). I could not use receipt of benefits to capture formal employment, as it would incorporate the dependent variable (health insurance coverage) into one of the predictor variables (employment status). The ENADID does not measure firm size. However, they do include a categorical variable that identifies workers' employment statuses. A recent study of Mexican return migrants found that this was a reliable proxy for labor market sector (Parrado & Gutierrez, 2016). The ENADID classifies respondents as employees, regular workers, day laborers, own-account workers, employers, and workers without pay. The significant majority of self-employed workers operate informally, either on their own account or as the owners of small firms with only a handful of employees (Levy, 2008). Similarly, day laborers almost certainly work in the informal sector, moving from one job to another without written contracts and the associated benefits. Therefore, I classified these workers as irregular to indicate their close proximity to informal sector workers. I treated the respondents who described themselves as employees or regular workers as regularly employed to reflect their more stable occupational statuses and proxy for formal sector employment.
To determine the validity of this classification scheme, I measured health insurance coverage (Table A1) and mode of affiliation (Table A2) by employment status. I restricted the consideration of mode of affiliation to the 2014 wave because this information was not available in 2009. These results, which are presented in Appendix A, indicate that employees and regular workers were far more likely than any other group to be affiliated with IMSS or ISSSTE. The group next most likely to participate in these employment-based coverage schemes were the inactive, likely affiliated via a formally employed family member. Consistent with formal employment, about 50% of employees and regular workers received their coverage via their work (Table A2), far more than any other category. Thus, this classification system appears to capture significant variation in the degree to which respondents work in formal sector jobs.
3.6 Individual, household, and community-level controls
Regression models were also adjusted for age and age-squared, educational attainment (Less than primary, completed primary, completed lower secondary, completed upper secondary).1 Age affects both employment status and eligibility for health insurance programs and other services that cater to children and the elderly. The squared term captures non-linearity in the association between age and health coverage. Education provides an indicator of social status and access to familial resources such as a parent's health coverage (Parker, Rubalcava, Teruel, & Behrman, 2007).
I included three variables to measure household context. First, I adjusted for marital status (single/never married, married, divorced/widowed). Married individuals can receive coverage through their partner's work. Additionally, returning migrants may receive assistance enrolling in Seguro Popular through a non-migrant spouse. Second, I included a dichotomous variable to indicate individuals who live alone, without any co-resident household members. Migrants' health insurance coverage may be impacted by household context. Mexican workers with employment-based coverage can affiliate unemployed or informally employed family members. Moreover, non-migrant household members could provide return migrants with information and logistical support in enrolling in Seguro Popular. Third, following Filmer and Pritchett (2011), I used principal component analysis to construct a composite indicator of household assets. The indicator includes items that tap different aspects of wealth ranging from home ownership and quality to utilities to possession of appliances and vehicles. Filmer and Pritchett (2011) have demonstrated that the asset index is a strong predictor of household expenditures.
Finally, all of the models were adjusted for community size (less than 2,500 inhabitants, 2,500 to 14,999 inhabitants, 15,000 to 99,999 inhabitants, or 100,000 plus). Rural areas tend to have weaker infrastructure and more limited access to services, such as healthcare. Yet, migrants are disproportionately drawn from rural areas (Rendall & Parker, 2014). Thus, migrants may have weaker access to health care in part due to their spatial context.
3.7 Analytic strategy
I conducted the analysis in three stages. First, I assessed changes in health coverage over time and identified differences in program affiliation by migrant status using the 2009 and 2014 data. T-tests identify significant changes across time. Results from stage 1 address the first set of hypotheses.
Second, I assessed potential explanations for the high rate of uninsurance among return migrants (second set of hypotheses), again using the pooled sample. To assess the proposed explanations for uninsurance among return migrants, I estimated three logistic regression models (Table 2), which regress health coverage on migration experience and all of the control variables (Model 1), controls plus labor market status (Model 2), and controls plus labor market status plus labor market status interacted with migration experience. These models test whether labor market status mediates or moderates the association between migration experience and health coverage.
