Abstract
Background
Besides physical problems, cigarette smoking is associated with a high prevalence of comorbid depression and anxiety symptoms. One of the reasons behind high post-cessation smoking lapse and relapse rates is inattentiveness to these symptoms during the process of cessation. The aim of this study was to examine the effects of acceptance and commitment therapy (ACT) on male smokers’ comorbid depression and anxiety symptoms and smoking cessation.
Methods
This two-group pre-test-post-test randomized controlled trial was done on a random sample of seventy male smokers. Participants were randomly and evenly allocated to an intervention and a control group. Patients in these groups received either acceptance or commitment therapy or routine psychological counseling services include cognitive behavior therapy, respectively. Study data were collected through a demographic questionnaire, the Structural Clinical Interview (SCI) for Diagnostic and Statistical Manual of Mental Disorders-4th Edition (DSM-IV) disorders, Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), and Micro Smokerlyzer carbon monoxide monitor. The SPSS software was employed to analyze the data.
Findings
After the intervention, depression and anxiety scores and smoking cessation rate in the intervention group were respectively lower and higher than the control group (P < 0.050).
Conclusion
ACT can significantly improve comorbid depression and anxiety symptoms and smoking cessation rate. Thus, it can be used to simultaneously manage depression, anxiety, and cigarette smoking.
Keywords: Smoking cessation, Depression, Anxiety, Acceptance and commitment therapy
Introduction
Cigarette smoking is among the most serious health problem in the world. Currently, about 1.2 billion people smoke cigarette worldwide.1,2 The prevalence of cigarette smoking in the world and in Iran has been reported to be 31.1% and 22.3%, respectively.3,4
Cigarette smoking is associated with the high risk of different developing health problems such as cardiovascular disease, different types of cancer, and premature death.5 On average, it leads to about five million deaths worldwide annually.5,6 Moreover, about 500 billion dollars are lost globally due to cigarette smoking.7
The most common treatment for cigarette smoking is medication therapy.8 Studies have shown the effectiveness of bupropion and varenicline in smoking cessation.9 However, as many different bio-psycho-social factors contribute to cigarette smoking, medication therapy is beneficial to only a small percentage of smokers.10 Thus, other therapies are used to increase cessation success rate. Recent studies have reported the short- and long-term positive effects of behavioral therapies on smoking cessation.11,12 People have more positive attitudes towards psychotherapy than medication therapy, and this positive attitude was found to have positive therapeutic effects.13,14
Cognitive behavioral therapy is the most common and effective type of behavioral therapy.11,15 It aims to identify and correct dysfunctional cognitions, emotions, and behaviors.13
Despite the known positive effects of medication and psychological therapies on smoking cessation, these treatments are associated with high lapse and relapse rates.16 Studies have reported that 80% of people who quit smoking will experience an early lapse during the first seven days of cessation.17,18 One of the most important factors behind early lapse and relapse is the failure to address and treat psychological problems among volunteers for smoking cessation.19 Psychological problems such as depression and anxiety have been reported to be significantly correlated with cigarette smoking.20 Similarly, negative emotions related to depression and anxiety are also associated with the high risk of post-cessation relapse21 and make cessation more difficult.20,22 In fact, each psychological problem is associated with a range of negative cognitions and emotions,23 and thus smokers who suffer from depression and anxiety have more cognitive problems. Furthermore, studies into the role of depression and anxiety in smoking cessation have shown that besides smoking cessation treatments, smokers need to receive treatments for anxiety and depression.22,24 The results of a study showed higher cessation rate among depressed smokers who received cognitive behavioral therapy based on mood management.19 Another study on 251 pregnant smokers decided to quit smoking also revealed that anxiety is a significant predictor of postnatal smoking lapse.25
Despite the wide use of cognitive behavioral therapies, the effects of these therapies on cessation success rate are not strong enough.26 The results of a study showed that during a three-month follow-up period after cognitive behavioral therapy for smoking cessation, lapse and relapse rates were more than 50%.27 Limited effectiveness of cognitive behavioral therapies in smoking cessation may be due to the fact that these therapies do not focus on comorbid depression and anxiety disorders.20,28 In principle, they just have focused on specific types of dysfunctional cognitions related to each problem and thus, cannot concurrently manage several problems.29 Besides, cognition modification may not be effective for all patient populations. In other words, some patients may be unable to modify their dysfunctional cognitions despite receiving cognitive behavioral therapies.30
Acceptance and commitment therapy (ACT) is one of the psychological therapies for behavioral problems. As a transdiagnostic treatment, ACT deals with the common pathological core of psychological problems instead of focusing just on one certain type of problem.31 Consequently, ACT can concurrently treat depression and anxiety.32 While receiving ACT, people do not continually and hardly attempt to change their feelings, thoughts, and emotions; rather, they simply change their relationships with those feelings, thoughts, and emotions.33 Through incorporating mindfulness and focusing on changing individuals’ relationships, the ACT model attempts to promote adaptation and flexibility. This model comprises six processes, namely acceptance, diffusion, self as context, committed action, values, and contact with the present moment.31 The main goal of ACT is to help people acquire psychological flexibility. While receiving ACT, individuals learn that negative emotions are parts of life, and thus not completely avoidable. Moreover, they understand that negative emotions do not necessarily entail actions.31
Previous studies have shown the effectiveness of ACT in treating cigarette smoking.5 For example, some studies investigated the efficacy of web-based or telephone-based of ACT in smokers. Their result showed the efficacy of ACT in these formats.34-36 Moreover, other studies have done in certain healthcare settings and on certain patient populations such as veterans with posttraumatic stress disorder.37,38 In other words, to the best of our knowledge, no study has yet evaluated the effects of this therapy on smokers who suffer from comorbid depression and anxiety symptoms. Consequently, we made this study to examine the effects of ACT on man smokers’ comorbid depression and anxiety symptoms and smoking cessation.
