Abstract
Background
Biospecimens from racially diverse groups are needed to advance cancer research. The Asian American Cancer Education Study (AACES) was developed to increase the number and proportion of blood biospecimen donations from Asian Americans for cancer research.
Methods
Our targeted approach included two types of community engagement, in-reach (within institution to Asian American cancer patients) and outreach (external to institution to the general Asian American community). Participants received in-language biospecimen education followed by the opportunity to donate blood biospecimens. Outreach participants donated through our community biospecimen blood drives and in-reach participants consented to donating an extra tube of blood during their routine blood draws as a patient. Donated blood biospecimens was spun down to serum and plasma to be stored in a biorepository or were sent to the laboratory to test for cancer related risk factors.
Results
Three hundred eighty-eight Asian Americans donated 1127 blood biospecimens for cancer research. Four hundred and twenty tubes of plasma and serum are currently being stored at the cancer center’s biorepository, 39 tubes have been utilized for cancer genomic research and 668 tubes were used to characterize cancer-related risk factors.
Conclusion
Building upon the past decade of the NCI funded Asian American Network for Cancer Awareness, Research and Training (AANCART)’s foundation of trust and service with the Asian Americans, researchers were able to leverage relationships to not only introduce the idea of biospecimen contribution to the community, but to also exceed our expectations in the quantity of blood biospecimens collected from Asian Americans.
Keywords: Biospecimen Donation, Cancer Research, Asian American, Biobanking, Community Engagement, Community Outreach
INTRODUCTION
Biospecimens provide researchers with the bases for measuring biological, pharmacological, and response differences among racial/ethnic populations thus offering great potential for personalized medicine approaches.1-3 Increasing the number and the proportion of biospecimens from racial/ethnic minority populations is essential to developing more effective cancer treatments for those groups and in the long term is essential to reducing cancer health disparities.4 To ensure that Asian Americans, the fastest-growing racial/ethnic group in the United States5-6 and the first U.S. racial/ethnic group to experience cancer as the leading cause of death7-8 are participating in donating biospecimens for cancer research, the Asian American Network for Cancer Awareness and Training (AANCART): The National Center for Reducing Asian American Cancer Health Disparities developed the Asian American Cancer Education Study (AACES). The goal of AACES was to increase the number and proportion of blood biospecimens donated for cancer research from Asian Americans through community engagement, outreach and in-reach (within the institution), and through education.
Through AACES we first examined individual factors associated with Asian Americans’ willingness to donate biospecimens for cancer research. Like other studies, we discovered that while Asian American had low levels of awareness and knowledge regarding biospecimen donation and biobanking, interventions that increased knowledge of and fostered more favorable attitudes towards biospecimen donation resulted in a higher willingness to donate.9-12 Common barriers to donation include: cultural beliefs about biospecimens such as the belief that there is a finite amount of blood in the body and once that blood leaves the body it will not be replenished; not being asked to donate; and distrust of research. 9-12 Common facilitators to donating include: altruism and wanting to benefit future generations.9-12 However, while we found common factors that influence Asian American’s decision to donate biospecimens, we also found ethnic specific differences as well. For example, our needs assessment revealed that not only did Chinese, Hmong, and Vietnamese respondents differed in the perceived benefits and their perceived barriers for donating biospecimens, but they also differed in terms of the setting they found most conducive for providing biospecimens.10,13-14
Based on our formative research and a review of the literature, we recognize that there is considerable heterogeneity within the Asian American community and that a one size fits all approach to engaging the Asian American community in biospecimen donation would not work. Thus we developed targeted community engagement and outreach campaigns tailored to each respective ethnic group: Chinese, Hmong and Vietnamese. Our assumption is that Asian Americans will donate blood biospecimens if researchers first established a foundation of trust by being transparent in their research endeavors and by committing the time necessary to build community capacity for biospecimen donation, and secondly by providing Asian Americans with an opportunity to donate.