Table 2. Weighted logistic regression estimates of the association bewteen U.S. migration and health insurance coverage, 2009-2014.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Migrant status (ref: non-migrant) | ||||||
| Five-year migrant | 0.420 | (0.382 0.461) *** | 0.436 | (0.396 0.481) *** | 0.280 | (0.239 0.328) *** |
| One-year migrant | 0.222 | (0.193 0.256) *** | 0.226 | (0.196 0.261) *** | 0.125 | (0.097 0.161) *** |
| Work status (ref: innactive) | ||||||
| Regularly employed | -- | -- -- | 1.138 | (1.111 1.166) *** | 1.131 | (1.104 1.159) *** |
| Irregularly employed | -- | -- -- | 0.470 | (0.460 0.482) *** | 0.467 | (0.456 0.478) *** |
| Interaction analysis | ||||||
| Five-year migrant* regularly employed | -- | -- -- | -- | -- -- | 2.010 | (1.579 2.560) *** |
| Five-year migrant* irregularly employed | -- | -- -- | -- | -- -- | 2.403 | (1.698 3.401) *** |
| One-year migrant* regularly employed | -- | -- -- | -- | -- -- | 2.242 | (1.791 2.808) *** |
| One-year migrant* irregularly employed | -- | -- -- | -- | -- -- | 3.075 | (2.161 4.376) *** |
| Male | 1.265 | (1.244 1.287) *** | 1.156 | (1.136 1.176) *** | 1.157 | (1.137 1.177) *** |
| Age | 1.006 | (1.005 1.006) *** | 1.009 | (1.008 1.010) *** | 1.009 | (1.008 1.010) *** |
| Agê2 | 1.000 | (1.000 1.000) *** | 1.000 | (1.000 1.000) *** | 1.000 | (1.000 1.000) *** |
| Educational attainment (ref: less than primary) | ||||||
| Primary complete | 1.056 | (1.025 1.088) *** | 1.076 | (1.044 1.109) *** | 1.075 | (1.043 1.108) *** |
| Secondary complete | 0.979 | (0.947 1.012) | 0.984 | (0.951 1.017) | 0.983 | (0.950 1.016) |
| Post-secondary | 1.117 | (1.081 1.155) *** | 1.087 | (1.050 1.125) *** | 1.086 | (1.050 1.124) *** |
| Lives alone | 0.903 | (0.860 0.949) *** | 0.913 | (0.869 0.960) *** | 0.912 | (0.868 0.959) *** |
| Marital status (ref: single, never married) | ||||||
| Married | 1.084 | (1.053 1.115) *** | 1.153 | (1.120 1.188) *** | 1.152 | (1.118 1.186) *** |
| Divorced/widowed | 0.932 | (0.903 0.963) *** | 0.970 | (0.939 1.002) | 0.969 | (0.938 1.001) |
| Household assets | 1.232 | (1.222 1.242) *** | 1.238 | (1.228 1.248) *** | 1.238 | (1.228 1.248) *** |
| Community size (ref: <2,500) | ||||||
| 2,500-14,999 | 1.094 | (1.065 1.123) *** | 1.114 | (1.085 1.144) *** | 1.114 | (1.085 1.144) *** |
| 15,000-99,999 | 1.015 | (0.988 1.043) | 1.071 | (1.042 1.100) *** | 1.071 | (1.042 1.100) *** |
| 100,000+ | 1.238 | (1.210 1.267) *** | 1.389 | (1.357 1.422) *** | 1.389 | (1.356 1.422) *** |
| Year = 2014 | 4.664 | (4.508 4.827) *** | 4.904 | (4.737 5.076) *** | 4.907 | (4.740 5.079) *** |
| Pseudo R-squared | 0.067 | 0.081 | 0.082 | |||
| Observations | 627,481 | 627,481 | 627,481 | |||
Source: Mexico' 2009 and 2014 National Survey of Demographic Dynamics
p<0.05,
p<0.01,
p<0.001
Notes: All models included state fixed effects. Robust standard errors were used to adjust for municipal clustering.
Finally, I assessed the third set of hypotheses concerning access to health care using the 2014 data. First, I identified descriptive differences in access to care by migrant status (Table 3) (H3a). Then, to assess whether migrants' uninsurance limits their access to a regular source of care (H3b), I estimated two logistic regression models on the odds of having no regular source of care, first without and then with a variable adjusting for health insurance coverage (Table 4). I used formal mediation analysis to measure the proportion of the association between U.S.-migration and lack of a regular source of care that is mediated by uninsurance (Baron & Kenny, 1986). Bear in mind, due to the cross-sectional nature of the data, the analysis does not provide causal evidence of mediation, but rather describes the importance of health insurance coverage to having a regular source of care.
Table 3. Weighted summary of respondents' regular sources of care by migrant status in 2014.
| Non-migrants | 5-year migrants | 1-year migrants | |
|---|---|---|---|
| IMSS, ISSSTE, PEMEX, SEDENA, SEMAR | 34.2% | 16.2%*** | 10.3%*** |
| Seguro Popular or other public clinic | 36.2% | 41.7%** | 27.7%** |
| none | 29.4% | 41.7%*** | 61.7%*** |
| Other | 0.2% | 0.4% | 0.1% |
|
| |||
| Observations | 318,555 | 1,966 | 524 |
Source: Mexico's 2014 National Survey of Demographic Dynamics
p<0.05,
p<0.01,
p<0.001, stars identify significant differences between each of the migrant types and non-migrants
Table 4. Weighted logistic regression estimates of the adjusted odds of having no regular source of care.