Methods
This randomized controlled trial was done using a two-group (pre- and post-test) design and with a six-week follow-up period.
Participants were randomly selected from man smokers who referred to Kargarnejad Teaching Psychiatric Hospital, Kashan, Iran, for receiving cessation-related services. Selection criteria were an age of 18-40 years, an educational degree of at least primary diploma, presence of nicotine dependence criteria according to the Diagnostic and Statistical Manual of Mental Disorders-4th Edition (DSM-IV), no comorbid psychiatric disorders except for depression and anxiety, no history of drug abuse and psychotic disorders, no history of receiving psychotherapies during the past six months, and a depression and an anxiety score of greater than 13 and 8, respectively. These scores are cut-off points which were used to diagnose depression and anxiety. Participants whose depression and anxiety were due to major life events (such as loss, marital conflicts, or divorce) were not included. On the other hand, participants were excluded if they were no longer willing to participate in ACT sessions, had two or more absences from the sessions, and received other medication or psychological therapies for cessation during the study.
In order to assess psychiatric disorders, depression, anxiety, and smoking cessation, we respectively used structural clinical interview (SCI) for DSM-IV disorders, Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), and micro Smokerlyzer carbon monoxide monitor.
SCI for DSM-IV disorders is a semi-structured interview used adjacent to the evaluator’s clinical judgment in order to establish psychiatric diagnosis based on DSM-IV. We used the Persian SCI in this study. The Persian version was cross-culturally adapted for the cultural context of Iran and reported to have a Kappa’s agreement coefficient of greater than 0.6 for most diagnoses.39
BDI is a 21-item inventory. Its items are scored from 0 to 3, yielding a total BDI score of 0 to 63. The cut-off scores of BDI are as follows: 0-9 for minimal depression, 10-18 for mild depression (the recommended cut-off point is 13), 19-29 for moderate depression, and 30-60 for severe depression. BDI is used for measuring depressed patients’ feedbacks and symptoms.40 The items of BDI had been developed mainly based on the common attitudes and symptoms of depressed patients. BDI score was reported to have a significant correlation with the scores of Hamilton depression rating scale (HDRS), ZUNG self-rating depression scale, Minnesota multiphasic personality inventory (MMPI), and Symptom checklist 90 (SCL-90) (r > 0.6), confirming its criterion validity. The test-retest correlation coefficient of BDI was 0.93. The Persian version of BDI was also reported to have acceptable validity and reliability.41
BAI is also a 21-item inventory, the items of which are scored on a Likert scale from 0 to 3. Each BAI item describes one of the most common subjective, somatic, or panic symptoms of anxiety. Total BAI score can range from 0 to 63. BAI cut-off scores are as follows: 0-7 for minimal anxiety, 8-15 for mild anxiety, 16-25 for moderate anxiety, and 26-63 for severe anxiety. The Cronbach’s alpha of the original and the Persian versions of BAI have been reported to be 0.8240 and 0.92,42 respectively. The high correlation of BAI score with the results of SCI for DSM-IV disorders (r = 0.73) also confirmed its acceptable criterion validity.42
Cigarette smoking or cessation status was assessed using micro Smokerlyzer carbon monoxide monitor (Bedfont® Scientific Ltd., Kent, England). Patients with an expiratory carbon monoxide level of 6 parts per million (PPM) were considered as smokers.43
Initially, all 119 patients who referred from March 5 to 10, 2017, to Kargarnejad Hospital for receiving cessation-related services were assessed by an addiction psychologist for eligibility criteria. In total, 93 men were eligible for the study, seventy of whom were randomly selected using a table of random numbers. Then, the patients were randomly and evenly allocated to an intervention and a control group. Before the intervention, all patients in both groups completed BDI and BAI. Then, patients in the intervention group received ACT, while their counterparts in the control group received psychological counseling services routinely provided to all patients in the study setting. Table 1 shows ACT content based on each session. Both interventions were implemented in eight ninety-minute one-to-one sessions. The sessions for the patients in the intervention group were held by a clinical psychologist who was a smoking cessation and ACT specialist. On the other hand, in the control group, the sessions were held by a clinical psychologist who was a smoking cessation and cognitive behavioral therapy specialist. Both psychologists held PhD degrees and were blind to the design and the methods of the study. Patients were also unaware of the presence of another intervention even though they had been provided with information about the aim of the study. Post-test and follow-up assessments were performed one and six weeks after the 8th session of interventions, respectively, using BDI, BAI, and Smokerlyzer. While pre-test assessments had been performed by the first author, post-test and follow-up assessments were performed by a psychologist who was external to the study. It is noteworthy that the Smokerlyzer machine could assess only one-week smoking status. Thus, we did not inform patients about the exact time of post-test and follow-up assessments in order not to make them avoid cigarette smoking during the last week before post-test and follow-up assessments.
