Abstract
Background:
Lateral meniscus posterior root tears (LMPRTs), if left untreated, can cause devastating effects to the knee, with rapid articular cartilage degeneration and loss of the meniscus as a secondary stabilizer. Detection and surgical repair of these defects have been linked to favorable outcomes, but preoperative identification of LMPRTs continues to be challenging.
Purpose:
To determine the rate of LMPRTs diagnosed preoperatively on magnetic resonance imaging (MRI) in a consecutive series of arthroscopically confirmed LMPRTs.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective cohort of 45 consecutive patients with arthroscopically confirmed LMPRTs between 2010 and 2017 were included in this study. The preoperative MRI report for each patient was evaluated and compared with intraoperative findings. Each preoperative MRI study was then reviewed by 2 fellowship-trained musculoskeletal radiologists who worked in consensus.
Results:
A total of 45 patients (32 males, 13 females) with arthroscopically confirmed LMPRTs and a mean age of 27 years (range, 14-54 years) were included in the study. Only 15 of 45 LMPRTs (33%) were initially diagnosed on preoperative MRI. Past or concurrent anterior cruciate ligament (ACL) reconstruction was present in 37 of 45 cases (82%). Upon retrospective review, 15 of the 30 missed LMPRTs were “clearly evident,” 12 “subtly evident,” and 3 “occult” (unavoidably missed). There were no significant differences in the rate of LMPRT diagnosis based on history of prior knee surgery, meniscus extrusion, or tearing of the meniscofemoral ligament.
Conclusion:
Despite improved identification of other meniscus tear patterns on MRI, a high percentage of LMPRTs were still missed. In the setting of previous ACL reconstruction, if the root cannot be confidently identified, the MRI interpretation should indicate that “the root is poorly visualized” to alert the surgeon to thoroughly evaluate this structure. The surgeon should maintain a high index of suspicion and carefully probe the posterior root of the lateral meniscus at the time of arthroscopy, especially in cases of ACL injury.
Keywords: meniscus root, lateral meniscus, magnetic resonance imaging, meniscus root tear
Lateral meniscus posterior root tears (LMPRTs) are clinically important injuries because of the role of the meniscus as a shock absorber and stabilizer for the knee.19,22,26 Meniscus insufficiency resulting from a posterior root tear increases joint contact pressures,15 especially with concomitant meniscofemoral ligament (MFL) disruption,10,13 leading to articular cartilage degeneration over time.25 In addition, root tears of the lateral meniscus have been shown in biomechanical studies to decrease knee stability due to loss of meniscus function as a secondary stabilizer.12,26 Outcomes of surgical repair of LMPRTs have been favorable1,3,15,17,23 but require specialized instrumentation and prolonged rehabilitation protocols as compared with other associated arthroscopic procedures.1,27 Therefore, the identification of LMPRTs on magnetic resonance imaging (MRI) is desirable for preoperative planning and discussion of postoperative rehabilitation with the patient.
In limited studies,6,16,20 the prevalence of LMPRTs among all patients who undergo arthroscopic knee surgery is approximately 3% to 7%; the rate increases to 7% to 15% for patients with anterior cruciate ligament (ACL) injuries.2,4,9,11 Patients with LMPRTs are 10 times more likely to have associated ACL tears than are patients with medial meniscus root tears.20 Despite these insights into the occurrence of LMPRTs, specific data on the accurate preoperative identification of LMPRTs remain lacking. In 2 studies,6,21 retrospective MRI review for LMPRTs demonstrated reasonably good sensitivity (71.8%-94%) and specificity (89%-98%) for diagnosis. However, such focused inspection of the posterior root structures may overestimate the actual prospective identification of these injuries. In another study, only 6 of 10 arthroscopically confirmed LMPRTs were diagnosed when a blinded review was performed on the preoperative MRI.16
The purposes of this study were to (1) identify the rate of preoperative MRI diagnosis in a consecutive series of arthroscopically confirmed LMPRTs, (2) determine the appearance and status of the LMPRT on MRI in retrospect, and (3) assess for secondary findings that may improve diagnosis of LMPRTs on MRI. Our hypothesis was that the majority of LMPRTs would be detected on preoperative MRI.