The purpose of this paper is to describe our approach and to report findings in increasing blood biospecimens donations for cancer research from both the general Asian American community and from Asian American cancer patients. Our approach included two types of community engagement, outreach and in-reach. Outreach refers to the approach we utilized with the general Asian Americans community and in-reach refers to the approach we utilized with Asian American cancer patients within our own institution.
MATERIALS AND METHODS
AACES Timeframe
AACES began in January 2010 and ended June 2016. From January 2010-December 2011 we conducted formative research on factors that influence Asian American’s decision to donate biospecimens for cancer research and based on those findings, developed in-language culturally appropriate biospecimen education material (video and brochure) in Cantonese, Hmong, Korean, Mandarin and Vietnamese. From January 2012 – August 2014 we held community biospecimen blood drives to recruit the general Asian American community to donate blood biospecimens for cancer research and from August 2014 – June 2016 we recruited Asian American cancer patients being seen at the University of California, Davis Comprehensive Cancer Center (UCD CCC). This paper will focus on January 2012 through June 2016, the period where we recruited Asian Americans to donate only blood biospecimens. Results from the AACES needs assessment, pilot studies and the development of the educational materials have been presented elsewhere.10,13-14
This study was approved by the University of California, Davis (UCD) Institutional Review Board. All participants were consented in their language of preference and all blood biospecimens donated were processed and stored at the University of California, Davis Biorepository, a Cancer Center Support Grant Shared Resource. Study activities occurred in Sacramento, CA, a city located in UCD CCC’s primary catchment area. Participants received a $10 giftcard to a local supermarket.
Outreach
Study Sites and Design
Through AANCART, we have developed and fostered a decade long relationship with the Chinese, Hmong and Vietnamese communities of Sacramento, CA. We utilized those relationships to approach and engage these communities in biospecimen donation. For the Hmong community, we collaborated with a local Hmong community based organization, Hmong Women’s Heritage Association (HWHA) and for the Chinese and Vietnamese communities we collaborated with two UC Davis student run medical clinics, Paul Hom Asian Clinic (PHAC) and the Vietnamese Cancer Awareness Research Education Society (VNCARES) Clinic. We have partnered with HWHA, PHAC and VNCARES on numerous cancer control and prevention projects including conduct of the AACES formative research and the development of the biospecimen educational materials. In addition to collecting blood biospecimens for future cancer research we also collected blood biospecimens to test for the hepatitis B virus and to test for diabetes (through the hemoglobin A1c test) to assess the prevalence of these two conditions in these communities. We chose hepatitis B and diabetes because these were two health problems our community partners informed us that impacted their respective communities.
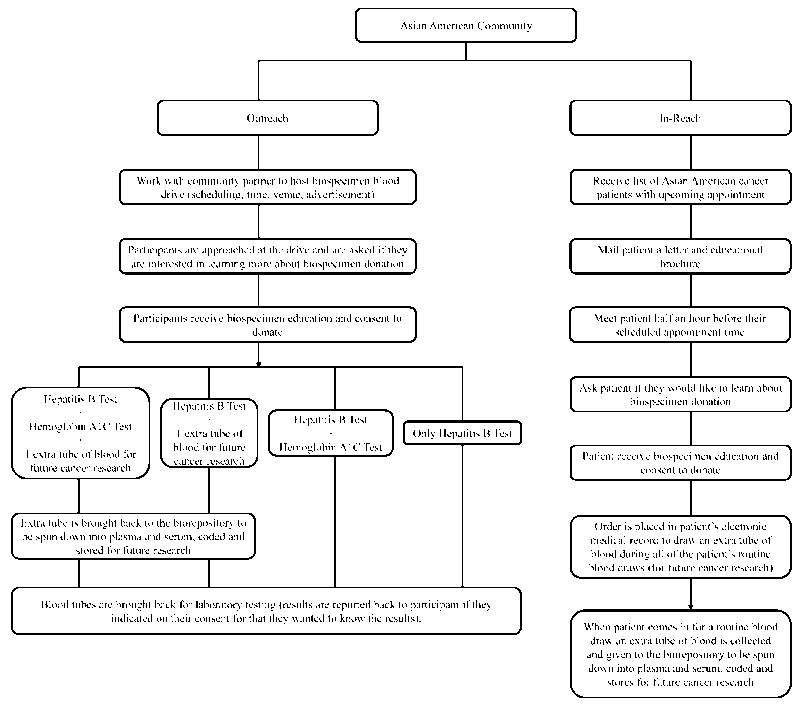
Our outreach approach was to work with our community partners to provide biospecimen education to their respective communities and then secondly to host community biospecimen blood drives to recruit interested individuals to donate. All engagement, outreach and educational activities were provided in both English and in the native language of the participants. See figure 1 below for a flowchart of our outreach community engagement strategy.
