Background:
Morbidly obese patients with severe osteoarthritis benefit from successful total joint arthroplasty. However, morbid obesity increases the risk of complications. Because of this, some surgeons enforce a body mass index (BMI) eligibility criterion above which total joint arthroplasty is denied. In this study, we investigate the trade-off between avoiding complications and restricting access to care when enforcing BMI-based eligibility criteria for total joint arthroplasty.
Methods:
In this retrospective cohort study, the Veterans Health Administration (VHA) Corporate Data Warehouse (CDW) and Veterans Affairs Surgical Quality Improvement Program (VASQIP) databases were reviewed for patients undergoing total joint arthroplasty from October 2011 through September 2014. We determined, if various BMI eligibility criteria had been enforced over that period of time, how many short-term complications would have been avoided, how many complication-free surgical procedures would have been denied, and the positive predictive value of BMI eligibility criteria as tests for major complications. To provide a frame of reference, we also determined what would have happened if eligibility for total joint arthroplasty were arbitrarily determined by flipping a coin.
Results:
In this study, 27,671 total joint arthroplasties were reviewed. With a BMI criterion of ≥40 kg/m2, 1,148 patients would have been denied a surgical procedure free of major complications, and 83 patients would have avoided a major complication. The positive predictive value of a complication using a BMI of ≥40 kg/m2 as a test for major complications was 6.74% (95% confidence interval [CI], 5.44% to 8.33%). The positive predictive value of a complication using a BMI criterion of 30 kg/m2 was 5.33% (95% CI, 4.99% to 5.71%). Flipping a coin had a positive predictive value of 5.05%.
Conclusions:
A 30 kg/m2 criterion for total joint arthroplasty eligibility is marginally better than flipping a coin and should not determine surgical eligibility. With a BMI criterion of ≥40 kg/m2, the number of patients denied a complication-free surgical procedure is about 14 times larger than those spared a complication. Although the acceptable balance between avoiding complications and providing access to care can be debated, such a quantitative assessment helps to inform decisions regarding the advisability of enforcing a BMI criterion for total joint arthroplasty.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Obesity in the United States has reached epidemic proportions. More than 37% of the American population is now obese and 7.7% is morbidly obese1. Because obesity predisposes patients to osteoarthritis, a growing percentage of patients undergoing total joint arthroplasty are obese2. Patients with a body mass index (BMI) of >40 kg/m2 (morbidly obese) are more than 8 times more likely to have total joint arthroplasty when compared with patients with a normal BMI (BMI < 25 kg/m2)3.
Morbid obesity is a risk factor for complications following total joint arthroplasty4-6. Morbidly obese patients thus assume an elevated risk of the medical, personal, and financial hardships associated with complications following total joint arthroplasty. Surgeons who perform operations on morbidly obese patients also assume responsibility and risk. A decision to operate is a commitment to care for complications. Complications are emotionally draining, require additional time and resources, and can be financially harmful to the surgeon’s practice. The increased risk to the patient and assumed by the surgeon has thus led some surgeons to advocate for a BMI-based eligibility criterion for total joint arthroplasty above which the surgical procedure is delayed or is denied7,8.
However, successful total joint arthroplasty provides improvements in pain and function to morbidly obese patients that are comparable with the improvements experienced by non-morbidly obese patients9-11. BMI-based eligibility criteria are thus controversial as they raise ethical concerns with regard to restricted access to care12. Hence, the use of BMI-based eligibility criteria in total joint arthroplasty practices is highly variable. Some centers in the United Kingdom restrict total joint arthroplasty to patients with a BMI of <30 kg/m2, according to 1 news report13, although many surgeons advocate restricting total joint arthroplasty to patients with a BMI of <40 kg/m2. Others do not restrict access to total joint arthroplasty based solely on BMI, but incorporate that information into an overall risk assessment. However, methods for calculating person-specific risks are underdeveloped14, making it difficult to discuss risks in real terms.
