Abstract
Depression is associated with subjective difficulties identifying one’s emotions, known as low emotional clarity, but the mediators and moderators of this relationship are not well understood. We hypothesized that the role of emotional clarity in emotion regulation and, in turn, depression depends on individual differences in negative affect intensity. In Study 1, conducted in an unselected sample (N=119), low emotional clarity more strongly predicted depression symptoms among individuals higher in affect intensity. In Study 2, conducted in a clinically diagnosed, treatment-seeking sample (N=245), we examined whether affect intensity moderated an indirect path of clarity through emotion regulation strategy use that has emerged in previous work. When affect intensity was very low, emotional clarity did not predict reappraisal, and when affect intensity was very high, emotional clarity did not predict non-acceptance or experiential avoidance. By contrast, rumination mediated associations of emotional clarity with depressive symptoms regardless of affect intensity. Findings support a process model of low emotional clarity in depression that integrates (1) emotion regulatory mediators and (2) moderation by negative affect intensity. Trait differences in affect intensity may determine whether and how emotional clarity and regulation processes factor into mood psychopathology.
Keywords: emotional clarity, emotion awareness, depression, affect intensity, emotion regulation
A key psychological ability supporting mental health is the ability to identify the emotions one feels. One particular index of this ability that has been robustly implicated in mental health is emotional clarity, or the subjective perception of being able to identify which emotions one feels with relative ease (Salovey, Mayer, Goldman, Turvey, & Palfai, 1995). Low emotional clarity has been repeatedly associated with symptoms of depression (Ehring, Fischer, Schnülle, Bösterling, & Tuschen-Caffier, 2008; Flynn & Rudolph, 2014; Kennedy et al., 2010; Lee & Guajardo, 2011; Salguero, Extremera, & Fernández-Berrocal, 2013; Stange, Alloy, Flynn, & Abramson, 2013; Vine & Aldao, 2014). However, the precise nature of this relationship is less clear. Specifically, the mechanisms by which emotional clarity relates to depression severity (e.g., Flynn & Rudolph, 2010, 2014; Vine & Aldao, 2014), and the moderators of these effects (e.g., Kennedy et al., 2010; Stange et al., 2013), are only beginning to be examined. Especially necessary are models integrating both mediators and moderators that co-determine relationships among emotional processes and symptomatology. Such models would better explain the diversity of clinical presentations associated with transdiagnostic emotional deficits and assist in tailoring treatments (Aldao, 2013; Nolen-Hoeksema & Watkins, 2011). To our knowledge, such integrated models of emotional clarity have not yet been proposed or examined. As a result, it is not yet known precisely why difficulties identifying emotions are problematic and represent targets for intervention, nor when or for whom they are important.
Below, we briefly review existing findings associating low emotional clarity with depression, discuss proposed emotion regulatory mediators of this relationship, and present the rationale for examining moderators of these relationships. Finally, we propose trait affect intensity as a likely moderator of the role of emotional clarity in emotion regulation and depression symptoms, and test this prediction in two studies.
Low Emotional Clarity and Depression
Mounting evidence indicates that individuals with depression tend to experience their emotions with a low degree of clarity. In cross-sectional studies, low self-reported emotional clarity has been correlated with depressive symptoms in college students (Lee & Guajardo, 2011) and children (Flynn & Rudolph, 2010). Case-control studies show a similar pattern: dysphoric adolescents report lower emotional clarity than their nondysphoric peers (Fernandez-Berrocal, Alcaide, Extremera, & Pizarro, 2006), and adults with remitted depression report lower emotional clarity compared to never-depressed adults (Ehring et al., 2008). Low emotional clarity has also been associated with the development of depression symptoms prospectively (Flynn & Rudolph, 2014; Kennedy et al., 2010; Salguero et al., 2013; Stange, et al., 2013), suggesting that difficulties understanding emotions may play a role in the etiology of depression.
Emotion Regulation as a Possible Mediator
If low emotional clarity plays a meaningful role in depression, why might this be? One potential mechanism is emotion regulation, which refers to the processes by which individuals modulate the type, intensity, valence, or duration of emotional experiences (Gross, 1998). Emotion regulatory deficits are so reliably linked with deficits in emotional clarity that numerous theorists consider emotional clarity to be a critical first step toward regulating emotions (Gratz & Roemer, 2004; Mennin, Holaway, Fresco, Moore, & Heimberg, 2007; Salovey et al., 1995). Broadly, the logic of this hypothesis is that clearly perceiving and understanding a problem (including an emotion that needs regulating) should help solve that problem. For instance, knowing what one is feeling may help by providing information about how best to respond to the situation (Barrett & Gross, 2001), or because it frees up cognitive resources that can be devoted to the task of regulating emotions (e.g., Lischetzke & Eid, 2003).
This possible emotion regulatory function of emotional clarity may have strong relevance to depression, which is increasingly conceptualized as a disorder of emotion regulation (e.g., Ehring et al., 2008; Hofmann, Sawyer, Fang, & Asnaani, 2012). Depressed individuals experience excessive negative affect and reduced positive affect (e.g., Watson, Clark, & Carey, 1988), irregular stress reactivity (e.g., Gotlib, Joormann, Minor, & Hallmayer, 2008) and abnormal physiological responding to emotional cues (e.g., Sloan & Sandt, 2010), and they tend to use maladaptive regulation strategies in response to emotional challenges (e.g., Aldao, Nolen-Hoeksema, & Schweizer, 2010; Berking et al., 2014; Joormann & Vanderlind, 2014). However, only a few recent studies have tested the hypothesis that emotion regulation deficits mediate the relationship between low emotional clarity and depression severity, and those that have focused exclusively on rumination-like approaches to emotion regulation.
Rumination, a repetitive, negative, and self-focused thought process most closely linked with depression (Nolen-Hoeksema, 1991), has more recently become viewed as a maladaptive style of regulating emotions with implications for multiple disorders (e.g., Aldao et al., 2010). In a cross-sectional sample, low emotional clarity was linked with depressive symptoms by an indirect path through self-reported tendency to ruminate (Salguero et al., 2013). Two other groups have found similar patterns using variables functionally similar to rumination. Vine and Aldao (2014) showed that difficulties in emotion regulation statistically mediate the relationship of low emotional clarity with five forms of psychopathology; in depression, however, the primary mediator was self-reported difficulty disengaging attention from irrelevant stimuli (a key component of rumination). Similarly, Flynn and Rudolph have shown cross-sectionally (2010) and longitudinally (2014) that the relationship between low emotional clarity and depression symptom severity is mediated by a tendency to respond to interpersonal stressors by using more passive and ruminative coping. Thus, although some evidence is emerging for rumination as a mediator of the low clarity-depression relationship, it is not yet known whether the same can be said of many other strategies people frequently employ (e.g., cognitive reappraisal, emotional avoidance).
Moderating Effects of Context: Considering the Role of Negative Affect Intensity
Contemporary emotion regulation theorists have pointed out that the processes of identifying and regulating emotions necessarily play out within the context of other aspects of emotion experience, such as meta-emotional beliefs (e.g., Hofmann et al., 2012) or emotion intensity (e.g., Aldao, 2013). As such, there is a mandate for studies of emotion regulation and related processes to better account for the role of such moderators, including individual differences in other affective dimensions (e.g., Aldao, 2013; Aldao, Sheppes, & Gross, 2015; Kashdan & Rottenberg, 2010; Nolen-Hoeksema & Watkins, 2011). Applied to emotional clarity, a contextual lens raises the question of whether the adaptive value of identifying emotions varies from person to person. Despite its overall disadvantageousness, low emotional clarity may be more problematic for some people than for others. Indeed, the magnitude of the relationship between low emotional clarity and depression has been inconsistent, ranging from relatively small (e.g., Salguero et al., 2013) to relatively large (e.g., Vine & Aldao, 2014). This suggests that the degree of depression risk associated with low clarity depends on other variables, a possibility indirectly supported by initial tests of moderation in other clinical domains. For instance, low emotional clarity appears to differentially predict rumination in unselected adults depending on their ability to tolerate ambiguity (Vine, Aldao, & Nolen-Hoeksema, 2014). And low emotional clarity has been differentially associated with posttraumatic stress disorder severity among military veterans depending on their use of cognitive reappraisal to regulate emotions (Boden et al., 2012).
If indeed emotional clarity plays a role in responding to regulatory demands, and in turn, affects depression, clarity would be especially important among individuals who experience greater regulatory demands. Studies examining external stressors as a moderator of emotional clarity effects are suggestive. For instance, physical pain and perceived stress moderate the relationship between emotional clarity and depression, such that low emotional clarity is more strongly related to depression outcomes when levels of these adversities are high (Kennedy et al., 2010; Stange et al., 2013). It appears possible that intense situational contexts essentially raise the mental health stakes of perceiving clearly how one feels.