Table 1.
The contents of the acceptance and commitment therapy (ACT) sessions
| Sessions | Contents |
|---|---|
| 1 | Building empathy-based rapport with clients to enhance their motivation, identifying internal and external factors behind lapse, making a therapeutic contract |
| 2 | Introducing creative hopelessness, assessing clients’ bad decisions and experiences in life, negotiating the reasons behind the ineffectiveness of other cessation-related therapies, explaining the effectiveness of ACT |
| 3 | Using metaphors to explain that the main problems of patients have been their excessive attempt to solve problems as well as their use of problem-solving strategies which were in contradiction with their feelings, thoughts, and emotions |
| 4 | Accepting self as a stable context in relation to the available experiences in order to reduce the effects of disturbing thoughts, training mindfulness, and exposure-based behavioral techniques in order to manage experiential avoidance |
| 5 and 6 | Exercising how to adapt to internal triggers, exploring clients’ values with respect to family, marriage, childrearing, friendship, job, education, recreation, spirituality, citizenship, and health, adjusting behaviors based on the identified values |
| 7 and 8 | Enhancing clients’ commitment to the therapeutic contract, discussing the action plan and clients’ probable problems |
ACT: Acceptance and commitment therapy
At the beginning of the study, informed consent was obtained from all participants. Moreover, all study instruments were anonymized using numerical codes. At the end of the study, ACT was also provided to the patients in the control group.
The SPSS software (version 11.5, SPSS Inc., Chicago, IL, USA) was used for data analysis and management. The data were described using descriptive statistics measures such as frequency, mean ± standard deviation (SD). Data analysis was performed through inferential statistics tests and techniques such as Pearson's chi-square test, Student's independent t-test and the repeated measures analysis of variance (MANOVA).
The current study was approved by the Ethics Committee of Kashan University of Medical Sciences, with an approval code of 95102, December 06, 2016 and is registered in the Iranian Registry of Clinical Trial with the IRCT2017011932057N1 code. Before implementing the intervention, participants were asked to fill out and sign the informed consent forms of this study.
Results
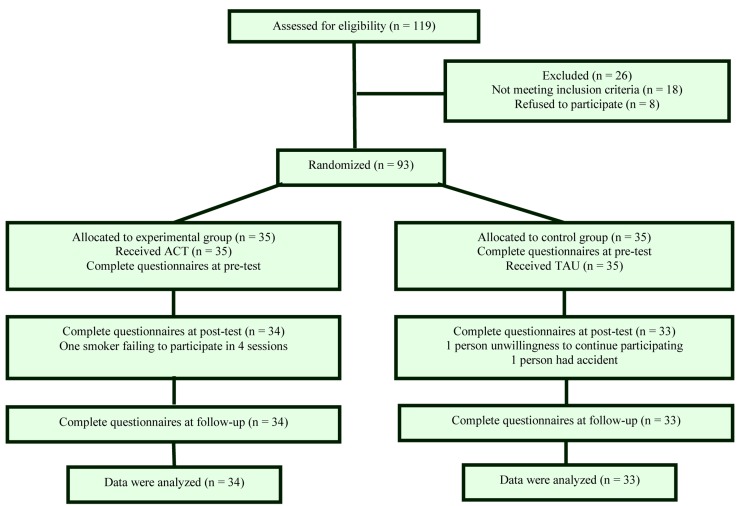
In total, two patients were excluded from the control group. One of them suffered a serious road accident and the other did not refer to the study setting because of an unknown reason. On the other hand, one patient was excluded from the intervention group due to having three absences from the ACT sessions. Therefore, final data analysis was performed on the data of 67 patients, 34 in the intervention and 33 in the control groups (Figure 1).
