Abstract
Objective:
Hazardous drinking in the armed forces is a significant problem. Alcohol use motivations, known risk factors for problem drinking, have been underexplored in this population. Our study extends knowledge about drinking motives among current and former U.S. service members and provides recommendations on their utility in identifying alcohol-related problems by examining the factor structure of multidimensional drinking motives and their association to alcohol use.
Method:
Post-9/11 separated service members and current reservists were recruited from 35 Oregon employers to participate in a workplace study of supervisor support. The resulting sample (N = 509; 84% male; mean age = 39) completed a baseline assessment, which included a comprehensive drinking motives assessment.
Results:
Drinkers comprised 88% of the sample, with a mean Alcohol Use Disorders Identification Test (AUDIT) score of 5.4 (SD = 4.6); 23.9% scored 8 or more. The four-factor structure of the Drinking Motives Questionnaire-Revised, short form (DMQ-R-SF) was affirmed through confirmatory factor analysis. Internal drinking motives related to enhancement (positive) and coping (negative) were most predictive of alcohol use; coping motives were uniquely predictive of alcohol-related problems, when drinking quantity/frequency, as well as psychological distress, were controlled for. Coping motives also mediate the relationship between psychological distress and AUDIT scores. Results thus demonstrated the generalizability of the DMQ-R-SF motives measure for use with separated service members and reservists.
Conclusions:
Drinking motives, assessed by the DMQ-R-SF, represent reliable and important predictors of drinking and associated problems among service members. Inclusion of motivated drinking questions may enhance screening for alcohol-related problems among current and former service members.
Hazardous alcohol use within the military has been well documented, even being referred to as a public health crisis (Institute of Medicine, 2012). Among National Guard/Reservists, 15% provided a positive response to at least one (of two) alcohol-screening indicator (Milliken et al., 2007). Twenty-six percent of reservists indicated that they relied on drinking as a stress-reduction strategy (Defense Manpower Data Center [DMDC], 2010). Among active duty service members, reported rates of heavy drinking (i.e., five or more drinks at least once per week over the past 30 days), as well as alcohol-related consequences, significantly increased from 1998 to 2008 (Bray et al., 2013).
The context of many military deployments in recent years likely plays a role; Jacobson et al. (2008) conducted a prospective study of veterans returning from deployments in Iraq and Afghanistan, revealing that service members who experienced combat exposure were significantly more likely to experience new-onset heavy weekly drinking and alcohol- related problems compared with the nondeployed same-era veterans. Younger service members who reported combat exposure during deployment were at additionally increased risk. Numerous studies show that the post-deployment period for returning veterans can be challenging. This time of transition is characterized by heightened emotional experiences (e.g., anger and hostility), heavy alcohol use, and increased risk-taking (DMDC, 2010; Killgore et al., 2008). Importantly, in longitudinal analyses, more than 40% of service members self-reported drinking more post-deployment (as compared with pre-deployment; DMDC, 2010).
Some veterans appear to be especially vulnerable to increased drinking following combat deployment. McDevitt- Murphy and colleagues (2015) found that among Operation Enduring Freedom/Operation Iraqi Freedom veterans who met the criteria for posttraumatic stress disorder (PTSD) and were identified as hazardous or problem drinkers on the Alcohol Use Disorders Identification Test (AUDIT; i.e., scores of 8 or more; Babor et al., 2001), there was stronger endorsement of drinking to cope with anxiety and depression compared with veterans who did not meet PTSD criteria. Similarly, coping motivations were associated with adverse alcohol consequences (McDevitt-Murphy et al., 2015). Such findings are consistent with previous work describing the developmental link between drinking-to-cope motivations and alcohol abuse (e.g., Cooper et al., 1995).
Coping motivation to consume alcohol has been described by multiple theoretical frameworks in terms of people’s desire to drink to alleviate tension (i.e., the Tension-Reduction Hypothesis; Conger, 1956; see review by Greeley & Oei, 1999) or more broadly to alleviate or escape unpleasant affective experiences (i.e., Self-Medication Hypothesis; Khantzian, 1985). Negative motivations include internally focused drinking to deal with negative experiences (i.e., coping motivation) and externally focused drinking to fit in and avoid social rejection (i.e., conformity motivation). Regarding positive motivations, individuals drink to enhance or prolong positive emotional experiences (i.e., enhancement motivation) and drink to have a good time with others socially (i.e., social motivation). Of note, coping motives have been uniquely predictive of alcohol-related problems among adults, when typical consumption (Cooper et al., 1992), negative affectivity (Cooper et al., 1995; Simons et al., 2005), and more severe forms of psychopathology (e.g., major depression; Young-Wolff et al., 2009) were controlled for.
However, more generally, we know little about motivations for alcohol consumption among military veterans. A handful of studies to date have assessed drinking motives in military personnel, although the link between motives and drinking (e.g., Whiteman & Barry, 2011; Williams et al., 2010), or coping styles and drinking (e.g., Norman et al., 2014), appears to be of growing interest. Yet, no studies of which we are aware have conducted an examination of the multidimensional factor structure of drinking motives and related them to drinking outcomes. Mash and colleagues (2014) administered a modified version of the Drinking Motives Questionnaire–Revised (DMQ-R; Cooper, 1994) with active duty military personnel. However, they did not conduct a confirmatory factor analysis (CFA), nor did they link responses to alcohol-related outcomes, particularly hazardous or problem-related drinking. Further, because the measure they used was modified, it is not comparable to other published samples. In particular, authors selected a subset of items from three of the four motive subscales, excluding enhancement motives; the items selected do not correspond to previously validated versions of the DMQ-R (e.g., DMQ short form [SF]). The exclusion of enhancement motives is unfortunate, as evidence from the studies noted above indicates that they may play an important role in predicting drinking outcomes for military-related individuals (e.g., McDevitt-Murphy et al., 2015; Whiteman & Barry, 2011).
Last, studies examining service members’ drinking motivations have mostly relied on clinical samples of individuals receiving treatment (e.g., McDevitt-Murphy et al., 2015; Simpson et al., 2014). There is much less known about the experiences of community-dwelling service members. We are not aware of any study that has included a diverse group of service members, including veterans and current reservists, in a study of drinking motives.