In the present investigation, we reason that high levels of subjective affect intensity might similarly moderate the relevance of emotion clarity to depressive symptoms. Much like the situational adversities of pain or stress, intense internal experiences might also heighten the importance of being able to identify one’s feelings. Affect intensity is a stable individual difference characteristic referring to the typical strength with which people subjectively experience emotions (Larsen & Diener, 1987). People who experience negative emotions intensely may need to rely more heavily on their ability to understand emotions in order to minimize distress, and may be more impaired if they are not able to achieve emotional clarity. Lower affect intensity, by contrast, may present lower regulatory demands and fewer challenges to adaptive psychological functioning, leaving little room for emotional clarity to be of benefit (or for low clarity to be a vulnerability).
Some evidence already suggests that the combination of low emotional clarity with high affect intensity may increase vulnerability to negative outcomes. Gohm and colleagues (Gohm 2003; Gohm & Clore, 2000) used cluster analysis to identify a sub-group of individuals in nonclinical samples, whom they dubbed ‘overwhelmed,’ whose profiles of emotional experience include low emotional clarity and high affect intensity. ‘Overwhelmed’ individuals report higher levels of neuroticism, stress, and mixed worried-anhedonic symptomatology (Berenbaum, Bredemeier, Thompson, & Boden, 2012; Gohm, Corser, & Dalsky, 2005), endorse more avoidant coping styles (Gohm & Clore, 2000), and appear to suppress negative affect in the lab (Gohm, 2003; Kerns & Bredemeier, 2010). For these reasons we would expect that experiencing low emotional clarity would be most associated with emotion dysregulation and depression in the context of high affect intensity.
Existing associations support considering affect intensity as a moderator of the relationships between emotional clarity and emotion regulation or depression. Trait affect intensity is sometimes (Flett et al., 1996), but not always (Cheavens & Heiy, 2011; Larsen & Diener, 1987), linked with depression, a pattern compatible with the hypothesis that its role in depression depends on other factors. It is important to note that the negative affect intensity construct, which refers to the perceived strength or power of the feelings, is not the same thing as negative affect occurrence or valence, which, unlike intensity, is consistently related with depression (e.g., Watson et al., 1988). Thus while depression is, by definition, associated with pervasive and excessive negative feelings, mixed results concerning affect intensity suggest that depression is not consistently related to the felt intensity of those negative feelings.
Notably, affect intensity and emotional clarity are weakly related, showing a correlation of zero (Gohm, 2003; Gohm & Clore, 2000; 2002) or a small inverse correlation (r = −.12; Berenbaum et al., 2012) in past work. This apparent independence suggests affect intensity and emotional clarity do not merely act as proxies for one another in their relations with depression. Rather, this independence is consistent with construing affect intensity as a variable part of the affective context in which the process of perceiving and regulating emotions unfolds. Viewing affect intensity in this way may have practical clinical implications. In psychosocial interventions, it is often more feasible and therapeutically indicated to modify internal affective conditions than patients’ external situations. For a clinically useful understanding of emotional clarity deficits in depression, it would be fruitful to discover how dimensions of affective experience within the individual set the stage for low emotional clarity to be problematic for some people but not others.
The Current Investigation
In two studies, we sought to extend the literature on the role of emotional clarity in emotion regulation and depression by investigating the moderating role of negative affect intensity. In the first study, we tested a moderation model in an unselected sample of adults to examine whether low emotional clarity was more strongly tied to depression symptoms among individuals who tended to experience negative affect more versus less intensely. In the second study, we used conditional process modeling in a clinical sample to test the more mechanistic prediction that the indirect effects of low emotional clarity on depressive symptoms through impaired emotion regulation similarly depend on patients’ levels of negative affect intensity.
Study 1
In Study 1, examining a nonclinical sample, we tested the hypothesis that the relation between emotional clarity and depressive symptoms depends on the trait intensity of negative affect. First, we predicted that clarity and intensity would be uncorrelated or modestly correlated, suggesting their relative independence. Second, we predicted that lower clarity and higher intensity would each be associated with higher levels of depression symptoms. Finally, following the hypothesis that adaptive effects of clarity are most salient under conditions of strong emotional experience, we predicted that clarity would show a statistical interaction with affect intensity, such that clarity’s negative associations with depressive symptoms would be strongest among individuals higher in affect intensity.
Method
Participants and procedure
Participants were 119 undergraduates and members of the community surrounding a university in the Northeastern United States. They were not recruited or prescreened for criteria other than a minimum age of 18 years. They were compensated with course credit or $10. The sample included 65 women (54.6%) and 54 men (45.4%) with a mean age of 19.7 years (SD=2.2; range=18–30). Participants identified as White (56.3%), Asian/Asian-American (16.8%), Hispanic (8.4%), Black/African-American (7.6%), Multi-ethnic (7.6%), and other (3.3%).
Measures included in the present study were among a larger battery examining affective traits, future-oriented cognition, and depression (see Marroquín, Boyle, Nolen-Hoeksema, & Stanton, 2016). All procedures were approved by the Institutional Review Board, and participants provided informed consent. They were debriefed and provided with mental health resources at the end of the study.
Measures
We assessed emotional clarity with the 11-item Clarity of Feelings subscale of the Trait Meta-Mood Scale (TMMS; Salovey et al., 1995). Items capture individuals’ subjective sense that they can typically identify which emotions they feel (e.g., “I am rarely confused about how I feel,” “I can’t make sense of my feelings” [reverse-coded]). Participants rated agreement using a 5-point scale, and their responses were averaged. This scale has shown convergent validity with similar measures, discriminant validity from measures of mood state or attention to one’s emotions, and association with depressive symptoms (Salovey et al., 1995). Internal consistency in this sample was good, α =.88.
We assessed negative affect intensity with the 6-item Negative Intensity (NI) subscale of the Affect Intensity Measure (Bryant, Yarnold, & Grimm, 1996). Although this measure was originally designed as a 40-item scale containing four factors (Weinfurt, Bryant, & Yarnold, 1994), Bryant and colleagues (1996) identified a stronger, 3-factor solution using 27 of the more reliable items. On the NI subscale from this version, participants report on the intensity of their typical emotional reactions (e.g., “My emotions tend to be more intense than those of most people;” “My friends might say I’m emotional”) from 1 (never) to 6 (always), and responses are summed. Negative intensity is distinct from negative reactivity (i.e., one’s sensitivity/threshold for an emotional response to negative stimuli) on this measure (Bryant et al., 1996), and has expected predictive relationships with relevant clinical impairments (e.g., problem drinking, borderline personality; Salsman & Linehan, 2012; Veillieux, Skinner, Reese, & Shaver, 2014). Internal consistency in this sample was good, α =.73.
We assessed symptoms of depression with the widely used second edition of the Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996). This 21-item measure assesses cognitive, emotional, behavioral, and somatic symptoms of depression over the past 2 weeks, with item scores ranging from 0 (e.g., “I have not lost interest in other people or activities”) to 3 (e.g., “It’s hard to get interested in anything”). The BDI-II has shown excellent reliability and validity, and it showed good internal consistency in the present study, α =.84.1
Results
Preliminary analyses
The mean depressive symptom score was 7.40 (SD = 5.63; range = 0–23). The mean score for emotional clarity was 3.49 (SD = 0.68; range = 1.36–4.91). Mean negative affect intensity was 19.51 (SD = 5.13; range = 9–32). As predicted, depressive symptoms were associated with higher affect intensity, r = .45, p < .001, and lower emotional clarity, r = −.38, p < .001. Consistent with the notion that they are independent dimensions of emotional experience, clarity and intensity scores were uncorrelated, r = −.11, p = .223.
Moderation analyses
We tested our moderation hypothesis using the PROCESS procedure for testing conditional effects (Hayes, 2013). We conducted a multiple regression analysis predicting depressive symptoms from clarity and intensity (centered around their means) and their interaction. The main effects of emotional clarity, b = −2.82, SE = 0.63, p < .001, and negative affect intensity, b = 0.46, SE = 0.08, p < .001, on depressive symptoms were qualified by a statistically significant clarity-by-intensity interaction, b = −0.31, SE = 0.12, p = .013, F(3,115) = 19.96, p < .001. The model accounted for 34% of variance in depressive symptoms.
