Abstract
Background and Purpose:
Participation in regular physical activity is associated with better physical function in older people (>65 years); however, older people are the least active of all age groups. Exercise-based active video games (AVGs) offer an alternative to traditional exercise programs aimed at maintaining or enhancing physical performance measures in older people. This review systematically evaluated whether AVGs could improve measures of physical performance in older people. Secondary measures of safety, game appeal, and usability were also considered.
Methods:
Electronic databases were searched for randomized controlled trials published up to April 2015. Included were trials with 2 or more arms that evaluated the effect of AVGs on outcome measures of physical performance in older people.
Results:
Eighteen randomized controlled trials (n = 765) were included. Most trials limited inclusion to healthy community-dwelling older people. With the exception of 1 trial, all AVG programs were supervised. Using meta-analyses, AVGs were found to be more effective than conventional exercise (mean difference [MD], 4.33; 95% confidence intervals [CIs], 2.93-5.73) or no intervention (MD, 0.73; 95% CI, 0.17-1.29) for improving Berg Balance scores in community-dwelling older people. Active video games were also more effective than control for improving 30-second sit-to-stand scores (MD, 3.99; 95% CI, 1.92-6.05). No significant differences in Timed Up and Go scores were found when AVGs were compared with no intervention or with conventional exercise.
Conclusions:
Active video games can improve measures of mobility and balance in older people when used either on their own or as part of an exercise program. It is not yet clear whether AVGs are equally suitable for older people with significant cognitive impairments or balance or mobility limitations. Given the positive findings to date, consideration could be given to further development of age-appropriate AVGs for use by older people with balance or mobility limitations.
Keywords: aged, exercise, older adult, video games
INTRODUCTION
Physical activity levels have been shown to decline with advancing age,1,2 yet regular participation in physical activity among older people (≥65 years) is associated with a reduced risk of cardiovascular and cardiometabolic disease, better physical fitness, and physical function.3–6 However, adults aged 70 to 85 years are reported to be the least active of all age groups.7
Active video games (AVGs), where the person is required to move to play the game, were first used to encourage activity in children,8,9 but they also show potential for encouraging activity in older people.10,11 Motivators to being active identified by older people include enjoyment and social interaction, as well as the perceived health benefits.12–14 A key attribute of AVGs is the immediate visual and auditory feedback on the player's performance, which is fun and motivating. In addition, the range of games, dance, and formal exercise programs available caters for individual preferences.
Active video games increase energy expenditure, with energy expended playing AVGs by older adults equivalent to light-to-moderate intensity activity.15–17 Perhaps more important is the ability to incorporate various motor control challenges into AVGs to improve balance and lower limb function, which are considered important for reducing falls risk and maintaining independence.18,19
Randomized controlled trials (RCTs) have begun to evaluate the effect of AVGs on physical function measures in older people. However, on the basis of narrative synthesis of 13 RCTs, 1 systematic review concluded that there was insufficient evidence to support the effectiveness of AVGs for improving physical function in older people.20
The objective of the current systematic review was to provide an updated analysis of RCTs that have used AVGs to improve physical function in older people, using meta-analyses where appropriate to increase the power of findings from the individual trials. This review also considered safety, game appeal, and usability aspects of AVGs for older people.
METHODS
Data Source and Search Strategy
Randomized controlled trials identified up to April 2015 were sourced from the following electronic databases: MEDLINE (OvidSP), Scopus, and the Cochrane Library (Wiley). Search terms combined the following subject headings and key words, formatted according to the requirements for each database: “Wii” or “Xbox*” or “Video games” or “Virtual” rehabilitation” or “Interactive video game” or “Virtual reality” and “Elderly” or “Old*” or “Senior” and “Physical activity” or “Exercise” or “Balance.”
Selection Criteria
Inclusion criteria were RCTs that compared exercise-based AVGs in older people with no intervention or usual care, traditional exercise or placebo, with outcomes that objectively measured physical performance (ie, balance, mobility or physical performance test batteries), or subjectively measured physical performance (ie, activity or balance confidence questionnaires).
Trials that used off-the-shelf, modified off-the-shelf or purpose-designed AVGs, offered over any length of time with the aim of improving physical performance measures were eligible.
The majority (>50%) of participants needed to be older adults (>65 years), living in the community, long-term care (rest home, nursing home, residential care, assisted living, and veteran's hospital), or acute hospital settings. Trials of AVGs targeting individuals with specific conditions (eg, stroke or diabetes) were excluded.
Data Extraction
Two review authors (LT, TF) independently screened the titles identified in the initial search to exclude those that were obviously outside the scope of the review. The same 2 authors then independently reviewed the abstracts of the remaining records. Where it was unclear from the abstract whether the study was relevant, the full article was reviewed. Characteristics of included trials were summarized according to population, intervention, comparator, and outcome characteristics.
The methodological quality was assessed independently by the same 2 authors (LT and TF) using the Cochrane Collaboration's risk of bias tool.21 Items were scored as high risk, low risk, or unclear risk of bias using the tool's set criteria. Consensus was reached on any item where there was any discrepancy between the 2 reviewers' evaluations.
Where trial outcome measures were the same and study group characteristics similar, studies were pooled and meta-analysis undertaken using Review Manager (Revman) software (Version 5.2). Effect sizes for outcomes were expressed using the mean difference (MD) and 95% confidence intervals (CIs). For each trial included in the meta-analyses, the MD was calculated using change from baseline scores for control and experimental groups. Standard deviations for the MD were calculated according to the protocol described in the Cochrane Handbook for Systematic Reviews.22 The I2 statistic was used to measure statistical heterogeneity. Where I2 was 50% or less, the fixed-effects model was used. Where I2 was more than 50, the more conservative random-effects model (REM) was used.
RESULTS
Included Studies
Eighteen RCTs met the eligibility criteria for the review (n = 765) (Figure 1). Studies were conducted in 9 countries: Australia (3), the United States (6), Denmark, Japan, Korea, Taiwan, France (2), Canada and Switzerland (2). A summary of population, intervention, comparator, and outcome characteristics is listed in Table 1.
Figure 1.
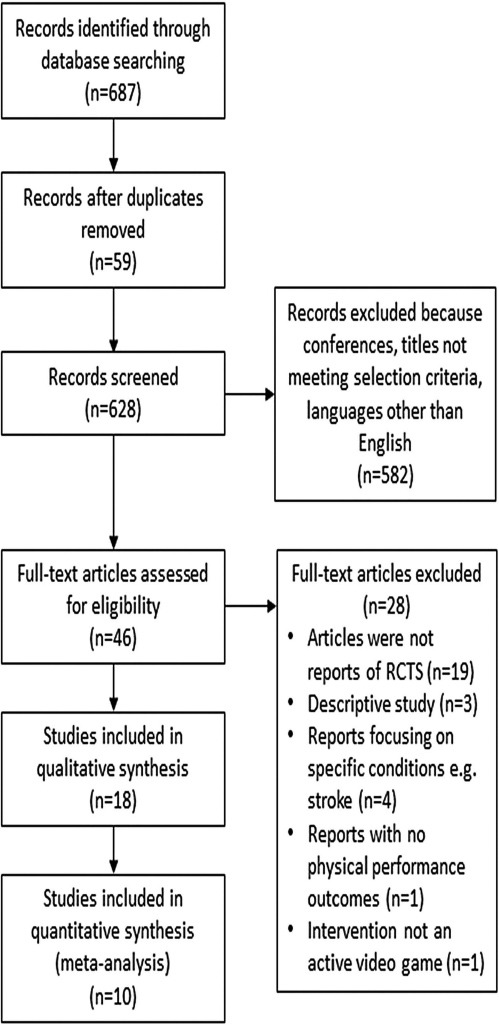
Study selection flow diagram.