Figure 1.
Clinical trial flowchart ACT: Acceptance and commitment therapy; TAU: Treatment-As-Usual
Table 2 summarizes patients’ demographic characteristics. The mean values of patients’ age in the groups were 30.6 ± 5.3 and 29.4 ± 5.7 years, respectively. At baseline, there were no significant differences between the groups regarding patients’ age, marital and educational status, a number of cigars smoked daily, and a number of smoking years (P > 0.050) (Table 2).
Table 2.
Participants’ demographic characteristics
| Characteristics | Intervention (n = 34) | Control (n = 34) | P | |
|---|---|---|---|---|
| Age (year) (mean ± SD) | 29.4 ± 5.7 | 30.6 ± 5.3 | 0.366* | |
| Number of cigars smoked a day (mean ± SD) | 15.4 ± 3.6 | 16.1 ± 3.3 | 0.374* | |
| Number of smoking years (mean ± SD) | 7.6 ± 3.9 | 8.1 ± 4.2 | 0.615* | |
| Marital status [n (%)] | Married | 24 (70.6) | 22 (66.7) | 0.817** |
| Single | 9 (26.5) | 9 (27.3) | ||
| Other | 1 (2.9) | 2 (6.1) | ||
| Educational status [n (%)] | Primary diploma | 12 (35.3) | 13 (39.4) | 0.253** |
| Secondary diploma | 19 (55.9) | 13 (39.4) | ||
| University degree | 3 (8.8) | 7 (21.2) |
Student's independent t-test
Pearson's chi-square test
SD: Standard deviation
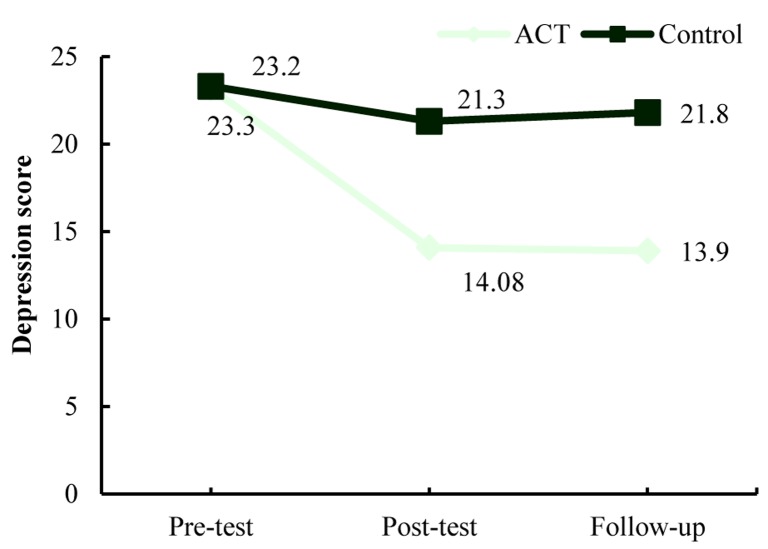
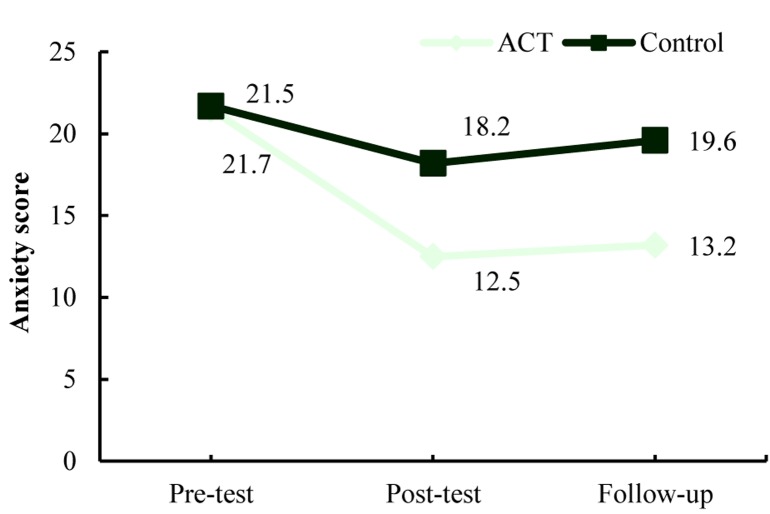
Table 3 shows the mean scores of depression and anxiety at three measurement time points in both study groups. At baseline, there were no significant differences between the groups respecting the mean scores of depression and anxiety (P > 0.050). However, the results of RM ANOVA illustrated significant between-group differences regarding the mean scores of depression and anxiety at post-test and follow-up time points (P < 0.001) (Table 3). The trends of depression and anxiety score variations are depicted in figures 2 and 3.