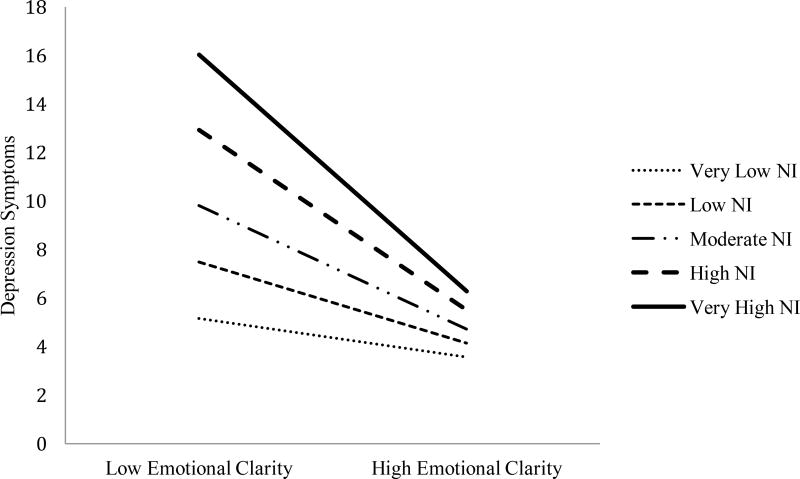
We probed this interaction in two ways: by examining and graphing the effects of emotional clarity on depression symptoms at 10th, 25th, 50th, 75th, and 90th percentile values (i.e., very low, low, moderate, high, and very high levels) of negative affect intensity, and by using the Johnson-Neyman technique to estimate the specific negative affect intensity score at which the relationship between emotional clarity and depression reaches statistical significance. As shown in Figure 1, the association between emotional clarity and symptoms was statistically significant at low, b = −1.75, SE = 0.74, p = .019, moderate, b = −2.66, SE = 0.63, p < .001, high, b = −3.88, SE = 0.78, p < .001, and very high, b = −5.11, SE = 1.14, p < .001 levels of negative affect intensity, such that clarity had a stronger association with depressive symptoms at increasingly high levels of negative intensity. At very low levels of intensity, emotional clarity was unassociated with symptoms, b = −0.83, SE = 0.98, p = .398. The Johnson-Neyman technique indicated that the relation between lower emotional clarity and higher depressive symptoms was significant at raw intensity values of 15.34 and above, or among the upper 76.47% of participants in the distribution of intensity scores.2
Figure 1.
Moderation of the relationship between emotional clarity and depression symptoms by negative affect intensity (Study 1). NI = negative affect intensity (Bryant et al., 1996). Relationships are estimated at 10th, 25th, 50th, 75th, and 90th percentile values of negative affect intensity for the present sample, or raw values of 13, 16, 19, 23, and 27. Regression lines are depicted terminating at 10th and 90th percentile points of the distribution of emotional clarity, or raw values of 19 and 9, respectively (high scores reflect low emotional clarity, given structure of DERS scale).
Discussion
In an unselected sample, participants lower in emotional clarity reported more depressive symptoms, consistent with past research (e.g., Lee & Guajardo, 2011). The tendency to experience negative emotions intensely was also linked to higher depressive symptoms, as has been found in some previous work (Cheavens & Heiy, 2011, Flett et al., 1996). Moreover, as predicted, the relation between emotional clarity and depressive symptoms depended on negative affect intensity. Low emotional clarity scores were more strongly linked with symptoms among people higher in negative affect intensity; indeed, among those who tended to experience negative emotions less intensely, emotional clarity was unrelated to symptoms.
These findings are consistent with prior work suggesting that the combination of intense affect that is experienced with a low degree of clarity is particularly problematic for mental health (Gohm, 2003; Berenbaum et al., 2012). While supporting the notion that emotional clarity plays a role in affective psychopathology (Vine & Aldao, 2014), these results also support our hypothesis that this role depends on other aspects of affective experience. Because experiencing negative emotions intensely can contribute to psychological suffering, including depression, it is encouraging that in this very context, the ability to be clear about one’s emotional experience may be especially beneficial.
Although the present findings support our primary hypothesis, they leave several questions unanswered about the role of these affective traits in depressive symptomatology. First, we did not use a clinical sample; it is important to determine whether these findings generalize to clinical levels of distress. If the role of clarity in affective psychopathology depends on particularly intense emotional experience, a clinical sample can shed better light on how and when clarity matters. Second, Study 1 did not address why or how the combination of low emotional clarity and high affect intensity is related to depression severity. In Study 2, we tested a more elaborated model including the mediating role of impaired emotion regulation that has emerged previously (Flynn & Rudolph, 2014; Vine & Aldao, 2014).
Study 2
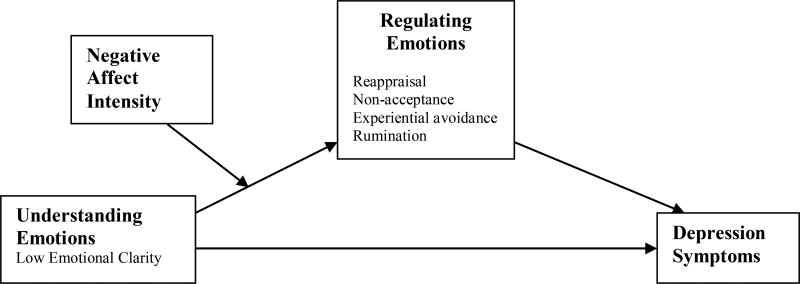
In this study, we examined a clinical sample to test the hypothesis that high versus low affect intensity represent moderators of the relationships between emotional clarity and emotion regulation and, in turn, depressive symptoms. As the conceptual diagram in Figure 2 shows, this study extended Study 1 by incorporating the mediational path through emotion regulation. We hypothesized that four emotion regulation strategies – each of which is implicated in depression and also associated with emotional clarity – would each mediate the association between emotional clarity and depression (Hypothesis 1). The strategies of interest were cognitive reappraisal, emotional non-acceptance, experiential avoidance, and rumination.
Figure 2.
Conceptual illustration of Study 2 conditional process model. Negative affect intensity is considered part of the context within which the process of understanding and regulating emotions unfolds. Study variables used to operationalize conceptual terms appear un-boldfaced.
Cognitive reappraisal involves reinterpreting an emotion-eliciting stimulus in a way that alters the resulting emotion (Gross & John, 2003). Lower self-reported use of reappraisal is related to depression severity (Aldao et al., 2010; Garnefski & Kraaij, 2006) and has been associated with reduced emotional clarity (Boden, Bonn-Miller, Kashdan, Alvarez, & Gross, 2012; Gohm & Clore, 2002). In addition to the more approach-oriented strategy of reappraisal, we also selected two emotion regulation variables involving the rejection of emotional experience. Emotional non-acceptance refers to negative second-order emotional reactions to emotion experience, such as becoming guilty or angry with oneself for feeling upset (Gratz & Roemer, 2004). Emotional non-acceptance is elevated in depression (Ehring et al., 2008) and related to low emotional clarity (Gratz & Roemer, 2004). Although related, experiential avoidance refers to a general negative stance toward emotions that is more cognitive, such as believing emotions cause problems in one’s life. Experiential avoidance is also elevated in depression (Bond et al., 2011) and linked with low emotional clarity (Tull & Gratz, 2008). Finally, rumination is a style of repetitive thinking about the causes and consequences of one’s distress that is strongly associated with depression (Nolen-Hoeksema, 1991). Rumination and related processes have been found to mediate the relationship between low emotional clarity and depression in past studies (Flynn & Rudolph, 2014; Salguero et al., 2013; Vine & Aldao, 2014).
In addition, we predicted that the mediational path from low emotional clarity to depression symptoms through each emotion regulation variable would depend on negative affect intensity (i.e., moderated mediation; Hypothesis 2). We drew specific hypotheses about the nature of each moderation effect from research demonstrating that the particular emotion regulation strategies people implement depends on affect intensity. When given a choice of how to regulate their emotions in response to upsetting images, participants in a nonclinical sample reappraised emotions elicited by low-intensity images, but distracted themselves while viewing intense images (Sheppes & Gross, 2011). This suggests a normative pattern of resorting or defaulting to certain emotion regulation strategies based on affect intensity: avoidance-based responses (e.g. experiential avoidance, non-acceptance) may dominate when emotions are strong, while engagement-based responses (e.g., reappraisal) may dominate when emotions are weaker. We predicted that these tendencies associated with high versus low state intensity would also operate at the level of trait differences in affect intensity.
Specifically, we predicted trait affect intensity would constrain effects of emotional clarity as follows:
(Hypothesis 2a) Emotional clarity would be positively associated with use of reappraisal, except those with lower affect intensity. Among those with low affect intensity, use of reappraisal would be high regardless of emotional clarity.
(Hypothesis 2b) Emotional clarity would be negatively associated with use of non-acceptance and experiential avoidance, except those with higher affect intensity. Among individuals with high affect intensity, use of these avoidant strategies would be high regardless of emotional clarity.