Table 1. Study Participant and Intervention Description.
| Study | Group | Group Size | Age | SD | Intervention Description | Outcome Measures | Outcomes |
|---|---|---|---|---|---|---|---|
| Bieryla and Dold23 | IG | 12 | 82.6 | 1.6 | AVGs alone. Wii yoga (half-moon, chair, warrior), aerobic (torso twists), and balance games (soccer heading, ski jump) modes. Advanced as participants could manage |
Balance and mobility • Berg Balance Scale (BBS) • Timed Up and Go (TUG) • Forward Reach • Fullerton Advanced Balance Scale |
• Significant change in BBS pre/post for IG but not CG • No significant change for other measures |
| CG | 12 | 80.5 | 7.8 | No intervention | |||
| Cho et al24 | IG | 17 | 73.1 | 1.1 | AVGs alone. Wii Fit ski slalom, table tilt and balance bubble |
Balance • COP eyes open and closed |
• Significant improvement (reduction) in COP excursion for IG but not CG |
| CG | 15 | 71.7 | 1.2 | No intervention | |||
| Duque et al32 | IG | 30 | 79.3 | 10 | AVGs combined with exercise. Balance Rehabilitation Unit—combination of visual vestibular retraining (saccadic, optokinetic stimulation, vestibular optokinetic and vestibular-ocular reflex exercises performed while standing) and postural retraining using the virtual reality head set, consisting of 3 different postural training games with increasing levels of complexity, in addition to usual care |
Balance • Limits of stability (LOS) and COP using the “Balance Rehabilitation Unit” • Survey of Activities and Fear of Falling in the Elderly (SAFE) questionnaire |
• Significant within-group improvements in COP and LOS for the IG but no significant difference between IG and CGs. Significant improvement (reduction) in COP excursion and improvement (increase) in LOS for IG compared with CG at 9 mos for some conditions • SAFE scores significantly better in IG compared with CG |
| CG | 40 | 75 | 8 | Usual care. A care plan on falls prevention including an invitation to join an exercise program (after the Otago protocol) medication review, home visit by an occupational therapist, hearing and visual assessment, nutritional supplements and vitamin D supplementation as required and education materials on falls prevention | |||
| Franco et al26 | IG | 11 | 79.8 | 4.7 | AVGs combined with exercise. Wii Fit balance, Individual supervised sessions plus home exercise program |
Balance and acceptability • Berg Balance Scale (BBS) • Tinetti Gait and Balance Assessment (POMA) • SF36 health survey • Wii Fit enjoyment questionnaire- specifically developed for the study |
• No significant between-group pre/post differences in BBS, POMA or SF36 scores • Participants enjoyed AVGs and many preferred them to usual exercise |
| IG | 11 | 77.9 | 6.9 | Balance exercise. “Matter of Balance” group exercises warm-up, strength and balance and cool down | |||
| CG | 10 | 76.9 | 6.3 | No intervention | |||
| Jorgensen et al27 | IG | 28 | 75.9 | 5.7 | AVGs combined with exercise. Wii Fit Balance games, leg strength and standing row squat |
Physical performance and balance • Maximal isometric voluntary contraction (MVC) of leg extensors • Postural sway (COP) • Timed Up and Go (TUG) • Short-form Falls Efficacy Scale International (FES-1) • 30-s repeated chair stand test |
• Significant improvement in MVC of IG compared with CG • No significant difference between groups for COP • Significant between-group differences in favor of the IG for TUG, FES-1, and chair stand tests |
| CG | 30 | 73.7 | 6.1 | Placebo insoles | |||
| Lai et al25 | IG | 15 | 70.6 | 3.5 | AVGs alone. Xavix measured step system (XMSS)—uses a step mat plus console and television |
Balance and mobility • Berg Balance Scale (BBS) • Timed Up and Go (TUG) • Modified Falls Efficacy Scale (MFES) • Unipedal stance test • Postural sway: sway area, sway velocity and COP tests |
• Significant within-group improvements in BBS, TUG and MFES and Sway Velocity test for the IG. No significant within-group improvements in BBS, TUG and MFES and Sway Velocity test for the CG. Between-group comparison not reported |
| CG | 15 | 74.5 | 4.7 | No intervention | |||
| Laver et al28 | IG | 22 | 85.2 | 4.7 | AVGs alone. Wii Fit program set and supervised by physiotherapists delivered one to one including balance, strength and light aerobics in standing |
Balance and mobility • Timed Up and Go (TUG) • Short Physical Performance Battery (SPPB) • Modified Berg Balance Scale (MBBS) • Timed Instrumental Activities of Daily Living (Timed IADL) test • Functional Independence Measure (FIM) • Activity-Specific Balance Confidence Scale (ABC) • Health-related quality of life (EQ5D) |
• Rate of improvement per session significantly greater in the IG than in the CG for TUG and BBS scores • No significant differences were found between groups for the SPPB, Timed IADL Test, ABC Scale or EQ5D |
| CG | 22 | 84.6 | 4.4 | Conventional physiotherapy. Walking balancing, transfers | |||
| Lee et al29 | IG | 40 | 75.2 | 6.6 | AVGs combined with exercise. Wii Fit and Wii sports games, walking, chair stands with weighted vest and another 5-min walk |
Balance and gait parameters • Balance Efficacy Scale (BES) • Gait performance parameters measured using GAITRite walkway, that is, velocity, stride length, cadence, double support time and swing time |
• No significant between-group differences in BES • Significant within-group differences in gait velocity, stride length, cadence, swing time and reduction in double support time but no between-group differences |
| CG | 42 | Conventional exercise, for example, chair stands, chair lunge, heel raise, stepping, and arm curl using Thera-Bands; stretching (upper and lower body muscles) and balancing activities (stand on one leg, hold a small ball) | |||||
| Maillot et al30 | IG | 16 | 73.5 | 4.1 | AVGs alone. Three time periods of (i) Nintendo Wii Fit (plus balance board), in pairs, playing Wii boxing/tennis/bowling; (ii) individual Wii balance board games; (iii) a final Wii game for either balance, energy, or cognition |
Physical performance and cognitive function • Senior Fitness Test (SFT): includes chair-stand test, arm curl, 6-Min Walking Test, chair-sit-and-reach test, back-scratch test and 8-foot up-and-go test • Cognitive test battery: (i) executive control tasks; (ii) visuospatial tasks; (iii) processing-speed tasks |
• Significant improvement in SFT scores in favor of the IG for all measures except flexibility • Significant improvement scores in favor of the IG for executive control and processing speed but not for visuospatial tasks |
| CG | 16 | 73.5 | 3.0 | No intervention | |||
| Pichierri et al31 | IG | 15 | 86.9 | 5.1 | AVGs combined with exercise. Exercise program consisting of progressive resistance and postural balance training including 2 sets of 10-15 repetitions of lower limb exercises with training intensity controlled using Borg's perceived exertion scale; plus a progressive video game dancing program using a modification of Step Mania (Dance Dance Revolution) |
Balance and gait parameters • Foot placement accuracy (FPA) • Gait performance parameters measured using GAITRite walkway, ie, velocity, stride length, cadence, double support time and swing time Gaze parameters • Falls Efficacy Scale International (FES-IG) |
• No significant difference between groups for FPA • Significant between-group differences in favor of the IG for gait velocity, stride length, cadence, swing time and single support time under dual-task conditions • No significant difference between groups for FES-IG |
| CG | 16 | 85.6 | 4.2 | Conventional exercise. Progressive resistance and postural balance training as above | |||
| Pichierri et al33 | IG | 9 | 83.6 | 3.4 | AVGs combined with exercise. Warm-up, resistance exercises with weighted vests, balance exercises, and dance video gaming using a modification of Step Mania (Dance Dance Revolution) |
Balance • Stepping reaction time tasks (SRT) using a force platform under single- and dual-task (Stroop test) conditions |