Present study
Our study aims to extend knowledge about drinking motives to a post-9/11 U.S.-separated service member and reservist sample. Veterans and reservists participating in the SERVe study (the Study for Employment Retention of Veterans) were recruited from organizations throughout Oregon to participate in a workplace study of supervisor support. They completed the 12-item DMQ-R-SF (Kuntsche & Kuntsche, 2009)—drawn from the longer DMQ-R (Cooper, 1994)—as part of a larger baseline assessment, along with questions related to drinking quantity/frequency and alcohol-related problems. We selected this inventory because it is well validated and frequently used in a variety of civilian populations.
Our first aim was to examine the factor structure of drinking motives in a sample of military veterans and service members. In Hypothesis 1, we predicted that the previously supported four-dimensional model of drinking motives would be affirmed in this population. Subsequently, our second aim was to examine mean levels of endorsement for each of the motives and relationships with related factors, such as deployment status. The third aim was to determine whether measuring drinking motives would be beneficial as a potential screening tool for identifying alcohol-related problems among veterans and reservists, beyond simply investigating level of consumption.
Because of the largely exploratory nature of the study, we refrained from positing specific hypotheses for all motives. However, given the aforementioned theory and research describing the relationship between coping motives and alcohol-related problems, in Hypothesis 2 we predicted that coping motives would uniquely relate to alcohol-related consequences, controlling for drinking quantity and frequency. Further, we considered the interrelationships among coping motives, psychological distress, and alcohol-related problems. We posited in Hypothesis 3 that coping motives would significantly contribute to alcohol-related problems when psychological distress symptoms were controlled for. In Hypothesis 4, we predicted that psychological distress would be related to alcohol outcomes indirectly through coping motives.
Method
Overview
Employers in the state of Oregon were invited to be randomized to the supervisor support training intervention condition or wait-list control condition. Once an employer agreed to participate, service member reservists and veterans within the organization were voluntarily recruited through emails distributed through their organization. Eligible participants included current active military serving in the Oregon National Guard or Reserve, or individuals separated from the military no earlier than September 2001 (heretofore referred to collectively as veterans for simplicity). Participants were required to work at least 20 hours per week at their organizations. Interested participants completed a brief eligibility screener; eligible participants were provided informed consent and received a link to the survey. Additional information about the study and sample is provided in Hammer et al. (2017).
Participants
Five hundred nine eligible veteran employees were recruited from 35 organizations to participate in the SERVe project. Of those 509 participants, 60 veterans (11.8%) indicated that they never drank and were therefore not administered the drinking motives questions. The drinking motives questions were not answered by one additional veteran, thus rendering a potential analysis sample of 448 participants. Veterans were mostly men (83.7%; i.e., “What is your gender?”), corresponding to the percentage of male service members (84.5%; U.S. Department of Defense, 2015). Most participants were also White (85%), which corresponds to the 2015 Oregon Census race statistics (87.6%), and were 38.7 years of age, on average (SD = 9.3). Seventy-seven percent were married or cohabiting for M = 11.5 years (SD = 8.1). The majority of participating veterans (70%) were parents, 82% of whom had M = 2 (SD = 0.9) dependent children living in the home at least 3 days/week.
Approximately 73% of veterans in the analysis sample were separated from the military for M = 6.3 years (SD = 3.5). In terms of military experience, 88% of veterans had been deployed for an average of 17 months since September 11, 2001; 82.7% of veterans were enlisted, and 17.3% were officers.
Measures and procedure
Participants were given approximately 2 weeks to complete an online survey of work-, family-, and health- related characteristics; the survey was hosted through Qual-trics©2013 (Provo, UT). Each participant received $25 in exchange for the baseline survey completion. Current study measures included the following: DMQ-R-SF, alcohol use, AUDIT, and psychological distress—all described below.
Drinking Motives Questionnaire.
The DMQ-R-SF (Kuntsche & Kuntsche, 2009) comprises 12 items (three items per factor) to assess the four-factor model of drinking motives. Participants reported how often they drank for each motive using a 5-point Likert-type scale (1 = almost never/never to 5 = almost always/always). Composite scores for each of the four drinking motives were computed by taking the average of each subscale: Coping (e.g., to forget about your problems), conformity (e.g., to fit in with a group you like), enhancement (e.g., because you like the feeling), and social (e.g., because it makes social gatherings more fun).
Alcohol use.
Participants reported how many alcoholic beverages they had on a typical day in the past 30 days (average drinks or quantity), as well as how many days they consumed alcohol (drinking days or frequency). Standard drinks were defined for participants in an accompanying graphic to aid their response (i.e., 12 oz. of regular beer, 8–9 oz. of malt liquor, 5 oz. of wine, and 1.5 oz. of distilled spirits; International Center for Alcohol Policies, 1988).
Alcohol Use Disorders Identification Test.
The 10-item AUDIT (Babor et al., 2001) was administered to assess alcohol-related problems. The AUDIT assesses quantity and frequency of consumption (e.g., how many drinks containing alcohol do you have on a typical day when you are drinking?), drinking behaviors (e.g., how often during the last year have you found that you were able to stop drinking once you had started?), as well as alcohol-related problems (e.g., have you or someone else been injured as a result of your drinking?) in the past year. Responses to each question are scored on a range from zero to four, with higher values indicating more hazardous consumption; the values are summed across the 10 items. Internal consistency for the measure in the present sample was α = .771. See Babor et al. (2001) for additional information.
Psychological distress.
The Kessler K-6 Questionnaire (Kessler et al., 2003) was administered. It is a six-item Likert-type standardized measure of nonspecific psychological distress, designed and validated to differentiate between serious and no serious mental illness (for full review, see Kessler et al., 2003). Items query emotional experiences over the past 30 days, for example, “How often did you feel nervous?” Responses to items are on a scale of 1 (none of the time) to 4 (most of the time). Internal consistency for the present sample was α = .898.
Data analysis
We conducted a CFA via MPlus Version 7.4 (Muthén & Muthén, 1998–2015), examining the proposed four-factor structure. Following other investigations of alcohol use motivation factor structure (e.g., Cooper et al., 1992; Kuntsche & Kuntsche, 2009), we considered alternative models in CFAs (i.e., one-, two-, or three-factor models) to determine if the four-factor model was the best-fitting model. Specifically, in addition to a one-factor model, we considered two-factor models in which negative (coping and conformity) and positive (social and enhancement) motives were modeled; alternately, internal (enhancement and coping) and external (social and conformity) motives were modeled. We also specified a three-factor model in which social and enhancement motives were combined into one positive factor.