In other words, in contexts in which past research has suggested a strong tendency to default to using an emotion regulation strategy based on affect intensity, we predicted emotional clarity would be less relevant. We did not make specific predictions about the nature of moderation in the rumination model, because rumination shares qualities with both emotion regulation strategies investigated by Sheppes and Gross (2011). On its face, like reappraisal, rumination involves engaging with emotional material; theoretically, however, rumination functions like experiential avoidance to help dampen or suppress emotional experience (Liverant, Kamholz, Sloan, & Brown, 2011).
Method
Participants and procedure
Participants were 245 individuals presenting for treatment at a mood and anxiety disorders clinic in the Northeastern United States.3 They ranged in age from 15 to 70 (M = 36.15, SD = 13.55), and 66.1% were female.4 Seventy-nine percent of participants self-identified as White, 8.2% as Hispanic, 7.3% as African-American, 1.6% as Asian or Asian-American, and 2.4% as ‘other.’ Structured clinical interviews for DSM-IV (SCID-IV; First, Spitzer, Gibbon & Williams, 2002) administered by advanced doctoral students revealed clinically significant levels of distress. The most prevalent Axis I diagnoses were generalized anxiety disorder (58.4%), major depressive disorder (53.5%), and social phobia (32.7%). Other diagnoses included panic disorder (19.2%), specific phobia (12.7%), obsessive-compulsive disorder (8.2%), eating disorders (10.6%), substance use disorders (9.4%), dysthymia (7.3%), and bipolar disorder (4.1%). Most participants (74.3%) met criteria for more than one Axis I disorder, and 20.4% met criteria for an Axis II disorder. Participants completed a battery of self-report measures of cognition, emotion, and personality, as well as mood and anxiety symptoms, including the following measures relevant to this investigation.
Measures
As in Study 1, participants reported trait negative affect intensity using the Negative Intensity subscale of the Affect Intensity Measure (Bryant et al., 1996). Internal consistency in the present sample was acceptable, α = .73. Emotional clarity was measured with the clarity subscale of the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004). Participants rate their agreement with five statements about the degree to which they typically understand their emotions on a 5-point Likert scale (e.g., “I am confused about how I feel,” “I am clear about my feelings”). In order to parallel Study 1, we keyed scores so that higher numbers indicated higher emotional clarity. Internal consistency in the present sample was good, α = .86.
To assess depression symptoms, we used scores from the Anhedonic Depression subscale of the Mood and Anxiety Symptom Questionnaire Short Form (MASQ AD; Watson & Clark, 1991). The MASQ AD subscale contains 22 items describing aspects of depression that are not shared with anxiety disorders (e.g., “I felt really slowed down,” “I felt like nothing was enjoyable”). Items are rated on a 5-point scale with higher scores indicating more symptoms. Internal consistency in our sample was good, α= .88.
We assessed reappraisal using the reappraisal subscale of the Emotion Regulation Questionnaire (ERQ; Gross & John, 2003). Participants rate their agreement on a 7-point scale with six statements about the extent to which they change their thinking in order to change how they feel (e.g., “When I want to feel less negative emotion, I change the way I’m thinking about the situation”). Higher scores represent a higher self-reported tendency to use reappraisal. Internal consistency in our sample was excellent, α = .91.
We assessed non-acceptance of emotions using the Non-Acceptance subscale of the DERS (Gratz & Roemer, 2004). This subscale consists of six items assessing negative meta-reactions to being upset (e.g., “When I’m upset, I feel guilty for feeling that way,” “When I’m upset, I feel like I am weak”). Participants rate their agreement with these items on a 5-point scale, so that higher scores correspond to more negative meta-reactions, or higher non-acceptance. Internal consistency in our sample was excellent, α = .91.
We assessed experiential avoidance using the Acceptance and Action Questionnaire—II (AAQ-II; Bond et al., 2011). The AAQ-II captures the extent to which individuals attempt to avoid or suppress difficult or unwanted internal experiences, including emotions. Using a 7-point scale, participants rate how frequently seven statements are true (e.g., “I am afraid of my feelings,” “Emotions cause problems in my life”), so that higher scores indicate higher levels of experiential avoidance. Internal consistency in our sample was good, α = .86.
We assessed rumination using the brooding subscale of the Response Styles Questionnaire (Treynor, Gonzalez, & Nolen-Hoeksema, 2003). This 5-item subscale assesses the extent to which people engage in negative, self-focused, repetitive thought processes when feeling sad, blue, or depressed (e.g., “I think, ‘why do I have problems other people don’t have?’”). Content of the brooding subscale is independent of symptoms of depression (Treynor et al., 2003). Reliability in our sample was acceptable, α = .79.
Results
Preliminary analyses
Means, standard deviations, and bivariate correlations for all study variables appear in Table 1. Consistent with prior research (e.g., Berenbaum et al., 2012) and Study 1 above, emotional clarity and negative affect intensity had a weak, inverse relationship, r = −.12, p = .056. Both low emotional clarity and negative affect intensity were positively correlated with depressive symptom severity, ps < .001. Low emotional clarity, negative affect intensity, and depressive symptoms were correlated with all emotion regulation measures, ps < .01, and emotion regulation measures were correlated with each other, ps < .05.
Table 1.
Means, Standard Deviations, and Bivariate Correlations for Study 2 Variables
| M | SD | 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Emotional Clarity | 14.45 | 4.18 | - | ||||||
| 2. AIM-NI | 22.89 | 5.32 | −.12† | - | |||||
| 3. MASQ-AD | 73.23 | 11.75 | −.24*** | .22*** | - | ||||
| 4. ERQ Reappraisal | 13.64 | 5.32 | −.36*** | −.20** | .28*** | - | |||
| 5. DERS Non-Acceptance | 16.54 | 6.57 | −.22*** | .26*** | .30*** | .16* | - | ||
| 6. AAQ-II | 29.84 | 8.30 | −.36*** | .52*** | .57*** | .19* | .43*** | - | |
| 7. RSQ Brooding | 13.67 | 3.19 | −.27*** | .48*** | .37*** | .17* | .40*** | .53*** | - |
Note. Emotional Clarity = Clarity subscale of DERS, reverse-keyed such that higher number indicate greater self-reported emotional clarity; AIM-NI = Negative Affect Intensity subscale, Affect Intensity Measure, following scoring by Bryant et al., 1996; MASQ-AD = Anhedonic Depression subscale, Mood and Anxiety Symptom Questionnaire; ERQ = Emotion Regulation Questionnaire; DERS = Difficulties in Emotion Regulation Scale; AAQ-II = Acceptance and Action Questionnaire – II;RSQ = Response Styles Questionnaire.
p < .10.
p<.05.
p<.01.
p<.001.
Moderated mediation analyses
We estimated four moderated mediation models corresponding to the conceptual diagram in Figure 2, one for each emotion regulation strategy being considered as a mediator (reappraisal, non-acceptance, experiential avoidance, and rumination). We used the procedure for conditional process modeling by Hayes (2013), which combines an ordinary least squares regression approach to moderation testing with bootstrapped mediation analysis, which estimates the magnitude of indirect effects by generating a confidence interval using repeated resampling of the available data. To facilitate interpretation of regression coefficients, we centered all predictor variables.
For each model, we first report (1) whether moderated mediation occurred, as indicated by a statistically significant change in the strength of the indirect effect of clarity through the emotion regulation variable as a function of the moderator, affect intensity (see Hayes 2013). Where moderated mediation was evident, we report (2) the values of intensity at which the indirect effect of clarity was statistically significant. Effects are considered statistically significant if their point estimate was significantly different from zero, or in other words, if the bias-corrected 95% confidence interval using 5,000 bootstrap samples does not contain zero. Next, we examined (3) the sub-portion of each model predicting the emotion regulation mediator from emotional clarity and probed any significant interactions between emotional clarity and negative affect intensity. Table 2 displays regression coefficients and bootstrapped confidence intervals for conditional indirect effects for all four models. Figure 3 depicts the interactions between emotional clarity and negative affect intensity on emotion regulation within each model.
Table 2.