Restricting total joint arthroplasty to patients below a certain BMI should reduce the overall number of complications and the cost of those complications to the health-care system. However, this practice limits patient access to the pain relief and functional improvements of total joint arthroplasty and may increase direct and indirect costs of care associated with advanced hip or knee arthritis. The balance between limiting access and avoiding complications by enforcing a BMI-based eligibility criterion has never been studied or reported, to our knowledge, yet it is essential to establishing such an eligibility criterion in the first place.
In this study, we evaluated what would have happened if a strict BMI-based eligibility criterion were enforced across a large, integrated health-care system. We sought to determine how many patients would have avoided a 30-day perioperative complication or 90-day death following total joint arthroplasty compared with how many patients would have been denied access to a complication-free total joint arthroplasty.
Materials and Methods
This study was approved by our institutional review board. This was a retrospective cohort study of patients with osteoarthritis who underwent primary total joint arthroplasty in the Veterans Health Administration (VHA) health-care system between October 1, 2011, and September 30, 2014. We drew national data from the VHA Corporate Data Warehouse (CDW) and the Veterans Affairs Surgical Quality Improvement Program (VASQIP) databases. The most proximal preoperative height and weight measurements were used to calculate BMI. VASQIP data were used to determine the occurrence of major complications or death. Thirty-day major complications were readmission, reoperation, cardiac arrest, myocardial infarction, coma, cerebrovascular accident, peripheral nerve injury, bleeding requiring >4 units of packed red blood cells, deep vein thrombosis, pulmonary embolism, prosthesis failure, systemic sepsis, failure to wean from the ventilator, pneumonia, reintubation, progressive renal insufficiency, wound dehiscence, organ/space surgical-site infection, and deep infection. In addition, we looked at death within 90 days of the surgical procedure. To understand the effect of obesity class on major complications, we performed logistic regression with age and the Charlson Comorbidity Index as covariates.
We then evaluated what would have happened to these patients if various BMI-based eligibility criteria had been enforced. We determined how many complications would have been avoided and how many patients who would not have experienced a complication would have been denied a surgical procedure. Considering the BMI-based eligibility criterion as a test for postoperative complications, we calculated the positive predictive value of the test at various BMI cutoffs. The positive predictive value is the number of true positives divided by the total number of positives indicated by the test. Similarly, we also determined how many patients who would not have had a complication would have been denied a surgical procedure for every 1 patient who would have avoided a complication because of enforcement of the BMI criterion.
We also determined what would have happened across the health-care system if eligibility for total joint arthroplasty were simply determined by flipping a coin. This arbitrary test was included to serve as a reference with which the various BMI-based eligibility criteria could be compared.
Results
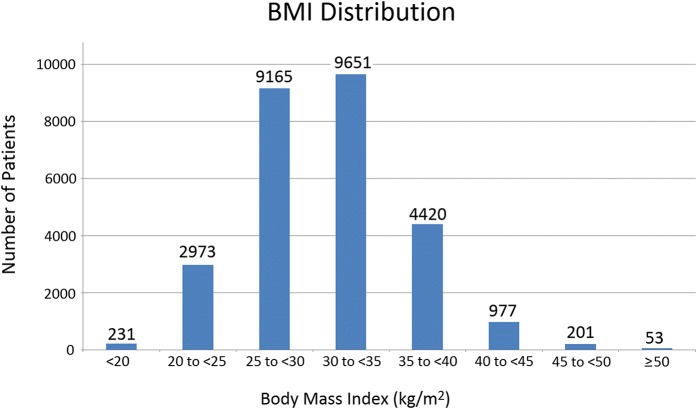
In this study, 27,671 primary total joint arthroplasties were sampled by VASQIP: 67.7% were total knee arthroplasties and 32.3% were total hip arthroplasties; and 93.7% of patients were male, reflecting the demographic characteristics of patients in the VHA. The distribution of BMI categories in this cohort is shown in Figure 1. The mean age, sex distribution, and mean Charlson Comorbidity Index for patients in each BMI category are shown in Table I.