| Model 1 | Model 2 | |||
| OR | (95% CI) | OR | (95% CI) | |
| Migrant status ref: non-migrant) | ||||
| Five-year migrant | 1.887 | 1.674 2.127 *** | 1.226 | 1.051 1.430 ** |
| One-year migrant | 4.341 | 3.479 5.416 *** | 2.565 | 1.960 3.356 *** |
| Insured | -- | -- -- | 0.057 | 0.056 0.059 *** |
| Work status (ref: innactive) | ||||
| Regularly employed | 1.001 | 0.973 1.029 | 0.972 | (0.942 1.003) |
| Irregularly employed | 1.811 | 1.758 1.866 *** | 1.344 | (1.297 1.393) *** |
| Male | 0.859 | (0.840 0.878) *** | 0.929 | (0.906 0.954) *** |
| Age | 0.997 | (0.997 0.998) *** | 0.997 | (0.996 0.998) *** |
| Agê2 | 1.000 | (1.000 1.000) *** | 1.000 | (1.000 1.000) *** |
| Educational attainment (ref: less than primary) | ||||
| Primary complete | 0.938 | (0.899 0.978) ** | 0.972 | (0.925 1.022) |
| Secondary complete | 1.013 | (0.969 1.058) | 0.981 | (0.931 1.034) |
| Post-secondary | 1.431 | (1.370 1.495) *** | 1.616 | (1.534 1.701) *** |
| Lives alone | 1.383 | (1.300 1.470) *** | 1.497 | (1.394 1.607) *** |
| Marital status (ref: single, never married) | ||||
| Married | 0.800 | (0.775 0.825) *** | 1.053 | (1.017 1.090) ** |
| Divorced/widowed | 0.853 | (0.814 0.894) *** | 0.941 | (0.892 0.992) * |
| Household assets | 0.824 | (0.796 0.853) *** | 0.826 | (0.792 0.862) *** |
| Community size (ref: <2,500) | ||||
| 2,500-14,999 | 0.763 | (0.739 0.788) *** | 0.743 | (0.716 0.771) *** |
| 15,000-99,999 | 0.587 | (0.567 0.608) *** | 0.540 | (0.518 0.564) *** |
| 100,000+ | 0.357 | (0.345 0.369) *** | 0.325 | (0.313 0.339) *** |
|
| ||||
| Pseudo R-squared | 0.051 | 0.246 | ||
| Observations | 318,448 | 318,448 | ||
Source: Mexico's 2014 National Survey of Demographic Dynamics
p<0.05,
p<0.01,
p<0.001
Notes: All models included state fixed effects. Robust standard errors were used to adjust for municipal clustering.
4. Results
4.1 Descriptive analysis of health insurance coverage
Health insurance coverage increased significantly among migrants and non-migrants between 2009 and 2014 (Table 1), reflecting the on-going implementation of Seguro Popular and confirming H1a. The increases in health insurance coverage by migrant status were similar and all of the improvements were statistically significant (p<0.001). There was very modest attenuation of the gap in coverage between migrants and non-migrants over this period. However, consistent with Wassink's (2016) analysis of coverage growth between 2000 and 2010, uninsurance among return migrants continued to decline at a slower rate relative to non-migrants. 21.2%/72.4% = 29% of uninsured one-year migrants and 18.8%/57% = 33% of uninsured five-year migrants gained coverage between 2009 and 2014 compared to 18.3%/37.6% = 49% of uninsured non-migrants. One-year migrants were far more likely than non-migrants or five-year migrants to be uninsured in 2014 (48.8%). The disparity between one- and five-year migrants supports H1b, indicating that reintegration among return migrants is a gradual process that unfolds across time.
Table 1. Changes in health insurance coverage between 2009 and 2014 by migrant status.
| N | % Insured, 2009 | % Insured, 2014 | Difference | T-test | |
|---|---|---|---|---|---|
| 1-year | 1,665 | 27.6% | 48.8% | 21.2% | *** |
| 5-year migrants | 3,745 | 43.0% | 61.9% | 18.8% | *** |
| Non-migrants | 627,268 | 62.3% | 80.6% | 18.3% | *** |
Source: Mexico's National Survey of Demographic Dynamics (2009 Demographic Dynamics (2014)
p<0.05,
p<0.01,
p<0.001
Figure 1 reports health insurance coverage by program and migrant status in 2009 and 2014. Coverage through employment-based programs was much higher among non-migrants than return migrants in both periods, a finding that is consistent with prior research documenting the deterring effect of formal sector employment on Mexican emigration (Villarreal & Blanchard, 2013) and a high rate of informal sector employment among Mexican return migrants (Lindstrom, 2013; Sheehan & Riosmena, 2013). As the figure shows, growth in coverage over the period was almost entirely accounted for by Seguro Popular. The greatest uptick in affiliation was among five-year migrants whose coverage through social programs surged from 18% in 2009 to 44% in 2014 (26% increase), outpacing the increases in social programs made among non-migrants (22%) and one-year migrants (only 15%). The low level of coverage among one-year migrants and their significantly lower growth in affiliation with available social programs lends further support to H1b.
Figure 1. Weighted estimates of percent covered by each insurance program among Mexican migrants and non-migrants in 2009 and 2014.
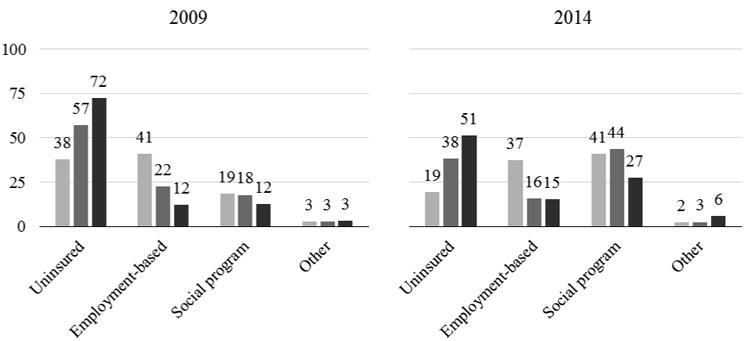
Note: Employment-based includes IMSS, ISSSTE, and PEMEX, SEDONA, and SEMAR. Social programs include Seguro Popular and Oportunidades. Other includes private and other.
