Abstract
Background:
The number of adolescent anterior cruciate ligament (ACL) injuries is rising with increased participation in higher level athletics at earlier ages. With an increasing number of primary ACL reconstructions (ACLRs) comes a rise in the incidence of revision ACLRs.
Purpose:
To evaluate the clinical results of revision ACLR across a group of high-level adolescent athletes with at least 2-year follow-up.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective review of 21 adolescent athletes (age range, 10-19 years) who underwent revision ACLR with at least 2-year follow-up was conducted. Patient-reported outcome measures (PROMs) included the International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Lysholm knee scoring scale, Tegner activity level scale, and modified Cincinnati Knee Rating System. Return to sport (RTS) and overall patient satisfaction were also assessed.
Results:
The mean age at the time of surgery was 16.5 years (range, 14-19 years), and the mean follow-up was 46.4 months (range, 24-97 months); 42.9% of patients were female, and 52.4% of patients participated in collision sports. The mean time to failure after primary ACLR was 13.1 ± 8.0 months, and the most common mechanism of failure was noncontact in at least 66.7% of cases. The revision graft type included bone–patellar tendon–bone (BPTB) in 71.4% of cases; 26.7% of BPTB grafts were from the contralateral extremity. Concomitant procedures were performed for intra-articular lesions in 71.4% of patients. The mean patient satisfaction rate was 95.3%. There were 3 cases of a graft reinjury at a mean of 25 months postoperatively. The mean PROM scores were as follows: IKDC, 87.5 ± 12.7; Tegner, 7.2 ± 2.0; Lysholm, 93.7 ± 9.8; and Cincinnati, 93.4 ± 10.0. Of those attempting to RTS, 68.4% of patients successfully returned at the same level of competition. Patients with a lateral compartment chondral injury were less likely to RTS (P < .05). Independent variables shown to have no significant relationship to PROMs or RTS included age, follow-up, sport classification, associated meniscal tears, revision graft size/type, and concomitant procedures.
Conclusion:
Revision ACLR can be an effective surgical option in adolescents participating in collision and contact sports, with good to excellent subjective outcome scores. At a minimum 2-year follow-up, a graft rupture after revision ACLR occurred in 14% of cases. Of the athletes attempting to RTS, 68.4% returned to their preinjury level of competition.
Keywords: revision, anterior cruciate ligament, reconstruction, outcomes, adolescents
The number of adolescent anterior cruciate ligament (ACL) injuries is rising with increased participation in higher level athletics at earlier ages, increased awareness of the injury in youth, and improved diagnostic methods.17 Dodwell et al10 found an increase in the rate of ACL reconstruction (ACLR) per 100,000 population from 17.6 in 1990 to 50.9 in 2009 in New York State alone and predicted that this increase was actually larger, as the figures did not include undiagnosed tears or those treated nonoperatively. Furthermore, with an increasing number of primary ACLRs comes a rise in the incidence of revision surgery, particularly in the adolescent population, which has been shown to be at a higher risk for reinjuries after ACLR than adults.13 Multiple factors seem to predispose the adolescent population to ACL reinjuries. Morgan et al17 showed that one-third of patients younger than 19 years are at risk of further ACL graft ruptures to either knee after primary ACLR, especially in patients with a family history of ACL injuries, young male patients, and those returning to cutting or pivoting sports.
While several large studies have shown return-to-sport (RTS) rates after primary ACLR to be somewhere between 43% and 75%,6,16 the rates of return after revision ACLR are not as widely studied. Reinhardt et al22 reported the first series on RTS rates after revision ACLR in competitive athletes younger than 18 years and noted that only 50% of patients were able to return to their preinjury level; however, over half of these patients’ grafts were allografs, which have had higher failure rates in primary reconstruction.4,11,15,20,27 Further studies have shown RTS rates around 74% when using bone–patellar tendon–bone (BPTB) autografts in this population.24 However, studies are lacking a comparison of multiple graft choices with RTS and clinical outcomes.
