Abstract
Objective:
To estimate the prevalence, comorbidities, and service use of people with autism spectrum disorders (ASDs) based on data from Quebec Integrated Chronic Diseases Surveillance System (QICDSS).
Methods:
We included all residents up to age 24 eligible for health plan coverage who were in Quebec for at least 1 day from January 1, 1996, to March 31, 2015. To be considered as having an ASD, an individual had to have had at least 1 physician claim or hospital discharge abstract from 2000 to 2015 indicating one of the following ASD diagnosis codes: ICD-9 codes 299.0 to 299.9 or their ICD-10 equivalents.
Results:
The QICDSS shows that the prevalence of ASD has risen steadily over the past decade to approximately 1.2% (n = 16,940) of children and youths aged 1 to 17 years in 2014 to 2015. The same prevalence was obtained using Ministry of Education data. Common medical comorbidities included congenital abnormalities of the nervous system, particularly in the first year of life. Psychiatric comorbidity was much more highly prevalent, especially common mental disorders like anxiety and attention-deficit/hyperactivity disorder. Children and youths with ASDs made on average 2.3 medical visits per year compared with 0.2 in the general population. Between 18 and 24 years old, the mental health needs of individuals with ASDs were met less by medical specialists and more by general practitioners.
Conclusion:
Information derived from this database could support and monitor development of better medical services coordination and shared care to meet the continuous and changing needs of patients and families over time.
Keywords: autism spectrum disorders, child and adolescent psychiatry, comorbidity, epidemiology, mental health services
Abstract
Objectif:
Estimer la prévalence, les comorbidités et l’utilisation des services des personnes souffrant des troubles du spectre de l’autisme (TSA) d’après les données du Système intégré de surveillance des maladies chroniques du Québec (SISMACQ).
Méthodes:
Nous avons inclus tous les résidents de 24 ans et moins admissibles au régime d’assurance-maladie qui étaient au Québec au moins 1 journée entre le 1er janvier 1996 et le 31 mars 2015. Pour être considérée comme souffrant de TSA, une personne devait avoir au moins une confirmation d’un médecin ou un registre des congés d’hôpitaux de 2000 à 2015 indiquant l’un des codes suivants du diagnostic de TSA: les codes 299,0 à 299,9 de la CIM-9 ou leurs équivalents de la CIM-10.
Résultats:
Le SISMACQ indique que la prévalence des TSA a augmenté régulièrement au cours des 10 dernières années pour toucher approximativement 1,2% (n = 16 940) des enfants et des adolescents âgés de 1 à 17 ans, en 2014-2015. La même prévalence a été obtenue à l’aide des données du ministère de l’Éducation. Les comorbidités médicales communes étaient notamment les anomalies congénitales du système nerveux, particulièrement dans la première année de vie. La prévalence de la comorbidité psychiatrique était beaucoup plus élevée, spécialement les troubles mentaux communs comme l’anxiété et le trouble de déficit de l’attention avec hyperactivité. Les enfants et les adolescents souffrant de TSA faisaient en moyenne 2,3 visites médicales par année, comparativement à 0,2 dans la population générale. Entre 18 et 24 ans, les besoins de santé mentale des personnes souffrant de TSA étaient satisfaits moins par des spécialistes médicaux et davantage par des omnipraticiens.
Conclusion:
L’information tirée de cette base de données pourrait soutenir et surveiller le développement d’une meilleure coordination des services médicaux et des soins partagés pour répondre aux besoins sans cesse changeants des patients et des familles avec le temps.
The prevalence of diagnosed autism spectrum disorders (ASDs) has been on the rise since the late 1960s, with recent studies reporting a prevalence of 1%.1,2 The US Centers for Disease Control and Prevention (CDC) estimated a bigger prevalence of ASDs at 14.6 per 1000 eight-year-old children in 2012, but the rate varied considerably across regions, with as much as a 3-fold difference between sites, possibly reflecting disparities in access to specialised services.3 Uncertainties remain regarding the generalisability of results as the CDC database does not provide a representative sample of the entire US population. It is therefore preferable to use data from whole population registries to assess prevalence and associated medical conditions.4
Studies of medical health records have shown that more than half of children with ASDs have at least 1 comorbid disorder5–9 and that 41% have 2 or more.8 Several health problems (psychiatric10–15 and medical16–21) are significantly more prevalent among individuals with ASDs than in the general population, with a mortality risk approximately 2 to 3 times greater than among same-sex peers in the general population.21 However, most studies of the association between ASDs and other health conditions were carried out with small samples8–10,22 generally drawn from specialised care settings.6,7,19,23 The few studies that have used a nationwide population administrative health database examined a narrow range of comorbidities.5,13,16,17,20
Health service utilisation records indicate that, compared with children without ASDs, those with ASDs make more medical visits, make longer-term use of medication, have a greater need for treatment and psychological counseling, and are much more likely to receive physical or language therapy.13 As adolescents with ASDs grow into adulthood, delivery of their specialised care passes from paediatricians and child psychiatrists to general practitioners supported by adult mental health specialists. However, there is limited information on this transition to adult care and the health service use of people diagnosed with ASD into adulthood.24–28
Canada’s universal health care system covers 99% of the population. It is administered by the provinces, and physicians are mostly self-employed and paid on a fee-for-service basis.29 The Public Health Agency of Canada (PHAC) has been operating a Chronic Disease Surveillance System (CCDSS) with aggregated administrative health data from each province.30 The Quebec Integrated Chronic Disease Surveillance System (QICDSS) covers a population of 8.2 million31 and collects information on prevalence, incidence, mortality, and service use associated with health issues.