Methods
A retrospective cohort of 45 consecutive LMPRTs that were arthroscopically confirmed (Figure 1) between 2010 and 2017 was included in this study. Medical records of identified patients were reviewed for demographic information, associated injuries, previous operations, and imaging reports. The preoperative MRI report for each patient was evaluated and compared with intraoperative findings. The LMPRTs were defined as complete avulsions of the lateral meniscus posterior root or complete radial tears within 9 mm of the lateral meniscus attachment to the tibia.14 After being identified on arthroscopy, all LMPRTs were repaired with a transtibial pull-through technique.27
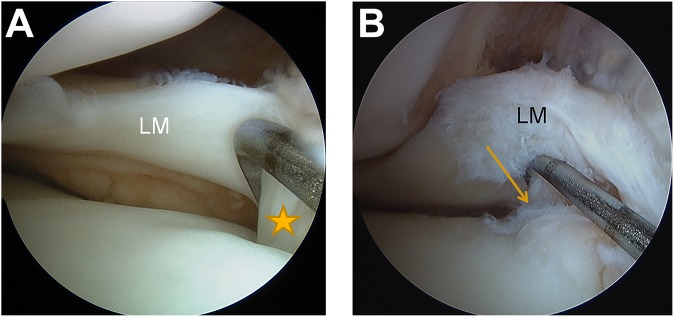
Figure 1.
Arthroscopic images of the lateral meniscus (LM) of the right knee in 2 patients. (A) LM viewed through the anterolateral portal, with the probe in the anteromedial portal, has an intact root (star) attached to the tibia. (B) Same view as panel A but in a different patient, demonstrating an LM posterior root tear (arrow) evident only when the probe is used to lift and inspect the LM root.
MRI Parameters
All MRI studies were retrospectively reviewed in consensus by 2 fellowship-trained musculoskeletal radiologists, with 19 and 10 years of experience (M.S.C. and N.S.M., respectively), working in consensus. Of 45 MRI examinations, 23 (51%) were imaged with a high–field strength magnet (3-T Signa HDX 16.0; GE Healthcare) with a dedicated 8-channel transmit-receive phased-array knee coil. Table 1 shows the standard knee MRI protocol utilized at our institution. Nineteen (42%) examinations were performed at 1.5-T field strength with the same parameters. The MRI protocols for cases performed outside our institution were similar, with few variations. In some cases, metal suppression techniques were utilized when metallic interference screws were present in the setting of prior ligament reconstruction.
TABLE 1.
Standard Knee Magnetic Resonance Imaging Positions and Parametersa
| Anatomic Plane | Sequence | TR/TE |
|---|---|---|
| Sagittal | Proton density weighted | 2200/18 |
| Sagittal, coronal, axial | Fat suppressed, intermediate weighted | 4000-6000/45 |
| Coronal | T1 weighted | 700-900/minimum |
aSlice thickness, 3 mm. TE, echo time; TR, repetition time.
Initial MRI Findings
The original MRI interpretations were provided preoperatively by fellowship-trained musculoskeletal radiologists at multiple institutions. The readings were then retrospectively compared with the intraoperative findings with regard to the presence, exact location, distribution, and configuration of meniscal tears involving the posterior root of the lateral meniscus. With the arthroscopic appearance as the test gold standard, the initial interpretation was designated as “diagnostic” or “missed.”
Consensus Review MRI Findings
All LMPRTs were more closely scrutinized and characterized by retrospective reinterpretation of the original MRI study via a dedicated high-resolution interactive picture archiving and communication system (PACS). The radiologists were aware of the operative findings at the time of re-review. The “2-slice-touch” rule described by De Smet and Tuite7 served as the primary finding for establishing the presence of a meniscal tear. This rule indicates that a meniscal tear is highly likely to be present if meniscal distortion or abnormal signal intensity extending to an articular surface is present on 2 or more MRIs. Each case that was missed at the time of original interpretation was further categorized on the basis of its MRI appearance at the time of re-review as “clearly evident,” “subtly evident,” or “occult” by strict application of the De Smet and Tuite7 criteria. Occult tears were defined as those that were unavoidably missed, as they could not be seen even during unblinded review. Clearly evident tears were readily apparent on multiple images. Subtly evident tears fit neither definition but were still visible on 2 or more MRIs, as evidenced by meniscal distortion or abnormal signal intensity extending to an articular surface. The 2 radiologists reviewed the images together and came to agreement on each designation.