Fig. 1.
A bar graph showing the BMI distribution for the patients in this study.
TABLE I.
Characteristics of Patients in Each BMI Category
| Sex† |
||||
| BMI Class | Age* (yr) | Male | Female | Charlson Comorbidity Index‡ |
| <20 kg/m2 | 63.3 ± 10.2 | 203 | 28 | 1.39 ± 2.02 (0 to 12) |
| 20 to <25 kg/m2 | 65.5 ± 10.1 | 2,793 | 180 | 1.17 ± 1.67 (0 to 13) |
| 25 to <30 kg/m2 | 65.2 ± 9.1 | 8,697 | 468 | 1.02 ± 1.45 (0 to 14) |
| 30 to <35 kg/m2 | 63.8 ± 8.3 | 9,052 | 599 | 1.12 ± 1.49 (0 to 13) |
| 35 to <40 kg/m2 | 62.6 ± 7.7 | 4,092 | 328 | 1.22 ± 1.47 (0 to 11) |
| 40 to <45 kg/m2 | 61.8 ± 7.0 | 862 | 115 | 1.31 ± 1.53 (0 to 13) |
| 45 to <50 kg/m2 | 60.7 ± 6.8 | 173 | 28 | 1.34 ± 1.48 (0 to 6) |
| ≥50 kg/m2 | 59.0 ± 8.0 | 45 | 8 | 1.28 ± 1.51 (0 to 7) |
The values are given as the mean and the standard deviation.
The values are given as the number of patients.
The values are given as the mean and the standard deviation, with the range in parentheses.
The overall major complication rate was 5.05%. Among patients with a BMI of ≥40 kg/m2, the major complication rate was 6.74%. This difference was significant (p = 0.005, chi square test), confirming that morbid obesity was associated with an elevated risk of perioperative complications. In our cohort, the risk of major complications in morbidly obese patients compared with the general patient population (relative risk) was increased by 32%. The absolute increase in risk was 1.6%. Major complications significantly associated with morbid obesity were peripheral nerve injury (absolute risk, 0.41%; p = 0.005), pulmonary embolism (absolute risk, 1.71%; p < 0.0001), and deep surgical-site infection (absolute risk, 0.81%; p = 0.001). The distribution of complications for all patients and for patients with a BMI of ≥40 kg/m2 is shown in Table II.
TABLE II.
Distribution of Complications Among All Patients and Patients with BMI ≥ 40 kg/m2
| Patients* |
|||
| Complications | All (N = 27,671) | With BMI ≥ 40 kg/m2 (N = 1,231) | P Value† |
| General | |||
| Readmission within 14 days postoperatively | 5 (0.02) | 1 (0.08) | Nonsignificant |
| Return to operating room | 575 (2.08) | 34 (2.76) | Nonsignificant |
| Systemic sepsis | 96 (0.35) | 4 (0.32) | Nonsignificant |
| Cardiac | |||
| Cardiac arrest requiring cardiopulmonary resuscitation | 47 (0.17) | 3 (0.24) | Nonsignificant |
| Myocardial infarction | 49 (0.18) | 0 (0.00) | Nonsignificant |
| Neurologic | |||
| Coma lasting >24 hours postoperatively | 2 (0.01) | 0 (0.00) | Nonsignificant |
| Cerebrovascular accident or stroke | 29 (0.10) | 1 (0.08) | Nonsignificant |
| Peripheral nerve injury | 35 (0.13) | 5 (0.41) | 0.005 |
| Vascular | |||
| Bleeding requiring >4 units of packed red blood cells | 34 (0.12) | 0 (0.00) | Nonsignificant |
| Deep vein thrombosis or thrombophlebitis | 196 (0.71) | 7 (0.57) | Nonsignificant |
| Pulmonary | |||
| Failure to wean from ventilator after 48 hours | 38 (0.14) | 0 (0.00) | Nonsignificant |
| Pneumonia | 127 (0.46) | 6 (0.49) | Nonsignificant |
| Pulmonary embolism | 173 (0.63) | 21 (1.71) | <0.0001 |
| Reintubation for respiratory or cardiac failure | 78 (0.28) | 5 (0.41) | Nonsignificant |
| Renal | |||
| Progressive renal insufficiency | 81 (0.29) | 4 (0.32) | Nonsignificant |
| Surgical site | |||
| Wound disruption or dehiscence | 58 (0.21) | 4 (0.32) | Nonsignificant |
| Organ/space surgical-site infection | 56 (0.20) | 3 (0.24) | Nonsignificant |
| Deep-wound surgical-site infection | 86 (0.31) | 10 (0.81) | 0.001 |
| Prosthesis failure | 8 (0.03) | 0 (0.00) | Nonsignificant |
| Death | |||
| Within 90 days of surgery | 113 (0.41) | 6 (0.49) | Nonsignificant |
| All major complications | 1,397 (5.05) | 83 (6.74) | 0.005 |
The values are given as the number of patients, with the percentage in parentheses.