• Significant between-group differences in favor of the IG SRT under dual-task conditions |
| CG | 6 | 86.2 | 4.8 | No intervention | |||
| Pluchino et al34 | IG | 12 | 70.7 | 8.5 | AVGs alone. Wii Fit Balance, that requires weight shifts to lay the game: soccer heading, ski slalom, ski jump, table tilt, tightrope walk, river bubble, penguin slide snowboard slalom, lotus focus |
Balance and mobility • Timed Up and Go (TUG) • One-leg stance • Forward Reach (FR) • Tinetti Performance-Oriented Mobility Assessment (POMA) • COP, dynamic posturography, postural sway test using a force platform • Falls Efficacy Scale (FES) |
• No significant difference between groups for TUG, one leg stance, FR, or POMA • No significant difference between groups for COP measures; all groups showed a significant improvements in COP parameters over time • No significant difference between groups for FES |
| IG | 14 | 69.3 | 6.0 | Tai Chi supervised program: 12 movements using small forward and backward steps, weight transfers from 1 leg to the other, posture alignment, small knee bends and moving slowly with a gentle resistance | |||
| CG | 14 | 76.0 | 7.7 | Conventional exercise. Traditional supervised balance program | |||
| Ray et al35 | IG | 29 | 75.0 | NS | AVGs combined with exercise. Wii Fit Wii-balance board and weighted vests. The intervention included 15-25 chair stands while wearing the weight vest and bouts of walking for 5-10 min at a time |
Balance and physical performance • Senior Fitness Test: includes chair-stand test, arm curl, 6-Min Walking Test, chair-sit-and-reach test, back-scratch test and 8-foot up-and-go test • “NeuroCom Sensory Organization Test”: COP and limits of stability (LOS), postural sway under a range of conditions (control, visual, auditory and cognitive distractors) (Stroop test) |
• Significant improvement in favor of IG for 8-ft up-and-go test and 30-s chair stands • No significant difference between groups for COP or LOS measures; all groups showed a significant improvements in COP parameters over time |
| IG | 40 | Conventional exercise. Group fitness strengthening exercises for lower leg and upper body strength, plus flexibility and walking | |||||
| CG | 18 | Conventional exercise. Balance using functional activities, for example, standing, stepping, and walking on a compliant surface; walking and pivoting 180°; stair walking | |||||
| Rendon et al36 | IG | 20 | 85.7 | 4.3 | AVGs combined with exercise. Wii Fit Balance plus exercycle |
Balance and mobility • 8-ft Timed Up and Go (TUG) • Activity-specific Balance Confidence Scale (ABC) • Geriatric Depression Scale (GDS) |
• Significant improvement in 8-ft TUG in favor of AVG group • Significant improvement in ABS score in favor of AVG group • Not significant difference in GDS |
| CG | 20 | 83.3 | 6.2 | No intervention | |||
| Sato et al37 | IG | 28 | 70.7 | 5.35 | AVGs alone. Balance games custom designed using Kinect motion sensor |
Balance, mobility, and gait parameters • Berg Balance Scale (BBS) • Functional reach (FR) • 30-s chair stand • Gait performance parameters measured using 3D motion analysis (ie, velocity, stride length, cadence, double support time, and swing time) |
• Significant between-group differences in favor of the IG for BBS, FR and 30-s Chair Stand |
| CG | 26 | 68.5 | 5.47 | No intervention | |||
| Schoene et al38 | IG | 19 | 77.5 | 4.5 | AVGs alone. Dance Dance Revolution—an open source platform with Step Mania, specifically modified, using a dance mat |
Balance and mobility • Stepping Reaction Time (SRT) • Physiological Profile Assessment test (PPA) battery: (i) visual contrast sensitivity, (ii) hand reaction time, (iii) standing balance on foam, (iv) knee joint position sense, and (v) knee extension strength • Timed Up and Go (TUG) • 5 times sit-stand |
• Significant between-group differences in favor of the IG for SRT • Significant between-group differences in favor of the IG for PPA composite scores • Significant between-group differences in favor of the IG for dual-task TUG scores • No significant between group-differences for TUG |
| CG | 18 | 78.4 | 4.5 | No intervention | |||
| Szturm et al39 | IG | 15 | 80.5 | 6.0 | AVGs alone. Custom-designed weight transfer progressive balance games on a pressure mat ± sponge surface, linked to computer monitor, requiring movement of COP |
Balance, mobility, and gait parameters • Berg Balance Scale (BBS) • Timed Up and Go (TUG) • Activity-specific Balance Confidence Scale (ABC) • Gait performance parameters measured using GAITRite walkway • Dynamic balance tests performed on foam. Outcome for tests was a “Loss of Balance” score |
• Significant between-group improvements in BBS scores in favor of the IG • No significant within or between-group differences in TUG scores • Significant within-group improvements in ABC scores in the IG the IG but not in the CG. • No significant within or between-group differences in gait velocity • Significant within-group improvements in “Loss of Balance” scores on foam in the IG but not in the CG |
| CG | 15 | 81.0 | 7.0 | Conventional exercise. Strength and balance program using Thera-Band, leg weights, cycle, weight-bearing balance exercises (eg, sit to stand, squats, and step-ups) | |||
| Toulotte et al40 | IG | 9 | 72.2 | 8.6 | AVGs alone. Wii Fit including balance board |
Balance • Tinetti balance test battery (POMA) • Unipedal standing |
• Significant within-group improvements in POMA scores in Exercise group, Wii group and Wii plus exercise groups • No between-group differences reported • Significant within-group improvements in Unipedal standing scores in exercise group, and Wii plus exercise groups. No significant change in Wii group |
| Bieryla and Dold23 | IG | 12 | 82.6 | 1.6 | AVGs alone. Wii yoga (half-moon, chair, warrior), aerobic (torso twists), and balance games (soccer heading, ski jump) modes. Advanced as participants could manage |
Balance and mobility • Berg Balance Scale (BBS) • Timed Up and Go (TUG) • Forward Reach • Fullerton Advanced Balance Scale |
• Significant change in BBS pre/post for IG but not CG • No significant change for other measures |
| CG | 12 | 80.5 | 7.8 | No intervention | |||
| Cho et al24 | IG | 17 | 73.1 | 1.1 | AVGs alone. Wii Fit ski slalom, table tilt and balance bubble |
Balance • COP eyes open and closed |
• Significant improvement (reduction) in COP excursion for IG but not CG |
| CG | 15 | 71.7 | 1.2 | No intervention | |||
| Duque et al32 | IG | 30 | 79.3 | 10 | AVGs combined with exercise. Balance Rehabilitation Unit—combination of visual vestibular retraining (saccadic, optokinetic stimulation, vestibular optokinetic and vestibular-ocular reflex exercises performed while standing) and postural retraining using the virtual reality head set, consisting of 3 different postural training games with increasing levels of complexity, in addition to usual care |
Balance • Limits of stability (LOS) and COP using the “Balance Rehabilitation Unit” • Survey of Activities and Fear of Falling in the Elderly (SAFE) questionnaire |
• Significant within-group improvements in COP and LOS for the IG but no significant difference between IG and CGs. Significant improvement (reduction) in COP excursion and improvement (increase) in LOS for IG compared with CG at 9 mos for some conditions. • SAFE scores significantly better in IG compared with CG |
| CG | 40 | 75 | 8 | Usual care. A care plan on falls prevention including an invitation to join an exercise program (following the Otago protocol) medication review, home visit by an occupational therapist, hearing and visual assessment, nutritional supplements and vitamin D supplementation as required and education materials on falls prevention | |||
| Franco et al26 | IG | 11 | 79.8 | 4.7 | AVGs combined with exercise. Wii Fit balance, individual supervised sessions plus home exercise program |
Balance and acceptability • Berg Balance Scale (BBS) • Tinetti Gait and Balance Assessment (POMA) • SF36 health survey • Wii Fit enjoyment questionnaire- specifically developed for the study |