Against this background, we undertook a study with the following objectives:
Estimate the prevalence of ASD from QICDSS administrative data and compare it to the rate obtained from Quebec Ministry of Education, Recreation and Sports (MELS) data
Examine the prevalence and type of comorbidity associated with ASDs
Describe the service utilisation profiles of people with ASDs
Methods
Data Sources
The present study analysed longitudinal anonymized data from the QICDSS, which links the following 5 administrative health data sets31: 1) the health insurance registry, which provides information on demographics and health insurance eligibility; 2) the physician claims database of all services billed to the provincial health plan, which includes information on diagnoses, procedures performed, and service setting (i.e., private office, emergency room, etc.); 3) the hospitalisation discharge database, which covers diagnoses and procedures received; 4) the vital statistics and death certificates database; and 5) the pharmaceutical services database, which covers prescription drug services received by Quebec residents aged 65 and older. The QICDSS contains data on all Quebec residents eligible for provincial health insurance. The International Classification of Diseases, Ninth Revision (ICD-9) was used to code diagnoses in the physician billing database for the entire observation period. In the hospitalisation database, the ICD-9 was used for the period up to March 31, 2006, and the tenth revision (ICD-10) was used thereafter.
Case Identification
We included all residents aged 24 and younger eligible for health care coverage who were in Quebec at least 1 day from January 1, 1996, to March 31, 2015. To be considered to have an ASD, an individual had to have at least 1 physician claim or hospital discharge abstract from 2000 to 2015 indicating one of the following: ICD-9 codes 299.0 to 299.9 or their ICD-10 equivalents, F84.0 to F84.9. It is noted that these codes include childhood disintegrative disorder and Retts syndrome, which are not perceived as an ASD in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). We have nevertheless included them because this longitudinal study covers the transition from the DSM-4 to DSM-5. Our case definition fits the one validated by Dodds et al.32
The ICD-9 codes used to identify comorbid conditions are presented in Table 1 (see first column). A case was considered as incident in the first year a diagnosis was recorded. A prevalent case was defined from the first year of diagnosis and remained a case thereafter.
Table 1.
Comorbidities of People Aged 1 to 17 Years, with and without ASDs, in First Year of Life and Lifetime, Quebec, 2014 to 2015.
| First Year of Life | Lifetime | |||||||
|---|---|---|---|---|---|---|---|---|
| With ASD (n =16,940) | Without ASD (n =1,447,660) | With ASD (n = 16,940) | Without ASD (n = 1,447,660) | |||||
| Comorbidity (ICD-9 Codes) | Prevalence (%) | 99% CI | Prevalence (%) | 99% CI | Prevalence (%) | 99% CI | Prevalence (%) | 99% CI |
| Endocrine, nutritional and metabolic diseases, and immunity disorders (240-279) | 7.1 | 6.6-7.7 | 3.7 | 3.7-3.7 | 24.9 | 23.9-25.9 | 12.4 | 12.3-12.4 |
| Mental disorders (290-319) | 85.2 | 83.4-87.0 | 25.3 | 25.2-25.4 | ||||
| Substance use disorders (291-292 and 303-305) | 2.1 | 1.8-2.4 | 0.7 | 0.6-0.7 | ||||
| Anxio-depressive disorders (296, 300, 311, 313) | 34.2 | 33.1-35.4 | 7.7 | 7.6-7.7 | ||||
| Behavioral disorders (301, 302, 312) | 13.2 | 12.5-13.9 | 2.2 | 2.1-2.2 | ||||
| Attention-deficit hyperactivity disorder (314) | 42.0 | 40.7-43.3 | 9.3 | 9.2-9.3 | ||||
| Developmental delay (315 and 317-319) | 57.1 | 55.6-58.6 | 8.4 | 8.3-8.4 | ||||
| Intellectual disability (317-319) | 6.0 | 5.5-6.5 | 0.2 | 0.2-0.2 | ||||
| Epilepsy (345) | 1.3 | 1.1-1.5 | 0.3 | 0.3-0.3 | 8.4 | 7.9-9.0 | 1.3 | 1.3-1.3 |
| Disorders of the eye and adnexa (360-379) | 15.1 | 14.4-15.9 | 9.9 | 9.9-10.0 | 42.9 | 41.6-44.2 | 27.9 | 27.8-28.0 |
| Diseases of the ear and mastoid process (380-389) | 30.0 | 28.9-31.1 | 27.8 | 27.7-27.9 | 83.1 | 81.3-84.9 | 69.6 | 69.4-69.8 |