Table 3.
The mean scores of depression and anxiety in both study groups at different measurement time points
| Variable | Time point | P* | F | |||||
|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Follow-up | ||||||
| Intervention | Control | Intervention | Control | Intervention | Control | |||
| Depression (mean ± SD) | 23.0 ± 8.1 | 23.3 ± 9.6 | 14.1 ± 8.1 | 21.3 ± 9.6 | 13.9 ± 6.8 | 21.8 ± 8.8 | < 0.050 | 9.44 |
| Anxiety (mean ± SD) | 21.5 ± 8.7 | 21.7 ± 6.2 | 12.5 ± 5.9 | 18.2 ± 5.6 | 13.2 ± 5.6 | 19.1 ± 4.9 | < 0.050 | 7.43 |
Repeated-measures analysis of variance (MANOVA)
SD: Standard deviation
Figure 2.
The trends of depression score variations across three measurement time points ACT: Acceptance and commitment therapy
Figure 3.
The trends of anxiety score variations across three measurement time points ACT: Acceptance and commitment therapy
The results of the Pearson's chi-square test showed that at post-test, the number of patients in the intervention group who quitted smoking was significantly greater than the number in the control group (22 vs. 12, Pearson chi-square = 5.38, P < 0.050). The significant between-group difference regarding the number of clients who quitted smoking was also observed at follow-up (18 vs. 9, Pearson chi-square = 4.5, P < 0.050).
Discussion
This study compared 34 man smokers who received ACT with 33 man smokers who received routine counseling services in terms of depression, anxiety, and smoking cessation rate.
Results illustrated that ACT-treated smokers had significantly lower levels of depression and anxiety and higher smoking cessation rate compared with their counterparts who received routine counseling services. Most of the previous studies also reported the same findings. For instance, Jones et al. investigated the effects of web-based ACT on smokers who had depression symptoms and found a clinically significant difference between ACT and routine treatments in terms of their effects on depression symptoms. However, there was no statistically significant difference between these two treatments respecting smoking cessation rate.44 Kelly et al. also found ACT effective in improving depression and anxiety symptoms and smoking cessation rate significantly.38 Similarly, Vinci et al. found that mindfulness, a component of ACT, weakened the relationship between depression symptoms and cigarette smoking.45 In another study, Rogojanski et al. found mindfulness more effective than suppression in reducing negative effects, depression, and nicotine dependence.46 Other studies also reported the positive effects of group, telephone-based, and web-based ACT on smoking cessation.34,36,37
ACT alleviates anxiety states through giving people positive attitudes towards their feelings and thoughts. Negative emotions cause anxious people excessive repression. Mindfulness exercises of ACT induce creative hopelessness and challenge pathologic repressive strategies.33 It is noteworthy that a low level of anxiety is a normal part of life and is non-pathologic; hence, no treatment, even repressive strategies, can completely treat it forever. When individuals find repressive strategies ineffective in completely alleviating anxiety, they may become more anxious and erroneously attempt to repress anxiety states more seriously. This vicious cycle gradually makes them more and more anxious and frustrated. In order to circumvent this ineffective strategy, ACT introduces acceptance. Accepting negative feelings and emotions as normal parts of daily experiences reduces internal conflicts and guides individuals towards a value-based life. In fact, acceptance isolates individuals from anxiety-inducing mechanisms used for repressing feelings and thoughts. Of course, accepting such feelings does not mean approving all of them; rather, it means recognizing them and getting rid of emotion-based acting-out thoughts.47
Acceptance also helps depressed people experience unpleasant internal feelings without making any attempt to repress them. Accepting unpleasant experiences gradually decreases their effects on daily life. Contrarily, people believing that there are more reasons to be depressed have greater desire for ruminating thoughts and emotions in response to their depressed moods. Such ruminations are mostly associated with depressed people’s frequent attempts for finding the reasons behind their depression and hence, prevent them from learning and understanding the status quo. People who cannot find any clear reason for their depression blame themselves for past events and become hopeless about the future.48 Living in the present moment is another technique of ACT. Through this technique, individuals attempt to understand every moment of their lives through the moment-by-moment supervision of their own emotions, affects and thoughts. This technique contradicts depressed people’s ruminations about past or future. Another problem of depressed people is severe alterations in their self-esteem. The “self as a context” component of ACT teaches people that the supposition of being a weak person is not necessarily equal to be really weak. Moreover, it helps them understand that every person has some sorts of defects, while mere focus on defects and self-blaming can prevent people from finding solutions to their problems. ACT teaches people that the solution is value-based committed action for repairing defects, resolving problems, and improving quality of life.47
When used for smoking cessation, ACT teaches people to identify internal and external factors which trigger cigarette smoking. Then, it helps them accept emotional states (such as temptation and distress) related to non-smoking. Other treatments require individuals to repress cessation-related emotions; whereas, excessive repression can cause unpleasant emotional states such as distress, anxiety, and depressed mood. These states, in turn, propel individuals into cigarette smoking. While receiving ACT, people learn that such emotional states are not stable, and thus, instead of repressing, they can recognize and accept them. Such an acceptance helps them avoid rapid emotion-based acting-out and experience emotions without making any judgment. Such techniques prevent lapses. Acceptance is performed through metaphors and mindfulness exercises.5,36,37,49
Present study faced several limitations. First, we did not include women smokers in the study due to the very low prevalence of cigarette smoking among Iranian women.3 Second, the follow-up period in this study was six weeks. Long-term (three, six, and twelve-month) follow-up can produce more credible information about the effects of ACT on smoking cessation. Future studies are recommended to assess long-term cessation-related outcomes of ACT, the pure effects of each ACT component, and the correlation of different components of mindfulness with the commitment to cessation.