Source: Mexico's 2009 and 2014 National Surveys of Demographic Dynamics (n=632,678).
4.2 Regression analysis of health insurance coverage
Adjustment for individual, household, and community factors strengthened the negative associations between one- and five-year migration experiences and health coverage in Mexico. In Model 1 in Table 2, being a five-year migrant was associated with 58% lower odds of having health insurance and being a one-year migrant was associated with 78% lower odds of having health insurance.
Consistent with H2a and prior research on Mexican migrants, five-year migrants (31%) and one-year migrants (31%) were significantly more likely than non-migrants (19%) to be irregularly employed (summary statistics available upon request). Yet, despite irregular employment being associated with 53% lower odds of being insured, both one- and five-year migrant statuses remained strongly and significantly associated with uninsurance in Model 2, with neither coefficient changing by more than 0.02. This result led to the rejection of H2a as the analysis revealed no evidence of mediation via labor market status.
Model 3 revealed a strong and highly significant interaction between migration experience and labor market status. As hypothesized, labor market inactivity was associated with much greater odds of being uninsured among return migrants relative to non-migrants. Among inactive migrants (the baseline coefficients), five- and one-year migrations were associated with 73% and 87% lower odds of having health insurance coverage respectively. By contrast, having regular employment reduced the negative effect of migration on health insurance coverage to just 44% and 72% lower odds among 5-year and one-year migrants respectively. Having an irregular job reduced the effect even further (likely do in part to the strong negative effect of irregular employment among the non-migrant population) to just 33% and 62%. The moderating effect of inactivity supports H2b that inactive migrants are likely to be focused on a job search or preparing to return to the United States, and thus opt not to devote resources to enrolling in health insurance programs. The significant interaction among five-year migrants who have been back in Mexico for at least one year indicates that labor market inactivity represents more than just a plan to return to the United States, as few labor migrants could afford to go without work voluntarily for a year or more following their return. Practically speaking, these interactions suggest that employment plays a central role in migrants' reintegration into Mexican sending communities. Programs focused on migrants' labor market re-entry might provide significant public health benefits.
4.3 Access to health care
Consistent with their health insurance coverage, migrants – especially one-year migrants – were significantly less likely to list one of Mexico's employment based clinics as their regular source of care (Table 3). Among five-year migrants, the gap is partially accounted for by public options, which in 2014 provided regular sources of care to 42% of Mexicans who lived in the United States in 2009. However, both five-year and particularly one-year migrants were far more likely than non-migrants to lack a regular source of care through employment or one of Mexico's publicly available options (p<0.001). Sixty-two percent of Mexicans who lived in the United States in 2013 and 42%of those who were abroad in 2009 relied on private clinics and pharmacies or had no regular source of care other than self-medication in 2014. These results support H3a, highlighting the significant barriers to medical care that confront recently returned Mexican migrants.
To test whether uninsurance mediates the association between migration experience and a lack of access to regular care, I estimated two logistic regression models, first unadjusted and then adjusted for health insurance coverage (Table 4). Net of controls, five-year migrant status (89% higher odds) and especially one-year migrant status (more than four-times the odds) were both associated with significantly greater risk of not having access to a regular source of care (Model 1). After adjustment for health insurance coverage (Model 2), the associations reduced substantially to 23% higher odds among five-year migrants and 157% higher odds among one-year migrants. I used the process described by Barron and Kenny (1986) to formally calculate the proportion of the association between migration and access to a regular source of care that is mediated through their health insurance coverage – or lack thereof. Among five-year migrants, 78% of the association (p<0.001) was mediated through uninsurance. Among one-year migrants, uninsurance accounted for 55% of the association (p<0.001). The mediating role of uninsurance in the association between recent migration experience and access to care supports H3b, highlighting the persistent costs of uninsurance among recently returned Mexican migrants.
5. Discussion
Despite the vast literature on the health of Mexican immigrants in the United States, scholars are only beginning to uncover the consequences of U.S.-migration for the well-being of those who return home (Arenas et al., 2015; Diaz et al., 2016; Familiar et al., 2011; Ullmann et al., 2011). As studies document the greater risk of poor mental and physical health among Mexico's growing population of return migrants, it is essential to assess returnees' access to medical care upon return. Using data from two waves of the ENADID, I examined recent changes in health insurance coverage among migrants relative to non-migrants, factors that may contribute to migrants' low level of health coverage, and the impact of uninsurance on return migrants' access to medical care. Throughout, I distinguished between migrants returned in the past year, versus those who had been back in Mexico for between 1-5 years, an improvement on prior studies (Aguila & Zissimopoulos, 2013; Martinez-Donate et al., 2017; Polsky et al., 2006; Wassink, 2016).