| Diseases of the circulatory system (390-459) | 4.9 | 4.4-5.3 | 2.6 | 2.6-2.7 | 14.3 | 13.5-15.0 | 7.7 | 7.6-7.7 |
| Diseases of the respiratory system (460-519) | 56.9 | 55.4-58.4 | 51.3 | 51.2-51.5 | 92.7 | 90.8-94.6 | 84.0 | 83.8-84.2 |
| Diseases of the digestive system (520-579) | 28.3 | 27.2-29.3 | 20.2 | 20.1-20.3 | 63.3 | 61.7-64.9 | 45.5 | 45.3-45.6 |
| Diseases of the genitourinary system (580-629) | 11.3 | 10.7-12.0 | 6.8 | 6.8-6.9 | 38.4 | 37.2-39.6 | 28.1 | 28.0-28.2 |
| Congenital anomalies (740-759) | 20.7 | 19.8-21.6 | 13.6 | 13.5-13.7 | 34.1 | 32.9-35.3 | 20.1 | 20.0-20.2 |
| Trauma (800-999) | 15.2 | 14.4-16.0 | 11.7 | 11.6-11.8 | 69.0 | 67.4-70.7 | 55.5 | 55.3-55.6 |
ASD, autism spectrum disorder; CI, confidence interval; ICD-9, International Classification of Diseases, Ninth Revision.
We used the following hierarchy to characterise health service use: a) inpatient care, b) nursing home/care center care, c) emergency room visits, d) outpatient psychiatric contacts, e) outpatient pediatric contacts, f) general practitioner office, and g) other medical specialist. In this scheme, a person hospitalised in the past year was included only in the “hospitalisation” category even though he or she might have visited a hospital emergency room or a paediatrician. Our prevalence results by region were validated against the prevalence estimates compiled by the MELS for children aged 4 to 17 years. Public education is mandatory until age 16 in Quebec, and the MELS keeps track of all children residing in the province.
Regarding the data quality of the QICDSS, psychiatrists and paediatricians entered the ICD-9 code in billing files in 95% of cases, and an internal medicine diagnosis code was indicated in 94% of claims.
Moreover, the MELS data, against which we compared our results, covered all students aged 4 to 17 years with ASDs evaluated by a psychiatrist, child psychiatrist, or physician as part of a multidisciplinary team.33,34 The data related to the 2014 to 2015 school years. Children’s age was estimated from their school grade. ASD prevalence was calculated from the ratio of “total number of students with ASD in a school year” to “total number of students in the school year” multiplied by 10,000.
Data Analysis
We used lifetime prevalence, which meant that a person who met the case definition at any age from birth to the end of the observation period was counted as a case. Annual incidence refers to the rate of new cases of ASDs identified in the population over a year. Comparisons over time and between regions were made using age-adjusted measures. Rates were directly standardised according to the age structure of the population of Quebec in 2001 and were derived for 15 regions of Quebec. To compare differences in ASD prevalence between regions, rates were estimated for people aged 4 to 17 years using QICDSS and MELS data.33,34 Prevalence of comorbid diseases (with 99% confidence interval) was calculated among people who used health services for ASDs and compared against the prevalence of these diseases among people who did not use such services (general population). This was carried out for 2 time frames: first year of life and after the first year of life. However, analyses of comorbidities were restricted to individuals aged 1 to 17 years because information from birth might be missing for older subjects given the QICDSS database was set up in 1996. We identified service utilisation based on service location and type of physician seen (i.e., general practitioner, psychiatrist, paediatrician, or other medical specialist). A distinction was made between office and hospital-based care, and the latter was subdivided into outpatient appointment, emergency room visit, or inpatient care. Hospital data took precedence over community-based care, and inpatient data took precedence over outpatient data. This hierarchy took into account that a given individual could consult various professionals or use various health services over a given period of time.