Athletic participation is common among adolescents, with more than half of all high school students participating in school-sanctioned sports during the 2014-2015 academic year.18 With increasing student participation in high school athletics over the past decade, reinjuries after ACLR continue to be more prevalent. Refining our understanding of these injuries is crucial to guide targeted evidence-based treatment approaches. The purpose of this study was to evaluate the clinical results of revision ACLR across a group of high-level adolescent athletes with at least 2-year follow-up. We sought to identify any demographic, injury, and surgical factors affecting patient-reported functional outcomes. Secondarily, we sought to characterize the success of RTS. We hypothesized that excellent results would be observed in this population at a minimum 2-year follow-up.
Methods
Patient Selection
Institutional review board approval was obtained before the initiation of this retrospective study. We reviewed a consecutive series of adolescent athletes who underwent revision ACLR with a minimum 2-year follow-up. All surgical procedures were performed by 2 fellowship-trained sports medicine surgeons (R.O. and J.R.A.) between October 2007 and February 2014. A total of 149 patients were identified through a Current Procedural Terminology code search of an institutional computerized database using the code 29888 (arthroscopically aided anterior cruciate ligament repair/augmentation or reconstruction). The search was limited to patients aged 10 to 19 years, consistent with the World Health Organization’s definition of adolescence.28 Operative reports were reviewed to identify a total of 34 patients whose procedures were revision ACLRs during the study period.
Patients were included in the study if they (1) experienced persistent instability after primary ACLR or a history of injury (noncontact or contact) to their knee resulting in an ACL graft rupture, (2) had a graft rupture confirmed both with magnetic resonance imaging and arthroscopically at the time of surgery, (3) had radiographically proven closed or nearly closed physes, and (4) had undergone a single-stage revision ACLR procedure using a transphyseal/transtibial technique. Those with associated meniscal lesions or chondral injuries were also included, and there were no limits regarding concomitant procedures. We considered a noncontact injury as one in which there was no physical contact with an opponent or stationary object at the time of injury. Exclusion criteria were ipsilateral lower extremity injuries and posterolateral corner or multiligament knee injuries requiring repair/reconstruction.
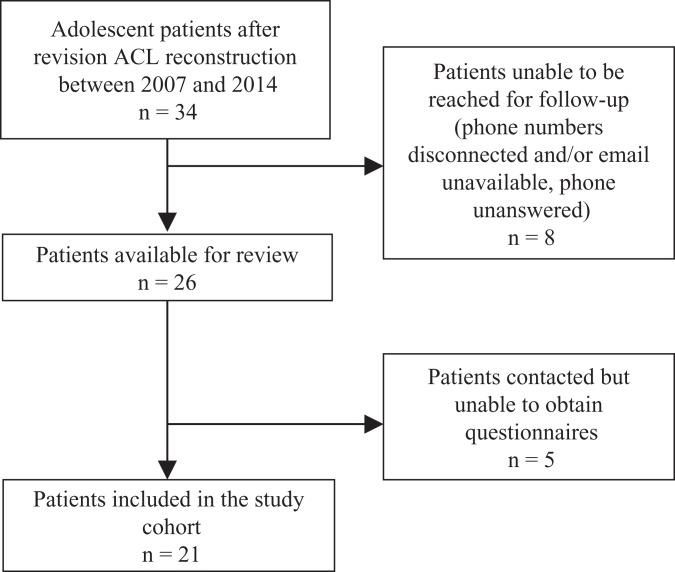
Patient-reported outcome data were obtained by contacting all patients via telephone. Those agreeable to taking part in the study completed a telephone interview or written questionnaire that was returned via email. Two orthopaedic surgery residents, both of whom had not been involved in the original surgery or care of the patients, conducted the telephone questionnaires. Eight patients were unable to be reached for follow-up. Ultimately, 21 patients provided follow-up information. A detailed flow diagram is included in Figure 1.
Figure 1.
Flow diagram outlining patient selection. ACL, anterior cruciate ligament.