The p value was determined with use of the chi-square test.
Table III shows the odds ratios for major complications for patients in each BMI category (adjusted for age and Charlson Comorbidity Index) referenced to patients with a BMI of 25 to <30 kg/m2. The odds ratio rises continuously across the range of BMI categories. Compared with patients with a BMI of 25 to <30 kg/m2, we found a 37% increased risk (1.6% increased absolute risk) of major complications in patients with a BMI of 40 to <45 kg/m2, a 63% increased risk (2.63% increased absolute risk) in patients with a BMI of 45 to <50 kg/m2, and a 531% increased risk (15.5% increased absolute risk) for patients with a BMI of ≥50 kg/m2.
TABLE III.
Odds Ratios and Absolute Risk for Major Complications for Each BMI Cutoff Adjusting for Age and Charlson Comorbidity Index
| Absolute Risk |
|||
| BMI Class | Odds Ratio* | Adjusted | Unadjusted |
| <20 kg/m2 | 0.82 (0.42 to 1.6) | 3.70% | 3.90% |
| 20 to <25 kg/m2 | 0.97 (0.79 to 1.18) | 4.35% | 4.68% |
| 25 to <30 kg/m2 | 1.00 | 4.50% | 4.71% |
| 30 to <35 kg/m2 | 1.12 (0.98 to 1.28) | 5.00% | 5.12% |
| 35 to <40 kg/m2 | 1.21 (1.03 to 1.43) | 5.40% | 5.43% |
| 40 to <45 kg/m2 | 1.37 (1.03 to 1.82) | 6.07% | 6.04% |
| 45 to <50 kg/m2 | 1.63 (0.94 to 2.84) | 7.13% | 6.97% |
| ≥50 kg/m2 | 5.31 (2.64 to 10.68) | 20.01% | 18.87% |
The values are given as the odds ratio, with the 95% CI in parentheses.
Table IV shows what would have happened to the 27,671 patients who had primary total joint arthroplasty if various strict BMI-based eligibility criteria had been enforced throughout the VHA. We can determine this because all of these patients had a surgical procedure, and individual BMI and complications are available in the medical record. For example, if there had been a system-wide BMI-based eligibility criterion for total joint arthroplasty of ≥40 kg/m2, of the 27,671 surgical procedures, 25,126 cases (90.8%) would have proceeded and would not have had a complication (true negative), 1,314 (4.75%) would have proceeded but would have resulted in a complication (false negative), 1,148 (4.15%) would have been needlessly blocked as there would not have been a complication (false positive), and 83 cases (0.3%) would have been properly blocked from proceeding because they would have resulted in a complication (true positive).
TABLE IV.