Results
Lifetime Prevalence and Annual Incidence of ASDs
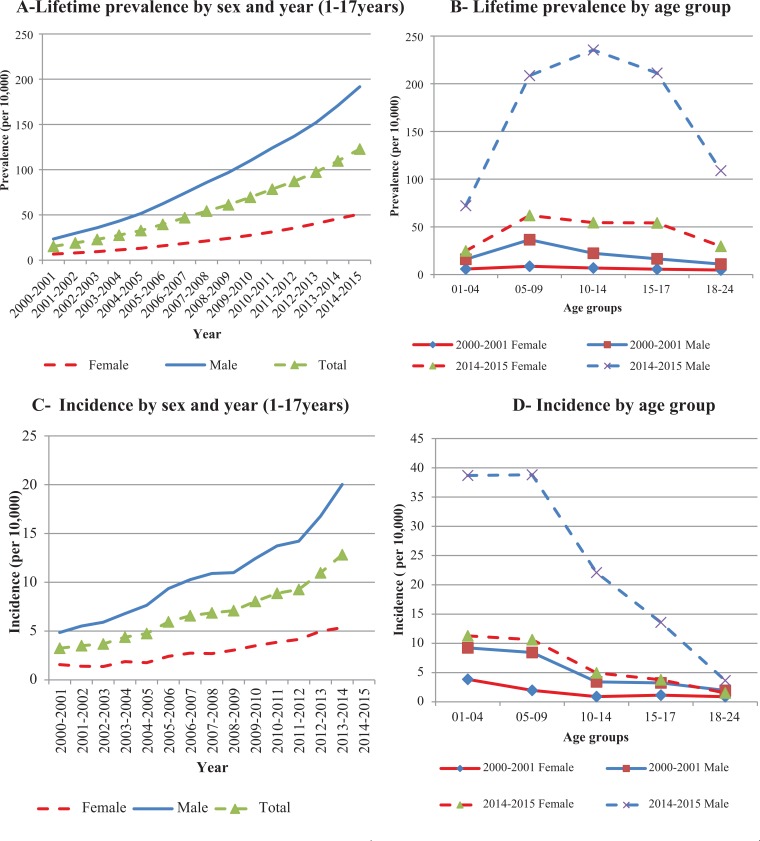
The prevalence of ASDs was about 1.2%, representing 16,940 children aged 1 to 17 years in 2014 to 2015 (Figure 1A). Prevalence increased from 15 per 10,000 in 2000-2001 to 122 per 10,000 in 2014-2015, was higher among boys, and was highest in the 5- to 14-year age group (Figure 1B). The Ministry of Education data yielded exactly the same provincial crude prevalence rate of 1.3% (see Quebec in graph of supplementary file).
Figure 1.
Lifetime prevalence and annual incidence of autism spectrum disorders by sex, year, and age group.
Figure 1C shows the annual incidence of ASDs from 2000-2001 to 2014-2015. In 2014 to 2015, the incidence was 19 per 10,000, which translated into 2758 newly diagnosed cases in the population aged 17 and younger. Incidence among boys was 4 times as high as among girls. ASDs were generally diagnosed before age 10 (Figure 1D).
The QICDSS and MELS data were remarkably similar for some regions but very different for others (see graph in supplementary file). For instance, in 2014 to 2015, the lifetime prevalence reported by the QICDSS for Estrie (155 vs. 61 per 10,000), Bas-St Laurent (125 vs. 88 per 10,000) and the Outaouais (112 vs. 80 per 10,000) were very high compared to those of the MELS. However, the MELS database reported higher rates than QICDSS for some regions such as Montérégie (205 vs. 183 per 10,000) Laval (172 vs. 152 per 10,000), and Lanaudière (126 vs. 104 per 10,000). In general, the Montreal metropolitan area, which accounts for nearly half of Quebec’s population, had the highest prevalence rates, followed by more semiurban and smaller regions. Similarly, although ASD prevalence did vary somewhat for certain regions depending on data source, the difference in the number of cases observed between the QICDSS (16,010 children aged 4-17 years) and MELS (13,275 children aged 4-17 years) data did not alter the ordinal ranking of the regions significantly.
Comorbidity Associated with ASDs
Table 1 compares levels of medical and psychiatric comorbidity in people with ASDs to those in the remaining population (without ASDs). It presents both first-year-of-life and lifetime prevalence. Overall, the proportion of individuals with at least one of the diagnoses was higher among people with ASDs than in the general population, irrespective of the condition of interest. In the first year of life, this difference was more pronounced for diseases of the digestive system, congenital anomalies, and perinatal disorders. Later in life, a higher proportion of people with ASDs had a mental disorder compared with the general population, and this was true also for specific conditions, including developmental delay, attention-deficit hyperactivity disorder, and anxio-depressive disorders. The frequency of congenital anomalies, behavioral disorders, intellectual disability, and epilepsy was also higher among people with ASDs.
Service Utilisation
People with ASDs had on average more than twice as many health service contacts (5.8 vs. 2.7), most commonly for reasons of mental illness (2.3 vs. 0.2), compared with those without ASDs (data not shown). The mental health service utilisation profile of people with ASDs indicated that before age 10, ASDs were initially diagnosed by paediatricians, followed by psychiatrists; the inverse was true after age 10 (Table 2).
Table 2.