The posterior root tears were further classified morphologically with anatomic criteria described by Forkel et al10,11 (Table 2). The imaging appearance of the MFL was also analyzed independently in all cases and described as normal, partially torn, or completely torn. If present, peripheral extrusion of the lateral meniscus midbody was assessed and measured on the coronal images as related to the peripheral osseous cortex of the lateral tibial plateau at the midportion of the lateral compartment. The presence or absence of focal bone marrow edema subjacent to the posterior root of the lateral meniscus was also observed and recorded. This was distinguished from more diffuse bone marrow edema involving the posterolateral tibia attributed to a pivot shift–type injury with the acute ACL injury.
TABLE 2.
| Type | Description of Tear Location and Pattern |
|---|---|
| 1 | Avulsion injury of the posterior lateral meniscus root with stable fixation of the meniscal posterior horn to the femur via the meniscofemoral ligament |
| 2 | A radial tear of the lateral meniscus posterior horn close to the root (between the root and the meniscal origin of the meniscofemoral ligament) |
| 3 | Complete detachment of the lateral meniscus posterior horn from its tibial and femoral attachments (root tear and rupture of the meniscofemoral ligament, functional loss of the meniscal ring) |
Statistical Analysis
Demographics and other characteristics of the LMPRT cases were described with counts and percentages for categorical variables and with means and ranges for continuous variables. The Fisher exact test was used for comparisons between the missed and diagnosed groups based on history of prior surgery, magnetic field strength, Forkel classification (type 2 vs type 3), presence of meniscus extrusion, and presence of a tear in the MFL. The level of significance was set at P < .05. All statistical analyses were performed with JMP Pro (v 10; SAS Institute Inc).
Results
Forty-five patients (32 males, 13 females) with arthroscopically confirmed LMPRTs and a mean age of 27 years (range, 14-54 years) were included in the study. Of 45 LMPRTs, 15 (33%) were diagnosed on preoperative MRI, while 30 (67%) examinations did not correctly identify a posterior root tear or avulsion. Of these, 12 reported a different tear in the lateral meniscus, most commonly in the posterior horn. Of the 30 missed cases, 16 had previous surgery in the same knee (11 of which were ACL reconstructions); 7 of the 15 diagnosed cases had undergone previous surgery. Overall, 16 of 45 (36%) patients had previously undergone ACL reconstruction. A history of prior surgery did not significantly increase the likelihood of missing the LMPRT (odds ratio [OR], 1.3; 95% CI, 0.4-4.5; P = .76). Median time from MRI to surgery was 43 days (mean, 81 days; range, 1-545 days). No patients reported a new knee injury between the MRI and the operation that confirmed the LMPRT. Thirty-two (71%) patients had a concomitant ACL tear procedure at the time of LMPRT repair: 21 underwent primary ACL reconstruction, 10 had revision ACL reconstruction, and 1 underwent ACL debridement. There were 10 patients out of the entire group who had a multiligament knee injury, and 4 of 10 LMPRTs were diagnosed in this subset.
The majority (84%) of MRI scans included in this study were performed from 2014 to 2017. Of 45 MRI scans, 26 (58%) were performed within 30 days of an acute injury, while 8 (18%) took place in a subacute setting (<12 months after injury). The remaining 11 imaging examinations were performed to evaluate chronic symptoms (instability, pain) following 1 or more previous surgical procedures. Twenty-three (51%) MRI scans were performed at 3-T field strength and 19 (42%) at 1.5 T, and 3 (7%) outside MRI evaluations did not have this information available; there was no significant association of MRI field strength (1.5 vs 3 T) with the likelihood of missing LMPRTs (OR, 2.9; 95% CI, 0.7-11.4; P = .19).