Surgical Technique
Patients underwent revision ACLR with either a hamstring autograft (n = 6) or BPTB autograft from the ipsilateral (n = 11) or contralateral (n = 4) knee. The choice of a revision graft was determined according to the individual preferences of the treating surgeon. However, in general, a BPTB graft was chosen after failed soft tissue primary ACLR (either allograft, autograft, or combined allograft + autograft). All 4 contralateral BPTB autografts were used in patients after failed ipsilateral primary ACLR with a BPTB autograft. If a BPTB autograft was used, it was harvested at the beginning of the case. Excess bone from the graft or tibia was used to fill the patella’s harvest site, and the patellar tendon defect was closed. Systematic arthroscopic surgery was performed, and any intra-articular abnormalities were addressed. Tunnel grafting was not required in any of the cases. Tibial and femoral tunnels were created using the same transphyseal/transtibial technique for all cases. BPTB autografts were secured with biocomposite interference screws (Smith & Nephew). In cases using hamstring autografts, the grafts were secured via suspensory fixation (Biomet or Arthrex) on the femur and a nonabsorbable screw and sheath (Mitek) on the tibia. All grafts were tensioned with the knee in full extension.
Postoperative Management
Postoperative rehabilitation was initiated the day after surgery and consisted of 6 separate phases. The same standardized rehabilitation protocol was utilized for all patients depending on the graft type. Weightbearing as tolerated was allowed immediately postoperatively in a hinged brace locked in full extension. The brace was worn during the first 6 weeks. It was kept locked in extension for the first 2 to 4 weeks. During the first week, range of motion (ROM) exercises were initiated, and exercises to re-establish quadriceps control were begun. During phase 2, the patient worked to gradually improve ROM (ideally 90° by week 4). Phase 3 goals included working to gradually restore full ROM, restoring muscular strength and balance, and enhancing neuromuscular control. In cases where a hamstring autograft was used, isolated isotonic hamstring contractions were avoided for 6 weeks. Phases 4 and 5 focused on strength, power, and endurance as well as the progression of functional activities. Track or treadmill running was not started before 4 months postoperatively. At 6 to 12 months, patients were cleared to RTS activities at the discretion of the treating surgeon. The timing and goals of each phase are presented in Table 1.
TABLE 1.
Rehabilitation Protocola
| Phase | Timing | Goals |
|---|---|---|
| 1 | Days 1-7 | Restore full passive knee extension, re-establish quadriceps control, gradually improve knee flexion, and diminish pain and inflammation |
| 2 | Weeks 2-3 | Maintain symmetrical knee extension, normalize patellar mobility, progress knee ROM, improve muscle control and activation, and restore proprioception/neuromuscular control |
| 3 | Weeks 4-12 | Improve muscular strength, power, and endurance; restore full knee ROM; and enhance proprioception, balance, and neuromuscular control |
| 4 | Weeks 13-16 | Normalize lower extremity strength, enhance strength and endurance, and perform selected sport-specific drills |
| 5 | Weeks 17-23 | Achieve maximal strength and endurance |
| 6 | Months 6-12 | Progress skill training, progress proprioception/balance skills, progress power, and return gradually to sport activities |
aROM, range of motion.
Clinical Evaluation
Clinical and operative data were extracted from patients’ medical records. Preoperative findings included age, side, sex, mechanism of injury, original graft type/size, and sport. Patients were classified as collision, contact, or limited contact athletes according to criteria established by the American Academy of Pediatrics23 (Table 2). Intraoperative findings included revision graft type/size, associated lesions, and any concomitant procedures. Chondral injuries were graded with the Outerbridge classification. Postoperative findings included graft failure and any postoperative complications. Patient-reported outcome measures (PROMs) and functional activity levels were evaluated using the International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form,1 modified Cincinnati Knee Rating System,19 Lysholm knee scoring scale,26 and Tegner activity level scale.26 Patient satisfaction was assessed with a 0- to 100-point scale, where 0 was considered “completely dissatisfied” and 100 was considered “completely satisfied.” RTS was directly assessed using a special questionnaire. Patients were also asked about their ability to return to their previous sport, including the level of play, and to describe their reasons if they returned at a decreased level or were unable to return at all.
TABLE 2.