Expected Outcome When Setting Various BMI Cutoff Values
| Surgery Allowed* |
Surgery Denied* |
|||||||
| BMI Cutoff | Without Complication | With Complication | Without Complication | With Complication | Percentage of All Complications Avoided | Percentage of All Complication-Free Surgeries Allowed | Positive Predictive Value† | No. of Patients Denied Complication-Free Surgery for Each Complication Avoided |
| 30 kg/m2 | 11,789 (42.60%) | 580 (2.10%) | 14,485 (52.35%) | 817 (2.95%) | 58 | 45 | 5.33% (4.99% to 5.71%) | 18 |
| 35 kg/m2 | 20,946 (75.70%) | 1,074 (3.88%) | 5,328 (19.25%) | 323 (1.17%) | 23 | 80 | 5.72% (5.13% to 6.36%) | 16 |
| 40 kg/m2 | 25,126 (90.80%) | 1,314 (4.75%) | 1,148 (4.15%) | 83 (0.30%) | 6 | 96 | 6.74% (5.44% to 8.33%) | 14 |
| 45 kg/m2 | 26,044 (94.12%) | 1,373 (4.96%) | 230 (0.83%) | 24 (0.09%) | 2 | 99.1 | 9.45% (6.27% to 13.90%) | 10 |
| 50 kg/m2 | 26,231 (94.80%) | 1,387 (5.01%) | 43 (0.16%) | 10 (0.04%) | 0.7 | 99.8 | 18.87% (9.89% to 32.41%) | 4 |
| Coin flip | 13,137 (47.48%) | 698.5 (2.52%) | 13,137 (47.48%) | 698.5 (2.52%) | 50 | 50 | 5.05% | 19 |
The values are given as the number of patients, with the percentage in parentheses.
The values are given as the positive predictive value, with or without the 95% CI in parentheses.
Considering a BMI of ≥40 kg/m2 as a test for postoperative complications, the positive predictive value would have been 6.74% (95% confidence interval [CI], 5.44% to 8.33%). This means that 6.74% of the people testing positive with a BMI of ≥40 kg/m2 would have had a complication. For every 1 patient who would have avoided a complication because of the BMI-based eligibility criterion of ≥40 kg/m2, about 14 patients who would not have had a complication would have been denied access to complication-free total joint arthroplasty.
Table IV also demonstrates that if the BMI-based eligibility criterion is very stringent (low), surgical procedures with complications are reduced, but many more surgical procedures that would not have had a complication are blocked from proceeding. As the BMI-based eligibility criterion for acceptable BMI becomes more lax (that is, the BMI cutoff rises), major complications rise, but many more people end up having a successful surgical procedure without a complication. The positive predictive value of the BMI criterion test for complications rises with an increasing value of BMI. With a BMI-based eligibility criterion of 50 kg/m2, the positive predictive value of the test for major complications improves to 18.9% (95% CI, 9.89% to 32.41%). In this case, only about 4 patients are denied a complication-free surgical procedure for every 1 patient who avoids a complication.
Finally, at the bottom of Table IV, one can see what would have happened if eligibility for total joint arthroplasty had been arbitrarily determined by flipping a coin. The total number of cases that had a complication (1,397 cases) is evenly distributed between proceeding to the surgical procedure or being denied the surgical procedure (698.5 cases in each group). Similarly, the total number of cases that did not have a complication (26,274 cases) is evenly distributed between proceeding to the surgical procedure or being denied a surgical procedure (13,137 in each group). Such an arbitrary test would have had a positive predictive value of 5.05% (the overall complication rate). If surgical eligibility had been determined with a coin flip, about 19 patients would have been denied a complication-free surgical procedure for every 1 patient who avoided a complication. As can be seen in Table IV, a BMI-based eligibility criterion of 30 kg/m2 has nearly the same performance as a coin flip in identifying patients who would have had a complication with total joint arthroplasty. The positive predictive value using a BMI eligibility criterion of 30 kg/m2 is 5.33% (95% CI, 4.99% to 5.71%), and the number of patients denied a surgical procedure for every complication avoided is 18.