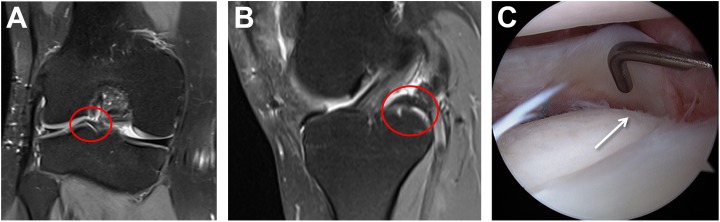
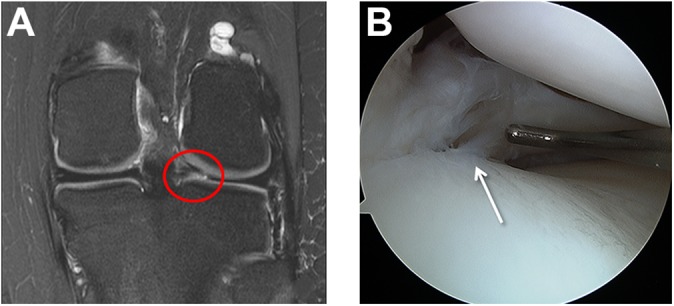
During the radiologists’ consensus review, the LMPRT was clearly evident in half of the missed cases (15 of 30) (Figure 2), subtly evident in 12 cases (Figure 3), and occult (Figure 4) in 3 cases. Among the 3 occult LMPRTs, 1 tear was truly not visible, and 2 were obscured by postoperative changes or metal artifact. When these 2 cases were excluded (ie, the 2-slice-touch rule could not be applied), 42 of 43 (98%) cases met the De Smet and Tuite7 criteria. When the root tears were assessed using the Forkel classification, 2 were graded as type 1, 10 as type 2, and 29 as type 3. There was no significant difference in the likelihood of missing the LMPRT diagnosis between type 2 and type 3 tears (OR, 2.8; 95% CI, 0.5-15.7; P = .28). Four cases were unable to be classified: 3 were absent or occult on imaging, and 1 was a complex case with an avulsion fracture.
Figure 2.
(A) Coronal T2-weighted magnetic resonance image of the left knee of a 16-year-old girl shows a “clearly evident” lateral meniscus posterior root tear (circled), as diagnosed on preoperative imaging and later confirmed (B) arthroscopically (arrow).
Figure 3.
Sequential coronal T2-weighted magnetic resonance images—(A) more posterior and (B) more anterior—of the left knee of a 33-year-old man demonstrate subtle irregularity and intermediate signal within an attenuated posterior root lateral meniscus (arrows). This tear was characterized as “subtly evident” by the reviewers. (C) The same meniscus tear (arrows) on subsequent arthroscopic examination.
Figure 4.
Twenty-seven-year-old woman with a history of multiple knee surgical procedures. T2-weighted magnetic resonance imaging demonstrated an “occult,” or unavoidably missed, tear (circled), even in consensus retrospective review of the (A) coronal and (B) sagittal views. (C) The patient was diagnosed with a lateral meniscus posterior root tear (arrow) during arthroscopic revision lateral meniscus repair.
In terms of associated imaging findings, there was no peripheral extrusion of the meniscus in 56% of the cases (25 of 45). Among the remaining cases, the mean extrusion was 2 mm (range, 1-4 mm), and 1 patient had a complete extrusion. The presence of meniscus extrusion made no significant difference in whether the LMPRT was diagnosed (OR, 1.87; 95% CI, 0.5-6.6; P = .36). The MFL showed varying changes: 26 partial tears, 7 complete tears, and 6 normal. The ligament was obscured because of postoperative changes or other artifact in the remaining 6 MRI scans. A torn MFL also made no significant difference in the diagnosis of LMPRTs (OR, 3.25; 95% CI, 0.3-31.1; P = .39). No cases demonstrated focal bone marrow edema changes. The bone edema pattern was generalized over a larger area in the posterolateral tibia, as is characteristic for pivot-shift ACL injury.
Discussion
Identification of LMPRTs on preoperative imaging is clinically important because of the role of the lateral meniscus posterior root in knee stability and articular cartilage protection.12,26 An appropriately identified meniscus root tear prior to surgery allows the surgeon to plan for the necessary operative time and surgical equipment to repair the meniscus. In addition, this knowledge facilitates an informed consent and discussion with the patient prior to surgery about the altered postoperative rehabilitation with protected weightbearing on crutches for 6 weeks.1,27 Currently, little data focus on the preoperative rate of diagnosis for LMPRTs. The main finding of this study is the high frequency (67%) of tears that were missed on preoperative MRI in a consecutive series of LMPRTs. Suspicion for these injuries, especially in the setting of ACL tear or ACL graft tear, must be high for both the radiologist and the surgeon. In such scenarios, these results suggest that the surgeon should carefully evaluate and probe the lateral meniscus posterior root at the time of arthroscopy.