Classification of Sports by Contacta
| Collision | Contact | Limited Contact |
|---|---|---|
| Football | Basketball | Baseball |
| Ice hockey | Soccer | Volleyball |
aAccording to the American Academy of Pediatrics.23
Statistical Analysis
Means and SDs were calculated for continuous variables (eg, age). Categorical variables (eg, sex) were expressed as numbers and percentages. Continuous variables were tested for normality using the Shapiro-Wilk test. Comparisons of categorical variables were made using chi-square tests. Comparisons of continuous variables between 2 or multiple study groups were made using the Student t test or analysis of variance, respectively. Logistic regression analysis was performed to identify factors associated with PROMs and successful RTS. Statistical significance was set at P ≤ .05. All data were tabulated in Excel (2012 version; Microsoft) and analyses conducted using open-source R.21
Results
Patient Characteristics
Athlete characteristics are summarized in Table 3. The mean age at the time of surgery was 16.5 years (range, 14-19 years), and the mean follow-up was 46.4 months (range, 24-97 months). Moreover, 42.9% of patients were female, and 52.4% of patients participated in collision sports. The mean time to failure after primary ACLR was 13.1 ± 8.0 months, and the most common mechanism of failure was noncontact in at least 66.7% of cases.
TABLE 3.
Athlete Characteristicsa
| Characteristic | Value |
|---|---|
| Age at surgery, y | 16.5 ± 1.6 |
| Sex, n (%) | |
| Male | 12 (57.1) |
| Female | 9 (42.9) |
| Follow-up, mo | 46.4 ± 19.8 |
| Time to failure, mo | 13.1 ± 8.0 |
| Original graft size, mm | 9.5 ± 0.9 |
| Revision graft size, mm | 9.9 ± 1.1 |
| Right side, n (%) | 12 (57.1) |
| Sport classification, n (%) | |
| Collision | 11 (52.4) |
| Contact | 8 (38.1) |
| Limited contact | 2 (9.5) |
| Sport, n (%) | |
| Football | 10 (47.6) |
| Baseball | 1 (4.8) |
| Basketball | 4 (19.0) |
| Hockey | 1 (4.8) |
| Soccer | 4 (19.0) |
| Volleyball | 1 (4.8) |
| Mechanism of injury, n (%) | |
| Contact | 3 (14.3) |
| No contact | 14 (66.7) |
| Unknown | 4 (19.0) |
aData are reported as mean ± SD unless otherwise specified.
Surgical Findings
Surgical findings are reported in Table 4. Associated intra-articular lesions were noted in 76.2% of patients. Concomitant procedures were performed in 71.4% of patients. The most common procedure was partial lateral meniscectomy in 42.9% of patients.
TABLE 4.
Surgical Findings (N = 21 Knees)a
| Finding | Value |
|---|---|
| Associated lesions | 16 (76.2) |
| Chondral injuries | 11 (52.4) |
| Medial compartment | 7 (33.3) |
| Grade I | 1 (4.8) |
| Grade II | 3 (14.3) |
| Grade III | 2 (9.5) |
| Grade IV | 1 (4.8) |
| Lateral compartment | 5 (23.8) |
| Grade I | 1 (4.8) |
| Grade II | 4 (19.0) |
| Patellofemoral compartment | 7 (33.3) |
| Grade I | 1 (4.8) |
| Grade II | 5 (23.8) |
| Grade III | 1 (4.8) |
| Meniscal tears | 13 (61.9) |
| Medial | 9 (42.9) |
| Lateral | 9 (42.9) |
| Other procedures | 15 (71.4) |
| Removal of hardware | 4 (19.0) |
| Chondroplasty | 2 (9.5) |
| Medial meniscal repair | 6 (28.6) |
| Partial meniscectomy (medial) | 3 (14.3) |
| Partial meniscectomy (lateral) | 9 (42.9) |
aData are reported as n (%).
Clinical Outcomes
Outcome data were available for all 21 patients. The mean patient satisfaction rate was 95.3%. The mean PROM scores were 87.5 ± 12.7 for the IKDC, 7.2 ± 2.0 for the Tegner, 93.7 ± 9.8 for the Lysholm, and 93.4 ± 10.0 for the Cincinnati (Table 5). Independent variables that had no significant relationship to PROMs included age, follow-up, sport classification, associated meniscal tears, revision graft size/type, and concomitant procedures. There were 3 cases of graft reinjuries. The mean time to a graft rerupture was 25 ± 14 months. No patient experienced a contralateral ACL injury during the follow-up period.