This study contributes to the literature on immigration and health in three important ways. First, I assessed changes in overall coverage and program affiliation by migrant status in 2009 and 2014. Despite steady overall growth in health coverage in Mexico, return migrants remain substantially underinsured relative to non-migrants. Uninsurance is especially low among those returned within the past year, a gap that largely results from lower employment-based coverage among return migrants, who tend to work in the informal sector of the economy (Sheehan & Riosmena, 2013; Villarreal & Blanchard, 2013).
Second, to better understand the impact of labor market status on return migrants' health insurance coverage, I used logistic regression analysis to assess whether controlling for workers' economic sector mediates the association between migration experience and health coverage. Despite revealing a strong negative association between irregular employment and health coverage, which is consistent with prior studies (Levy, 2008; Tornarolli et al., 2014), adjustment for labor market status only marginally attenuated the association between migration and health insurance coverage. Thus, despite return migrants' overrepresentation in irregular work, I rejected the hypothesis that labor market status operates as a intervening mechanism, explaining the relationship between U.S. migration and health coverage upon return to Mexico.
However, the addition of an interaction term between labor market status and migration experience revealed that labor market inactivity, is associated with significantly lower coverage among return migrants than non-migrants. The significant interaction effect suggests that returning migrants' high levels of uninsurance may in large part be driven by unsuccessful job searches, which likely take priority over their reintegration into institutions such as health care. Migrants who rapidly reintegrate into the Mexican labor market can turn their energy to other tasks, while those who struggle to find work may put off enrolling in health care, placing themselves at risk of incurring catastrophic medical expenses should an emergency occur. This finding suggests that policies aimed at reintegrating return migrants into the labor market may have broader benefits for their reintegration into important institutions such as health care.
Third, I provided the first comparison of access to regular care between Mexican return migrants and non-migrants that used data collected after the implementation Seguro Popular. Recently returned Mexican migrants are disproportionately dependent on private clinics, pharmacies, and self-medication. Such dependence likely reduces their utilization of preventative services and creates significant financial risk when health emergencies occur. Costs associated with unexpected medical procedures disrupt families' socioeconomic strategies by diverting resources away from investments such as children's education or the formation of a businesses (Galárraga et al., 2010; Knaul & Frenk, 2005), important mobility strategies among less educated Mexicans. Moreover, among return migrants, health costs can motivate future migrations, disrupting returnees' settlement plans and potential investments in their origin communities (Davies, Borland, Blake, & West, 2011; Hagan & Wassink, 2016). Formal mediation analysis revealed that more than half of the association between migration experience and access to care was explained by migrants' low levels of health insurance coverage. These results are consistent with a recent assessment of return migrants in Tijuana (Martinez-Donate et al., 2017), suggesting that migrants' uninsurance is a primary barrier to receiving medical care.
Though this study makes several important contributions to understanding access to medical care among Mexican return migrants, it is not without limitations that highlight the need for additional investigation. First, the data is cross-sectional. Thus, while I showed differences between migrants by time since return, I was unable to consider pre-migration coverage or repeat migration – I explored longitudinal data sources such as the Mexican Family Life Survey, but they lacked sufficiently large longitudinal migrant samples to reliably assess health insurance coverage pre- and post-migration. Second, this analysis had limited measures of labor market status and sectors of employment. Although the indicator of regular employment was correlated with formal sector benefits, measurement error likely weakened its ability to mediate between migration and health insurance coverage. Third, this study lacked direct measures of health care utilization or medical expenditures. Thus, although the results suggest that migrants' low levels of health coverage limit their access to care, I was unable to directly assess the impact of migration on receipt of medical attention or the type of services received.
International migrants exist in a liminal institutional space, simultaneously distanced from their origin community and marginalized in the place of destination (Waldinger, 2015). Torres and Waldinger (2015) recently documented the layers of “civic stratification” that systematically exclude Mexicans in the United States from basic health services. When Mexican immigrants return home expressly to procure medical care, they disproportionately rely on private clinics, highlighting their separation from institutional supports in sending communities (González-Block & Sierra-de la Vega, 2011; Vargas Bustamante et al., 2012; Wallace et al., 2009). My study extends these findings by revealing that, as Mexicans in the United States too often lack access to medical care, those who return home are also disproportionately uninsured and report their regular source of care as a private clinic, pharmacy, self-medication, or none. As research on return migration to Mexico and other Latin American countries moves beyond labor market outcomes to consider returnees' health and well-being, studies should investigate the factors that enable and constrain former migrants' access to essential social resources such as medical care (For a recent example, see Martinez-Donate et al., 2017). Such analysis is vital to policymakers as they attempt to cope with the growing population of return migrants who are increasingly opting to remain at home permanently, rather than return to the United States.