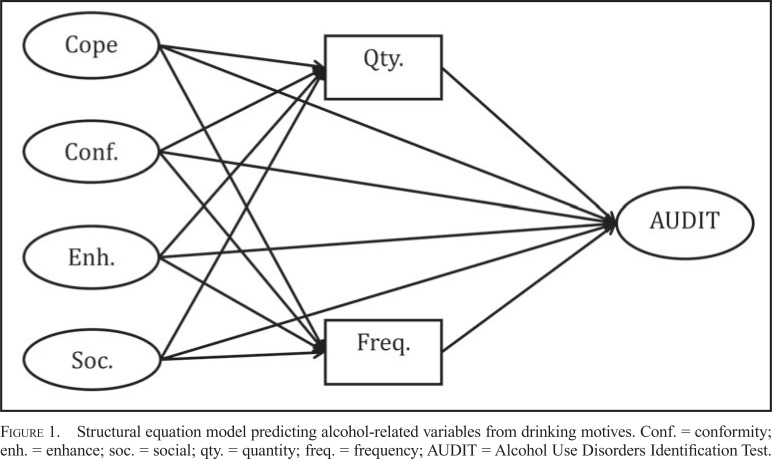
Once the factor structure of drinking motives was affirmed, we conducted structural equation modeling (SEM) analyses modeling AUDIT scores as a function of drinking motives in MPlus (Figure 1). Drinking quantity and frequency were also modeled as outcomes in separate analyses. Models were run using maximum likelihood estimation and bias-corrected bootstrapping with resampling (10,000) to account for nonnormality in alcohol outcomes and any missing data. We note that preliminary inspection of the data revealed an extreme outlying female veteran regarding drinking quantity and AUDIT score (i.e., 30), who uniquely contributed to a significant gender difference in some drinking variables; data from this individual were excluded from analyses. Further, based on inspection of correlations and previous research, we considered gender, military rank, age, and deployment status as potential covariates in SEM analyses. Covariates significantly predicted alcohol outcomes, except for age. The inclusion of age also reduced model fit, leading us to exclude it from covariates in our analyses. Last, for the SEM analyses, we recalculated AUDIT scores, excluding the three quantity/frequency drinking items (Questions 1–3) to address the predictor-criterion overlap that resulted from the inclusion of drinking quantity and frequency in the model predicting AUDIT scores.
Figure 1.
Structural equation model predicting alcohol-related variables from drinking motives. Conf. = conformity; enh. = enhance; soc. = social; qty. = quantity; freq. = frequency; AUDIT = Alcohol Use Disorders Identification Test.
Results
Sample descriptives
Mean AUDIT score for the sample was 5.340 (SD = 4.687), with 23.9% of the sample scoring 8 or more. Of those completing the AUDIT, 8.7% indicated that they did not consume alcohol in the previous 30 days. The average number of drinking days among recent drinkers ranged from 1 to 30 (of 30 days), with a mean of 9.642 (SD = 8.626). The average number of drinks per typical day was 2.125 (SD = 1.635) for veterans. We also considered whether gender differences were present among veterans in terms of drinking variables. No significant differences emerged for alcohol quantity/frequency or AUDIT scores.
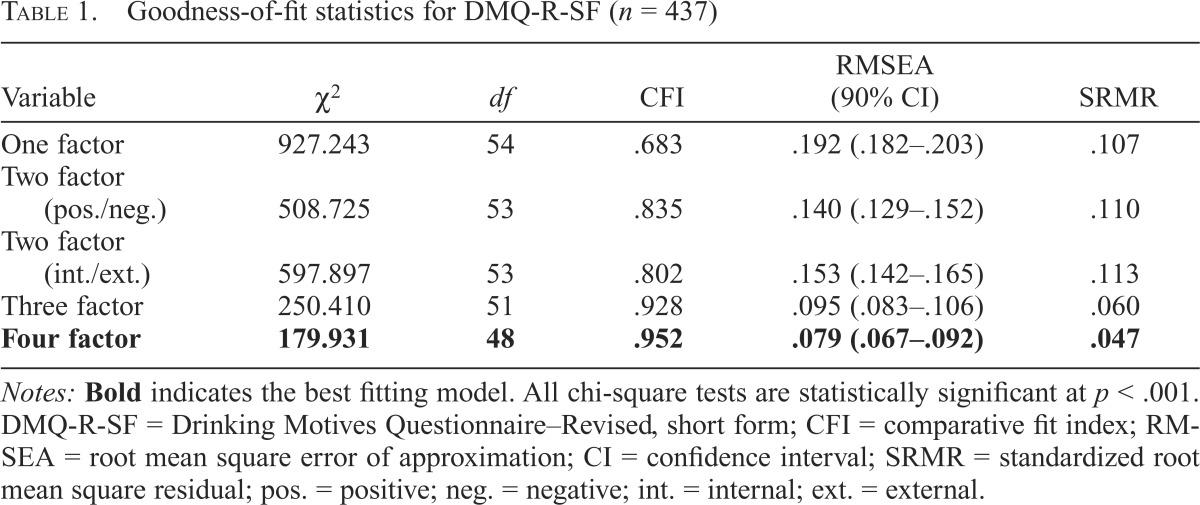
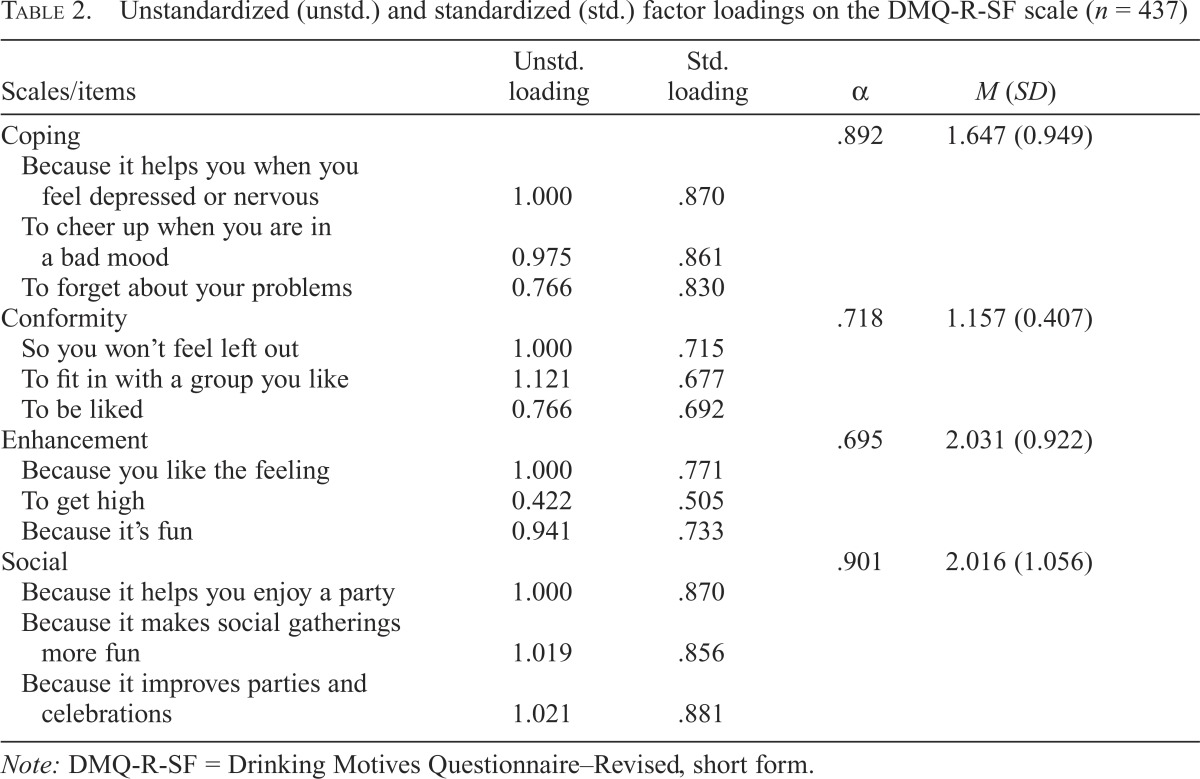
Confirmatory factor analysis
As shown in Table 1, the four-factor model was the best fitting model we tested, confirming Hypothesis 1. The three- factor model demonstrated a significant decrement in fit compared with the four-factor model, Δχ2(3) = 70.479, p < .001. All other models demonstrated poor model fit. Indeed, the four-factor model was the only one tested in which the upper confidence interval value for root mean square error of approximation (RMSEA) was below .10, allowing us to reject the poor-fit hypothesis (Kline, 2011). Factor loadings and subscale descriptive statistics of the four factors are provided in Table 2. Internal consistencies of each of the four factors were also investigated and revealed to be acceptable. Thus, CFA results support the four-factor structure of the DMQ-R-SF as the optimal choice for assessing drinking motives among veterans.