In the current study, two-thirds of LMPRTs were missed on preoperative MRI. LaPrade et al16 reported a sensitivity of 0.600 (95% CI, 0.281-0.860) and a positive predictive value of 0.181 (95% CI, 0.085-0.261) for the diagnosis of LMPRTs on 3-T MRI by a blinded fellowship-trained musculoskeletal radiologist. Although their sample included only 10 cases of LMPRT, it supports the findings of our study, which showed even greater unreliability in a larger sample size. In contrast with the LaPrade et al16 study, our series reflected a “real life” clinical scenario in which the radiologist was not aware that she or he would be looking for root tears in a group of study patients. The MRI reports were reviewed afterward to see if the radiologist had correctly diagnosed the root tear. In another study, Brody et al4 reviewed 264 knee MRI scans of patients with ACL tears and found evidence of LMPRTs in 26 (9.8%) of the images studied. However, upon arthroscopic examination of 5 knees diagnosed with LMPRTs, only 4 had a true lesion—1 had a tear of the posterior horn instead. This underlies the difficulty of accurately differentiating these tears from potential confounders on preoperative imaging.
On retrospective review by 2 musculoskeletal radiologists, the 30 missed LMPRTs were clearly evident in 15 cases, subtly evident in 12 cases, and occult in 3 cases. The most common reason for a missed LMPRT was postoperative scarring with obscured anatomy, especially after a ligament reconstruction case, although our study did not find a statistically significant correlation (P = .76). Acute ACL injuries resulting in hemorrhage and edema also obscured the relevant anatomy, but this was observed qualitatively to have less of an effect than postoperative changes. Other meniscal pathology, such as bucket-handle tears or large flap tears, contributed to the missed diagnosis in 12 cases by dominating the meniscal assessment. Still, with application of the 2-slice-touch criteria to all applicable MRI,7 42 of 43 (98%) cases could be identified on re-review. A similar retrospective identification by De Smet et al6 reported high sensitivity (15 of 16; 94%) and specificity (40 of 45; 89%) for detection of arthroscopically confirmed LMPRTs on MRI. This higher rate of identification is reassuring, indicating that, with emphasis and attention to the posterior horn lateral meniscus root, more of these injuries can be diagnosed.
The absence of secondary findings makes the radiographic diagnosis of LMPRTs more challenging. In contrast with the recent observation that meniscal ramp lesions are associated with posteromedial bone bruising,8 focal bone contusion subjacent to the LMPRT was not present on any of the MRI scans in this study. Instead, diffuse bone edema was present in the posterolateral tibia from the pivot-shift mechanism in patients with ACL injury. Peripheral extrusion of the lateral meniscus, suggesting root insufficiency, may be present but is not as prevalent as with posterior root tears of the medial meniscus. The rate of meniscus extrusion on MRI in this study (25 of 45; 56%) was similar to the rate (48.7%) reported by Minami et al21 but twice that (23%) reported by Brody et al.4 The latter found that meniscus extrusion was significantly increased in ACL-injured cases with LMPRTs as compared with isolated ACL controls, while Pula et al24 found no significant difference when comparing mean extrusion between similar groups. Of note, Pula et al24 measured meniscus extrusion at a mean of 9 days after acute ACL injury, and the MFL was intact in all cases included. Other studies have shown that the MFL plays a role in meniscus stabilization and that disruption of the MFL leads to increased contact pressures in the lateral compartment of the knee.10,13 De Smet et al6 did not evaluate the MFL in their study, but the majority of our cases (26 of 45; 58%) had a partially torn MFL, as defined by the presence of at least intermediate signal change. Determination of MFL integrity was challenging because of the presence of generalized edema and hemorrhage immediately posterior to the ACL midsubstance in most cases. On the basis of these complicating factors, one should be cautioned to follow the MFL centrally to avoid mistaking the MFL for meniscal tissue itself. The posterior horn of the lateral meniscus is thinner and flatter on MRI than the posterior horn of the medial meniscus, making it harder to recognize. Although medial meniscus root tears can often be identified by meniscus extrusion on the coronal images and a ghost sign on the sagittal images,5,18 such findings are not reliably present for the lateral meniscus root.