Figure 1.
Outreach and In-reach Community Engagement Approach
Screening and Recruitment
Participants of the community biospecimen blood drive were recruited through our collaborating organizations and through ethnic-media (newspaper advertisements and radio ads). All participants who donated blood biospecimens were required to be at least 18 years of age. Participants also filled out a short survey regarding their age, gender, and country of birth.
Community Biospecimen Blood Drives
Similar in concept to a blood drive, we held community biospecimen blood drive to offer interested individuals the opportunity to donate blood biospecimens on site and at a location convenient to them. These drives typically lasted between two to three hours and were held in conjunction with health promotion activities sponsored by the collaborating organizations (i.e. health fairs, health screenings, community forums, etc.) and at community-based venues (i.e. community centers, churches, temples, community health clinics, at the offices of the community-based organizations, etc.).
During these health promotion activities, our health educators would approach potential participants and engage them in a conversation (in the language of preference of the participant) regarding biospecimen donation. If the individual agreed to participate, the health educator would consent them and help them complete the short survey. A phlebotomist would than draw the participant’s blood and a staff from the UCD CCC Biorepository collected the donated blood biospecimens and transported it back to the UCD CCC Biorepository. For each participant, the entire process took about 15-20 minutes to complete. Participants had the option of donating 1, 2 or 3 (3.5mL) tubes of blood for either hepatitis B testing, hemoglobin A1c testing, and/or for future cancer research. Additionally, participants had the option of whether they wanted to be contacted with the results of the hepatitis B and/or hemoglobin A1C test.
Once the blood was transported back to UCD CCC, depending on what the participant decided to consent to donating, the blood was either processed by the laboratory for the appropriate testing and/or was either given to the biorepository to be spun down into plasma and serum, coded, and stored in the biorepository freezer.
In-reach
Study Sites and Design
We worked with UCD CCC providers and staff to develop a protocol that would allow us to approach and engage Asian American cancer patients in biospecimen donation. Our approach had three main components: we first had to set up a standing monthly report to get a list of all Asian American patients who had an upcoming appointment at the UCD CCC; next we contacted the patient and invited them to come to their appointment times half an hour early to learn more about biospecimen donation; and lastly for those who did arrive early we educated them on donating biospecimens and after the education session asked them to if they consent to donating an extra tube of blood for cancer research at each of their next routine blood draw as a patient. See Figure 1 for a flowchart of our in-reach community engagement strategy.
Screening and Recruitment
We worked with the UC Davis Health Clinical and Translational Science Center Biomedical Informatics team to utilize our electronic health system to generate an automated monthly report of all the Asian American patients that had an upcoming UCD CCC appointment. This report was created by developing an algorithm that identified Asian American patients by the 50 most common surnames for each ethnicity15 and by self-reported race/ethnicity. We focused only on patients for whom we had health educators that can provide in-language education (Chinese, Hmong, and Vietnamese) and on Asian American patients who listed English as their preferred language. This report included the contact information (address and phone number) for each patient, the patient’s scheduled appointment date and time and the patient’s preferred language. We excluded all new Asian American patients so that their providers would be able to establish a relationship with them first. Additionally, we did not review the patient’s electronic medical record, thus we chose not to know the reason for their visit or the stage of their treatment.