Path Coefficients with Standard Errors and Bootstrap Point Estimates with Confidence Intervals for Moderated Mediation Models (Study 2)
| Mediator (Med) |
Effect of EC on Med. (a1) |
Effect of NI on Med. (a2) |
Effect of EC × NI interactionon Med. (a3) |
Effect of Med. on Depressive Symptoms (b) |
Direct Effect of EC on Depressive Symptoms (c’) |
Conditional Indirect Effect of EC on Depressive Symptoms via Med. (ab) at Percentile Levels of NI |
||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Very Low (10%) |
Low (25%) |
Moderate (50%) |
High (75%) |
Very High (90%) |
||||||
| Reappraisal | .39 (11)*** | −.31 (.09)*** | .04 (.02)* | −.39 (.11)*** | −.54 (.19)** | −.05 [−.25, .09] | −.09 [−.27, .01] | −.15 [−.31, −.06] | −.21 [−.40, −.10] | −.26 [−.48 −.11] |
| Non-acceptance | −.35 (.09)*** | .30 (.08)*** | .04 (.02)** | .46 (.11)*** | −.50 (.17)** | −.30 [−.53, −.12] | −.24 [−.43, −.10] | −.16 [−.30, −.06] | −.08 [−.21, .02] | −.02 [−.16, .12] |
| Experiential Avoidance | −.70 (.13)*** | .75 (.10)*** | .06 (.02)** | .82 (.10)*** | −.29 (.22) | −.95 [− 1.46, −.58] | −.79 [− 1.21, −.48] | −.58 [−.89, −.33] | −.36 [−.62, −.15] | −.21 [−.47, .04] |
| Rumination | −.17 (.04)*** | .27 (.03)*** | .01 (.01) | 1.27 (.23)*** | −.40 (.17)* | −.28 [−.54, −.12] | −.25 [−.46, −.13] | −.22 [−.37, −.11] | −.18 [−.33, −.06] | −.15 [−.32, −.00] |
Note. EC = Emotional Clarity (Gratz & Roemer, 2004 [reverse-scored, so that higher numbers correspond to higher self-reported clarity]). NI = Negative Intensity subscale, Affect Intensity Measure (Bryant et al., 1996). Raw values for 10th, 25th, 50th, 75th, and 90th percentiles of negative affect intensity are 16, 19, 23, 27, and 30, respectively. Standard errors for path coefficients appear in parentheses. 95% bias-corrected confidence intervals for point estimates appear in brackets; point estimates are interpreted as significant if confidence intervals do not contain zero; significant point estimates are boldfaced.
p<.05.
p<.01.
p<.001.
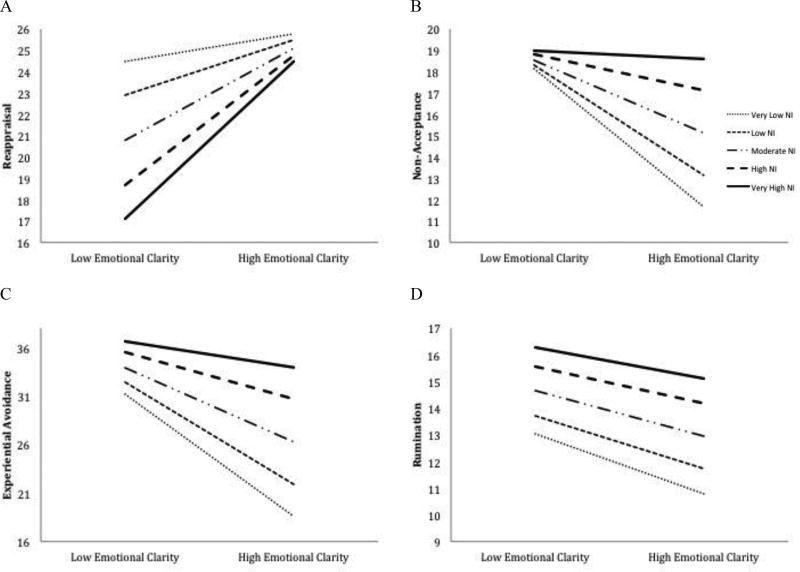
Figure 3.
Moderation of the relationships between emotional clarity and use of emotion regulation strategies within larger moderated mediation models (Study 2). NI = negative affect intensity (Bryant et al., 1996). Relationships are estimated at 10th, 25th, 50th, 75th, and 90th percentile values of affect intensity for the present sample, or at raw values of 16, 19, 23, 27, and 30. Regression lines are depicted terminating at 10th and 90th percentile points of the distribution of emotional clarity, or raw values of 2.45 and 4.36, respectively.
Reappraisal model
This model explained 11.43% of variance in depression symptoms, F(2,217) = 14.00, p < .001. As predicted, the indirect effect of low emotional clarity on depression symptoms through reappraisal was significantly moderated by negative affect intensity, b = −0.02, SE = 0.01, [−.04, −.01]. Inspection of bootstrap confidence intervals (Table 2) revealed that low emotional clarity predicted lower reappraisal, which in turn predicted higher depression, but only at moderate, high, and very high levels of negative affect intensity.
Together, emotional clarity, negative affect intensity, and their interaction explained 14.99% of variance in reappraisal scores, F(3,216) = 12.69, p < .001. Emotional clarity and negative affect intensity both had significant main effects on reappraisal, ps < .001. These main effects were further qualified by a significant interaction, p = .030, that uniquely accounted for 1.87% of the variance in reappraisal scores, F(1,216) = 4.76, p=.030 The pattern of effects was such that emotional clarity was associated with reappraisal, but only among individuals reporting moderate, high, and very high negative affect intensity (Figure 3A; Table 2). Specifically, the relationship between emotional clarity and reappraisal was significant when negative affect intensity was above a raw value of 19.81, or among patients in the top 73% of the observed distribution of negative affect intensity scores.
Non-acceptance model
This model explained 11.81% of variance in depression symptoms, F(2,241) = 16.14, p < .001. As predicted, the indirect effect of low emotional clarity on depression symptoms through non-acceptance was significantly moderated by negative affect intensity, b = 0.02, SE = 0.01, [.01, .04]. Specifically, we found statistical mediation such that low emotional clarity predicted increased non-acceptance, which in turn predicted higher depression, but only at very low, low, and moderate levels of negative affect intensity.
Emotional clarity, negative affect intensity, and their interaction explained 12.89% of variance in non-acceptance scores, F(3,240) = 11.84, p < .001. Emotional clarity and negative affect intensity both had significant main effects on non-acceptance, ps < .001. These main effects were further qualified by a significant interaction, p = .006, that uniquely accounted for 2.75% of the variance in non-acceptance scores, F(1,240) = 7.59, p = .006. The pattern of effects was such that emotional clarity was inversely associated with non-acceptance, but only among individuals reporting very low, low, and moderate negative affect intensity (Figure 3B). Specifically, the relationship between emotional clarity and non-acceptance was significant when negative affect intensity was below 26.25, or among the lower 73% of patients in the sample.
Experiential avoidance model
The model explained 33.18% of variance in depression symptoms, F(2,165) = 40.96, p < .001. As we predicted, the indirect effect of low emotional clarity on depression symptoms through experiential avoidance was significantly moderated by negative affect intensity, b = 0.05, SE = 0.02, [.03, .09]. In other words, a statistical mediation emerged, such that low emotional clarity predicted higher experiential avoidance, which in turn predicted higher depression, but only among individuals very low, low, moderate, and high in negative affect intensity. The mediation was not significant among those very high in negative affect intensity.
Emotional clarity, negative affect intensity, and their interaction explained 38.71% of variance in experiential avoidance scores, F(3,164) = 34.53, p < .001. Emotional clarity and negative affect intensity both had significant main effects on experiential avoidance, ps < .001. These main effects were further qualified by a significant interaction, p = .003, that uniquely accounted for 3.42% of the variance in experiential avoidance scores F(1,164) = 9.15, p = .003. The pattern of effects was such that emotional clarity was inversely associated with experiential avoidance among all individuals reporting very low, low, and moderate negative affect intensity (Figure 3C). More precisely, the relationship between emotional clarity and experiential avoidance was only significant below a negative affect intensity score of 28.86, or among the lower 83% of patients in the sample.
Rumination model
This model explained 16.36% of variance in depression symptoms, F(2,241)=23.57, p<.001. The indirect effect of low emotional clarity on depression symptoms through rumination was significant, but it was not conditional on negative affect intensity, b = 0.01, SE = 0.17, [–.01, .03]. In other words, low emotional clarity predicted higher rumination, and in turn higher depression, and this was true at all levels of negative affect intensity. Emotional clarity and negative affect intensity, along with their interaction term, explained 27.84% of the variance in rumination scores, F(3,240) = 30.87, p < .001.
Emotional clarity had a significant main effect on rumination scores, p < .001, such that lower reports of emotional clarity were associated with higher self-reported rumination. Negative affect intensity was also significantly related to rumination, p < .001. The interaction between emotional clarity and affect intensity was not significant, p = .263 (Figure 3D).
Discussion
In Study 1, we observed that the relationship between low emotional clarity and depression symptoms was strongest among individuals reporting high affect intensity, and non-significant among those reporting very low affect intensity. In Study 2 we found a similar pattern regarding intensity as a moderator, but this time in terms of moderating the indirect relationship between low emotional clarity and depression through emotion regulation. Consistent with Hypothesis 1, low emotional clarity was associated with self-reported use of three out of four emotion regulation strategies, and in turn depression symptoms. Consistent with Hypothesis 2, for three of the four emotion regulation mediators (i.e., reappraisal, non-acceptance, and experiential avoidance), indirect effects were only significant for patients reporting some levels of affect intensity.