Conclusion
Study findings indicate that ACT is effective in improving comorbid depression and anxiety symptoms and smoking cessation rate. Thus, it can be used to simultaneously manage depression, anxiety, and cigarette smoking.
Acknowledgments
This study was approved and funded by the Deputy of Research of Kashan University of Medical Sciences, Iran. We wish to very thankful the Research Deputy of Kashan University of Medical Sciences for financially supporting this project. Moreover, authors are grateful to staffs of Kargarnejad Psychiatric Hospital.
Footnotes
Conflicts of Interest
The Authors have no conflict of interest.
REFERENCES
- 1.PDQ Screening and Prevention Editorial Board. Cigarette smoking: Health risks and how to quit (PDQ®) [Online]. 2017. Available from: URL: https://www.cancer.gov/about-cancer/causes-prevention/risk/tobacco/quit-smoking-hp-pdq.
- 2.World Health Organization. The tobacco atlas. 1st. Geneva, Switzerland: WHO; 2002. [Google Scholar]
- 3.Azizi F, Rahmani M, Emami H, Mirmiran P, Hajipour R, Madjid M, et al. Cardiovascular risk factors in an Iranian urban population: Tehran lipid and glucose study (phase 1). Soz Praventivmed. 2002;47(6):408–26. doi: 10.1007/s000380200008. [DOI] [PubMed] [Google Scholar]
- 4.Ng M, Freeman MK, Fleming TD, Robinson M, Dwyer-Lindgren L, Thomson B, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980-2012. JAMA. 2014;311(2):183–92. doi: 10.1001/jama.2013.284692. [DOI] [PubMed] [Google Scholar]
- 5.McCracken L. Mindfulness and acceptance in behavioral medicine: Current theory and practice. Oakland, CA: New Harbinger Publications; 2011. [Google Scholar]
- 6.Hatsukami DK, Stead LF, Gupta PC. Tobacco addiction. Lancet. 2008;371(9629):2027–38. doi: 10.1016/S0140-6736(08)60871-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ekpu VU, Brown AK. The economic impact of smoking and of reducing smoking prevalence: Review of evidence. Tob Use Insights. 2015;8:1–35. doi: 10.4137/TUI.S15628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sotiriou I, Chalkiadaki K, Nikolaidis C, Sidiropoulou K, Chatzaki E. Pharmacotherapy in smoking cessation: Corticotropin releasing factor receptors as emerging intervention targets. Neuropeptides. 2017;63:49–57. doi: 10.1016/j.npep.2017.02.082. [DOI] [PubMed] [Google Scholar]
- 9.Aubin HJ, Luquiens A, Berlin I. Pharmacotherapy for smoking cessation: pharmacological principles and clinical practice. Br J Clin Pharmacol. 2014;77(2):324–36. doi: 10.1111/bcp.12116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gifford EV, Kohlenberg BS, Hayes SC, Pierson HM, Piasecki MP, Antonuccio DO, et al. Does acceptance and relationship focused behavior therapy contribute to bupropion outcomes? A randomized controlled trial of functional analytic psychotherapy and acceptance and commitment therapy for smoking cessation. Behav Ther. 2011;42(4):700–15. doi: 10.1016/j.beth.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Killen JD, Fortmann SP, Schatzberg AF, Arredondo C, Murphy G, Hayward C, et al. Extended cognitive behavior therapy for cigarette smoking cessation. Addiction. 2008;103(8):1381–90. doi: 10.1111/j.1360-0443.2008.02273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roberts NJ, Kerr SM, Smith SM. Behavioral interventions associated with smoking cessation in the treatment of tobacco use. Health Serv Insights. 2013;6:79–85. doi: 10.4137/HSI.S11092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Midlarsky E, Pirutinsky S, Cohen F. Religion, ethnicity, and attitudes toward psychotherapy. J Relig Health. 2012;51(2):498–506. doi: 10.1007/s10943-012-9599-4. [DOI] [PubMed] [Google Scholar]
- 14.Sapp M. Basic psychological measurement, research designs, and statistics without math. Springfield, IL: Charles C. Thomas Publisher; 2006. [Google Scholar]
- 15.Kawai A, Kano M, Sato T. Motivational interviewing and cognitive behavior therapy for smoking cessation. Nihon Rinsho. 2013;71(3):493–8. [PubMed] [Google Scholar]