TABLE 5.
Clinical Outcomesa
| Outcome Measure | Value |
|---|---|
| Lysholm | 93.7 ± 9.8 |
| IKDC | 87.5 ± 12.7 |
| Cincinnati | 93.4 ± 10.0 |
| Tegner | 7.2 ± 2.0 |
| Global satisfaction (0-100) | 95.3 ± 23.5 |
| Recurrence, n (%) | |
| Yes | 3 (14.3) |
| No | 18 (85.7) |
| Return to sport, n (%) | |
| Did not attempt return | 2 (9.5) |
| Fear of reinjury | 2 (100.0) |
| Attempted/able to return | 19 (90.5) |
| Same level or higher | 13 (68.4) |
| Decreased level | 6 (31.6) |
| Fear of reinjury | 4 (66.7) |
| Personal reasons | 2 (33.3) |
aData are reported as mean ± SD unless otherwise specified. IKDC, International Knee Documentation Committee.
Return to Sport
A total of 19 patients (90.5%) attempted to RTS postoperatively (Table 5). Two patients (a 15-year-old female basketball player and an 18-year-old male football player) did not attempt to return to their sports because they feared reinjury. However, both patients returned to pain-free recreational jogging and reported excellent PROM scores and global satisfaction at 24- and 48-month follow-up, respectively. Of the patients who attempted to RTS, 13 (68.4%) were able to return to the same level or higher for at least 1 season. The most common reason for returning at a decreased level was fear of reinjury (n = 4 patients). Patients with a lateral compartment chondral injury were less likely to RTS (P < .05). Independent variables shown to have no significant relationship to RTS included age, follow-up, sport classification, associated meniscal tears, revision graft size/type, and concomitant procedures.
Discussion
The principal findings of this study suggest that revision ACLR is an effective treatment option for secondary ACL tears in adolescent patients participating in collision and contact sports. Excellent PROM scores were seen at a minimum of 2-year follow-up. Recurrence after revision ACLR occurred in 14% of cases. However, only 68.4% of patients who attempted to RTS returned to the same level for at least 1 season. A lateral compartment chondral injury was associated with decreased RTS rates, with the fear of reinjury being the most common reason.
There are limited published data concerning outcomes after revision ACLR and even less information available in the adolescent population. When examining PROMs such as the IKDC in other studies of adolescent revision ACLR, our study revealed similar excellent IKDC scores that are reflective of the normative data for men and women.3 The adolescent primary ACLR literature also reports IKDC outcomes similar to the normative data.22,24 Ellis et al11 compared graft differences in primary ACLR in adolescents, reporting good Lysholm scores for autografts and excellent scores for allografts. Our cohort, which consisted of only autografts, similarly reported good to excellent Lysholm scores. Tegner scores were 1 to 2 points above the standardized activity rating for the asymptomatic population, which is similar to reported adolescent primary ACLR outcomes in the literature.5,11 The above-average activity scores in this population may in part be caused by the fact that the typical adolescent patient requiring ACLR is usually involved in athletic activities, and all patients in our cohort were highly competitive athletes. While adolescent patients undergoing revision ACLR seem to do as well as their primary reconstruction counterparts, both groups appear to do better than the adult revision population, as demonstrated by Anand et al,2 who found a mean IKDC score of only 69.2 in a recent study.
Graft size has been found to make a difference in outcomes and revision rates among the adult ACL literature; it is well known that grafts smaller than 8 mm tend to do poorly and have a higher rerupture rate than larger grafts.7,14,25 Additionally, hybrid hamstring autografts supplemented with an allograft to enlarge the overall graft size have also been shown to have a higher failure rate than hamstring autografts alone.8 A recent study of the Swedish National Knee Ligament Register reported a 0.86 times lower likelihood of revision surgery with every 0.5-mm increase in graft size from their large cohort.25 In our study, revision graft size and type had no significant relationship to PROMs or RTS, although no patient had a graft smaller than 8 mm.