Specifically, the indirect effect of low emotional clarity on depression through reappraisal was significant for patients in the upper 73% range of negative affect intensity, or for most patients except those reporting very low negative affect intensity. These results support Hypothesis 2a, that emotional clarity would matter more for reappraisal among participants higher in negative affect intensity, when the natural tendency to reappraise is weaker (Sheppes & Gross, 2011), whereas those lower in affect intensity would report using reappraisal regardless of emotional clarity. The indirect effect of low emotional clarity on depression through non-acceptance and experiential avoidance was significant for participants in the lower 73% and 83% range of negative affect intensity, respectively. In other words, low emotional clarity predicted use of these avoidant strategies among most patients, except those reporting tendencies to experience their negative emotions extremely intensely. This pattern is consistent with Hypothesis 2b, that emotional clarity would matter most for avoidant strategies when participants were lower in negative affect intensity, or when the natural tendency to reject or avoid emotional experience is weaker (Sheppes & Gross, 2011).
We did not make specific predictions about the moderation of the indirect path through rumination, and results indicated that this path was not conditional on affect intensity. The relationship between low emotional clarity and depression through rumination was significant regardless of patients’ levels of negative affect intensity. This mediation effect replicates existing findings (e.g., Flynn & Rudolph, 2010; Salguero et al., 2013; Vine & Aldao, 2014) and further suggests that affect intensity is not a moderator of the relationship between low emotional clarity and rumination.
General Discussion
In two studies, we investigated the moderators of the relationships between low emotional clarity, use of emotion regulation strategies, and depressive symptoms. Study 1, conducted with a nonclinical sample, showed that the degree to which low emotional clarity was associated with depression symptoms depended on individuals’ tendencies to experience negative affect intensely. These results reveal limits of previous findings that low emotional clarity plays a role in depressive symptoms and other psychopathology. Results are also consistent with past work on the ‘overwhelmed’ emotional style in nonclinical samples, which is characterized primarily by low emotional clarity and high affect intensity (e.g., Gohm, 2003), and highlight a potential role of this emotional style in depression.
Study 2, conducted in patients diagnosed with DSM-IV emotional disorders, added further nuance by demonstrating that the mediating role of emotion regulation, found previously to link low emotional clarity to depression (e.g., Flynn & Rudolph, 2014), may also depend on negative affect intensity. People tend to reappraise negative emotional stimuli when their intensity is low and avoid paying attention to stimuli when their intensity is high (Sheppes & Gross, 2011). Our findings indicate that these tendencies may constitute boundaries beyond which emotional clarity has no reliable relationship with emotion regulation and depression symptoms. When affect intensity was extremely low, emotional clarity played no role in predicting reappraisal, and when affect intensity was extremely high, emotional clarity did not predict non-acceptance or experiential avoidance. These results suggest that the beneficial effects of emotional clarity play out only within limits set by the subjective intensity of emotional responses. At more extreme (high and low) levels of intensity, default patterns of regulating emotions in certain ways may ‘kick in,’ making emotional clarity of little use. Of the strategies investigated here, only rumination mediated effects of low emotional clarity on depression at all levels of affect intensity. This may indicate that the use of rumination is linked to difficulties identifying emotions for distinct reasons. For instance, rumination may be a misguided effort aimed at increasing emotional clarity (Vine, Aldao, & Nolen-Hoeksema, 2014).
The present investigation adds to a small literature suggesting that low emotional clarity is not always a problem. For instance, low emotional clarity has been associated with rumination prospectively, but only among individuals who reported high intolerance of ambiguity (Vine et al., 2014). Among military veterans, low emotional clarity was associated with more severe posttraumatic stress disorder, but only if they reported lower use of cognitive reappraisal to regulate their emotions (Boden et al., 2012). Most applicably to the present investigation, depressive symptoms have been associated with low emotional clarity in the contexts of physical pain and perceived life stressors, but not when these intense external situations are absent (Kennedy et al., 2010; Stange et al., 2013). Our findings extend these: the extent to which emotional clarity matters for depression-related outcomes depended on the subjective intensity of internal experiences as well.
Importantly, emotional clarity and negative affect intensity were uncorrelated in both our samples, supporting the notion that they represent distinct constructs. Thus, it is unlikely that difficulty understanding one’s emotions is just a function of not experiencing them strongly enough to detect, or experiencing them too strongly to handle. Instead, emotional clarity can be considered a relatively independent trait that may interact with other affective traits within the individual. This apparent independence echoes previous reports (e.g., Extermera & Fernández-Berrocal, 2005; Palmer, Donaldson, & Stough, 2002; Salovey at al., 1995) that have provided evidence of discriminant validity of emotional clarity as distinct from broader and famously robust individual differences implicated in depression such as negative affectivity or neuroticism (e.g., Weinstock & Whisman, 2006). Further, this seeming independence supports the notion that varying combinations of emotional clarity and affect intensity are possible and may even constitute distinct emotional “styles” (Gohm, 2003). Research on emotion regulation increasingly acknowledges the role of context – such as social context or characteristics of emotional stimuli (Aldao, 2013). Our findings are consistent with the notion that features of subjective experience like trait affect intensity may also contribute importantly to this context.
In general, our findings support the increasing emphasis in psychosocial prevention and treatments for depression on helping individuals better understand their emotions in order to regulate them adaptively (e.g., Berking, Ebert, Cuijpers, & Hofmann, 2013; Hagelskamp, Brackett, Rivers, & Salovey, 2013). Given our findings, it might serve clinicians to anticipate that patients experiencing depressive symptoms will disproportionately exhibit both low emotional clarity and high affect intensity, and to be prepared to assess and target both difficulties in tandem. By construing affect intensity as part of the context in which people understand and regulate emotions, our framework may help streamline decision-making about when and how to introduce training in emotion awareness. A patient whose affect intensity is exceedingly high may be taught to apply clarity or information about emotions to the task of cognitively reappraising emotion-eliciting situations, even if he cannot allow himself to fully experience or accept the emotion. In order to use emotional clarity to engage in more experiential forms of emotion regulation, however, the intensity of affect might need to be within – or, through treatment, be brought within – a more moderate range.
To our knowledge, this is the first report to examine the mediating role of emotion regulation in explaining the relationship of low emotional clarity to depressive symptoms using a clinical sample. The treatment-seeking sample in Study 2 exhibited considerable levels of clinically diagnosable Axis I and Axis II psychopathology with high rates of comorbidity. Historically, the majority of research on emotional clarity has been interested in its consequences for adaptive emotional functioning in non-clinical settings (e.g., job success, interpersonal relationships; Brackett, Rivers, & Salovey, 2013; Extermera & Fernández-Berrocal, 2005; Palmer et al., 2002; Salovey at al., 1995). The present study is one of the first to test a statistical model of the consequences of emotional clarity for the emotion regulation and psychological adaptation in the context of complex, ecologically valid clinical presentations. This is also the first study to examine moderators of the hypothesized emotion regulatory mechanism (Vine & Aldao, 2014) by which low emotional clarity may be implicated in emotion dysregulation and depression. Thus, the present results suggest not only the specific emotion regulatory difficulties that may explain why low emotional clarity is implicated in clinically significant depressive symptoms, but also which patients with low emotional clarity may experience which emotion regulatory difficulties.
Despite these strengths, the present studies must be interpreted within the context of some limitations. First, both studies were cross-sectional, which prevents them from addressing causal aspects of our theory. Future prospective work could examine effects over time, and experimental manipulations of intensity and clarity might test causal roles in emotion regulation. Second, the present studies examined clarity and intensity as trait variables. Although individual differences in these traits are relevant to depression, future work could also examine how these phenomena influence regulation in the moment (and how these state processes are modifiable in emotion-focused treatment). Third, the use of self-report measures cannot address other important dimensions of affective experience (e.g., whether one’s perception of emotional clarity maps on to the ability to label emotions in objectively accurate, or normative, ways). However, the perceived ability to understand emotions is a clear and robust predictor of psychosocial and clinical outcomes (e.g., Flynn & Rudolph, 2014; Vine & Aldao, 2014). Moreover, although we examined four individual emotion regulation strategies independently, people vary in the depth, breadth, and use of multiple strategies in their repertoires. The ability to flexibly deploy strategies depending on situational demands and resources is adaptive with respect to depression (Aldao et al., 2015) and may itself depend on emotional clarity and intensity.