Table 1.
Goodness-of-fit statistics for DMQ-R-SF (n = 437)
| Variable | χ2 | df | CFI | RMSEA (90% CI) | SRMR |
| One factor | 927.243 | 54 | .683 | .192 (.182–.203) | .107 |
| Two factor (pos./neg.) | 508.725 | 53 | .835 | .140 (.129–.152) | .110 |
| Two factor (int./ext.) | 597.897 | 53 | .802 | .153 (.142–.165) | .113 |
| Three factor | 250.410 | 51 | .928 | .095 (.083–.106) | .060 |
| Four factor | 179.931 | 48 | .952 | .079 (.067–.092) | .047 |
Notes: Bold indicates the best fitting model. All chi-square tests are statistically significant at p < .001. DMQ-R-SF = Drinking Motives Questionnaire-Revised, short form; CFI = comparative fit index; RMSEA = root mean square error of approximation; CI = confidence interval; SRMR = standardized root mean square residual; pos. = positive; neg. = negative; int. = internal; ext. = external.
Table 2.
Unstandardized (unstd.) and standardized (std.) factor loadings on the DMQ-R-SF scale (n = 437)
| Scales/items | Unstd. loading | Std. loading | α | M (SD) |
| Coping | .892 | 1.647 (0.949) | ||
| Because it helps you when you feel depressed or nervous | 1.000 | .870 | ||
| To cheer up when you are in a bad mood | 0.975 | .861 | ||
| To forget about your problems | 0.766 | .830 | ||
| Conformity | .718 | 1.157 (0.407) | ||
| So you won’t feel left out | 1.000 | .715 | ||
| To fit in with a group you like | 1.121 | .677 | ||
| To be liked | 0.766 | .692 | ||
| Enhancement | .695 | 2.031 (0.922) | ||
| Because you like the feeling | 1.000 | .771 | ||
| To get high | 0.422 | .505 | ||
| Because it’s fun | 0.941 | .733 | ||
| Social | .901 | 2.016 (1.056) | ||
| Because it helps you enjoy a party | 1.000 | .870 | ||
| Because it makes social gatherings more fun | 1.019 | .856 | ||
| Because it improves parties and celebrations | 1.021 | .881 |
Note: DMQ-R-SF = Drinking Motives Questionnaire-Revised, short form.
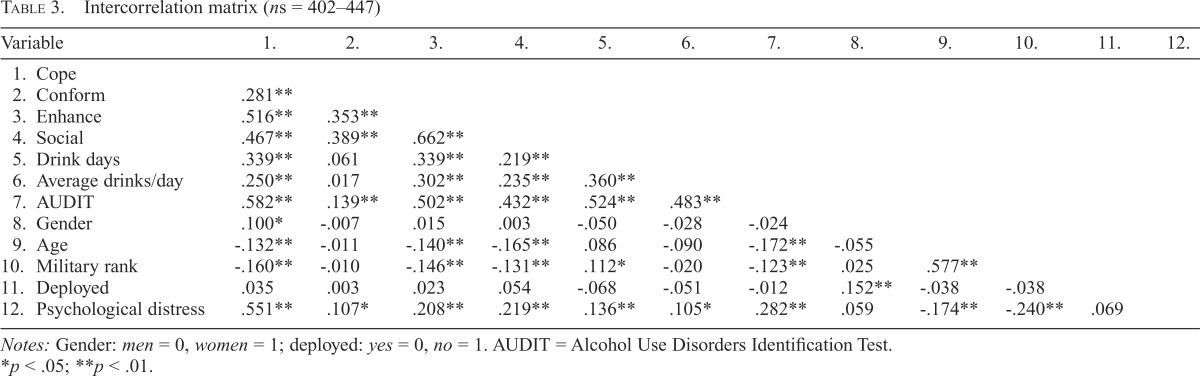
Frequency of motive endorsement
Consistent with other published reports of the DMQ-R-SF (e.g., Kuntsche et al., 2014), social and enhancement motives were the most strongly endorsed drinking motives, followed by coping and then conformity motives. In terms of gender, there were no significant relationships. Table 3 provides an intercorrelation matrix between drinking motives and related factors. Accordingly, age was significantly negatively correlated with three of the motives (cope, enhance, social) but not conformity motives. Age was also associated negatively with AUDIT scores. Experiencing either a domestic or international deployment (compared with never deploying) was not significantly correlated with alcohol-related variables. However, military rank (present or most recent) was inversely related to all motives, except conformity motives. Rank was also negatively related to AUDIT scores but positively related to drinking frequency. We also examined military status (active reservist, separated reservist vs. separated active duty) and found that it was unrelated to drinking motives or use variables. All drinking motives were significantly and positively correlated, with the strongest correlation between enhancement and social motives (r = .662, p < .01).