Biospecimen Educational Sessions
Only providers who consented for their patients to be included in AACES were invited to be part of this study. Two weeks before a patient had a scheduled appointment, research staff mailed the patient a letter letting them know that a health educator will meet with them in the reception area thirty minutes prior to their appointment time to talk to them about donating biospecimens for cancer research. In addition to the letter, patients received a tri-fold biospecimen brochure that was double sided with English on one side and the patient’s preferred language on the other side (if not English).
On the day of their appointment, a health educator arrived at the stated time and checked in with the front desk staff to see if the patient had arrived. If the patient had arrived the health educator approached the patient and asked them if they are interested in learning about biospecimen donation. If the patient did not arrive, the health educator waited in the reception area until they did arrive and then proceeded to ask them if they wanted to participate. If the patient was not interested, the health educator thanked them for their time and gave them a business card in case they wanted to participate at a later time. If the patient agreed to participate, the health educator had the patient view a five minute biospecimen educational video on an iPad in the patient’s preferred language. The health educator next proceeded to answer any questions participants had regarding donating. Educational sessions usually lasted about 15-30 minutes long and after the session was over, the health educator asked the patient if they would like to donate an extra tube of blood during their next routine blood draw for cancer research. If the patient agreed, the team member would consent them. All consent forms were then handed over the UCD CCC Biorepository staff to enter an order into the patient’s electronic medical record (EMR) indicating that the patient agreed to donating an extra tube of blood for cancer research at each of their next routine blood draw.
Time
AANCART has partnered with the Asian American community of Sacramento, CA since 2002, when AANCART’s headquarters moved from Columbus, Ohio to Sacramento, CA. This partnership has led to many collaboration over the years to not only increase cancer awareness, prevention and control in the community but also to build capacity and facilitate community-based participatory research.16 We partnered with the Sacramento Hmong community on two-five year randomized controlled trials to increase hepatitis B testing17 and colorectal cancer screening18 in their community and with the Vietnamese and Chinese community we collaborated on a three year project to increase hepatitis B testing.19 These partnerships, established over a decade represents our commitment to the community. Our ability to approach and engage the Asian American community on the topic of biospecimen donation stems from the time we have devoted to earning the trust of the community.
In terms of our in-reach, we wanted to be mindful of the patient’s time, thus we started AACES in the community and circled back to patients equipped with our lessons learned and materials developed. The same values that motivated the community to donate (benefiting future generations) and the approach used (health educators and a direct opportunity to donate) resulted in the recruitment of both cancer patients and the general community.
Trust
Central to the responsiveness of our participants is earning their trust. In our case, that trust was earned by nearly a decade of working in the local Asian American community through AANCART. We acknowledge that not everyone will have a decade of community partnership to cultivate trust; however, we believe that trust was also earned through utilizing bilingual and bicultural health educators to provide the biospecimen education and through cohosting biospecimen blood drives with local trusted community based organizations. Those organizations serve as gatekeepers to their communities and by engaging them at the start of the study, we received their full support. Not only was trust earned through the longevity of partnerships and collaborations, but also we believe trust must continue to be earned through every event and through the research team being transparent about their research endeavors.
Transparency
We as well as others have cited mistrust as a significant barrier to engaging diverse communities in biospecimen donation.10,20 Similarly, mistrust of the research being conducted can be avoided by having researchers commit to being upfront and transparent to the community about their research objectives.20 In our approach, we found that by inviting the community to be a part of the research team we could overcome issues around mistrust. The community was assured that our processes were transparent because they were given full disclosure of our research. They provided input in the design of the study, assisted in the development of our engagement strategies and reviewed all our study documents (e.g. the consent forms, educational materials, survey questions, and protocol).
RESULTS
A total of 388 Asian Americans donated 1127 blood biospecimens for cancer research (359 from outreach and 29 from in-reach). Four hundred and twenty tubes of plasma and serum are currently being stored for future cancer research in the UCD CCC Biorepository, 39 blood biospecimens have been utilized for cancer genomic research and 668 were used for laboratory testing of hepatitis B and diabetes. The majority of donors were between the ages of 18-29 (33.0%); female (66.8%); and foreign-born (53.9%).