The use of the MASQ AD to assess depressive symptoms in Study 2 represents a trade-off. One the one hand, the scale’s freedom from anxiety-related items ensures that results are specific to depression. On the other, this means our results may not generalize to helping explain related forms of psychopathology. Importantly, the majority of the sample was diagnosed with at least one anxiety disorder; despite the specificity of the depressive symptom measure, findings represent a population with high anxiety-depression comorbidity. To more fully understand the clinical relevance of combinations of emotional clarity and affect intensity, it will be important to investigate the present model from a transdiagnostic perspective. The transdiagnostic and continuous nature of the model’s key constructs makes it suited to future investigations utilizing transdiagnostic classification systems (e.g., Research Domain Criteria; Insel et al., 2010).
This investigation highlights other avenues for further research. In three of our four models, the associations between emotional clarity and depressive symptoms were statistically significant even when taking the mediational path through emotion regulation strategies into account. This raises the possibility that there are additional routes through which low emotional clarity relates to depression that future studies could identify. Experiments using cognitive paradigms are needed to test hypotheses that understanding emotions helps regulate them by providing information (Barrett & Gross, 2001) or by alleviating cognitive load (e.g., Lischetzke & Eid, 2003). Furthermore, in addition to understanding the role of intrapersonal emotion regulation in depression (e.g., Hofmann et al., 2012), it is also important to better illuminate interpersonal emotion regulation mechanisms (Hofmann, 2014; Marroquín, 2011); the interactive effects of low emotional clarity and affect intensity could be examined in this context as well. For example, close others may be able, through either everyday or supportive interactions, to increase clarity through thoughtful questioning, or decrease intensity through soothing, and thus counteract individuals’ affective tendencies, making way for more effective regulation. Finally, given the role of dampened positive emotion in depression (e.g., Watson et al., 1988) and findings that individual differences in meta-cognitions about positive emotion can defuse consequences of negative mood states (Marroquín et al., 2016), future research could examine the role of emotional clarity and intensity in facilitating regulation of and maximizing benefits of positive emotion. Such approaches could augment the present findings that the relationship of low emotional clarity to clinically significant depressive symptoms—directly, and indirectly via emotion regulation strategies—depend on trait differences in the intensity with which individuals experience negative affect.
Acknowledgments
The authors are grateful to the Yale Center for Anxiety and Mood Disorders. They thank Jutta Joormann and the members of the Affect Regulation and Cognition Lab at Yale University for comments on an earlier version of this manuscript.
Funding: Author A was partially supported by National Institute of Mental Health grant T32 MH018951. Author B was partially supported by National Institute of Mental Health grant T32 MH015750.
Footnotes
Given the nonclinical nature of this sample, the distribution was checked for normalcy. Using the benchmarks of skewness and kurtosis < 2.0 (Tabachnik & Fidell, 2007), the BDI-II scores are considered adequately distributed (skewness = 0.91, SE = .22; kurtosis = 0.16, SE = .90). We observed three extreme scores at BDI-II values of 22, 23, and 23 (2.59, 2.77, and 2.77 SD above the sample mean, respectively).
Because of the slight skew in BDI-II scores, it was possible the clarity-intensity interaction was driven by just a few participants with elevated depression symptoms. To investigate this possibility, we re-ran our model excluding the three more extreme BDI-II scores. As in the full sample, motional clarity and negative affect intensity interacted to predict depression scores, b = −0.31, SE = 0.11, p = .008, such that the association between emotional clarity and symptoms was statistically significant at low, b = −1.79, SE = 0.68, p < .01, moderate, b = −2.71, SE = 0.58, p < .001, high, b = −3.95, SE = 0.73, p < .001, and very high, b = −4.87, SE = 0.98, p < .001 levels of negative affect intensity. At very low levels of intensity, emotional clarity was unassociated with symptoms, b = −0.86, SE = 0.90, p = .341. To further examine the relevance of this interaction at low levels of depression severity, we repeated analyses in a subsample (n = 101) restricted to the subclinical range (i.e., less than “mild depression,” or BDI-II < 14). Even in this healthier subset, the pattern of results mirrored the full sample. Specifically, emotional clarity was inversely associated with depression severity at moderate, high and very high levels of negative affect intensity (ps < .005; i.e., among the upper 73.27% of this subsample), but unrelated at lower values of negative affect intensity. The differences between these effects were strong enough to yield a marginally significant clarity-by-intensity interaction (b = −0.18, SE = 0.10, p = .09). Taken together, follow-up analyses show the clarity-intensity interaction was not explained by outliers and appears to operate in both clinical and subclinical participants. This needs to be confirmed with further analyses predicating a broader distribution of depression severity scores (see Study 2).
Some participants skipped occasional items on the emotion regulation questionnaires; we considered data to be missing if the individual had completed fewer than 80% of the items from a given measure. For this reason, and because the ERQ and AAQ-II were added to the questionnaire battery later than the other measures, the sample size differed between models (N = 244 for rumination and non-acceptance models, N = 220 for reappraisal, and N = 168 for experiential avoidance).
Adult participants provided consent for their responses to be used in research; adolescent participants provided assent, and their guardians provided consent.
Compliance with Ethical Standards
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Conflict of Interest: Author A and Author B declare that they have no conflict of interest.
References
- Aldao A. The future of emotion regulation research: Capturing context. Perspectives on Psychological Science. 2013;8(2):155–172. doi: 10.1177/1745691612459518. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, Schweizer S. Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review. 2010;30(2):217–37. doi: 10.1016/j.cpr.2009.11.004. [DOI] [PubMed] [Google Scholar]
- Aldao A, Sheppes G, Gross JJ. Emotion regulation flexibility. Cognitive Therapy and Research. 2015;39:263–278. [Google Scholar]
- Barrett LF, Gross JJ. Emotional intelligence: A process model of emotion representation and regulation. In: Mayne TJ, Bonanno GA, editors. Emotions: Current issues and future directions. New York: Guilford Press; 2001. pp. 286–310. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory-II: Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. pp. 1–82. [Google Scholar]
- Berenbaum H, Bredemeier K, Thompson RJ, Boden MT. Worry, anhedonic depression, and emotional styles. Cognitive Therapy and Research. 2012;36:72–80. [Google Scholar]
- Berking M, Ebert D, Cuijpers P, Hofmann SG. Emotion regulation skills training enhances the efficacy of inpatient cognitive behavioral therapy for major depressive disorder: A randomized controlled trial. Psychotherapy and Psychosomatics. 2013;82(4):234–245. doi: 10.1159/000348448. [DOI] [PubMed] [Google Scholar]
- Boden MT, Berenbaum H. What you are feeling and why: Two distinct types of emotional clarity. Personality and Individual Differences. 2011;51:652–656. doi: 10.1016/j.paid.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden MT, Bonn-Miller MO, Kashdan TB, Alvarez J, Gross JJ. The interactive effects of emotional clarity and cognitive reappraisal in posttraumatic stress disorder. Journal of Anxiety Disorders. 2012;26(1):233–2388. doi: 10.1016/j.janxdis.2011.11.007. [DOI] [PubMed] [Google Scholar]
- Boden MT, Thompson RJ, Dizén M, Berenbaum H, Baker JP. Are emotional clarity and emotion differentiation related? Cognition & Emotion. 2013;27(6):961–78. doi: 10.1080/02699931.2012.751899. [DOI] [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Zettle RD. Preliminary psychometric properties of the Acceptance and Action Questionnaire--II: A revised measure of psychological inflexibility and experiential avoidance. Behavior Therapy. 2011;42(4):676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Brackett MA, Rivers SE, Reyes MR, Salovey P. Enhancing academic performance and social and emotional competence with the RULER feeling words curriculum. Learning and Individual Differences. 2012;22(2):218–224. doi: 10.1016/j.lindif.2010.10.002. [DOI] [Google Scholar]
- Bryant FB, Yarnold PR, Grimm LG. Toward a measurement model of the affect intensity measure: A three-factor structure. Journal of Research in Personality. 1996;30(2):223–247. [Google Scholar]
- Cheavens JS, Heiy J. The differential roles of affect and avoidance in major depressive and borderline personality disorder symptoms. Journal of Social and Clinical Psychology. 2011;30(5):441–457. [Google Scholar]