One limitation of this study was that the surgeons and the radiology reviewers were not blinded to the original MRI interpretation. For standard clinical practice, the operating surgeon was required to have knowledge of the MRI findings to provide appropriate patient care. The high frequency of missed LMPRTs on preoperative diagnosis also raises the concern that if any additional root tears were not identified during arthroscopy, then the rate of misses would be further increased. This consecutive series of patients also reflects a tertiary referral practice, with a higher proportion of revision ACL reconstructions. In terms of the MRI review, a “blinded” reading was essentially provided by the initial preoperative interpretation. The unblinded secondary review could have been performed separately, with calculation of interrater correlation. However, consensus review allowed the radiologists to discuss and agree on the more qualitative aspects of this investigation, such as designations for the root status (eg, clearly evident, subtly evident, or occult) and reasons for the miss, since the tear was already missed at the time of initial interpretation by a fellowship-trained musculoskeletal radiologist.
As another limitation, the original readings were performed by a heterogeneous sample of radiologists rather than a single reader, and data were not available for the experience levels of all radiologists who performed the initial readings. This potentially limits the applicability of the estimated diagnostic frequency in settings where the interpreters possess different levels of training. There was no association between MRI field strength and a missed LMPRT diagnosis in this study, which corroborates a recent meta-analysis that found no significant difference between the sensitivities of 1.5- and 3-T MRI for lateral meniscus injuries,27 although analysis has not been performed for root tears in particular. Other variations in imaging technique that were not analyzed could have influenced the results. A final constraint in this study was the lack of a control group of patients without LMPRTs, which prevented the calculation of sensitivity and specificity for this sample.
Conclusion
Despite improving identification of other meniscus tear patterns on MRI, a high percentage of LMPRTs are still missed. Although the MRI may be complicated by the presence of postoperative changes or acute edema and hemorrhage, and the anatomy of the lateral meniscus is more challenging than that of the medial meniscus, most of these tears should be evident if the De Smet and Tuite7 2-slice-touch rule is strictly applied. In the setting of a previous ACL reconstruction, if the root cannot be confidently identified, the MRI interpretation should indicate that “the root is poorly visualized” to alert the surgeon to thoroughly evaluate this structure. The surgeon should maintain a high index of suspicion and prepare the patient and operation accordingly. Finally, the posterior root of the lateral meniscus should be carefully probed at the time of arthroscopy, especially in cases of ACL injury.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: A.J.K. receives research support from Aesculap/B. Braun, the Arthritis Foundation, Ceterix, and Histogenics; is a paid consultant for Arthrex and Vericel; and is on the board of the Musculoskeletal Transplant Foundation. D.B.F.S. receives research support from Arthrex, Ivy Sports, and Smith & Nephew and is a paid consultant for Cartiheal, Smith & Nephew, and Vericel. B.A.L. receives royalties from Arthrex; is paid consultant for Arthrex and Smith & Nephew; and receives research support from Arthrex, Biomet, Smith & Nephew, and Stryker. M.J.S. is a paid consultant for Arthrex, receives royalties from Arthrex, and receives research support from Stryker.
Ethical approval for this study was obtained from the Mayo Clinic (Institutional Review Board application 15-000601).