Outreach versus In-reach
We hosted 10 community biospecimen blood drives (5 in the Hmong community and 5 in the Chinese/Vietnamese community). At these drives a total of 359 Asian American community members donated 1,068 blood biospecimens for cancer research. The majority of donors were Hmong (48.2%); between the ages of 18-29 (34.8%); female (66.9%); and foreign-born (53.8%). In terms of in-reach, the staff contacted 117 patients and enrolled 34 patients into AACES. After receiving the education session, 29 (85%) consented to donating blood biospecimens for cancer research. Thirteen of those 29 patients donated (59 serum and plasma biospecimens) and the remaining 16 have orders for blood draw in their EMR. The majority of donors were female (65.5%); 60 years of age and older (62.1%); Chinese (34.5%); and foreign-born (55.2%).
DISCUSSION
To the best of our knowledge, AACES has collected one of the largest numbers of blood biospecimens from Asian Americans (community members and cancer patients) for cancer research. Our approach, building upon our formative research and the literature, demonstrates that Asian Americans are willing to participate in biospecimen collection. By incorporating culturally and linguistically appropriate, ethnically-specific, and cognitively empowering educational materials and strategies into our approach we were able to appropriate addressed the potential cognitive (i.e. language, lack of knowledge), cultural (i.e. significance of biospecimens) and social (i.e. research mistrust) issues surrounding biospecimen donation.21 We discovered that once participants understood how blood biospecimens can be used to further cancer research and improve health outcomes for future generations, the majority were willing to donate despite their initial hesitancy if they are given an opportunity to donate.
Cognitively, the first issue we encountered was with translating the term, “biospecimen” appropriately into the different Asian languages as there are not Asian language equivalents for the term. After consulting with the communities we decided that instead of trying to technically translate “biospecimen” into the different languages we would give examples of the types of biospecimens individuals could donate instead, e.g., blood, hair, saliva, urine, toe nail clippings, etc. Additionally, historically and culturally speaking, traditional Chinese, Hmong and Vietnamese viewed blood as a source of life or vitality, thus blood donation was avoided where possible.9-10 In terms of addressing social barriers to donating, including community members as a part of the research team alleviated many of the concerns regarding research mistrust. For example, the community members voiced that their community would not be uncomfortable with the idea having donated biospecimens stored indefinitely, thus we worked collaboratively to establish an acceptable timeframe for utilizing the samples (10 years from date of collection). Additionally, because the most compelling reason to donate was to benefit future generations, we unanimously decided that all donated biospecimens would be utilized for only Asian American cancer health disparities research.
Similarly to the studies conducted by Gao et al. (2014), and Rodriguez et al. (2016), we discovered that individuals would be willing to blood donate biospecimens for research if given an opportunity to donate immediately following a biospecimen educational session.22-23 However, while both of those studies focused on engaging the general community and required participants to attend an in-depth (45-60 minutes) biospecimen educational seminar prior to donating, our approach included engaging both cancer patients and the general community and did not require participants to attend an in-depth educational session on biospecimens. Our study provides evidence that in-depth education may not be required for communities to donate biospecimens for cancer research and also suggest that simply not being asked to donate is a significant barrier to donating.9-12
Limitations/Strengths
Despite many strengths, our study has some limitations. The participants were a convenience sample comprised of mostly foreign-born female Asian American participants; and in terms of outreach the majority of the participants were Hmong because of the large number of community biospecimen blood drives we held in the Hmong community; for in-reach the majority were Chinese cancer patients. On the other hand, relatively few of foreign-born women, particularly Hmong, are being served by mainstream health systems and are under-represented in cancer research. We attribute our success to the trust imputed to us through our collaborators and the provision of in-language services. Additionally, individuals who participated in the events could have been motivated by their interest in the sponsoring organization’s theme, e.g., getting tested for HBV etc. and for patients, only those interested in learning more about biospecimens participated in the educational sessions. We also recognize that some intra-group variations may exist between those who choose to donate and those who did not (i.e., those who are more acculturated versus less acculturated as well as educational and socioeconomic differences). Thus, we cannot generalize our findings because our sample may not be representative of the ethnic group they are from.