Table 3.
Intercorrelation matrix (ns = 402–447)
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. |
| 1. Cope | ||||||||||||
| 2. Conform | .281** | |||||||||||
| 3. Enhance | .516** | .353** | ||||||||||
| 4. Social | .467** | .389** | .662** | |||||||||
| 5. Drink days | .339** | .061 | .339** | .219** | ||||||||
| 6. Average drinks/day | .250** | .017 | .302** | .235** | .360** | |||||||
| 7. AUDIT | .582** | .139** | .502** | .432** | .524** | .483** | ||||||
| 8. Gender | .100* | -.007 | .015 | .003 | -.050 | -.028 | -.024 | |||||
| 9. Age | -.132** | -.011 | -.140** | -.165** | .086 | -.090 | -.172** | -.055 | ||||
| 10. Military rank | -.160** | -.010 | -.146** | -.131** | .112* | -.020 | -.123** | .025 | .577** | |||
| 11. Deployed | .035 | .003 | .023 | .054 | -.068 | -.051 | -.012 | .152** | -.038 | -.038 | ||
| 12. Psychological distress | .551** | .107* | .208** | .219** | .136** | .105* | .282** | .059 | -.174** | -.240** | .069 |
Notes: Gender: men = 0, women = 1; deployed: yes = 0, no = 1. AUDIT = Alcohol Use Disorders Identification Test.
p < .05;
p < .01
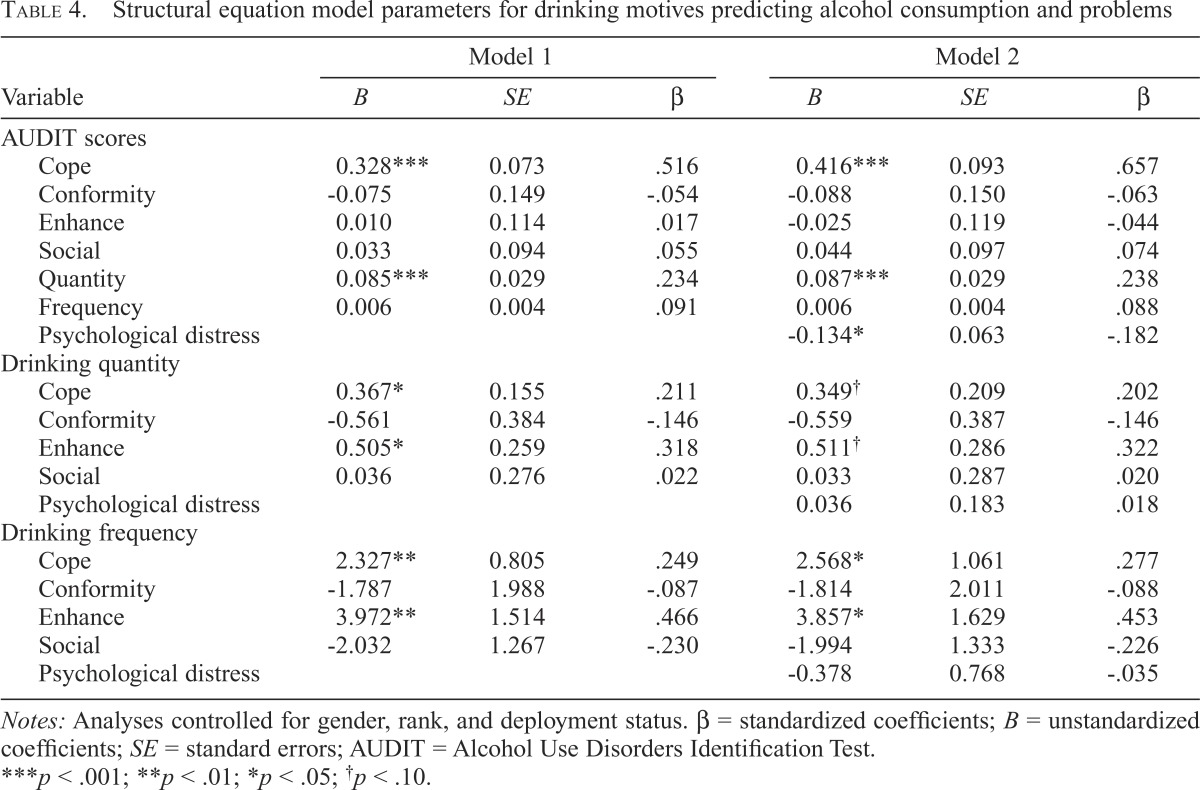
Associations with alcohol use
We modeled drinking quantity and frequency as a function of drinking motives, all of which were simultaneously modeled as a function of AUDIT scores (Figure 1). An inspection of model fit revealed an adequate-to-good fitting model (RMSEA = .056, 90% confidence interval [CI] = [.050, .062]; comparative fit index [CFI] = .918; standardized root mean square residual [SRMR] = .055). As shown in Table 4, enhancement and coping motives were both positively and significantly predictive of past-30-day quantity and frequency of consumption. Further, when quantity and frequency were controlled for, coping motives were uniquely and positively predictive of AUDIT scores, as specified in Hypothesis 2.
Table 4.