Autism Spectrum Disorder Incident Cases 1 to 24 Years Old, by Type of Diagnosing Physician on First Visit and Age Group, Quebec, 2014 to 2015.
| Age Group, y | Type of Diagnosing Physician on First Visit, n (%) | ||||
|---|---|---|---|---|---|
| Psychiatrist | Paediatrician | General practitioner | Other Specialist | Total | |
| 1-4 | 75 (8.2) | 644 (70.2) | 123 (13.4) | 76 (8.3) | 918 (100.0) |
| 5-9 | 221 (20.1) | 652 (59.3) | 182 (16.6) | 45 (4.1) | 1100 (100.0) |
| 10-14 | 188 (35.7) | 259 (49.2) | 67 (12.7) | 13 (2.5) | 527 (100.0) |
| 15-17 | 104 (48.8) | 69 (3.4) | 30 (14.1) | 10 (4.7) | 213 (100.0) |
| 18-24 | 97 (51.6) | 15 (8.0) | 66 (35.1) | 10 (5.3) | 188 (100.0) |
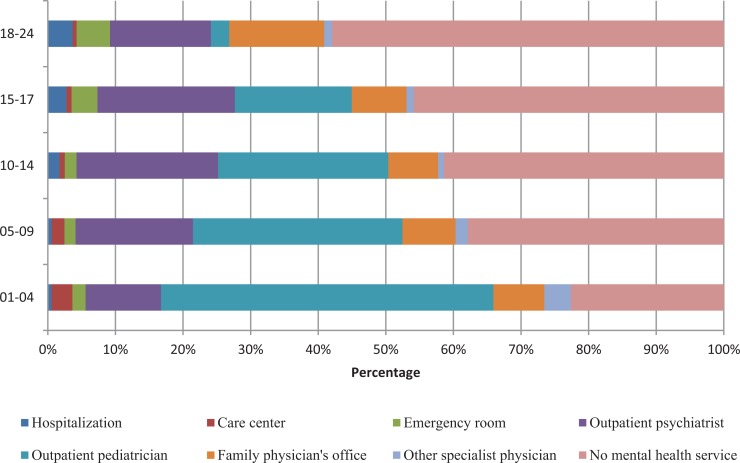
People with ASDs consulted mostly psychiatrists and paediatricians and were more likely than individuals without ASDs to be hospitalised or seen in emergency settings (Table 3). With age, individuals with ASDs received fewer mental health services, and the role of family physicians increased (Figure 2).
Table 3.
Hierarchical Mental Health Service Utilisation Profile of People with and without ASD, 1-24 Years of Age, Quebec, 2014 to 2015.a
| Mental Health Services | With ASD | Without ASD | ||
|---|---|---|---|---|
| % | 99% CI | % | 99% CI | |
| Hospitalisation | 1.9 | 1.7-2.2 | 0.3 | 0.2-0.3 |
| Care center | 1.2 | 1.0-1.4 | 0.1 | 0.1-0.1 |
| Emergency room | 2.8 | 2.5-3.1 | 0.8 | 0.8-0.8 |
| Outpatient psychiatrist | 17.7 | 17.0-18.5 | 1.0 | 1.0-1.0 |
| Outpatient paediatrician | 22.3 | 21.5-23.1 | 3.0 | 2.9-3.0 |
| Family physician’s office | 9.2 | 8.7-9.7 | 4.0 | 4.0-4.0 |
| Other medical specialist | 1.5 | 1.3-1.7 | 0.2 | 0.2-0.2 |
| None | 43.4 | 42.3-44.6 | 90.7 | 90.5-90.9 |
aASD, autism spectrum disorder; CI, confidence interval.
Figure 2.
Hierarchical mental health service utilization profile of persons with autism spectrum disorders by age group, 2014 to 2015.
Discussion
Our findings support the value of the QICDSS as a register for ASDs. This database covers 96% to 99% of all insured individuals, accounting for 99% of the Quebec population. Unlike previous work carried out in the United States, Finland, and Thailand,13,16,17,20 our study was not restricted to an age group or localised areas. As our databases covered practically the entire population, it allowed us to obtain a representative prevalence of ASDs in Quebec by age group and region and to investigate population-based determinants that can vary between or within regions. Quebec’s school board registers had been used previously to study the prevalence and possible determinants of neuro-developmental disorders.35 We demonstrate here that linked health administrative databases produced similar prevalence and captured regional differences attributed to school services availability.
The QICDSS shows that ASDs have risen steadily over the past decade, reaching a lifetime prevalence of 12.2 per 1000 persons aged 17 years and younger in 2014 to 2015. This is comparable to existing data that have yielded prevalence rates of 0.6% to 1.1%.1 However, compared with the CDC’s data for 2012 (14.6 per 1000 children 8 years of age),3 we obtained a slightly lower prevalence for children 8 years old (12.3 per 1000 in 2012). The annual incidence rate followed the same growth trend over time and was estimated at 1.9% in 2014 to 2015. The predominance of boys over girls is also consistent with results from previous epidemiological studies.2 However, there was a 3-fold variation in prevalence rates across regions of the province, with the Montreal metropolitan area registering the highest. This is consistent with an Australian study that showed people living in rural areas had a lower prevalence of ASDs, possibly because of lower service availability.36 Rates have been shown to vary also in the United States (e.g., in an area where both education and health care records were reviewed, 12.2 per 1000 in South Carolina vs. 24.6 per 1000 in New Jersey, a 2-fold difference).3 The sites that used both education and health care records reported a higher prevalence than did sites that used only health care records. The provincial estimates from the 2 data sources (i.e., health-QICDSS and education ministries–MELS) were remarkably similar. This might be explained by the fact that school boards require that a child be diagnosed with an ASD before receiving school-based specialised services for ASDs.33,34 The disparity in overall numbers between the 2 data sets may reflect the possibility that the additional cases in the QICDSS include cases such as Asperger’s syndrome, and these individuals do not receive services in school.