Nevertheless, the findings are useful as it one of the first studies to collect blood biospecimens from diverse Asian Americans for cancer research. The approach we have outlined significantly increased the number of biospecimens donated by Asian Americans for cancer research and exemplifies a model approach. The more biospecimens we have from diverse populations, the closer we get to understanding the mechanism behind biological, molecular and cancer population research. For example, the biospecimens collected in this study has been utilized to characterize Asian American cancer risk factors based on clinical diagnosis (rather than self-report)24 and the community blood biospecimens have been the bases for positing that the high frequency of the PNPLA3 rs738409 [G] single nucleotide polymorphism may potentially explain the genetic predisposition for chronic liver disease among Hmong.25
CONCLUSIONS
Our approach has the potential to serve as a model for cancer centers interested in engaging diverse communities in their research endeavors. By adhering to the three principles of time, trust and transparency, we were able to introduce a new concept to the community, receive their buy-in and successfully engage them in donating biospecimens. However, in order to foster and nurture these relationships, community engagement efforts need to be viewed as mutually beneficial and not as a one-sided effort, and also need to embrace the cultural and social values embedded in these communities. These collaborations should build community capacity to not only understand the value of research but also advocate for their need. Researchers need to commit to investing the time necessary to developing community relationships and earning community trust by being transparent in their research motives. Our result of community responsiveness to this approach testifies to the effectiveness for what has been accomplished.
Table 1.
Demographics of Asian American Biospecimen Donors by Ethnicity, January 2012 – June 2016
| Chinese n = 69 (%) | Hmong n = 174 (%) | Filipino n = 6 | Japanese n = 8 | Vietnamese n = 114 (%) | Other n = 17 (%) | Total n = 388 (%) | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Age | |||||||
| 18-29 | 25 (36.2%) | 30 (17.2%) | 0 | 0 | 69 (60.5%) | 4 (23.5) | 128 (33.0%) |
| 30-39 | 2 (2.9%) | 20 (11.5%) | 0 | 0 | 7 (6.1%) | 1 (5.9%) | 30 (7.7%) |
| 40-49 | 2 (2.9%) | 32 (18.4%) | 0 | 0 | 5 (4.4%) | 7 (41.2%) | 46 (11.9%) |
| 50-59 | 17 (24.6%) | 51 (29.3%) | 1 (16.7%) | 1 (12.5%) | 14 (12.3%) | 4 (23.5%) | 88 (22.7%) |
| 60+ | 18 (26.1%) | 35 (20.1%) | 5 (83.3%) | 7 (87.5%) | 16 (14.0%) | 0 | 81 (20.9%) |
| Unknown | 5 (7.2%) | 6 (3.4%) | 0 | 0 | 3 (2.6%) | 1 (5.9) | 15 (3.9%) |
|
| |||||||
| Gender | |||||||
| Female | 43 (62.3%) | 125 (71.8%) | 4 (66.7%) | 5 (62.5% | 73 (64.0%) | 9 (52.9%) | 259 (66.8%) |
| Male | 26 (37.7%) | 42 (24.1%) | 2 (33.3%) | 3 (37.5%) | 41 (36.0%) | 8 (47.1%) | 122 (31.4%) |
| Unknown | 0 | 7 (4.0%) | 0 | 0 | 0 | 0 | 7 (1.8%) |
|
| |||||||
| Foreign-Born | |||||||
| Yes | 40 (58.0%) | 73 (42.0%) | 5 (83.3%) | 2 (25.0%) | 76 (66.7%) | 13 (76.5%) | 209 (53.9%) |
| No | 20 (29.0%) | 9 (5.2%) | 1 (16.7%) | 6 (75.0%) | 25 (21.9%) | 4 (23.5%) | 65 (16.8%) |
| Unknown | 9 (13.0%) | 92 (52.9%) | 0 | 0 | 13 (11.4%) | 0 | 114 (29.4%) |
Percentages may not total 100% because of rounding
Acknowledgments
The authors would like to thank Irmgard Feldman of the UCD Biorepository; local community partners (Hmong Women’s Heritage Association, Paul Hom Asian Clinic, California Northstate University Cancer Awareness Research and Education Club, and Vietnamese Cancer Awareness Research and Education Society Clinic) for their assistance in this research.