Discussion
Prior studies have shown that patients with high BMI are at increased risk of having complications following total joint arthroplasty4-6. It is therefore no surprise that we found this to be true within the VHA. Although it may thus seem prudent to restrict access to total joint arthroplasty to patients below a BMI threshold, our analysis reveals the unintended consequence of enforcing a strict system-wide BMI-based eligibility criterion for total joint arthroplasty. On a population level, such a policy would reduce the overall number of complications, but would also result in denying total joint arthroplasty access to a much larger number of patients who would not have had a complication. We have quantified this effect for the largest integrated health-care system in the United States.
This study did have important limitations. The most important limitation is that VASQIP tracks complications over 30 days following the surgical procedure and death over 90 days following the surgical procedure. Late failure such as loosening, instability, and late infection may be related to morbid obesity, but was not accounted for in this study. Several studies have compared the longer-term survivorship of total joint arthroplasty in morbidly obese and non-morbidly obese patients, and the findings have been mixed. Issa et al.15 (105 morbidly obese patients undergoing total knee arthroplasties), at a mean follow-up of 52 months, and Bordini et al.16 (172 morbidly obese patients undergoing total knee arthroplasties), at a mean follow-up of 5 years, did not find an effect of morbid obesity on total knee arthroplasty survivorship. In the largest study of which we are aware on total knee arthroplasty survival as a function of obesity class published to date, Zingg et al. found no significant effect of obesity on survival at 5 years, but a more than twofold increase in revision for any reason in patients with a BMI of ≥35 kg/m2 at 10 years17. The 10-year implant survivorship was approximately 97% for patients with a BMI of <35 kg/m2 compared with approximately 93% in patients with a BMI of ≥35 kg/m2. In patients undergoing total hip arthroplasty, including 206 patients who were morbidly obese, McCalden et al. were unable to find a significant difference in implant survivorship between patients in all weight categories, including morbidly obese patients, in a survivorship analysis that spanned 15 years18. In contrast, Chee et al. compared 55 morbidly obese patients with 53 non-obese patients and found that 5-year survivorship in morbidly obese patients (90%) was worse than in non-obese patients (100%)19. However, these patients all had fully cemented total hip arthroplasties. An additional study with longer follow-up would be needed to accurately determine the effects of late failure on the advisability of establishing a strict BMI eligibility criterion for total joint arthroplasty. This was beyond the capabilities of our current data set.
Additional limitations included that this study was conducted on health data from the VHA. Patients in this system are overwhelmingly male and have a different distribution of comorbidities than general patients. We looked at the effect of sex on our results and found that male patients were slightly more likely to have a major complication than female patients (odds ratio, 1.34 [95% CI, 1.03 to 1.75]), but there were too few patients in the highest BMI categories to conclude anything regarding whether there was a difference based on sex at the highest BMI categories.
Furthermore, it is important to note that, as in the general community, the various VHA surgeons and facilities may or may not have been enforcing various BMI-based eligibility criteria for surgery. It is thus likely that the true number of potentially operable morbidly obese patients in the VHA system over the studied time period was actually higher than the number presented here. However, the calculated positive predictive value of morbid obesity as a test for complications should be unaffected. This calculation depends on the ratio between complicated and uncomplicated surgical procedures in patients with BMI above the criterion of interest. If more surgeons had chosen to operate on morbidly obese patients who were otherwise acceptable for a surgical procedure, the actual numbers would have gone up, but the ratio should have remained constant.
Finally, it is very important for the reader to recognize that the morbidly obese patients who ended up having a surgical procedure in this cohort were considered to be otherwise acceptable surgical candidates by the surgeons who chose to operate. Presumably these morbidly obese patients who had a total joint arthroplasty did not have many of the comorbidities that are commonly associated with morbid obesity. We are not comparing the application of a strict criterion to indiscriminately operating on everyone with a high BMI. Rather, we are comparing application of a strict criterion to the current practice in the VHA system, which includes highly variable selection criteria. In this retrospective analysis, there were no uniform criteria used to establish suitability for a surgical procedure. We cannot estimate how many morbidly obese patients were denied a surgical procedure because of a strict BMI criterion or how many morbidly obese patients were denied a surgical procedure in this time period because of a comprehensive assessment of their overall health.