As reported in other research, people with ASDs had greater comorbidity, although this varied by comorbid disorder and life stage.5–10,13,16,17,20 Some comorbidities were particularly common in the first year of life, while others were diagnosed only later. The prevalence of comorbidity observed among individuals with ASDs in other studies has varied, but this could be explained by differences in research methodology. The sampling frame is a capital factor, as studies that used a clinical sample have tended to overestimate the association between comorbidities and ASDs. Variations may also be due to diagnostic practices. In the QICDSS, diagnoses are formulated mainly by paediatricians and psychiatrists, as is the case in clinical sample studies. These health professionals may be reluctant to formulate a diagnosis of “intellectual disability” for children with ASDs lest it result in these children being denied special school services. Instead, they may prefer to hand down an ICD-9 diagnosis of “developmental delay.”3 This would explain why prevalence is much lower for intellectual disability than for developmental delay (Table 1).
Average number of medical contacts was twice as high among people with ASDs as in the general population. This might be explained by the greater prevalence of comorbidity among people with ASDs.13 However, the pattern changed over time: most of the younger people saw psychiatrists and paediatricians, but use of specialist mental health services decreased considerably in young adulthood. This finding echoes concern raised in the recent literature to the effect that the transition to adulthood is associated with a break in continuity of care provided by the health system for people with mental disorders.25,27 Another explanation could be that the core symptoms of ASDs37,38 improve to such an extent over time as to no longer require specialist services.
The QICDSS constitutes an inestimable source of information for the surveillance of ASDs given that it documents all health care services used by the Quebec population.31
However, it is not without limitations. First, as the QICDSS was designed for administrative purposes, it may be subject to a recording bias, especially regarding diagnosis. Databases and case definitions need to be validated before they can be used for epidemiological purposes.39–41 However, studies have shown that diagnoses recorded in medical records fully corresponded to entries in administrative databases for other diseases, in Quebec as in other provinces.40,42 In addition, Dodds et al.32 reported that administrative health databases can clearly identify children with autism. Second, since QICDSS data only include information on people who use health care services, the case definition only identifies people who have received a diagnosis or treatment from a physician. However, individuals with ASDs can also be treated by other professionals, including resource teachers, speech-language pathologists, and psychologists, both in schools and in private clinics. The QICDSS does not cover these cases and cannot report them. We partly addressed this issue by comparing the results from the QICDSS with rates from the MELS, which include diagnoses made by psychologists and speech-language pathologists working in both public and private schools. This gave similar rates for most regions, although we accept that this does not include psychologists and speech-language pathologists working in the community. We would suggest that although administrative data probably underestimate the prevalence of ASDs, they are still useful for identifying temporal and regional trends among treated cases.
Conclusion
Our research confirms that ASDs have risen steadily in terms of prevalence and incidence and that they vary considerably across regions. It also demonstrates the QICDSS’s capacity to identify associated comorbidities and their associated risk factors. Furthermore, the measurement of health service utilisation (for mental and other health reasons) across the life trajectory of this disorder beginning in the first years of life may shed light on the specific needs of people with ASDs and on possible deficits in the service offer.
Our results may have implications for future research. These include exploring the etiology of ASDs and the excess mortality found in this condition, as well as investigating the association between variations in health service availability and the prevalence of ASDs. Finally, the QICDSS is a surveillance system similar to those of other Canadian provinces that provide aggregated data to the PHAC’s CCDSS, and this could serve as a model for nationwide surveillance, service planning, evaluation, and research on ASDs.
Supplemental Material
Supplemental Material, CPA737031_supplementary_ASD_graphs for Prevalence and Correlates of Autism Spectrum Disorders in Quebec by Fatoumata Binta Diallo, Éric Fombonne, Steve Kisely, Louis Rochette, Helen-Maria Vasiliadis, Alain Vanasse, Manon Noiseux, Éric Pelletier, Johanne Renaud, Danielle St-Laurent, and Alain Lesage in The Canadian Journal of Psychiatry
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Canadian Institutes of Health Research (CIHR). The authors have no financial relationships relevant to this article to disclose. The authors also acknowledge financial support from a contract by the Public Health Agency of Canada (PHAC). The results and conclusions are those of the authors and no official endorsement by the Public Health Agency of Canada is intended or should be inferred.
Supplemental Material: Supplementary material for this article is available online.