With regard to RTS after revision ACLR, 90.5% of those who attempted it returned to their sport, with 68.4% returning to their preinjury level of competition. These findings are consistent with reported pediatric primary ACLR RTS rates of 69% to 96%9,17 as well as the 60% to 75% rates reported in adults.2,12 Reinhardt et al22 reported the first series on RTS rates after revision ACLR for competitive athletes under 18 years of age, finding that only 50% of patients returned to their preinjury level of sport. Shelbourne et al24 compared school-aged athletes (<17.9 years), college-aged athletes (18.0-21.9 years), and adult recreational athletes (>22.0 years ) who underwent revision ACLR and reported that 74% of school-aged and college-aged athletes returned to their preinjury level of sport, while only 62% of the adult recreational athletes returned to their preinjury level. While the reasons were not discussed as to why patients did not return to the same level (eg, knee pain, fear of reinjury, personal reasons), the adolescent revision ACLR RTS rates in these studies appear to be similar to the adult primary ACLR rates of 60% to 75%.9,12,24 The available literature supports the suggestion that younger athletes tend to return to similar levels of competition more often than their adult counterparts.9,24 The reasons for the increased RTS rates in adolescents are unknown, but theories include the lower athletic demand of sports at that age, a higher neurophysiological healing rate and plasticity of healing, and/or a lower fear of reinjury in younger athletes.9
Psychological factors, primarily fear of reinjury, may have an underestimated effect on RTS outcomes after ACLR at all levels of competition.12,16 A study from the Multicenter Orthopaedic Outcomes Network (MOON) registry reviewing high school and college football athletes returning to play after primary ACLR revealed that 67% of high school patients did not RTS because of “other interests” (including lost interest, interest in other sports, other life interests) and that 53% did not return because of a fear of reinjury.16 Our study revealed a similar finding that, for adolescent patients who did not RTS at the same level of competition, 67% cited a fear of reinjury as the reason. In contrast, 33% of high school athletes in the MOON cohort did not return because of physical symptoms or loss of speed or strength,16 whereas our study demonstrated that only 11.7% of patients were not able to return because of knee pain.
When comparing objective variables limiting RTS in patients undergoing ACLR, the MOON study reviewing high school and college football players noted no statistical impact from the presence of associated chondral, meniscal, or other ligamentous injuries on RTS rates, despite over half of the cohort's having concurrent meniscal injuries.16 A lateral compartment chondral injury was the only significant intra-articular concomitant injury seen in our study to negatively affect returning to competition. Age, sex, sport classification, associated meniscal tears, revision graft size, graft type, and concomitant procedures did not affect RTS rates. This discrepancy may be because of the smaller size of our cohort, the less-detailed intra-articular evaluations of the MOON cohort, and/or the fact that our study reviewed revision cases of ACLR.
Similar to our findings, a study of the adult revision population has shown that the status of the menisci at the time of revision surgery had no effect on RTS rates.2 However, the chondral injuries in our cohort were relatively minor, and the negative effects of meniscectomy and/or a chondral injury can take years to manifest. Age and sex were the only predictors of RTS in a separate MOON study involving young adult soccer players after primary ACLR, with female athletes less likely than male athletes to initially return to play. Yet, at 7-year follow-up, there was no difference in age or sex in return-to-play rates, which is consistent with our data.6
The recurrence of ACL tears after revision surgery in the adolescent population has been reported to be around 2% to 10%,22,24 whereas the adult revision failure rate is approximately 13% to 19%.15,29 Our series showed a 14.3% recurrence rate with a mean survival of 25 months. This is consistent with the rates in studies on adults and is slightly higher than those in the pediatric and adolescent literature for primary ACLR.22,24,27 The time to failure after revision ACLR in adolescents may be longer than that in the primary ACLR population,8 indicating that studies reviewing revision ACLR may need to have a longer follow-up period than 2 years to ensure capturing graft failures, which tend to occur just after the 2-year postoperative period.