Structural equation model parameters for drinking motives predicting alcohol consumption and problems
| Variable | Model 1 |
Model 2 |
||||
| B | SE | β | B | SE | β | |
| AUDIT scores | ||||||
| Cope | 0.328*** | 0.073 | .516 | 0.416*** | 0.093 | .657 |
| Conformity | -0.075 | 0.149 | -.054 | -0.088 | 0.150 | -.063 |
| Enhance | 0.010 | 0.114 | .017 | -0.025 | 0.119 | -.044 |
| Social | 0.033 | 0.094 | .055 | 0.044 | 0.097 | .074 |
| Quantity | 0.085*** | 0.029 | .234 | 0.087*** | 0.029 | .238 |
| Frequency | 0.006 | 0.004 | .091 | 0.006 | 0.004 | .088 |
| Psychological distress | -0.134* | 0.063 | -.182 | |||
| Drinking quantity | ||||||
| Cope | 0.367* | 0.155 | .211 | 0.349† | 0.209 | .202 |
| Conformity | -0.561 | 0.384 | -.146 | -0.559 | 0.387 | -.146 |
| Enhance | 0.505* | 0.259 | .318 | 0.511† | 0.286 | .322 |
| Social | 0.036 | 0.276 | .022 | 0.033 | 0.287 | .020 |
| Psychological distress | 0.036 | 0.183 | .018 | |||
| Drinking frequency | ||||||
| Cope | 2.327** | 0.805 | .249 | 2.568* | 1.061 | .277 |
| Conformity | -1.787 | 1.988 | -.087 | -1.814 | 2.011 | -.088 |
| Enhance | 3.972** | 1.514 | .466 | 3.857* | 1.629 | .453 |
| Social | -2.032 | 1.267 | -.230 | -1.994 | 1.333 | -.226 |
| Psychological distress | -0.378 | 0.768 | -.035 | |||
Notes: Analyses controlled for gender, rank, and deployment status. β = standardized coefficients; B = unstandardized coefficients; SE = standard errors; AUDIT = Alcohol Use Disorders Identification Test.
p< .001;
p < .01;
p < .05;
p < .10.
Next, we considered the potential prediction of AUDIT scores when psychological distress was controlled for. We first modeled AUDIT scores as a function of drinking quantity and frequency and psychological distress but not motives (RMSEA = .067, 90% CI = [.060, .075]; CFI = .899; SRMR = .064). As anticipated, psychological distress significantly and positively predicted drinking quantity (B = 0.372, SE = 0.123; β = .184, p < .01), frequency (B = 1.714, SE = 0.563; β = .160, p < .01) and AUDIT scores (B = 0.137, SE = 0.046; β = .186, p < .01). We added the four drinking motive variables to the model, which resulted in an improved model fit (RMSEA = .054, 90% CI [.049, .059]; CFI = .915; SRMR = .058). As predicted in Hypothesis 3 (Table 4, Model 2), coping motives significantly predicted drinking frequency and AUDIT scores. When including coping motives in the model, psychological distress was no longer a significant predictor of drinking quantity or frequency and was inversely related to AUDIT scores.
Last, we reran our model including indirect pathways between psychological distress and alcohol variables through coping motives, calculating the indirect effects for each of 10,000 bootstrapped samples. Affirming Hypothesis 4, the bootstrapped unstandardized indirect effect between psychological distress and AUDIT scores was statistically significant (0.272, 95% CI [0.170, 0.411], p < .001). The bootstrapped unstandardized indirect effects were also statistically significant for drinking quantity (0.303, 95% CI [0.086, 0.536], p < .05) and drinking frequency (2.219, 95% CI [1.146, 3.418], p < .001). Results also revealed an indirect effect between coping motives and AUDIT via drinking quantity (B = 0.037, 95% CI [0.009, 0.090], p = .06).
Discussion
We investigated the utility of the multidimensional drinking motives questionnaire, DMQ-R-SF (Kuntsche & Kuntsche, 2009) to measure drinking motives among separated service members and current reservists. First, we evaluated model fit of the four-factor structure compared with alternative models. Second, we considered mean levels of motive endorsement, and correlations between motives and individual differences. Third, we examined the extent to which motives predicted alcohol outcomes, and whether coping motives uniquely predicted alcohol-related problems when drinking quantity and frequency were controlled for. Last, we determined whether coping motives predicted alcohol-related outcomes when psychological distress was controlled for and whether coping motives mediated the relationship between psychological distress and alcohol outcomes.
Results from CFAs support the four-factor structure of the DMQ-R-SF in this population, although some fit indices did not meet the criteria for a good-fitting model. Thus, marginal model fit for the four-factor CFA is a limitation of the current study. However, model fit was acceptable when predicting alcohol use outcomes. Indeed, despite high correlations between factors, we documented the predictive ability of drinking motives for understanding veteran drinking. In support of multidimensional models of alcohol use, coping-related motives were uniquely predictive of alcohol-related problems, beyond quantity and frequency of consumption, and psychological distress, thereby confirming Hypotheses 2 and 3. Thus, our study documented the value of considering drinking motives for understanding alcohol use and associated problems among veterans.
The two internal motives were most consistently predictive of drinking variables—that of enhancement and coping motives. One strength of our analysis was the inclusion of all four (positively correlated) drinking motives to determine the extent to which each uniquely predicted drinking-related outcomes. In terms of positive motivations, veterans’ drinking was more strongly associated with drinking “because they like the feeling” than with drinking “to enjoy a party.” Although social motives did not predict alcohol-related variables in our models, CFAs affirm the separation of social and enhancement motives as distinct drinking motives for veterans, although enhancement was more predictive of veteran drinking. Conversely, in terms of negative motivations, veterans’ drinking was more closely associated with drinking “to forget problems” than with “to fit in with others.” Conformity motives were the least endorsed and were not related to drinking variables in the study when other motives were controlled for. These trends parallel findings regarding drinking motives in civilian young adult and college student samples (e.g., Stewart et al., 2006).
We revealed that coping-related motives are an important factor associated with alcohol-related problems, consistent with the self-medication hypothesis (Khantzian, 1985), previous studies with the civilian population (Cooper et al., 1995), and historical accounts of soldiers drinking to alleviate combat-related stress (Jones & Fear, 2011). Also consistent with self-medication are relationships we revealed for psychological distress as a predictor of alcohol-related problems, and mediated relationships between distress and alcohol variables by coping motives. Yet, the coping items remained a significant predictor of alcohol-related problems in models, when alcohol use and psychological distress were controlled for. Therefore, psychological symptoms do not fully account for the relationship between motives and alcohol-related variables. Thus, the endorsement of drinking- to-cope carries with it additional risk; consequently, coping motives are valuable to consider as a screening tool for alcohol-related problems in military contexts, along with drinking quantity/frequency.