Appendix A
Table A1. Health insurance coverage by employment status in 2014.
| Uninsured | IMSS | ISSSTE | PEMEX | Other Public | Seguro Popular | Oportuni dades | Private | Other | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Innactive | 17% | 27% | 7% | 1% | 0% | 42% | 3% | 2% | 0% | 100% |
| Employee | 17% | 42% | 11% | 1% | 1% | 23% | 1% | 3% | 0% | 100% |
| Regular worker | 16% | 53% | 1% | 1% | 0% | 26% | 1% | 0% | 0% | 100% |
| Day laborer | 26% | 5% | 1% | 0% | 0% | 63% | 4% | 0% | 0% | 100% |
| Own-account worker | 29% | 15% | 4% | 1% | 0% | 46% | 2% | 2% | 0% | 100% |
| Employer | 34% | 22% | 5% | 0% | 0% | 20% | 0% | 18% | 0% | 100% |
| Unpaid family worker | 26% | 11% | 3% | 0% | 0% | 52% | 5% | 1% | 0% | 100% |
Source: Mexico's 2014 National Survey of Demographic Dynamics (N=632,678)
Table A2. Mode of affiliation with health insurance coverage by employment status in 2014.
| None | Relative in household | Employment | Relative outside household | Retirement or disability | Student | Personal contract | Social program | None | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Innactive | 17% | 43% | 2% | 3% | 3% | 2% | 7% | 23% | 0% | 100% |
| Employee | 17% | 10% | 50% | 1% | 0% | 1% | 7% | 14% | 0% | 100% |
| Regular worker | 16% | 10% | 52% | 0% | 0% | 0% | 5% | 15% | 0% | 100% |
| Day laborer | 26% | 23% | 3% | 1% | 1% | 0% | 10% | 35% | 0% | 100% |
| Own-account worker | 29% | 19% | 4% | 3% | 2% | 0% | 13% | 30% | 0% | 100% |
| Employer | 34% | 13% | 17% | 3% | 1% | 0% | 21% | 11% | 0% | 100% |
| Unpaid family worker | 26% | 27% | 2% | 2% | 2% | 2% | 9% | 30% | 0% | 100% |
Source: Mexico's 2014 National Survey of Demographic Dynamics (N=318,511)
Footnotes
These categories reflect major transitions in Mexico's education system and roughly correspond to quartiles of the adult population.
References
- Aguila E, Zissimopoulos J. Retirement and health benefits for Mexican migrant workers returning from the United States. International Social Security Review. 2013;66(2):101–125. doi: 10.1111/issr.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amuedo-Dorantes C, Puttitanum T, Martinez-Donate AP. How Do Tougher Immigration Measures Affect Unauthorized Immigrants? Demography. 2013;50(3):1067–1091. doi: 10.1007/s13524-013-0200-x. https://doi.org/10.1007/s13524-013-0200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Donate Ana P, Z X. Healthcare access among circular and undocumented Mexican migrants: results from a pilot survey on the Mexico-US border. International Journal of Migration and Border Studies. 2014;1(1):57–108. doi: 10.1504/IJMBS.2014.065069. https://doi.org/10.1504/IJMBS.2014.065069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arenas E, Goldman N, Pebley AR, Teruel G. Return Migration to Mexico: Does Health Matter? Demography. 2015;52(6):1853–1868. doi: 10.1007/s13524-015-0429-7. https://doi.org/10.1007/s13524-015-0429-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias J, Azuara O, Bernal P, Heckman JJ, Villarreal C. Policies to Promote Growth and Economic Efficiency in Mexico 2010 [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Cassarino JP. Theorizing Return Migration: The Conceptual Approach to Return Migrants Revisited. International Journal on Multicultural Societies. 2004;6(2):253–79. [Google Scholar]
- Chishti M, Hipsman F. Historic Shift, New Migration Flows from Mexico Fall Below Those from China and India. Washington, DC: Migration Policy Institute; 2015. [Google Scholar]
- Creighton MJ, Goldman N, Pebley AR, Chung CY. Durational and generational differences in Mexican immigrant obesity: Is acculturation the explanation? Social Science & Medicine. 2012;75(2):300–310. doi: 10.1016/j.socscimed.2012.03.013. https://doi.org/10.1016/j.socscimed.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies AA, Borland RM, Blake C, West HE. The Dynamics of Health and Return Migration. PLoS Med. 2011;8(6):e1001046. doi: 10.1371/journal.pmed.1001046. https://doi.org/10.1371/journal.pmed.1001046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diaz CJ, Koning SM, Martinez-Donate AP. Moving Beyond Salmon Bias: Mexican Return Migration and Health Selection. Demography. 2016;53(6):2005–2030. doi: 10.1007/s13524-016-0526-2. https://doi.org/10.1007/s13524-016-0526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Familiar I, Borges G, Orozco R, Medina-Mora ME. Mexican migration experiences to the US and risk for anxiety and depressive symptoms. Journal of Affective Disorders. 2011;130(1–2):83–91. doi: 10.1016/j.jad.2010.09.025. [DOI] [PubMed] [Google Scholar]