In this study, we investigated what would have happened if the VHA had uniformly enforced various BMI-based eligibility criteria for total joint arthroplasty, and we compared the results with those of the current practice. We found that a very strict BMI criterion for total joint arthroplasty eligibility, such as a BMI of 30 kg/m2, would have been marginally more effective than flipping a coin in identifying patients who were destined to have a complication following a surgical procedure. Such an overly stringent test, which has been applied in some centers in the United Kingdom, would have had the effect of arbitrarily rationing care. Such a practice should not be used to determine whether someone is eligible for total joint arthroplasty.
If the VHA health-care system had uniformly adopted the commonly advocated BMI eligibility criterion of ≥40 kg/m2, such a policy would have resulted in approximately 14 morbidly obese patients being denied an uncomplicated surgical procedure for every 1 patient who would have avoided a complication following the surgical procedure. Is this balance acceptable? Some patients may conclude that a health-care system that applies a blanket criterion with this ratio is overrestricting access to care and is not allowing enough autonomy to individual patients to determine their personal tolerance to risk. However, some surgeons may consider this to be an acceptable trade-off, particularly if they do not have a suitable practice setting, level of support, or degree of comfort in exposing patients to elevated risks and handling complications. For the health-care system, setting a hard BMI cutoff for surgical eligibility is an economic decision, and it is unclear whether this ratio is acceptable or not. Total joint arthroplasty has been shown to be highly cost-effective, even in higher-risk patients20, as the quality-adjusted life-years gained and the savings from no longer having to support the disability and medical costs associated with advanced arthritis offset the expenditures associated with the operation and its aftercare20,21. At some point, as patients become even higher risk, operating may no longer be cost-effective. Ultimately, given our current level of understanding, we believe that it is unreasonable to interfere with the patient and physician relationship by administratively setting rigid surgical eligibility standards for joint replacement as they can have broad and poorly understood consequences. Further research that accounts for both the advantages and disadvantages of enforcing a BMI eligibility criterion for joint replacement is needed to determine whether any cutoff level of risk can be identified and supported.
Footnotes
Written work prepared by employees of the Federal Government as part of their official duties is, under the United States Copyright Act, a ‘work of the United States Government’ for which copyright protection under that Act is not available. As such, copyright protection does not extend to the contributions of employees of the Federal Government prepared as part of their employment.
A commentary by James A. Shaw, MD, is linked to the online version of this article at jbjs.org.
Investigation performed at the VA Palo Alto Health Care System, Palo Alto, California
Disclosure: Three authors of this study (S.G., T.B., and A.H.S.H.) received grants from the Department of Veterans Affairs Health Services Research and Development Merit Review (grant numbers IIR 13-051-3 and RCS-14-232); funds were used to pay for salary support. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/E560).
Disclaimer: The opinions and views expressed are of the authors and not necessarily of the Department of Veterans Affairs, the United States Government, or Stanford University.