For those endorsing coping motives, it may be particularly important to strengthen coping skills, as they are explicitly relying on drinking to manage stress or discomfort. Norman and colleagues (2014) suggest that the efficacy of coping-related interventions in reducing alcohol use can be strengthened through the inclusion of factors related to avoidant coping. Although Norman and colleagues recommended targeting alcohol use expectancies, alcohol use motivations may be a similarly beneficial target as motives are shown to be a more proximal predictor of alcohol use and problems (Cox & Klinger, 1988). There is also recent attention to the importance of delivering cognitive behavioral therapy designed to enhance coping with symptomatology and alcohol use disorders simultaneously as the best way to reduce problematic drinking (Hien et al., 2015).
Regarding alcohol-related problems, the veterans in our sample demonstrated a relatively high percentage of heavy drinking, with 23.9% of the sample scoring 8 or more on the AUDIT. This compares to a rate of 10.8% in a sample of primary care patients (including some veterans seen at a VA clinic; Gordon et al., 2001). What is noteworthy about this estimate is that our sample was gleaned from mostly full-time employees in the community who were recruited through their workplaces, indicating relatively high levels of functioning. This suggests that there are unrecognized or undiagnosed alcohol-related problems in community members for whom support for reducing drinking would be important.
Another area of potential concern identified in our investigation was the relatively high levels of consumption in the female veteran population. Male and female veterans were not significantly different in their drinking behaviors in our sample. Follow-up analyses revealed that 27.8% of veteran men and 51.5% of veteran women have typical drinking levels that exceed U.S. Department of Health and Human Services (2015) recommended daily levels (i.e., one standard drink per day for women/two for men). Veteran women may be at particular risk for developing alcohol-related problems and should be a focus of screening efforts. Yet, we caution that the gender imbalance in our study and in the armed services more generally (U.S. Department of Defense, 2015) significantly reduces power to detect gender differences in drinking, motives, and the interrelationships among them. Additional research is necessary to further explore gender as a factor in motivated consumption among veterans, studies in which female veterans are oversampled.
In terms of other individual differences, we note that separated active duty service members were similar in drinking behavior to current and separated reservists. Military rank, however, was related to drinking, such that those with higher rank or pay grade engaged in less drinking. Our study did not detect significant relationships with deployment status in bivariate correlations, although in SEM models, we revealed that those who were never deployed report a lower quantity of consumption (B = -3.159, SE = 1.051; β = -.115, p < .01), consistent with previous research showing that deployment is a risk factor for increased drinking frequency and higher AUDIT scores (Bray et al., 2013; Jacobson et al., 2008; Milliken et al., 2007). Yet, the majority of our participants (88%) had deployed, leaving little variability in that dimension to enable detection of differences (although deployments in the sample included domestic and international deployments and not necessarily combat).
Conclusions
Our results supported the benefits of examining the drinking motives of military veterans and reservists. The proposed four-factor drinking motives structure was affirmed through CFA of the DMQ-R-SF. Of note, the internal drinking motives related to enhancement and coping were the most predictive of alcohol use, with coping motives being uniquely predictive of alcohol-related problems, when alcohol use and psychological distress were controlled for. Our investigation sheds light on a constellation of factors that place separated active duty and current reservists at risk for alcohol-related problems.
Footnotes
The U.S. Army Medical Research Acquisition Activity, 820 Chandler Street, Fort Detrick MD 21702-5014, is the awarding and administering acquisition office. This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs, through the USAMRMC Broad Agency Announcement under Award No. W81XWH-13-2-0020. Portions of this research were supported by the Grant # T03OH008435. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense. Special thanks go to Alicia Starkey, Todd Bodner and Anne Marie Greenhalgh for their assistance with the paper.
References
- Babor T. F., Higgins-Biddle J. C., Saunders J. B., Monteiro M. G. Geneva, Switzerland: World Health Organization; 2001. AUDIT: The Alcohol Use Disorders Identification Test. [Google Scholar]
- Bray R. M., Brown J. M., Williams J. Trends in binge and heavy drinking, alcohol-related problems, and combat exposure in the U.S. military. Substance Use & Misuse. 2013;48:799–810. doi: 10.3109/10826084.2013.796990. doi:10.3109/10826084.2013.796990. [DOI] [PubMed] [Google Scholar]
- Conger J. J. Alcoholism: Theory, problem and challenge. II. Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol. 1956;17:296–305. [PubMed] [Google Scholar]
- Cooper M. L. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6:117–128. doi:10.1037/1040-3590.6.2.117. [Google Scholar]
- Cooper M. L., Frone M. R., Russell M., Mudar P. Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology. 1995;69:990–1005. doi: 10.1037//0022-3514.69.5.990. doi:10.1037/0022-3514.69.5.990. [DOI] [PubMed] [Google Scholar]
- Cooper M. L., Russell M., Skinner J. B., Windle M. Development and validation of a three-dimensional measure of drinking motives. Psychological Assessment. 1992;4:123–132. doi:10.1037/1040-3590.4.2.123. [Google Scholar]
- Cox W. M., Klinger E. A motivational model of alcohol use. Journal of Abnormal Psychology. 1988;97:168–180. doi: 10.1037//0021-843x.97.2.168. doi:10.1037/0021-843X.97.2.168. [DOI] [PubMed] [Google Scholar]
- Defense Manpower Data Center. June 2009 status of forces survey of reserve component members: Family life briefing (unpublished report) 2010 (DMDC, Note N. 2010-013) [Google Scholar]
- Gordon A. J., Maisto S. A., McNeil M., Kraemer K. L., Conigliaro R. L., Kelley M. E., Conigliaro J. Three questions can detect hazardous drinkers. Journal of Family Practice. 2001;50:313–320. [PubMed] [Google Scholar]