- Fernández-Niño JA, Ramírez-Valdés CJ, Cerecero-Garcia D, Bojorquez-Chapela I. Deported Mexican migrants: health status and access to care. Revista de Saúde Pública. 2014;48(3):478–485. doi: 10.1590/S0034-8910.2014048005150. https://doi.org/10.1590/S0034-8910.2014048005150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galárraga O, Sosa-Rubí S, Salinas-Rodríguez A, Sesma-Vázquez S. Health insurance for the poor: impact on catastrophic and out-of-pocket health expenditures in Mexico. 2010;11 doi: 10.1007/s10198-009-0180-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman N, Pebley AR, Creighton MJ, Teruel GM, Rubalcava LN, Chung C. The Consequences of Migration to the United States for Short-Term Changes in the Health of Mexican Immigrants. Demography. 2014;51(4):1159–1173. doi: 10.1007/s13524-014-0304-y. https://doi.org/10.1007/s13524-014-0304-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Barrera A. Washington, DC: Pew Research Center; 2015. More Mexicans Leaving Than Coming to the U.S. Retrieved from http://www.pewhispanic.org/2015/11/19/more-mexicans-leaving-than-coming-to-the-u-s/ [Google Scholar]
- González-Block MA, Bustamante AV, Sierra LA, Cardoso AM. Redressing the Limitations of the Affordable Care Act for Mexican Immigrants Through Bi-National Health Insurance: A Willingness to Pay Study in Los Angeles - Springer. Journal of Immigrant and Minority Health. 2014;16(2):179–188. doi: 10.1007/s10903-012-9712-5. https://doi.org/10.1007/s10903-012-9712-5. [DOI] [PubMed] [Google Scholar]
- González-Block MA, Sierra-de la Vega LA. Hospital utilization by Mexican migrants returning to Mexico due to health needs. BMC Public Health. 2011;11:241–248. doi: 10.1186/1471-2458-11-241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan J, Rodriguez N, Castro B. Social Effects of mass Deportations by the United States Government, 2000-10. Ethnic and Racial Studies. 2011;34(8):1374–91. [Google Scholar]
- Hagan J, Wassink J. New Skills, New Jobs: Return Migration, Skill Transfers, and Business Formation in Mexico. Social Problems. 2016;63(4):513–533. doi: 10.1093/socpro/spw021. https://doi.org/http://dx.doi.org/10.1093/socpro/spw021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King G, Gakidou E, Imai K, Lakin J, Moore RT, Nall C, et al. Llamas H. Public policy for the poor? A randomised assessment of the Mexican universal health insurance programme. Lancet. 2009;373(9673):1447–54. doi: 10.1016/S0140-6736(09)60239-7. [DOI] [PubMed] [Google Scholar]
- Knaul FM, Frenk J. Health Insurance In Mexico: Achieving Universal Coverage Through Structural Reform. Health Affairs. 2005;24(6):1467–1476. doi: 10.1377/hlthaff.24.6.1467. [DOI] [PubMed] [Google Scholar]
- Knaul FM, González-Pier E, Gómez-Dantés O, García-Junco D, Arreola-Ornelas H, Barraza-Lloréns M, et al. Frenk J. The quest for universal health coverage: achieving social protection for all in Mexico. Lancet. 2012;380(9849):1259–79. doi: 10.1016/S0140-6736(12)61068-X. [DOI] [PubMed] [Google Scholar]
- Levy S. Good Intentions, Bad Outcomes: Social Policy, Informality, and Economic Growth in Mexico. Brookings Institution Press; 2008. [Google Scholar]
- Lindstrom DP. The Occupational Mobility of Return Migrants: Lessons from North America. In: Neyer G, Andersson G, Kulu H, Bernardi L, Bühler C, editors. The Demography of Europe. Springer; Netherlands: 2013. pp. 175–205. https://doi.org/10.1007/978-90-481-8978-6_8. [Google Scholar]
- López-Sanders L. Changing the navigator's course: How the increasing rationalization of healthcare influences access for undocumented immigrants under the Affordable Care Act. Social Science & Medicine. 2017;178:46–54. doi: 10.1016/j.socscimed.2017.01.066. [DOI] [PubMed] [Google Scholar]
- Martinez JN, Aguayo-Tellez E, Rangel-Gonzalez E. Explaining the Mexican-American Health Paradox Using Selectivity Effects. International Migration Review. 2014:878–906. https://doi.org/10.1111/imre.12112.