- 16.Nakamura M, Oshima A, Ohkura M, Arteaga C, Suwa K. Predictors of lapse and relapse to smoking in successful quitters in a varenicline post hoc analysis in Japanese smokers. Clin Ther. 2014;36(6):918–27. doi: 10.1016/j.clinthera.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 17.Kenford SL, Fiore MC, Jorenby DE, Smith SS, Wetter D, Baker TB. Predicting smoking cessation. Who will quit with and without the nicotine patch. JAMA. 1994;271(8):589–94. doi: 10.1001/jama.271.8.589. [DOI] [PubMed] [Google Scholar]
- 18.Zvolensky MJ, Gibson LE, Vujanovic AA, Gregor K, Bernstein A, Kahler C, et al. Impact of posttraumatic stress disorder on early smoking lapse and relapse during a self-guided quit attempt among community-recruited daily smokers. Nicotine Tob Res. 2008;10(8):1415–27. doi: 10.1080/14622200802238951. [DOI] [PubMed] [Google Scholar]
- 19.Kapson HS, Haaga DA. Depression vulnerability moderates the effects of cognitive behavior therapy in a randomized controlled trial for smoking cessation. Behav Ther. 2010;41(4):447–60. doi: 10.1016/j.beth.2009.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fluharty M, Taylor AE, Grabski M, Munafo MR. The association of cigarette smoking with depression and anxiety: A systematic review. Nicotine Tob Res. 2017;19(1):3–13. doi: 10.1093/ntr/ntw140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: within-subjects analysis of real-time reports. J Consult Clin Psychol. 1996;64(2):366–79. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- 22.Capron DW, Allan NP, Norr AM, Zvolensky MJ, Schmidt NB. The effect of successful and unsuccessful smoking cessation on short-term anxiety, depression, and suicidality. Addict Behav. 2014;39(4):782–8. doi: 10.1016/j.addbeh.2013.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hofmann SG. The Wiley handbook of cognitive behavioral therapy. Hoboken, NJ: Wiley; 2013. [Google Scholar]
- 24.Bland P. Smoking cessation improves anxiety depression. Practitioner. 2014;258(1769):5. [PubMed] [Google Scholar]
- 25.Correa-Fernandez V, Ji L, Castro Y, Heppner WL, Vidrine JI, Costello TJ, et al. Mediators of the association of major depressive syndrome and anxiety syndrome with postpartum smoking relapse. J Consult Clin Psychol. 2012;80(4):636–48. doi: 10.1037/a0027532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guichenez P, Guillaumin C. Cognitive behavior therapy in smoking cessation. Rev Mal Respir. 2008;25(10):1351–2. doi: 10.1016/s0761-8425(08)75107-6. [DOI] [PubMed] [Google Scholar]
- 27.Patten CA, Martin JE, Myers MG, Calfas KJ, Williams CD. Effectiveness of cognitive-behavioral therapy for smokers with histories of alcohol dependence and depression. J Stud Alcohol. 1998;59(3):327–35. doi: 10.15288/jsa.1998.59.327. [DOI] [PubMed] [Google Scholar]
- 28.Teasdale JD, Segal ZV, Williams JM, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J Consult Clin Psychol. 2000;68(4):615–23. doi: 10.1037//0022-006x.68.4.615. [DOI] [PubMed] [Google Scholar]
- 29.Cayoun BA. Mindfulness-integrated CBT: Principles and practice. Hoboken, NJ: Wiley; 2011. [Google Scholar]
- 30.Lau MA, McMain SF. Integrating mindfulness meditation with cognitive and behavioural therapies: the challenge of combining acceptance- and change-based strategies. Can J Psychiatry. 2005;50(13):863–9. doi: 10.1177/070674370505001310. [DOI] [PubMed] [Google Scholar]
- 31.Hayes SC, Strosahl KD. A Practical guide to acceptance and commitment therapy. New York, NY: Springer; 2004. [Google Scholar]
- 32.Saedy M, Kooshki S, Jamali FM, Emamipour S, Rezaei AA. Effectiveness of acceptance-commitment therapy on anxiety and depression among patients on methadone treatment: A pilot study. Iran J Psychiatry Behav Sci. 2015;9(1):e222. doi: 10.17795/ijpbs222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davison TE, Eppingstall B, Runci S, O'Connor DW. A pilot trial of acceptance and commitment therapy for symptoms of depression and anxiety in older adults residing in long-term care facilities. Aging Ment Health. 2017;21(7):766–73. doi: 10.1080/13607863.2016.1156051. [DOI] [PubMed] [Google Scholar]