References
- 1. Anagnostou E, Zwaigenbaum L, Szatmari P, et al. Autism spectrum disorder: advances in evidence-based practice. CMAJ. 2014;186(7):509–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fombonne E, Quirke S, Hagen A. Epidemiology of pervasive developmental disorders In: Amaral D, Geschwind D, Dawson G, editors. Autism spectrum disorders. Oxford (UK): Oxford University Press; 2011. p. 90–111. [Google Scholar]
- 3. Centers for Disease Control and Prevention. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2012. MMWR Surveill Summ. 2016;65(3):1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ouellette-Kuntz H, Coo H, Yu CT, et al. Status report—National Epidemiologic Database for the Study of Autism in Canada (NEDSAC). Chronic Dis Inj Can. 2012;32(2):84–89. [PubMed] [Google Scholar]
- 5. Lundstrom S, Reichenberg A, Melke J, et al. Autism spectrum disorders and coexisting disorders in a nationwide Swedish twin study. J Child Psychol Psychiatry. 2015;56(6):702–710. [DOI] [PubMed] [Google Scholar]
- 6. Noterdaeme MA, Hutzelmeyer-Nickels A. Comorbidity in autism spectrum disorders—II. Genetic syndromes and neurological problems [in German]. Z Kinder Jugendpsychiatr Psychother. 2010;38(4):267–272. [DOI] [PubMed] [Google Scholar]
- 7. Noterdaeme MA, Wriedt E. Comorbidity in autism spectrum disorders—I. Mental retardation and psychiatric comorbidity [in German]. Z Kinder Jugendpsychiatr Psychother. 2010;38(4):257–266. [DOI] [PubMed] [Google Scholar]
- 8. Simonoff E, Pickles A, Charman T, et al. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. [DOI] [PubMed] [Google Scholar]
- 9. van Steensel FJ, Bogels SM, de Bruin EI. Psychiatric comorbidity in children with autism spectrum disorders: a comparison with children with ADHD. J Child Fam Stud. 2013;22(3):368–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Berenguer-Forner C, Miranda-Casas A, Pastor-Cerezuela G, et al. Comorbidity of autism spectrum disorder and attention deficit with hyperactivity: a review study [in Spanish]. Rev Neurol. 2015;60(suppl 1):S37–S43. [PubMed] [Google Scholar]
- 11. Chakrabarti S, Fombonne E. Pervasive developmental disorders in preschool children: confirmation of high prevalence. Am J Psychiatry. 2005;162(6):1133–1141. [DOI] [PubMed] [Google Scholar]
- 12. Fombonne E. Epidemiological surveys of autism and other pervasive developmental disorders: an update. J Autism Dev Disord. 2003;33(4):365–382. [DOI] [PubMed] [Google Scholar]
- 13. Gurney JG, McPheeters ML, Davis MM. Parental report of health conditions and health care use among children with and without autism: National Survey of Children’s Health. Arch Pediatr Adolesc Med. 2006;160(8):825–830. [DOI] [PubMed] [Google Scholar]
- 14. van Steensel FJ, Bogels SM, Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clin Child Fam Psychol Rev. 2011;14(3):302–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Yeargin-Allsopp M, Rice C, Karapurkar T, et al. Prevalence of autism in a US metropolitan area. JAMA. 2003;289(1):49–55. [DOI] [PubMed] [Google Scholar]
- 16. Chen CY, Chen KH, Liu CY, et al. Increased risks of congenital, neurologic, and endocrine disorders associated with autism in preschool children: cognitive ability differences. J Pediatrics. 2009;154(3):345–350, 50.e1. [DOI] [PubMed] [Google Scholar]
- 17. Chen M, Su TP, Chen YS, et al. Comorbidity of allergic and autoimmune diseases in patients with autism spectrum disorder: a nationwide population-based study. Res Autism Spectr Disord. 2013;7(2):205–212. [Google Scholar]
- 18. Frye RE. Metabolic and mitochondrial disorders associated with epilepsy in children with autism spectrum disorder. Epilepsy Behav. 2015;47:147–157. [DOI] [PubMed] [Google Scholar]
- 19. Kohane IS, McMurry A, Weber G, et al. The co-morbidity burden of children and young adults with autism spectrum disorders. PLoS One. 2012;7(4):e33224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Timonen-Soivio L, Sourander A, Malm H, et al. The association between autism spectrum disorders and congenital anomalies by organ systems in a Finnish national birth cohort. J Autism Dev Disord. 2015;45(10):3195–3203. [DOI] [PubMed] [Google Scholar]
- 21. Woolfenden S, Sarkozy V, Ridley G, et al. A systematic review of two outcomes in autism spectrum disorder—epilepsy and mortality. Dev Med Child Neurol. 2012;54(4):306–312. [DOI] [PubMed] [Google Scholar]
- 22. Evans DW, Canavera K, Kleinpeter FL, et al. The fears, phobias and anxieties of children with autism spectrum disorders and Down syndrome: comparisons with developmentally and chronologically age matched children. Child Psychiatry Hum Dev. 2005;36(1):3–26. [DOI] [PubMed] [Google Scholar]