- Greeley J., Oei T. Alcohol and tension reduction. Psychological Theories of Drinking and Alcoholism. 1999;2:14–53. [Google Scholar]
- Hammer L. B., Wan W. H., Brockwood K. J., Mohr C. D., Carlson K. F. Military, work, and health characteristics of separated and active service members from the Study for Employment Retention of Veterans (SERVe) Military Psychology. 2017 Advance online publication. doi:10.1037/mil0000196. [Google Scholar]
- Hien D. A., Levin F. R., Ruglass L. M., López-Castro T., Papini S., Hu M. -C., Herron A. Combining seeking safety with sertraline for PTSD and alcohol use disorders: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2015;83:359–369. doi: 10.1037/a0038719. doi:10.1037/a0038719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Center for Alcohol Policies (ICAP) 1998What is a standard drink? (ICAP Report 5). Washington DC: Author [Google Scholar]
- Institute of Medicine. Washington, DC: The National Academies Press; 2012. Substance use disorders in the US. armed forces. [PubMed] [Google Scholar]
- Jacobson I. G., Ryan M. A. K., Hooper T. I., Smith T. C., Amoroso P. J., Boyko E. J., Bell N. S. Alcohol use and alcohol-related problems before and after military combat deployment. JAMA. 2008;300:663–675. doi: 10.1001/jama.300.6.663. doi:10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones E., Fear N. T. Alcohol use and misuse within the military: A review. International Review of Psychiatry. 2011;23:166–172. doi: 10.3109/09540261.2010.550868. doi:10.3109/09540261.2010.550868. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Barker P. R., Colpe L. J., Epstein J. F., Gfroerer J. C., Hiripi E., Zaslavsky A. M. Screening for serious mental illness in the general population. Archives of General Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. doi:10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- Khantzian E. J. The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Journal of Psychiatry. 1985;142:1259–1264. doi: 10.1176/ajp.142.11.1259. doi:10.1176/ajp.142.11.1259. [DOI] [PubMed] [Google Scholar]
- Killgore W. D., Cotting D. I., Thomas J. L., Cox A. L., McGurk D., Vo A. H., Hoge C. W. Post-combat invincibility: Violent combat experiences are associated with increased risk-taking propensity following deployment. Journal of Psychiatric Research. 2008;42:1112–1121. doi: 10.1016/j.jpsychires.2008.01.001. doi:10.1016/j.jpsychires.2008.01.001. [DOI] [PubMed] [Google Scholar]
- Kline R. 3rd ed. New York, NY: Guilford Press; 2011. Principles and practice of structural equation modeling. [Google Scholar]
- Kuntsche E., Kuntsche S. Development and validation of the Drinking Motive Questionnaire Revised Short Form (DMQ-R SF) Journal of Clinical Child and Adolescent Psychology. 2009;38:899–908. doi: 10.1080/15374410903258967. doi:10.1080/15374410903258967. [DOI] [PubMed] [Google Scholar]
- Kuntsche E., Gabhainn S. N., Roberts C., Windlin B., Vieno A., Bendtsen P., Wicki M. Drinking motives and links to alcohol use in 13 European countries. Journal of Studies on Alcohol and Drugs. 2014;75:428–437. doi: 10.15288/jsad.2014.75.428. doi:10.15288/jsad.2014.75.428. [DOI] [PubMed] [Google Scholar]
- Mash H. B. H., Fullerton C. S., Ng T. H. H., Ursano R. J. Factor analysis of the Drinking Motives Questionnaire in a young adult U.S. Army sample. Psychological Reports: Disability & Trauma. 2014;115:339–350. doi: 10.2466/18.PR0.115c21z6. doi:10.2466/18.PR0.115c21z6. [DOI] [PubMed] [Google Scholar]
- McDevitt-Murphy M. E., Fields J. A., Monahan C. J., Bracken K. L. Drinking motives among heavy-drinking veterans with and without posttraumatic stress disorder. Addiction Research and Theory. 2015;23:148–155. doi: 10.3109/16066359.2014.949696. doi:10.3109/16066359.2014.949696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milliken C. S., Auchterlonie J. L., Hoge C. W. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. doi:10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. 7th ed. Los Angeles, CA: Authors; 1998–2015. Mplus user's guide. [Google Scholar]
- Norman S. B., Schmied E., Larson G. E. Predictors of continued problem drinking and substance use following military discharge. Journal of Studies on Alcohol and Drugs. 2014;75:557–566. doi: 10.15288/jsad.2014.75.557. doi:10.15288/jsad.2014.75.557. [DOI] [PubMed] [Google Scholar]
- Simpson T. L., Stappenbeck C. A., Luterek J. A., Lehavot K., Kaysen D. L. Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology. 2014;123:237–247. doi: 10.1037/a0035193. doi:10.1037/a0035193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons J. S., Gaher R. M., Correia C. J., Hansen C. L., Christopher M. S. An affective-motivational model of marijuana and alcohol problems among college students. Psychology of Addictive Behaviors. 2005;19:326–334. doi: 10.1037/0893-164X.19.3.326. doi:10.1037/0893-164X.19.3.326. [DOI] [PubMed] [Google Scholar]
- Stewart S. H., Morris E., Mellings T., Komar J. Relations of social anxiety variables to drinking motives, drinking quantity and frequency, and alcohol-related problems in undergraduates. Journal of Mental Health. 2006;15:671–682. doi:10.1080/09638230600998904. [Google Scholar]
- U.S. Department of Defense. Washington, DC: Author; 2015. Demographics report: Profile of the military. [Google Scholar]
- U.S. Department of Health and Human Services. 2015-2020 Dietary guidelines for Americans. 2015 Retrieved from https://health.gov/dietaryguidelines/2015/
- Whiteman S. D., Barry A. E. A comparative analysis of student service member/veteran and civilian student drinking motives. Journal of Student Affairs Research and Practice. 2011;48:297–313. doi: 10.2202/1949-6605.6322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J., Jones S. B., Pemberton M. R., Bray R. M., Brown J. M., Vandermaas-Peeler R. Measurement invariance of alcohol use motivations in junior military personnel at risk for depression or anxiety. Addictive Behaviors. 2010;35:444–451. doi: 10.1016/j.addbeh.2009.12.012. doi:10.1016/j.addbeh.2009.12.012. [DOI] [PubMed] [Google Scholar]
- Young-Wolff K. C., Kendler K. S., Sintov N. D., Prescott C. A. Mood-related drinking motives mediate the familial association between major depression and alcohol dependence. Alcoholism: Clinical and Experimental Research. 2009;33:1476–1486. doi: 10.1111/j.1530-0277.2009.00978.x. doi:10.1111/j.1530-0277.2009.00978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]