FUNDING SUPPORT
Funding for this study was provided in part through a cooperative agreement grant funded by the National Cancer Institute’s Center to Reduce Cancer Health Disparities (grants 3U01CA114640-05S4, 1U54 CA153499, U54 CA153499-01S1, 1U54 153499-02S1).
Footnotes
AUTHOR CONTRIBUTIONS
Julie H.T Dang: Conceptualization, methodology, primary data collection; project administration, writing (original draft), and writing. Moon S. Chen Jr.: Conceptualization, methodology, supervision, and writing. Both authors provided substantial contributions to the analysis and interpretation of the data, critically revising it for intellectual content, approving the final version, and agreed to be accountable for all aspects of the work.
CONFLICT OF INTEREST DISCLOURES
Other than funding from the NIH grants cited in Funding Support, the authors declare no other conflicts of interest disclosures.
References
- 1.Moore HM, Compton CC, Lim MD, Vaught J, Christiansen KN, Alper J. 2009 biospecimen research network symposium: advancing cancer research through biospecimen science. Cancer Res. 2009;69(17):6770–6772. doi: 10.1158/0008-5472.CAN-09-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hewitt RE. Biobanking: the foundation of personalized medicine. Curr Opin Oncol. 2010;23:112–9. doi: 10.1097/CCO.0b013e32834161b8. [DOI] [PubMed] [Google Scholar]
- 3.Olson JE, Bielinski SJ, Ryu E, Winkler EM, Takahashi PY, Pathak J, Cerhan JR. Biobanks and personalized medicine. Clin Genet. 2014;86(1):50–55. doi: 10.1111/cge.12370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moore HM, Compton CC, Lim MD, Vaught J, Christiansen KN, Alper J. 2009 Biospecimen research network symposium: advancing cancer research through biospecimen science. Cancer Res. 2009 Sep 1;69(17):6770–2. doi: 10.1158/0008-5472.CAN-09-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.United States Census Bureau. Newsroom. Available at: https://www.census.gov/newsroom/press-releases/2013/cb13-112.html Retrieved on August 8, 2017.
- 6.Colby SL, Ortman JM. Current Population Reports. Washington, DC: US Census Bureau; 2014. Projections of the Size and Composition of the US Population: 2014 to 2060; pp. P25–1143. [Google Scholar]
- 7.Torre LA, Sauer MG, Chen MS, Jr, Kagawa Singer M, Jemal A, Siegel RL. Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: Converging incidence in males and females. CA: a cancer journal for clinicians. 2016;66(3):182–202. doi: 10.3322/caac.21335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Center for Health Statistics. Health, United States, 2005 with Chartbook on Trends in the Health of Americans. Washington, DC: U.S. Government Printing Office; 2005. Table 31. [PubMed] [Google Scholar]
- 9.Tong EK, Fung LC, Stewart SL, Paterniti DA, Dang JH, Chen MS., Jr Impact of a biospecimen collection seminar on willingness to donate biospecimens among Chinese Americans: results from a randomized, controlled community-based trial. Cancer Epidemiology and Prevention Biomarkers. 2014;23(3):392–401. doi: 10.1158/1055-9965.EPI-13-0744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dang JH, Rodriguez EM, Luque JS, Erwin DO, Meade CD, Chen MS., Jr Engaging diverse populations about biospecimen donation for cancer research. Journal of community genetics. 2014;5(4):313–327. doi: 10.1007/s12687-014-0186-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gao W, Ma GX, Tan Y, Fang C, Weaver J, Jin M, Lai P. Factors associated with willingness to participate in biospecimen research among Chinese Americans. Biopreservation and biobanking. 2014;12(2):131–138. doi: 10.1089/bio.2013.0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Culhane-Pera KA, Moua M, Vue P, Xiaaj K, Lo MX, Straka RJ. Leaves imitate trees: Minnesota Hmong concepts of heredity and applications to genomics research. Journal of community genetics. 2017;8(1):23–34. doi: 10.1007/s12687-016-0284-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dang JH, Moua DF, Chen MS., Jr Abstract ED01-03: Collecting blood biospecimens from Asian American communities through trust and informed consent; Abstracts: AACR International Conference on the Science of Cancer Health Disparities; Sep 18-Sep 21, 2011; Washington, DC. [Google Scholar]