- 23. Salazar F, Baird G, Chandler S, et al. Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. J Autism Dev Disord. 2015;45(8):2283–2294. [DOI] [PubMed] [Google Scholar]
- 24. Read N, Schofield A. Autism: are mental health services failing children and parents? J Fam Health Care. 2010;20(4):120–124. [PubMed] [Google Scholar]
- 25. Watson R, Parr JR, Joyce C, et al. Models of transitional care for young people with complex health needs: a scoping review. Child Care Health Dev. 2011;37(6):780–791. [DOI] [PubMed] [Google Scholar]
- 26. Russell AJ, Murphy CM, Wilson E, et al. The mental health of individuals referred for assessment of autism spectrum disorder in adulthood: a clinic report. Autism. 2016;20(5):623–627. [DOI] [PubMed] [Google Scholar]
- 27. Kuhlthau KA, Warfield ME, Hurson J, et al. Pediatric provider’s perspectives on the transition to adult health care for youth with autism spectrum disorder: current strategies and promising new directions. Autism. 2015;19(3):262–271. [DOI] [PubMed] [Google Scholar]
- 28. Cadman T, Eklund H, Howley D, et al. Caregiver burden as people with autism spectrum disorder and attention-deficit/hyperactivity disorder transition into adolescence and adulthood in the United Kingdom. J Am Acad Child Adolesc Psychiatry. 2012;51(9):879–888. [DOI] [PubMed] [Google Scholar]
- 29. Mossialos E, Wenzl M, Osborn R, et al. 2015 International profiles of health care systems. Washington, DC: The Commonwealth Fund; 2016. [Google Scholar]
- 30. Public Health Agency of Canada. Report from the Canadian Chronic Disease Surveillance System: mental illness in Canada 2015. Ottawa (Canada): Ministry of Health, Government of Canada; 2015. Available from: http://healthycanadians.gc.ca/publications/diseases-conditions-maladies-affections/mental-illness-2015-maladies-mentales/index-eng.php. Accessed August 17, 2017. [Google Scholar]
- 31. Blais C, Jean S, Sirois C, et al. Quebec Integrated Chronic Disease Surveillance System (QICDSS), an innovative approach. Chronic Dis Inj Can. 2014;34(4):226–235. [PubMed] [Google Scholar]
- 32. Dodds L, Spencer A, Shea S, et al. Validity of autism diagnoses using administrative health data. Chronic Dis Can. 2009;29(3):102–107. [PMC free article] [PubMed] [Google Scholar]
- 33. Noiseux M. Surveillance des troubles envahissants du développement chez les enfants de 4 à 17 ans de la Montérégie, 2000-2001 à 2007-2008 Direction de santé publique de la Montérégie. Longueuil (Canada): Direction de santé publique de la Montérégie; 2009. [Google Scholar]
- 34. Noiseux M. Prévalence du TSA: la Montérégie en tête de peloton. Longueuil (Canada): Agence de la santé publique et des services sociaux de la Montérégie, Direction de santé publique, Surveillance de l’état de santé de la population; 2014.
- 35. Fombonne E, Zakarian R, Bennett A, et al. Pervasive developmental disorders in Montreal, Quebec, Canada: prevalence and links with immunizations. Pediatrics. 2006;118(1):e139–e150. [DOI] [PubMed] [Google Scholar]
- 36. Leonard H, Glasson E, Nassar N, et al. Autism and intellectual disability are differentially related to sociodemographic background at birth. PLoS One. 2011;6(3):e17875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Seltzer MM, Shattuck P, Abbeduto L, et al. Trajectory of development in adolescents and adults with autism. Ment Retard Dev Disabil Res Rev. 2004;10(4):234–247. [DOI] [PubMed] [Google Scholar]
- 38. Korkmaz B. Infantile autism: adult outcome. Semin Clin Neuropsychiatry. 2000;5(3):164–170. [DOI] [PubMed] [Google Scholar]
- 39. Hux JE, Ivis F, Flintoft V, et al. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. 2002;25(3):512–516. [DOI] [PubMed] [Google Scholar]
- 40. Jean S, Candas B, Belzile E, et al. Algorithms can be used to identify fragility fracture cases in physician-claims databases. Osteoporos Int. 2012;23(2):483–501. [DOI] [PubMed] [Google Scholar]
- 41. Lambert L, Blais C, Hamel D, et al. Evaluation of care and surveillance of cardiovascular disease: can we trust medico-administrative hospital data? Can J Cardiol. 2012;28(2):162–168. [DOI] [PubMed] [Google Scholar]
- 42. Ouhoummane N. Impact du diabète sur la mortalité à la suite d’une hospitalisation pour un premier infarctus aigu du myocarde au Québec Université Laval, QC; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, CPA737031_supplementary_ASD_graphs for Prevalence and Correlates of Autism Spectrum Disorders in Quebec by Fatoumata Binta Diallo, Éric Fombonne, Steve Kisely, Louis Rochette, Helen-Maria Vasiliadis, Alain Vanasse, Manon Noiseux, Éric Pelletier, Johanne Renaud, Danielle St-Laurent, and Alain Lesage in The Canadian Journal of Psychiatry