• No significant between-group pre/post differences in BBS, POMA or SF36 scores • Participants enjoyed AVGs and many preferred them to usual exercise |
| IG | 11 | 77.9 | 6.9 | Balance exercise. “Matter of Balance” group exercises warm-up, strength and balance and cool-down | |||
| CG | 10 | 76.9 | 6.3 | No intervention | |||
| Jorgensen et al27 | IG | 28 | 75.9 | 5.7 | AVGs combined with exercise. Wii Fit Balance games, leg strength and standing row squat |
Physical performance and balance • Maximal isometric voluntary contraction (MVC)of leg extensors • Postural sway (COP) • Timed Up and Go (TUG) • Short-form Falls Efficacy Scale International (FES-1) • 30-s repeated chair stand test |
• Significant improvement in MVC of IG compared with CG • No significant difference between groups for COP • Significant between-group differences in favor of the IG for TUG, FES-1 and chair stand tests |
| CG | 30 | 73.7 | 6.1 | Placebo insoles | |||
| Lai et al25 | IG | 15 | 70.6 | 3.5 | AVGs alone. Xavix measured step system (XMSS)––uses a step mat plus console and television |
Balance and mobility • Berg Balance Scale (BBS) • Timed Up and Go (TUG) • Modified Falls Efficacy Scale (MFES) • Unipedal stance test • Postural sway: sway area, sway velocity, and COP tests |
• Significant within-group improvements in BBS, TUG and MFES and Sway Velocity test for the IG. No significant within-group improvements in BBS, TUG and MFES and Sway Velocity test for the CG. Between-group comparison not reported |
| CG | 15 | 74.5 | 4.7 | No intervention | |||
| Laver et al28 | IG | 22 | 85.2 | 4.7 | AVGs alone. Wii Fit program set and supervised by physiotherapists delivered one to one including balance, strength and light aerobics in standing |
Balance and mobility • Timed Up and Go (TUG) • Short Physical Performance Battery (SPPB) • Modified Berg Balance Scale (MBBS) • Timed Instrumental Activities of Daily Living (Timed IADL) test • Functional Independence Measure (FIM) • Activity-Specific Balance Confidence Scale (ABC) • Health-related quality of life (EQ5D) |
• Rate of improvement per session significantly greater in the IG than in the CG for TUG and BBS scores • No significant differences were found between groups for the SPPB, Timed IADL Test, ABC Scale, or EQ5D |
| CG | 22 | 84.6 | 4.4 | Conventional physiotherapy. Walking balancing, transfers | |||
| Lee et al29 | IG | 40 | 75.2 | 6.6 | AVGs combined with exercise. Wii Fit and Wii sports games, walking, chair stands with weighted vest and another 5-min walk | Balance and gait parameters • Balance Efficacy Scale (BES) • Gait performance parameters measured using GAITRite walkway (ie, velocity, stride length, cadence, double support time, and swing time) | • No significant between-group differences in BES • Significant within-group differences in gait velocity, stride length, cadence, swing time and reduction in double support time but no between-group differences |
| CG | 42 | Conventional exercise, for example, chair stands, chair lunge, heel raise, stepping, and arm curl using Thera-Bands; stretching (upper and lower body muscles) and balancing activities (stand on one leg, hold a small ball) | |||||
| Maillot et al30 | IG | 16 | 73.5 | 4.1 | AVGs alone. Three time periods of (i) Nintendo Wii Fit (plus balance board), in pairs, playing Wii boxing/tennis/bowling; (ii) individual Wii balance board games; (iii) a final Wii game for either balance, energy, or cognition |
Physical performance and cognitive function • Senior Fitness Test (SFT): includes chair-stand test, arm curl, 6-Min Walking Test, chair-sit-and-reach test, back-scratch test and 8-ft up-and-go test • Cognitive test battery: (i) executive control tasks, (ii) visuospatial tasks, (iii) processing-speed tasks |
• Significant improvement in SFT scores in favor of the IG for all measures except flexibility • Significant improvement scores in favor of the IG for executive control and processing speed but not for visuospatial tasks |
| CG | 16 | 73.5 | 3.0 | No intervention | |||
| Pichierri et al31 | IG | 15 | 86.9 | 5.1 | AVGs combined with exercise. Exercise program consisting of progressive resistance and postural balance training including 2 sets of 10-15 repetitions of lower limb exercises with training intensity controlled using Borg's perceived exertion scale; plus a progressive video game dancing program using a modification of Step Mania (Dance Dance Revolution) | Balance and gait parameters • Foot placement accuracy (FPA) • Gait performance parameters measured using GAITRite walkway (ie, velocity, stride length, cadence, double support time, and swing time Gaze parameters) • Falls Efficacy Scale International (FES-IG) | • No significant difference between groups for FPA • Significant between-group differences in favor of the IG for gait velocity, stride length, cadence, swing time and single support time under dual-task conditions • No significant difference between groups for FES-IG |
| CG | 16 | 85.6 | 4.2 | Conventional Exercise. Progressive resistance and postural balance training as above | |||
| Pichierri et al33 | IG | 9 | 83.6 | 3.4 | AVGs combined with exercise. Warm-up, resistance exercises with weighted vests, balance exercises, and dance video gaming using a modification of Step Mania (Dance Dance Revolution) |
Balance • Stepping reaction time tasks (SRT) using a force platform under single- and dual-task (Stroop test) conditions |
• Significant between-group differences in favor of the IG SRT under dual-task conditions |
| CG | 6 | 86.2 | 4.8 | No intervention | |||
| Pluchino et al34 | IG | 12 | 70.7 | 8.5 | AVGs alone. Wii Fit Balance, that requires weight shifts to lay the game: soccer heading, ski slalom, ski jump, table tilt, tightrope walk, river bubble, penguin slide snowboard slalom, lotus focus |
Balance and mobility • Timed Up and Go (TUG) • One-leg stance • Forward Reach (FR) • Tinetti Performance-Oriented Mobility Assessment (POMA) • COP, dynamic posturography, postural sway test using a force platform • Falls Efficacy Scale (FES) |
• No significant difference between groups for TUG, one leg stance, FR, or POMA • No significant difference between groups for COP measures; all groups showed a significant improvements in COP parameters over time • No significant difference between groups for FES |
| IG | 14 | 69.3 | 6.0 | Tai Chi supervised program: 12 movements using small forward and backward steps, weight transfers from one leg to the other, posture alignment, small knee bends and moving slowly with a gentle resistance | |||
| CG | 14 | 76.0 | 7.7 | Conventional exercise. Traditional supervised balance program | |||
| Ray et al35 | IG | 29 | 75.0 | NS | AVGs combined with exercise. Wii Fit Wii-balance board and weighted vests. The intervention included 15-25 chair stands while wearing the weight vest and bouts of walking for 5-10 min at a time |
Balance and physical performance • Senior Fitness Test: includes chair-stand test, arm curl, 6-Min Walking Test, chair-sit-and-reach test, back-scratch test and 8-ft up-and-go test • “NeuroCom Sensory Organization Test”: COP and limits of stability (LOS), postural sway under a range of conditions (control, visual, auditory, and cognitive distractors) (Stroop test) |
• Significant improvement in favor of IG for 8-ft up-and-go test and 30-s chair stands • No significant difference between groups for COP or LOS measures; all groups showed a significant improvements in COP parameters over time |
| IG | 40 | Conventional exercise. Group Fitness strengthening exercises for lower leg and upper body strength, plus flexibility and walking | |||||
| CG | 18 | Conventional exercise. Balance using functional activities, for example, standing, stepping and walking on a compliant surface; walking and pivoting 180°; stair walking | |||||
| Rendon et al36 | IG | 20 | 85.7 | 4.3 | AVGs combined with exercise. Wii Fit Balance plus exercycle |