Limitations of this study included the small sample size, the retrospective nature of the study design, and a short follow-up interval of only 2 years minimum, rendering long-term conclusions difficult to make. Obtaining follow-up information by a telephone interview may have introduced response bias, and we did not obtain objective follow-up data (ROM, KT-1000 arthrometer, diagnostic imaging), the inclusion of which could have added greatly to the study. Patients in our cohort were highly competitive athletes, which may have introduced selection bias. It is possible that less competitive athletes may have chosen not to undergo revision ACLR or may not have attempted to return to their respective sport. These results reflect the outcomes of 2 surgeons with a high volume of young, high-level athletes and, as such, might not be generalizable to the broader orthopaedic community. Including patients with different revision graft types added heterogeneity to the study cohort but did allow for within-group analysis of PROMs between graft types. Furthermore, there was no comparison group to contrast our technique with a different method of ACLR.
Another limitation was the difficulty of classifying patients who returned to sport as returning to the same or decreased level if they entered college during their rehabilitation period. Most college sports are felt to be at a higher level than high school sports; thus, not qualifying for a Division I athletic team does not mean that the patient did not return to the same level of play as before the injury. However, patients were asked qualitatively if they felt that they returned to the same level of play to minimize the skewing of results. Finally, our response rate (62%) for follow-up data was limited; this may in part have been caused by patient mobility unique to this population as they entered into adulthood. Despite these limitations, this study represents one of the largest investigations of revision ACLR in this specific adolescent population.
Conclusion
Revision ACLR can be an effective surgical option in adolescents participating in collision and contact sports, with good to excellent subjective outcome scores. At a minimum of 2-year follow-up, graft ruptures after revision ACLR occurred in 14% of cases. Of the athletes attempting to RTS, 68.4% returned to their preinjury level of competition.
Acknowledgment
The authors thank Mary Jane Robinson, LPN, and Sarah Johnson of the Andrews Institute for Orthopaedics & Sports Medicine for their assistance with this study.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: M.S. has received educational support from Arthrex and Smith & Nephew and has received grant support for fellowship training from DJO Global. R.O. is a consultant for DePuy Synthes and Halyard Health, has received honoraria from Halyard Health, and has received hospitality payments from Halyard Health. J.R.A. is a consultant for Arthrex and Halyard Health, has received educational support from Smith & Nephew, and has received hospitality payments from Arthrex.
Ethical approval for this study was obtained from the Baptist Health Institutional Review Board (study 900709-1).
References
- 1. American Orthopaedic Society for Sports Medicine. IKDC Knee Form. Available at: http://www.sportsmed.org/AOSSMIMIS/members/downloads/research/IKDCEnglishUS.pdf. Accessed August 7, 2017.
- 2. Anand BS, Feller JA, Richmond AK, Webster KE. Return-to-sport outcomes after revision anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2016;44(3):580–584. [DOI] [PubMed] [Google Scholar]
- 3. Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ; International Knee Documentation Committee. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34(1):128–135. [DOI] [PubMed] [Google Scholar]
- 4. Barrett GR, Luber K, Replogle WH, Manley JL. Allograft anterior cruciate ligament reconstruction in the young, active patient: Tegner activity level and failure rate. Arthroscopy. 2010;26(12):1593–1601. [DOI] [PubMed] [Google Scholar]
- 5. Briggs KK, Steadman JR, Hay CJ, Hines SL. Lysholm score and Tegner activity level in individuals with normal knees. Am J Sports Med. 2009;37(5):898–901. [DOI] [PubMed] [Google Scholar]
- 6. Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Conte EJ, Hyatt AE, Gatt CJ, Dhawan A. Hamstring autograft size can be predicted and is a potential risk factor for anterior cruciate ligament reconstruction failure. Arthroscopy. 2014;30(7):882–890. [DOI] [PubMed] [Google Scholar]