References
- 1. Ahn JH, Lee YS, Chang J-Y, Chang MJ, Eun SS, Kim SM. Arthroscopic all inside repair of the lateral meniscus root tear. Knee. 2009;16(1):77–80. [DOI] [PubMed] [Google Scholar]
- 2. Ahn JH, Lee YS, Yoo JC, Chang MJ, Park SJ, Pae YR. Results of arthroscopic all-inside repair for lateral meniscus root tear in patients undergoing concomitant anterior cruciate ligament reconstruction. Arthroscopy. 2010;26(1):67–75. [DOI] [PubMed] [Google Scholar]
- 3. Anderson L, Watts M, Shapter O, et al. Repair of radial tears and posterior horn detachments of the lateral meniscus: minimum 2-year follow-up. Arthroscopy. 2010;26(12):1625–1632. [DOI] [PubMed] [Google Scholar]
- 4. Brody JM, Lin HM, Hulstyn MJ, Tung GA. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239(3):805–810. [DOI] [PubMed] [Google Scholar]
- 5. Choi SH, Bae S, Ji SK, Chang MJ. The MRI findings of meniscal root tear of the medial meniscus: emphasis on coronal, sagittal and axial images. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2098–2103. [DOI] [PubMed] [Google Scholar]
- 6. De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol. 2009;192(2):480–486. [DOI] [PubMed] [Google Scholar]
- 7. De Smet AA, Tuite MJ. Use of the “two-slice-touch” rule for the MRI diagnosis of meniscal tears. AJR Am J Roentgenol. 2006;187(4):911–914. [DOI] [PubMed] [Google Scholar]
- 8. DePhillipo NN, Cinque ME, Chahla J, Geeslin AG, Engebretsen L, LaPrade RF. Incidence and detection of meniscal ramp lesions on magnetic resonance imaging in patients with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(10):2233–2237. [DOI] [PubMed] [Google Scholar]
- 9. Feucht MJ, Bigdon S, Mehl J, et al. Risk factors for posterior lateral meniscus root tears in anterior cruciate ligament injuries. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):140–145. [DOI] [PubMed] [Google Scholar]
- 10. Forkel P, Herbort M, Sprenker F, Metzlaff S, Raschke M, Petersen W. The biomechanical effect of a lateral meniscus posterior root tear with and without damage to the meniscofemoral ligament: efficacy of different repair techniques. Arthroscopy. 2014;30(7):833–840. [DOI] [PubMed] [Google Scholar]
- 11. Forkel P, Reuter S, Sprenker F, et al. Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):112–118. [DOI] [PubMed] [Google Scholar]
- 12. Frank JM, Moatshe G, Brady AW, et al. Lateral meniscus posterior root and meniscofemoral ligaments as stabilizing structures in the ACL-deficient knee: a biomechanical study. Orthop J Sports Med. 2017;5(6):2325967117695756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Geeslin AG, Civitarese D, Turnbull TL, Dornan GJ, Fuso FA, LaPrade RF. Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1469–1477. [DOI] [PubMed] [Google Scholar]
- 14. LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–369. [DOI] [PubMed] [Google Scholar]
- 15. LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96(6):471–479. [DOI] [PubMed] [Google Scholar]
- 16. LaPrade RF, Ho CP, James E, Crespo B, LaPrade CM, Matheny LM. Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):152–157. [DOI] [PubMed] [Google Scholar]
- 17. LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45(4):884–891. [DOI] [PubMed] [Google Scholar]
- 18. Lee YG, Shim JC, Choi YS, Kim JG, Lee GJ, Kim HK. Magnetic resonance imaging findings of surgically proven medial meniscus root tear: tear configuration and associated knee abnormalities. J Comput Assist Tomogr. 2008;32(3):452–457. [DOI] [PubMed] [Google Scholar]
- 19. Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64(6):883–888. [PubMed] [Google Scholar]
- 20. Matheny LM, Ockuly AC, Steadman JR, LaPrade RF. Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3127–3131. [DOI] [PubMed] [Google Scholar]
- 21. Minami T, Muneta T, Sekiya I, et al. Lateral meniscus posterior root tear contributes to anterolateral rotational instability and meniscus extrusion in anterior cruciate ligament-injured patients [published online May 8, 2017]. Knee Surg Sports Traumatol Arthrosc. [DOI] [PubMed] [Google Scholar]
- 22. Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38(8):1591–1597. [DOI] [PubMed] [Google Scholar]
- 23. Pan F, Hua S, Ma Z. Surgical treatment of combined posterior root tears of the lateral meniscus and ACL tears. Med Sci Monit. 2015;21:1345–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Pula DA, Femia RE, Marzo JM, Bisson LJ. Are root avulsions of the lateral meniscus associated with extrusion at the time of acute anterior cruciate ligament injury? Am J Sports Med. 2013;42(1):173–176. [DOI] [PubMed] [Google Scholar]
- 25. Shelbourne KD, Roberson TA, Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39(7):1439–1443. [DOI] [PubMed] [Google Scholar]
- 26. Shybut TB, Vega CE, Haddad J, et al. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2015;43(4):905–911. [DOI] [PubMed] [Google Scholar]
- 27. Woodmass JM, Mohan R, Stuart MJ, Krych AJ. Medial meniscus posterior root repair using a transtibial technique. Arthrosc Tech. 2017;6(3):e511–e516. [DOI] [PMC free article] [PubMed] [Google Scholar]