Balance and mobility • 8-ft Timed Up and Go (TUG) • Activity-specific Balance Confidence Scale (ABC) • Geriatric Depression Scale (GDS) |
• Significant improvement in 8-ft TUG in favor of AVG group • Significant improvement in ABS score in favor of AVG group • Not significant difference in GDS |
| CG | 20 | 83.3 | 6.2 | No intervention | |||
| Sato et al37 | IG | 28 | 70.7 | 5.35 | AVGs alone. Balance games custom designed using Kinect motion sensor |
Balance, mobility, and gait parameters • Berg Balance Scale (BBS) • Functional reach (FR) • 30-s chair stand • Gait performance parameters measured using 3D motion analysis (ie, velocity, stride length, cadence, double support time, and swing time) |
• Significant between-group differences in favor of the IG for BBS, FR and 30-s Chair Stand |
| CG | 26 | 68.5 | 5.47 | No intervention | |||
| Schoene et al38 | IG | 19 | 77.5 | 4.5 | AVGs alone. Dance Dance Revolution—an open source platform with Step Mania, specifically modified, using a dance mat |
Balance and mobility • Stepping Reaction Time (SRT) • Physiological Profile Assessment test (PPA) battery: (i) visual contrast sensitivity, (ii) hand reaction time, (iii) standing balance on foam, (iv) knee joint position sense, and (v) knee extension strength • Timed Up and Go (TUG) • 5 times sit-stand |
• Significant between-group differences in favor of the IG for SRT. • Significant between-group differences in favor of the IG for PPA composite scores • Significant between-group differences in favor of the IG for dual-task TUG scores • No significant between-group differences for TUG |
| CG | 18 | 78.4 | 4.5 | No intervention | |||
| Szturm et al39 | IG | 15 | 80.5 | 6.0 | AVGs alone. Custom-designed weight transfer progressive balance games on a pressure mat ± sponge surface, linked to computer monitor, requiring movement of COP |
Balance, mobility, and gait parameters • Berg Balance Scale (BBS) • Timed Up and Go (TUG) • Activity-Specific Balance Confidence Scale (ABC) • Gait performance parameters measured using GAITRite walkway • Dynamic balance tests performed on foam. Outcome for tests was a “Loss of Balance” score |
• Significant between-group improvements in BBS scores in favor of the IG • No significant within or between-group differences in TUG scores • Significant within-group improvements in ABC scores in the IG the IG but not in the CG. • No significant within or between-group differences in gait velocity • Significant within-group improvements in “Loss of Balance” scores on foam in the IG but not in the CG. |
| CG | 15 | 81.0 | 7.0 | Conventional exercise. Strength and balance program using Thera-Band, leg weights, cycle, weight-bearing balance exercises (eg, sit to stand, squats, and step–ups) | |||
| Toulotte et al40 | IG | 9 | 72.2 | 8.6 | AVGs alone. Wii Fit including balance board |
Balance • Tinetti balance test battery (POMA) • Unipedal standing |
• Significant within-group improvements in POMA scores in exercise group, Wii group and Wii plus exercise groups • No between-group differences reported • Significant within-group improvements in Unipedal standing scores in exercise group, and Wii plus exercise groups. No significant change in Wii group. |
| IG | 9 | 84.2 | 8.1 | Conventional exercise alone. Adapted Physical Activities (APA): muscle strength, lower limb mobility, proprioception, balance | |||
| IG | 9 | 76.4 | 4.7 | AVGs combined with exercise APA and Wii Fit | |||
| CG | 9 | 71.8 | 8.0 | Board games and TV watching |
Abbreviations: AVGs, active video games; CG, control group; COP, center of pressure; IG, intervention group; NS, not significant, SD, standard deviation.
Seven trials compared AVGs with no intervention25,30,33,36–38 or usual care32; 5 trials compared AVGs with conventional exercise (ie, strength, balance, mobility, and/or balance exercises that did not use video game technology)28,29,31,35,39 and 3 trials compared AVGs with both conventional exercise and a no intervention control.26,34,40 The remaining trial compared AVGs with a placebo shoe insole.27
Risk of Bias
Four of the 18 trials were assessed as low risk of bias across 3 or more of the 6 items assessed.27,28,38,39 The remainder had 4 or more items assessed as either high or unclear risk because there was insufficient information reported for evaluation (Table 2).23–26,30–32,33–37,40
Table 2. Cochrane Risk of Bias Ratings for Included Trials.
| Study | Random Sequence Generation (Selection Bias) | Allocation Concealment (Selection Bias) | Blinding of Participants and Personnel (Performance Bias) | Blinding of Outcome Assessment (Detection Bias) | Incomplete Outcome Data (Attrition Bias) | Selective Reporting (Reporting Bias) |
|---|---|---|---|---|---|---|
| Bieryla and Dold23 | Unclear risk | Unclear risk | High risk | High risk | High risk | Unclear risk |
| Cho et al24 | Unclear risk | Unclear risk | High risk | Unclear risk | Unclear risk | Unclear risk |
| Duqu et al32 | Unclear risk | Unclear risk | High risk | Low Risk | Unclear risk | High risk |
| Franco et al26 | Low Risk | High risk | High risk | High risk | Low Risk | Unclear risk |
| Jorgensen et al27 | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk | Low Risk |
| Lai et al25 | Unclear risk | Unclear risk | High risk | Unclear risk | Unclear risk | Unclear risk |
| Laver et al28 | Low Risk | Low Risk | High risk | Low Risk | Low Risk | Unclear risk |
| Lee et al29 | Unclear risk | Unclear risk | High risk | Unclear risk | Low Risk | Unclear risk |
| Maillot et al30 | Unclear risk | Unclear risk | High risk | Unclear risk | High risk | Unclear risk |
| Pichierri et al31 | Low Risk | Unclear risk | High risk | Unclear risk | Unclear risk | Low Risk |
| Pichierri et al33 | Low Risk | Unclear risk | High risk | High risk | High risk | Unclear risk |
| Pluchino et al34 | Low Risk | Low Risk | High risk | Unclear risk | High risk | Unclear risk |
| Ray et al35 | Unclear risk | Unclear risk | High risk | Unclear risk | Unclear risk | Unclear risk |
| Rendon et al36 | Unclear risk | Unclear risk | High risk | Unclear risk | Low Risk | Unclear risk |
| Sato et al37 | Low Risk | Unclear risk | High risk | Unclear risk | Low Risk | Unclear risk |
| Schoene et al38 | Low Risk | Low Risk | High risk | Low Risk | Low Risk | Low Risk |
| Szturm et al39 | Unclear risk | Unclear risk | High risk | Low Risk | Low Risk | Low Risk |
| Toulotte et al40 | Unclear risk | Unclear risk | High risk | Unclear risk | Low Risk | High risk |
For all outcomes analyzed, there was no indication that outcome measures were influenced either positively or negatively by the risk of bias scores.
Intervention Characteristics
The duration of AVG programs for community dwellers was 3 to 20 weeks, with most offered for 8 weeks, usually 2 to 3 times weekly for approximately 40 minutes each session. For hospitalized older people, the program ran daily for the duration of the patient's stay (usually 7 days).
With the exception of 1 trial, delivered in the home environment,38 all trials were supervised programs conducted in a gymnasium or research center setting. Most were delivered on an individual basis, although 2 trials used either game play with a partner30 or in small groups.31
Eleven trials used Nintendo Wii,23,24,26–30,34–36,40 5 used pressure-sensitive mat systems,25,31,33,38,39 1 used the Kinect motion sensor,37 and the remaining trial used a virtual reality head set.32
The focus of all trials except 130 was to improve balance. Nine trials used solely AVGs.23–25,28,30,34,37–39 Eight trials combined the AVGs with conventional exercise to develop balance, strength, or aerobic capacity.26,27,29,31–33,35,36 One 3-arm trial compared AVGs alone with exercise alone and a third intervention group that combined AVGs with exercise.40
There was no clear indication that trials that combined exercise and AVGs programs had better or worse outcomes and trials that used AVGs alone.