- Martinez-Donate AP, Ejebe I, Zhang X, Guendelman S, Lê-Scherban F, Rangel G, et al. Amuedo-Dorantes C. Access to Health Care among Mexican Migrants and Immigrants: A Comparison across Migration Phases. Journal of Health Care for the Poor and Underserved. 2017;28(4):1314–1326. doi: 10.1353/hpu.2017.0116. https://doi.org/10.1353/hpu.2017.0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massey DS, Espinosa KE. What's Driving Mexico-U.S. Migration? A Theoretical, Empirical, and Policy Analysis. American Journal of Sociology. 1997;102(4):939–999. [Google Scholar]
- Massey DS, Zenteno R. A Validation of the Ethnosurvey: The Case of Mexico-U.S. Migration. International Migration Review. 2000;34(3):766–793. [Google Scholar]
- MATT. The US/Mexico Cycle End of an Era: Quantitative Research Study Preliminary Findings and Insights. 2013:1–64. MATT. [Google Scholar]
- Parker S, Rubalcava LN, Teruel GM, Behrman JR. The Quality of Education in Latin America and the Caribbean Region: The Mexican Case. Inter-American Development Bank; 2007. [Google Scholar]
- Parrado EA, Gutierrez EY. The Changing Nature of Return Migration to Mexico, 1990–2010. Sociology of Development. 2016;2(2):93–118. https://doi.org/10.1525/sod.2016.2.2.93. [Google Scholar]
- Passell J, Cohn D, Gonzalez-Barrera A. Net Migration from Mexico Falls to Zero–and Perhaps Less. Washington, DC: Pew Research Center; 2012. [Google Scholar]
- Perry GE, Maloney WF, Arias OS, Fajnzlber P, Mason AD, Saavedra-Chanduvi J. Informality: Exit and Exclusion. The World Bank; 2007. [Google Scholar]
- Polsky D, Pagan JA, Ross SJ. Access to Health Care for Migrants Returning to Mexico. Journal of Health Care for the Poor and Underserved. 2006;17(2):374–385. doi: 10.1353/hpu.2006.0067. https://doi.org/10.1353/hpu.2006.0067. [DOI] [PubMed] [Google Scholar]
- Potochnick SR, Perreira KM. Depression and anxiety among first-generation immigrant Latino youth: key correlates and implications for future research. The Journal of Nervous and Mental Disease. 2010;198(7):470–477. doi: 10.1097/NMD.0b013e3181e4ce24. https://doi.org/10.1097/NMD.0b013e3181e4ce24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendall MS, Parker SW. Two Decades of Negative Educational Selectivity of Mexican Migrants to the United States. Population and Development Review. 2014;40(3):421–446. doi: 10.1111/j.1728-4457.2014.00692.x. https://doi.org/10.1111/j.1728-4457.2014.00692.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riosmena F, Massey DS. Pathways to El Norte: Origins, Destinations, and Characteristics of Mexican Migrants to the United States1. International Migration Review. 2012;46(1):3–36. doi: 10.1111/j.1747-7379.2012.00879.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz-Tagle JC, Wong R. Determinants of Return Migration to Mexico among Mexicans in the United States; Population Association of America Annual Meeting (Vol Population Association of American Annual Meeting).2009. [Google Scholar]
- Schulthies R, Ruiz Soto AG. A Revolving Door no More: A Statistical Profile of Mexican Adults Repatriated from the United States. Lanham, MD: Migration Policy Institute; 2017. [Google Scholar]
- Sheehan CM, Riosmena F. Migration, business formation, and the informal economy in urban Mexico. Social Science Research. 2013;42(4):1092–1108. doi: 10.1016/j.ssresearch.2013.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su D, Richardson C, Wen M, Pagán JA. Cross-Border Utilization of Health Care: Evidence from a Population-Based Study in South Texas. Health Services Research. 2011;46(3):859–876. doi: 10.1111/j.1475-6773.2010.01220.x. https://doi.org/10.1111/j.1475-6773.2010.01220.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tornarolli L, Battistón D, Gasparini L, Gluzmann P. Exploring Trends in Labor Informality in Latin America, 1990-2010. 2014;(No. 159) CEDLAS. [Google Scholar]
- Torres JM, Waldinger R. Civic Stratification and the Exclusion of Undocumented Immigrants from Cross-border Health Care. Journal of Health and Social Behavior. 2015;56(4):438–459. doi: 10.1177/0022146515610617. https://doi.org/10.1177/0022146515610617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullmann SH, Goldman N, Massey DS. Healthier before they migrate, less healthy when they return? The health of returned migrants in Mexico. Social Science & Medicine. 2011;73(3):421–428. doi: 10.1016/j.socscimed.2011.05.037. https://doi.org/10.1016/j.socscimed.2011.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hook J, Zhang W. Who Stays? Who Goes? Selective Emigration among the Foreign-Born. Population Research and Policy Review. 2011;30(1):1–24. doi: 10.1007/s11113-010-9183-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vargas Bustamante A, Fang H, Garza J, Carter-Pokras O, Wallace SP, Rizzo JA, Ortega AN. Variations in Healthcare Access and Utilization Among Mexican Immigrants: The Role of Documentation Status. Journal of Immigrant and Minority Health. 2012;14(1):146–155. doi: 10.1007/s10903-010-9406-9. https://doi.org/10.1007/s10903-010-9406-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villarreal A, Blanchard S. How Job Characteristics Affect International Migration: The Role of Informality in Mexico. Demography. 2013;50(2):751–75. doi: 10.1007/s13524-012-0153-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldinger R. The Cross-Border Connection: Immigrants, Emigrants, and Their Homelands. Harvard University Press; 2015. [Google Scholar]
- Wallace SP, Mendez-Luck C, Castañeda X. Heading South: Why Mexican Immigrants in California Seek Health Services in Mexico. Medical Care. 2009;47(6):662–69. doi: 10.1097/MLR.0b013e318190cc95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassink JT. Implications of Mexican Health Care Reform on the Health Coverage of Nonmigrants and Returning Migrants. American Journal of Public Health. 2016;106(5):848–850. doi: 10.2105/AJPH.2016.303094. https://doi.org/10.2105/AJPH.2016.303094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wassink JT, Hagan JM. A Dynamic Model of Self-Employment and Socioeconomic Mobility among Return Migrants: The Case of Urban Mexico. Social Forces. doi: 10.1093/sf/sox095. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheatley C. Push Back: U.S. Deportation Policy and the Reincorporation of Involuntary Return Migrants in Mexico*. The Latin Americanist. 2011;55(4):35–60. [Google Scholar]