- Ehring T, Fischer S, Schnülle J, Bösterling A, Tuschen-Caffier B. Characteristics of emotion regulation in recovered depressed versus never depressed individuals. Personality and Individual Differences. 2008;44(7):1574–1584. [Google Scholar]
- Extermera N, Fernández-Berrocal P. Perceived emotional intelligence and life satisfaction: Predictive and incremental validity using the Trait Meta-Mood Scale. Personality and Individual Differences. 2005;39:937–948. [Google Scholar]
- Fernandez-Berrocal P, Alcaide R, Extremera N, Pizarro D. The role of emotional intelligence in anxiety and depression among adolescents. Individual Differences Research. 2006;4(1):16–27. [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured clinical interview for DSM-IV-TR Axis I disorders. New York: NY State Psychiatric Institute, Biometrics Research; 2002. [Google Scholar]
- Flett GL, Blankstein KR, Obertynski M. Affect intensity, coping styles, mood regulation expectancies, and depressive symptoms. Personality and Individual Differences. 1996;20(2):221–228. [Google Scholar]
- Flynn M, Rudolph KD. The contribution of deficits in emotional clarity to stress responses and depression. Journal of Applied Developmental Psychology. 2010;31(4):291–7. doi: 10.1016/j.appdev.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn M, Rudolph KD. A prospective examination of emotional clarity, stress responses, and depressive symptoms during early adolescence. The Journal of Early Adolescence. 2014;34(7):923–939. doi: 10.1177/0272431613513959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnefski N, Kraaij V. Relationships between cognitive emotion regulation strategies and depressive symptoms: A comparative study of five specific samples. Personality and Individual Differences. 2006;40(8):1659–1669. [Google Scholar]
- Gohm CL. Mood regulation and emotional intelligence: Individual differences. Journal of Personality and Social Psychology. 2003;84(3):594. [PubMed] [Google Scholar]
- Gohm CL, Clore GL. Individual differences in emotional experience: Mapping available scales to processes. Personality and Social Psychology Bulletin. 2000;26(6):679–697. [Google Scholar]
- Gohm CL, Clore GL. Four latent traits of emotional experience and their involvement in well-being, coping, and attributional style. Cognition and Emotion. 2002;16(4):495–518. doi: 10.1080/02699930143000374. [DOI] [Google Scholar]
- Gohm CL, Corser GC, Dalsky DJ. Emotional intelligence under stress: Useful, unnecessary, or irrelevant? Personality and Individual Differences. 2005;39(6):1017–1028. [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- Gross JJ. The emerging field of emotion regulation: An integrative review. Review of General Psychology. 1998;2(3):271. [Google Scholar]
- Gross JJ, John OP. Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology. 2003;85(2):348–362. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- Hagelskamp C, Brackett MA, Rivers SE, Salovey P. Improving classroom quality with the RULER approach to social and emotional learning: Proximal and distal outcomes. American Journal of Community Psychology. 2013:1–14. doi: 10.1007/s10464-013-9570-x. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Hofmann SG. Interpersonal emotion regulation model of mood and anxiety disorders. Cognitive Therapy and Research. 2014;38(5):483–492. doi: 10.1007/s10608-014-9620-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Fang A, Asnaani A. Emotion dysregulation model of mood and anxiety disorders. Depression and Anxiety. 2012;29(5):409–416. doi: 10.1002/da.21888. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Rottenberg J. Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review. 2010;30(7):865–878. doi: 10.1016/j.cpr.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy LA, Cohen TR, Panter AT, Devellis BM, Yamanis TJ, Jordan JM, Devellis RF. Buffering against the emotional impact of pain: Mood clarity reduces depressive symptoms in older adults. Journal of Social and Clinical Psychology. 2010;29(9):975–987. [Google Scholar]
- Kerns JG, Berenbaum H. Affective processing in overwhelmed individuals: Strategic and task considerations. Cognition and Emotion. 2010;24(4):638–660. [Google Scholar]
- Larsen RJ, Diener E. Affect intensity as an individual difference characteristic: A review. Journal of Research in Personality. 1987;21(1):1–39. [Google Scholar]
- Lee SA, Guajardo NR. Affect intensity and alexithymia differentially influence the relationship between neuroticism and depressive symptomatology among college students. Personality and Individual Differences. 2011;50(5):646–650. [Google Scholar]
- Lischetzke T, Eid M. Is attention to feelings beneficial or detrimental to affective well-being? Mood regulation as a moderator variable. Emotion. 2003;3(4):361–77. doi: 10.1037/1528-3542.3.4.361. [DOI] [PubMed] [Google Scholar]
- Liverant GI, Kamholz BW, Sloan DM, Brown TA. Rumination in clinical depression: A type of emotional suppression? Cognitive Therapy and Research. 2011;35(3):253–265. doi: 10.1007/s10608-010-9304-4. [DOI] [Google Scholar]
- Marroquín B. Interpersonal emotion regulation as a mechanism of social support in depression. Clinical Psychology Review. 31:1276–1290. doi: 10.1016/j.cpr.2011.09.005. [DOI] [PubMed] [Google Scholar]
- Marroquín B, Boyle CC, Nolen-Hoeksema S, Stanton AL. Using emotion as information in future-oriented cognition: Individual differences in the context of state negative affect. Personality and Individual Differences. 2016;95:121–126. doi: 10.1016/j.paid.2016.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, Holaway RM, Fresco DM, Moore MT, Heimberg RG. Delineating components of emotion and its dysregulation in anxiety and mood psychopathology. Behavior Therapy. 2007;38(3):284–302. doi: 10.1016/j.beth.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100(4):569. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Watkins ER. A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Science. 2011;6(6):589–609. doi: 10.1177/1745691611419672. [DOI] [PubMed] [Google Scholar]
- Palmer B, Donaldson C, Stough C. Emotional intelligence and life satisfaction. Personality and Individual Differences. 2002;33(7):1091–1100. [Google Scholar]
- Salguero JM, Extremera N, Fernández-Berrocal P. A meta-mood model of rumination and depression: Preliminary test in a non-clinical population. Scandinavian Journal of Psychology. 2013;54(2):166–72. doi: 10.1111/sjop.12026. [DOI] [PubMed] [Google Scholar]
- Salovey P, Mayer JD, Goldman SL, Turvey C, Palfai TP. Emotional attention, clarity, and repair: Exploring emotional intelligence using the trait meta-mood scale. In: Pennebaker JW, editor. Emotion, disclosure, and health. Washington, DC: American Psychological Association; 1995. pp. 125–154. [Google Scholar]
- Salsman NL, Linehan MM. An investigation of the relationships among negative affect, difficulties in emotion regulation, and features of borderline personality disorder. Journal of Psychopathology and Behavioral Assessment. 2012;34(2):260–267. [Google Scholar]
- Sheppes G, Gross JJ. Is timing everything? Temporal considerations in emotion regulation. Personality and Social Psychology Review. 2011;15(4):319–331. doi: 10.1177/1088868310395778. [DOI] [PubMed] [Google Scholar]
- Stange JP, Alloy LB, Flynn M, Abramson LY. Negative inferential style, emotional clarity, and life stress: Integrating vulnerabilities to depression in adolescence. Journal of Clinical Child and Adolescent Psychology. 2013;42(4):508–18. doi: 10.1080/15374416.2012.743104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnik BL, Fidell LS. Using multivariate statistics. 5. Boston, MA: Pearson Education, Inc; 2007. [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S. Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research. 2003;27(3):247–259. [Google Scholar]
- Tull MT, Gratz KL. Further examination of the relationship between anxiety sensitivity and depression: The mediating role of experiential avoidance and difficulties engaging in goal-directed behavior when distressed. Journal of Anxiety Disorders. 2008;22(2):199–210. doi: 10.1016/j.janxdis.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Veilleux JC, Skinner KD, Reese ED, Shaver JA. Negative affect intensity influences drinking to cope through facets of emotion dysregulation. Personality and Individual Differences. 2014;59:96–101. [Google Scholar]
- Vine V, Aldao A. Impaired emotional clarity and psychopathology: A transdiagnostic deficit with symptom-specific pathways through emotion regulation. Journal of Social and Clinical Psychology. 2014;33(4):319–342. [Google Scholar]
- Vine V, Aldao A, Nolen-Hoeksema S. Chasing clarity: Rumination as a strategy for making sense of emotions. Journal of Experimental Psychopathology. 2014;5(3):229–243. [Google Scholar]
- Watson D, Clark LA. The mood and anxiety symptom questionnaire. Unpublished Manuscript, University of Iowa, Department of Psychology, Iowa City 1991 [Google Scholar]
- Watson D, Clark LA, Carey G. Positive and negative affectivity and their relation to anxiety and depressive disorders. Journal of Abnormal Psychology. 1988;97(3):346. doi: 10.1037//0021-843x.97.3.346. [DOI] [PubMed] [Google Scholar]
- Weinfurt KP, Bryant FB, Yarnold PR. The factor structure of the Affect Intensity Measure: In search of a measurement model. Journal of Research in Personality. 1994;28(3):314–331. [Google Scholar]
- Weinstock LM, Whisman MA. Neuroticism as a common feature of the depressive and anxiety disorders: A test of the revised integrative hierarchical model in a national sample. Journal of Abnormal Psychology. 2006;115(1):68–74. doi: 10.1037/0021-843X.115.1.68. [DOI] [PubMed] [Google Scholar]