Participant Characteristics
Participants were mostly community-dwelling older people. The exception was 1 trial conducted in an acute hospital setting,28 and 2 trials that recruited from care homes.31,33 The average age of community-dwelling participants was 75.6 (6.9) years (n = 675) and of hospitalized or nursing home older participants was 85.3 (4.5) years (n = 90).
Inclusion and Exclusion Criteria
Thirteen trials limited inclusion to higher functioning older people24–26,30,31,33–38,40 (ie, those with no major cardiovascular, neuromuscular, or vestibular impairments, who were independent in ambulatory function). Three trials targeted people with balance limitations or falls risk.27,32,39 One trial did not report exclusion criteria29 and the remaining trial recruited hospitalized older people.28
Twelve trials excluded those with cognitive impairment.24–26,28,31–34,37–40 Cognitive impairment was not specified as an exclusion criterion in 1 trial, but baseline cognitive scores indicated normal cognition for all participants.24 Cognitive status was not specified in the remaining 5 trials.23,27,29,35,36
Physical Performance (Mobility) Measures
Changes in physical performance measures were assessed in 10 trials.23,25,27,28,30,34–36,38,39 The most frequently used mobility measure was the Timed Up and Go (TUG)41 and its modification, the 8-ft Up and Go.42 Seven trials used the TUG23,25,27,28,34,38,39 and 3 trials used the 8-ft Up and Go.30,35,36
One trial43 used the Short Physical Performance Battery44 and 2 trials30,35 used the Senior Fitness Test, which includes the 30-second chair stand test.45
The mean baseline TUG score for trials that used this measure was 10.3 (4.1) seconds (n = 169),23,25,27,34,38 which was within the expected range of 7 to 15 seconds for healthy older people.46,47 The mean baseline 8-ft TUG score was 7.9 (1.6) seconds (n = 159)30,36 which was also within the normal range for healthy older people.48 In participants with balance and mobility limitations, baseline TUG scores were higher (20.9 (3.5) seconds; n = 30)39 and in the only inpatient-based study,28 baseline TUG group means were considerably higher (36.7 (18.7) seconds; n = 44).
A meta-analysis on pooled TUG scores from 6 trials (n = 206) that compared AVGs with conventional exercise or no intervention failed to reach significance (REM, MD = −2.29; 95% CI, −5.20 to 0.64).
A meta-analysis on pooled 30-second chair stand scores from 4 trials (n = 188)27,30,35,37 showed a significant effect in favor of AVGs (REM, MD = 3.99; 95% CI, 1.92-6.05) (Figure 2). No significant effect was found for the 5 times sit-to-stand used in 1 trial.38
Figure 2.
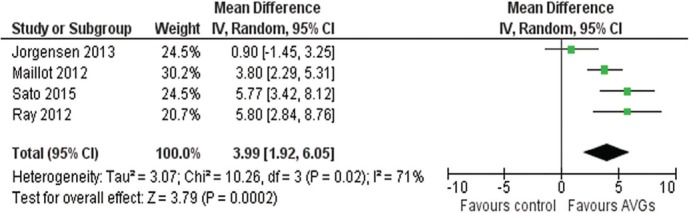
Summary of inverse variance (IV) random-effects meta-analysis examining effects of active video games (AVGs) on 30 second chair stand scores.
Balance Measures
Changes in direct measures of balance were assessed in 5 trials.24,25,32,34,35 Two trials reported significant within-group differences in center of pressure (COP) in the intervention group,24,25 but no significant difference between intervention and control (no intervention) groups. The 3 trials that compared AVGs with conventional exercise reported significant within-group differences in COP34,35 and limits of stability32,35 measures for both AVG and conventional exercise groups, but no significant difference between groups for COP measures. This suggests AVGs were as effective as conventional exercise at improving COP measures.32,34,35
Finally, 2 trials measured stepping reaction time in response to visual cues.33,38 Both reported significant between-group differences in favor of AVGs over the control group.
Indirect measures of balance, including 1 legged standing, the forward reach test, the Berg Balance Scale (BBS),49 and the Tinetti Performance-Oriented Mobility Assessment (the Tinetti POMA),50 were assessed in 9 trials.23,25,26,28,34,36,37,39,40 Five trials used the BBS,23,25,26,37,39 1 used a modified BBS,28 and 3 used versions of the Tinetti POMA.26,34,40
The mean baseline BBS score for trials that used this measure was 51.7 (5.2) points (n = 126),23,25,26,37 or for trials that used the Tinetti POMA,23,34 the mean baseline score was 26.4 (0.9) points (n = 72) indicating normal balance.50,51 For participants with limited balance and mobility, baseline BBS scores were in the low to medium fall risk category (range 37-42 points).39
Mean BBS scores from 3 trials in community-dwelling participants25,26,37 (n = 105) that compared AVGs with no intervention on BBS scores were pooled for meta-analyses (Figure 3). A significant difference in favor of AVGs over no intervention was demonstrated (MD = 0.73; 95% CI, 0.17-1.29). Pooled data (n = 49) that compared active video game BBS scores with conventional exercise26,39 also showed an effect in favor of AVGs (MD = 4.33; 95% CI, 2.93-5.73) (Figure 2). In addition, Laver et al28 also reported a significant improvement in the modified BBS scores in hospitalized inpatients in favor of AVGs compared with conventional exercise (MD = 0.59; 95% CI, 0.02-1.16).
Figure 3.
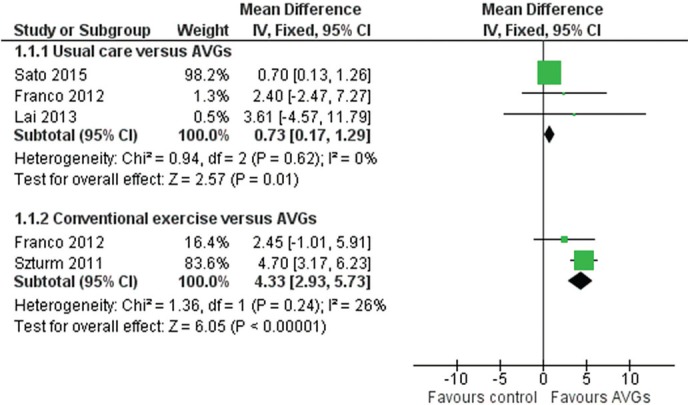
Summary of inverse variance (IV) random-effects meta-analysis examining effects of active video games (AVGs) on Berg Balance Scale sores.
For trials that used the Tinetti POMA, no significant between-group changes in balance scores were reported.26,34,40
Other individual item balance measures used were the single-legged stance25,34 and the forward reach test.23,34,37 One trial reported a significant change in the forward reach score for the AVG group over the control,37 but no significant findings were reported for the single-legged stance.
Self-Report Balance Confidence Measures
Three trials used the Activities-Specific Balance Confidence Scale28,36,39 and 5 trials used a Falls Efficacy Scale (FES).25,27,31,34,38
Significant change scores in favor of the AVGs were reported for the Activities-Specific Balance Confidence Scale in 236,39 of the 3 trials.28
Differences in study participants and variation in a FES used precluded combined analyses of the subjective balance measures. Of the 5 trials that used an FES, 2 showed significant between-group differences favoring AVGs25,27 and 3 showed no significant differences between groups.31,34,38
Adverse Events
Two trials monitored adverse events.28,38 Of these, 1 reported adverse events that were minor in nature (musculoskeletal strain, feeling giddy) and occurred in both control (conventional exercise) and intervention groups.28
Trial Completion and Program Adherence Rates
Trial completion rate was defined as the number of participants who completed the trial. The median trial completion rate was 89% (interquartile range, 80-100).