- 34.Bricker JB, Copeland W, Mull KE, Zeng EY, Watson NL, Akioka KJ, et al. Single-arm trial of the second version of an acceptance and commitment therapy smartphone application for smoking cessation. Drug Alcohol Depend. 2017;170:37–42. doi: 10.1016/j.drugalcdep.2016.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bricker JB, Mann SL, Marek PM, Liu J, Peterson AV. Telephone-delivered acceptance and commitment therapy for adult smoking cessation: a feasibility study. Nicotine Tob Res. 2010;12(4):454–8. doi: 10.1093/ntr/ntq002. [DOI] [PubMed] [Google Scholar]
- 36.Mak YW, Lee PH, Loke AY. Predictors of participation in a telephone-based acceptance and commitment therapy for smoking cessation study. BMC Public Health. 2015;15:1288. doi: 10.1186/s12889-015-2650-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mak YW, Loke AY. The acceptance and commitment therapy for smoking cessation in the primary health care setting: A study protocol. BMC Public Health. 2015;15:105. doi: 10.1186/s12889-015-1485-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kelly MM, Sido H, Forsyth JP, Ziedonis DM, Kalman D, Cooney JL. Acceptance and commitment therapy smoking cessation treatment for veterans with posttraumatic stress disorder: a pilot study. J Dual Diagn. 2015;11(1):50–5. doi: 10.1080/15504263.2014.992201. [DOI] [PubMed] [Google Scholar]
- 39.Sharifi V, Asadi SM, Mohammadi MR, Amini H, Kaviani H, Semnani Y, et al. Structured clinical interview for DSM-IV (SCID): Persian translation and cultural adaptation. Iran J Psychiatry. 2007;2(1):46–8. [Google Scholar]
- 40.Wetherell JL, Gatz M. The Beck Anxiety Inventory in older adults with generalized anxiety disorder. J Psychopathol Behav Assess. 2005;27(1):17–24. [Google Scholar]
- 41.Azkhosh M. Application of mental assessments and clinical diagnostics. 3rd. Tehran, Iran: Ravan Publications; 2008. [Google Scholar]
- 42.Kaviani H, Mousavi AS. Psychometric properties of the Persian version of Beck Anxiety Inventory (BAI). Tehran Univ Med J. 2008;66(2):136. [Google Scholar]
- 43.Jarvis MJ, Russell MA, Saloojee Y. Expired air carbon monoxide: a simple breath test of tobacco smoke intake. Br Med J. 1980;281(6238):484–5. doi: 10.1136/bmj.281.6238.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jones HA, Heffner JL, Mercer L, Wyszynski CM, Vilardaga R, Bricker JB. Web-based acceptance and commitment therapy smoking cessation treatment for smokers with depressive symptoms. J Dual Diagn. 2015;11(1):56–62. doi: 10.1080/15504263.2014.992588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vinci C, Spears CA, Peltier MR, Copeland AL. Facets of mindfulness mediate the relationship between depressive symptoms and smoking behavior. Mindfulness (NY) 2016;7(6):1408–15. doi: 10.1007/s12671-016-0582-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rogojanski J, Vettese LC, Antony MM. Coping with cigarette cravings: Comparison of suppression versus mindfulness-based strategies. Mindfulness. 2011;2(1):14–26. [Google Scholar]
- 47.Eifert GH, Forsyth JP. Acceptance and commitment therapy for anxiety disorders: A practitioner's treatment guide to using mindfulness, acceptance, and values-based behavior change strategies. Oakland, CA: New Harbinger Publications; 2005. [Google Scholar]
- 48.Blackledge JT, Ciarrochi J, Deane FP. Acceptance and commitment therapy: Contemporary theory research and practice. Bowen Hills, Australia: Australian Academic Press; 2009. [Google Scholar]
- 49.De Groot F, Morrens M, Dom G. Acceptance and commitment therapy (ACT) and addiction: a literature review. Tijdschr Psychiatr. 2014;56(9):577–85. [PubMed] [Google Scholar]