- 14.Dang JH, Chen MS, Jr, et al. Abstract B43: Assessment of an educational video and brochure in four languages: Cantonese, Hmong, Vietnamese, and English for biospecimen contributions; Abstracts: AACR International Conference on the Science of Cancer Health Disparities; Sep 30-Oct 3, 2010; Miami, FL. [Google Scholar]
- 15.Lauderdale DS, Kestenbaum B. Asian American ethnic identification by surname. Population Research and Policy Review. 2000;19(3):283–300. [Google Scholar]
- 16.Shimizu R, Chen MS, Snipes KP, et al. Friendships and relationships. Cancer. 2005;104(S12):2937–2939. doi: 10.1002/cncr.21510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen MS, Jr, Fang DM, Stewart SL, et al. Increasing hepatitis B screening for hmong adults: results from a randomized controlled community-based study. Cancer Epidemiology and Prevention Biomarkers. 2013;22(5):782–791. doi: 10.1158/1055-9965.EPI-12-1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tong EK, Nguyen TT, Lo P, et al. Community health educators increase colorectal cancer screening among Hmong Americans: A cluster randomized controlled trial. Cancer. 2017;123(1):98–106. doi: 10.1002/cncr.30265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dang JH, Chen MS., Jr Increasing Hepatitis B Testing and Linkage to Care of Foreign-Born Asians, Sacramento, California, 2012–2013. Public Health Reports. 2016;131(2_suppl):119–124. doi: 10.1177/00333549161310S218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dash C, Wallington SF, Muthra S, Dodson E, Mandelblatt J, Adams-Campbell LL. Disparities in knowledge and willingness to donate research biospecimens: a mixed-methods study in an underserved urban community. Journal of community genetics. 2014;5(4):329–336. doi: 10.1007/s12687-014-0187-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Partridge EE. Yes, minority and underserved populations will participate in biospecimen collection. Cancer Epidemiology and Prevention Biomarkers. 2014;23(6):895–897. doi: 10.1158/1055-9965.EPI-14-0018. [DOI] [PubMed] [Google Scholar]
- 22.Rodriguez EM, Saad-Harfouche FG, Miller A, et al. Engaging diverse populations in biospecimen donation: results from the Hoy y Mañana study. Journal of community genetics. 2016;7(4):271–277. doi: 10.1007/s12687-016-0275-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao W, Ma GX, Tan Y, et al. Culturally appropriate education intervention on biospecimen research participation among Chinese Americans. Cancer Epidemiology and Prevention Biomarkers. 2014;23(3):383–391. doi: 10.1158/1055-9965.EPI-13-0742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stewart SL, Dang J, Chen MS., Jr Diabetes Prevalence and Risk Factors in Four Asian American Communities. Journal of community health. 2016;41(6):1264–1273. doi: 10.1007/s10900-016-0214-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tepper CG, Dang JHT, Stewart SL, Fang DM, Wong KA, Liu SY, Davis RR, Dao DY, Gregg JP, Török NJ, Chen MS., Jr High Frequency of the PNPLA3 rs738409 [G] Single Nucleotide Polymorphism in Hmong Individuals as a Potential Basis for Predisposition to Chronic Liver Disease. Cancer. 2017 doi: 10.1002/cncr.31122. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]