Program adherence was defined as the percentage of prescribed exercise sessions completed over the program duration. For the 10 trials that reported program adherence, the range was 77% to 100% in the intervention (AVG) group and 87% to 100% in the control group,26,27,30–34,37,38,43 which is at the higher end of previously reported adherence rates for exercise RCTs.52 On the basis of the reported reasons for participant dropouts, there was no indication that completion or adherence rates were associated with any dislike of the intervention (AVG) itself.
Game Appeal
Five trials evaluated participants' perceptions of game appeal.26,27,30,38,43 Of these, 4 reported positive feedback, noting that participants found AVGs to be motivating and enjoyable,27,38 manageable and comparable or preferable to other physical activity.26,30 The fifth trial, which used hospital inpatients,28,43 reported no strong preference for the way in which their therapy was delivered before therapy commencement. However, after using the AVGs, respondents reported a preference for conventional therapy, citing they felt it to be more effective, despite having not received the other approach.43
DISCUSSION
This review included 18 RCTs that compared AVGs with conventional exercise or with no intervention or usual care in older people. Active video games were found to be more effective than conventional exercise and no intervention for improving balance (BBS) and mobility (30-second sit to stand) in community-dwelling older people. In addition, the only trial that enrolled hospitalized older people reported that AVGs were more effective at improving balance and mobility scores when compared with conventional rehabilitation.
Strengths and Limitations
This is the first systematic review of AVGs that has included a meta-analysis of RCTs for improving physical performance measures in older people. Limitations of this review include the relatively high risk of bias scores of some of the trials included in the meta-analysis. The diversity in trial design and outcome measures limited the extent to which study results could be pooled. To minimize this heterogeneity, only studies with the same outcome measures were pooled. For this reason analyses were undertaken on a small number of studies, which increased the CIs for pooled data. Furthermore, the conservative assumptions made for pooled data regarding standard deviations may have influenced the calculated effect size effects.
Participants
Participant eligibility criteria of included trials were strict, with exclusion of people with cognitive impairment and mobility limitations, with the exception of 1 trial in an acute hospital environment.28 Because of this, it is unclear whether AVGs are equally suitable for older people with significant cognitive impairments or with balance or mobility limitations.
Interestingly, the high baseline mobility and balance scores of participants in some trials might have masked clinically relevant improvements that may be seen in a more mobility-limited group of older people. Although the improvement in BBS scores for AVGs compared with conventional exercise shown in the meta-analyses was above the 4-point change considered clinically meaningful,53 some trials noted that participants scored near the ceiling of the baseline balance tests, making it difficult to measure improvement.26,27,34
Program Usability and Safety
With the exception of 1 trial conducted in the home environment,38 game play was supervised and offered to individuals rather than groups. Whether participants other than high-functioning individuals could manage the AVGs without supervision has not been adequately explored. Nevertheless, there were few adverse events reported, suggesting the AVGs are safe when supervised.
The program adherence rates were good, but the intervention durations were short. Hence, the high adherence was likely related to the novelty factor; and the sustained effect of AVG use is unclear.
In terms of game appeal, community dwellers enjoyed the games. However, the hospitalized older people who received AVGs reported a preference for conventional therapy.43 This variance of opinion may be due to both an older person's perception of using AVGs for rehabilitation, and the suitability of the game for the older person, in terms of the visual display and the ease of use of the control devices. Some trials modified the AVGs to suit the older person, in terms of reduction of onscreen information, selection of age-appropriate music, and speed of play.31,37,54 Future development of AVGs for older people may need to consider these aspects of game play.
Lastly, whether AVGs can be used with groups rather than individuals requires investigation. Environments such as care homes do not always have the capacity to supervise individual exercise programs. On this basis, AVGs may be unsuitable for a group exercise program, unless combined with other activities as part of an activity circuit.
SUMMARY
Active video games are a useful intervention for improving physical performance measures of balance and mobility in older people. Future work may consider monitoring adherence to an AVG program combined with conventional exercise, offered over longer period (12 months), to older people with a broader range of physical and cognitive abilities.
Footnotes
The authors declare no conflicts of interest.
Bernadette Williams-York was the Decision Editor.
REFERENCES
- 1.Buchman AS, Wilson RS, Yu L, James BD, Boyle PA, Bennett DA. Total daily activity declines more rapidly with increasing age in older adults. Arch Gerontol Geriatr. 2014;58(1):74–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johannsen DL, Delany JP, Frisard MI, et al. Physical activity in aging: comparison among young, aged, and nonagenarian individuals. J Appl Physiol. 2008;105(2):495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094–1105. [DOI] [PubMed] [Google Scholar]
- 4.Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41(7):1510–1530. [DOI] [PubMed] [Google Scholar]
- 5.Buchner DM. Physical activity and prevention of cardiovascular disease in older adults. Clin Geriatr Med. 2009;25(4):661–675. [DOI] [PubMed] [Google Scholar]
- 6.Shah R, Buchman A, Leurgans S, Boyle P, Bennett D. Association of total daily physical activity with disability in community-dwelling older persons: a prospective cohort study. BMC Geriatr. 2012;12(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LeBlanc AG, Chaput JP, McFarlane A, et al. Active video games and health indicators in children and youth: a systematic review. PLoS One. 2013;8(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foley L, Maddison R. Use of active video games to increase physical activity in children: a (virtual) reality? Pediatr Exerc Sci. 2010;22(1):7–20. [DOI] [PubMed] [Google Scholar]
- 10.Bleakley CM, Charles D, Porter-Armstrong A, McNeill MD, McDonough SM, McCormack B. Gaming for Health. A systematic review of the physical and cognitive effects of interactive computer games in older adults. J Appl Gerontol. 2015;34(3):NP166–89. [DOI] [PubMed] [Google Scholar]
- 11.Smith ST, Schoene D. The use of exercise-based videogames for training and rehabilitation of physical function in older adults: current practice and guidelines for future research. Aging Health. 2012;8(3):243–252. [Google Scholar]
- 12.Baert V, Gorus E, Mets T, Geerts C, Bautmans I. Motivators and barriers for physical activity in the oldest old: a systematic review. Ageing Res Rev. 2011;10(4):464–474. [DOI] [PubMed] [Google Scholar]
- 13.Costello E, Kafchinski M, Vrazel J, Sullivan P. Motivators, barriers, and beliefs regarding physical activity in an older adult population. J Geriatr Phys Ther. 2011;34(3):138–147. [DOI] [PubMed] [Google Scholar]
- 14.Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Prev Med. 2004;39(5):1056–1061. [DOI] [PubMed] [Google Scholar]
- 15.Graves LEF, Ridgers ND, Stratton G. The contribution of upper limb and total body movement to adolescents' energy expenditure whilst playing Nintendo Wii. Eur J Appl Physiol. 2008;104(4):617–623. [DOI] [PubMed] [Google Scholar]