- 8. Darnley JE, Léger-St-Jean B, Pedroza AD, Flanigan DC, Kaeding CC, Magnussen RA. Anterior cruciate ligament reconstruction using a combination of autograft and allograft tendon: a MOON cohort study. Orthop J Sports Med. 2016;4(7):232596711666224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. J Bone Joint Surg Am. 2017;99(11):897–904. [DOI] [PubMed] [Google Scholar]
- 10. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. [DOI] [PubMed] [Google Scholar]
- 11. Ellis HB, Matheny LM, Briggs KK, Pennock AT, Steadman JR. Outcomes and revision rate after bone-patellar tendon-bone allograft versus autograft anterior cruciate ligament reconstruction in patients aged 18 years or younger with closed physes. Arthroscopy. 2012;28(12):1819–1825. [DOI] [PubMed] [Google Scholar]
- 12. Ellman MB, Sherman SL, Forsythe B, LaPrade RF, Cole BJ, Bach BR. Return to play following anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2015;23(5):283–296. [DOI] [PubMed] [Google Scholar]
- 13. Fauno P, Rahr-Wagner L, Lind M. Risk for revision after anterior cruciate ligament reconstruction is higher among adolescents: results from the Danish registry of knee ligament reconstruction. Orthop J Sports Med. 2014;2(10):2325967114552405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Arthroscopy. 2013;29(12):1948–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. MARS Group, Ding DY, Zhang AL, et al. Subsequent surgery after revision anterior cruciate ligament reconstruction: rates and risk factors from a multicenter cohort. Am J Sports Med. 2017;45(9):2068–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McCullough KA, Phelps KD, Spindler KP, et al. Return to high school– and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40(11):2523–2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Morgan MD, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. Am J Sports Med. 2016;44(2):384–392. [DOI] [PubMed] [Google Scholar]
- 18. National Federation of State High School Associations. 2014-15 high school athletics participation survey results. Available at: http://www.nfhs.org/ParticipationStatics/PDF/2014-15_Participation_Survey_Results.pdf. Accessed January 18, 2016.
- 19. Noyes FR, Barber SD, Mooar LA. A rationale for assessing sports activity levels and limitations in knee disorders. Clin Orthop Relat Res. 1989;(246):238–249. [PubMed] [Google Scholar]
- 20. Pallis M, Svoboda SJ, Cameron KL, Owens BD. Survival comparison of allograft and autograft anterior cruciate ligament reconstruction at the United States Military Academy. Am J Sports Med. 2012;40(6):1242–1246. [DOI] [PubMed] [Google Scholar]
- 21. R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing; 2008. [Google Scholar]
- 22. Reinhardt KR, Hammoud S, Bowers AL, Umunna B-P, Cordasco FA. Revision ACL reconstruction in skeletally mature athletes younger than 18 years. Clin Orthop Relat Res. 2012;470(3):835–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rice SG; American Academy of Pediatrics Council on Sports Medicine and Fitness. Medical conditions affecting sports participation. Pediatrics. 2008;121(4):841–848. [DOI] [PubMed] [Google Scholar]
- 24. Shelbourne KD, Benner RW, Gray T. Return to sports and subsequent injury rates after revision anterior cruciate ligament reconstruction with patellar tendon autograft. Am J Sports Med. 2014;42(6):1395–1400. [DOI] [PubMed] [Google Scholar]
- 25. Snaebjörnsson T, Hamrin Senorski E, Ayeni OR, et al. Graft diameter as a predictor for revision anterior cruciate ligament reconstruction and KOOS and EQ-5D values: a cohort study from the Swedish National Knee Ligament Register based on 2240 patients. Am J Sports Med. 2017;45(9):2092–2097. [DOI] [PubMed] [Google Scholar]
- 26. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]
- 27. van Eck CF, Schkrohowsky JG, Working ZM, Irrgang JJ, Fu FH. Prospective analysis of failure rate and predictors of failure after anatomic anterior cruciate ligament reconstruction with allograft. Am J Sports Med. 2012;40(4):800–807. [DOI] [PubMed] [Google Scholar]
- 28. World Health Organization. Adolescent development. Available at: http://www.who.int/maternal_child_adolescent/topics/adolescence/dev/en/. Accessed February 12, 2016.
- 29. Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J Bone Joint Surg Am. 2012;94(6):531–536. [DOI] [PMC free article] [PubMed] [Google Scholar]