- 16.Guderian B, Borreson LA, Sletten LE, et al. The cardiovascular and metabolic responses to Wii Fit video game playing in middle-aged and older adults. J Sports Med Phys Fitness. 2010;50(4):436–442. [PubMed] [Google Scholar]
- 17.Taylor LM, Maddison R, Pfaeffli LA, Rawstorn JC, Gant N, Kerse NM. Activity and energy expenditure in older people playing active video games. Arch Phys Med Rehabil. 2012;93(12):2281–2286. [DOI] [PubMed] [Google Scholar]
- 18.Welk G. Physical Activity Assessments for Health-Related Research. Champaign, IL: Human Kinetics; 2002. [Google Scholar]
- 19.Howe TE, Rochester L, Jackson A, Banks PMH, Balair VA. Exercise for improving balance in older people. Cochrane Database of Syst Rev. 2007;(4):CD004963. [DOI] [PubMed] [Google Scholar]
- 20.Molina KI, Ricci NA, de Moraes SA, Perracini MR. Virtual reality using games for improving physical functioning in older adults: a systematic review. J Neuroengineering Rehabil. 2014;11:156–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JPT, Altman DG, Sterne JA. Assessing risk of bias in included studies. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Vol 5.1.0. 5.1.0 ed: Wiley Online Library; 2011. [Google Scholar]
- 22.Higgins JPT, Deeks JJ, Altman DG. Special topics in statistics. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. Vol 5.1.0. 5.1.0 ed: Wiley Online Library; 2011. [Google Scholar]
- 23.Bieryla KA, Dold NM. Feasibility of Wii Fit training to improve clinical measures of balance in older adults. Clin Interv Aging. 2013;8:775–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cho GH, Hwangbo G, Shin HS. The effects of virtual reality-based balance training on balance of the elderly. J Phys Ther Sci. 2014;26(4):615–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lai CH, Peng CW, Chen YL, Huang CP, Hsiao YL, Chen SC. Effects of interactive video-game based system exercise on the balance of the elderly. Gait Posture. 2013;37(4):511–515. [DOI] [PubMed] [Google Scholar]
- 26.Franco JR, Jacobs K, Inzerillo C, Kluzik J. The effect of the Nintendo Wii Fit and exercise in improving balance and quality of life in community dwelling elders. Technol Health Care. 2012;20(2):95–115. [DOI] [PubMed] [Google Scholar]
- 27.Jorgensen MG, Laessoe U, Hendriksen C, Nielsen OBF, Aagaard P. Efficacy of Nintendo Wii training on mechanical leg muscle function and postural balance in community-dwelling older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2013;68(7):845–852. [DOI] [PubMed] [Google Scholar]
- 28.Laver K, George S, Ratcliffe J, et al. Use of an interactive video gaming program compared with conventional physiotherapy for hospitalised older adults: a feasibility trial. Disabil Rehabil. 2012;34(21):1802–1808. [DOI] [PubMed] [Google Scholar]
- 29.Lee A, Biggan JR, Taylor W, Ray C. The effects of a Nintendo Wii exercise intervention on gait in older adults. Act Adapt Aging. 2014;38(1):53–69. [Google Scholar]
- 30.Maillot P, Perrot A, Hartley A. Effects of interactive physical-activity video-game training on physical and cognitive function in older adults. Psychol Aging. 2012;27(3):589–600. [DOI] [PubMed] [Google Scholar]
- 31.Pichierri G, Murer K, De Bruin ED. A cognitive-motor intervention using a dance video game to enhance foot placement accuracy and gait under dual task conditions in older adults: a randomized controlled trial. BMC Geriatr. 2012;12:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duque G, Boersma D, Loza-Diaz G, et al. Effects of balance training using a virtual-reality system in older fallers. Clin Interv Aging. 2013;8:257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pichierri G, Coppe A, Lorenzetti S, Murer K, de Bruin ED. The effect of a cognitive-motor intervention on voluntary step execution under single and dual task conditions in older adults: a randomized controlled pilot study. Clin Interv Aging. 2012;7:175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pluchino A, Lee SY, Asfour S, Roos BA, Signorile JF. Pilot study comparing changes in postural control after training using a video game balance board program and 2 standard activity-based balance intervention programs. Arch Phys Med Rehabil. 2012;93(7):1138–1146. [DOI] [PubMed] [Google Scholar]
- 35.Ray C, Melton F, Ramirez R, Keller D. The effects of a 15-week exercise intervention on fitness and postural control in older adults. Act Adapt Aging. 2012;36(3):227–241. [Google Scholar]
- 36.Rendon AA, Lohman EB, Thorpe D, Johnson EG, Medina E, Bradley B. The effect of virtual reality gaming on dynamic balance in older adults. Age Ageing. 2012;41(4):549–552. [DOI] [PubMed] [Google Scholar]
- 37.Sato K, Kuroki K, Saiki S, Nagatomi R. Improving walking, muscle strength, and balance in the elderly with an exergame using Kinect: a randomized controlled trial. Games Health J. 2015;4(3):161–167. [DOI] [PubMed] [Google Scholar]
- 38.Schoene D, Lord SR, Delbaere K, Severino C, Davies TA, Smith ST. A randomized controlled pilot study of home-based step training in older people using videogame technology. PLoS One. 2013;8(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Szturm T, Betker AL, Moussavi Z, Desai A, Goodman V. Effects of an interactive computer game exercise regimen on balance impairment in frail community-dwelling older adults: a randomized controlled trial. Phys Ther. 2011;91(10):1449–1462. [DOI] [PubMed] [Google Scholar]
- 40.Toulotte C, Toursel C, Olivier N. Wii Fit® training vs. Adapted Physical Activities: Which one is the most appropriate to improve the balance of independent senior subjects? A randomized controlled study. Clin Rehabil. 2012;26(9):827–835. [DOI] [PubMed] [Google Scholar]
- 41.Podsiadlo D, Richardson S. The Timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. [DOI] [PubMed] [Google Scholar]
- 42.Rose DJ, Jones CJ, Lucchese N. Predicting the probability of falls in community-residing older adults using the 8-foot up-and-go: a new measure of functional mobility. J Aging Phys Act. 2002;10(4):466–475. [Google Scholar]
- 43.Laver K, Ratcliffe J, George S, Burgess L, Crotty M. Is the Nintendo Wii Fit really acceptable to older people? A discrete choice experiment. BMC Geriatr. 2011;11(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85–M94. [DOI] [PubMed] [Google Scholar]
- 45.Rikli RE, Jones J. The Senior Fitness Test. Defining Functional Fitness Parameters. Senior Fitness Test Manual; 2001:11–24.
- 46.Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82(2):128–137. [DOI] [PubMed] [Google Scholar]
- 47.Newton RA. Balance screening of an inner city older adult population. Arch Phys Med Rehabil. 1997;78(6):587–591. [DOI] [PubMed] [Google Scholar]
- 48.Rikli RE, Jones CJ. Functional fitness normative scores for community-residing older adults, ages 60-94. J Aging Phys Act. 1999;7(2):162–181. [Google Scholar]
- 49.Berg K, Wood-Dauphinee S, Williams JI, Gayton D. Measuring balance in the elderly: preliminary development of an instrument. Physiother Can. 1989;41(6):304–311. [Google Scholar]
- 50.Tinetti ME. Performance-orientated assessment of mobility problems in elderly patients. J Am Geriatr Soc. 1986;34(2):119–126. [DOI] [PubMed] [Google Scholar]
- 51.Lajoie Y, Gallagher SP. Predicting falls within the elderly community: comparison of postural sway, reaction time, the Berg Balance Scale and the Activities-specific Balance Confidence (ABC) scale for comparing fallers and non-fallers. Arch Gerontol Geriatr. 2004;38(1):11–26. [DOI] [PubMed] [Google Scholar]
- 52.Martin KA, Sinden AR. Who will stay and who will go? A review of older adults' adherence to randomized controlled trials of exercise. J Aging Phys Act. 2001;9(2):91–114. [Google Scholar]
- 53.Donoghue D, Murphy A, Jennings A, et al. How much change is true change? The minimum detectable change of the Berg Balance Scale in elderly people. J Rehabil Med. 2009;41(5):343–346. [DOI] [PubMed] [Google Scholar]
- 54.Schoene D, Lord SR, Verhoef P, Smith ST. A novel video game-based device for measuring stepping performance and fall risk in older people. Arch Phys Med Rehabil. 2011;92(6):947–953. [DOI] [PubMed] [Google Scholar]