References
- 1.Flegal KM, Kruszon-Moran D, Carroll MD, Fryar CD, Ogden CL. Trends in obesity among adults in the United States, 2005 to 2014. JAMA. 2016. June 7;315(21):2284-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012. September 26;308(12):1227-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bourne R, Mukhi S, Zhu N, Keresteci M, Marin M. Role of obesity on the risk for total hip or knee arthroplasty. Clin Orthop Relat Res. 2007. December;465:185-8. [DOI] [PubMed] [Google Scholar]
- 4.D’Apuzzo MR, Novicoff WM, Browne JA. The John Insall Award: morbid obesity independently impacts complications, mortality, and resource use after TKA. Clin Orthop Relat Res. 2015. January;473(1):57-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ward DT, Metz LN, Horst PK, Kim HT, Kuo AC. Complications of morbid obesity in total joint arthroplasty: risk stratification based on BMI. J Arthroplasty. 2015. September;30(9)Suppl:42-6. Epub 2015 Jun 3. [DOI] [PubMed] [Google Scholar]
- 6.Wagner ER, Kamath AF, Fruth KM, Harmsen WS, Berry DJ. Effect of body mass index on complications and reoperations after total hip arthroplasty. J Bone Joint Surg Am. 2016. February 3;98(3):169-79. [DOI] [PubMed] [Google Scholar]
- 7.McElroy MJ, Pivec R, Issa K, Harwin SF, Mont MA. The effects of obesity and morbid obesity on outcomes in TKA. J Knee Surg. 2013. April;26(2):83-8. Epub 2013 Mar 11. [DOI] [PubMed] [Google Scholar]
- 8.Workgroup of the American Association of Hip and Knee Surgeons Evidence Based Committee. Obesity and total joint arthroplasty: a literature based review. J Arthroplasty. 2013. May;28(5):714-21. Epub 2013 Mar 19. [DOI] [PubMed] [Google Scholar]
- 9.Baker P, Petheram T, Jameson S, Reed M, Gregg P, Deehan D. The association between body mass index and the outcomes of total knee arthroplasty. J Bone Joint Surg Am. 2012. August 15;94(16):1501-8. [DOI] [PubMed] [Google Scholar]
- 10.Jameson SS, Mason JM, Baker PN, Elson DW, Deehan DJ, Reed MR. The impact of body mass index on patient reported outcome measures (PROMs) and complications following primary hip arthroplasty. J Arthroplasty. 2014. October;29(10):1889-98. Epub 2014 Jun 2. [DOI] [PubMed] [Google Scholar]
- 11.Judge A, Batra RN, Thomas GE, Beard D, Javaid MK, Murray DW, Dieppe PA, Dreinhoefer KE, Peter-Guenther K, Field R, Cooper C, Arden NK. Body mass index is not a clinically meaningful predictor of patient reported outcomes of primary hip replacement surgery: prospective cohort study. Osteoarthritis Cartilage. 2014. March;22(3):431-9. Epub 2014 Jan 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis W, Porteous M. Joint replacement in the overweight patient: a logical approach or new form of rationing? Ann R Coll Surg Engl. 2007. April;89(3):203-6; discussion 203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.BBC News. Obese patients denied surgery in a third of areas in England. 2016. April 22 http://www.bbc.com/news/health-36101302. Accessed 2017 Sep 29.
- 14.Manning DW, Edelstein AI, Alvi HM. Risk prediction tools for hip and knee arthroplasty. J Am Acad Orthop Surg. 2016. January;24(1):19-27. [DOI] [PubMed] [Google Scholar]
- 15.Issa K, McElroy MJ, Pourtaheri S, Patel S, Jauregui J, Mont MA. Outcomes of primary total knee arthroplasty in the morbidly obese patients. J Long Term Eff Med Implants. 2013;23(4):301-7. [DOI] [PubMed] [Google Scholar]
- 16.Bordini B, Stea S, Cremonini S, Viceconti M, De Palma R, Toni A. Relationship between obesity and early failure of total knee prostheses. BMC Musculoskelet Disord. 2009. March 5;10:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zingg M, Miozzari HH, Fritschy D, Hoffmeyer P, Lübbeke A. Influence of body mass index on revision rates after primary total knee arthroplasty. Int Orthop. 2016. April;40(4):723-9. Epub 2015 Nov 12. [DOI] [PubMed] [Google Scholar]
- 18.McCalden RW, Charron KD, MacDonald SJ, Bourne RB, Naudie DD. Does morbid obesity affect the outcome of total hip replacement? An analysis of 3290 THRs. J Bone Joint Surg Br. 2011. March;93(3):321-5. [DOI] [PubMed] [Google Scholar]
- 19.Chee YH, Teoh KH, Sabnis BM, Ballantyne JA, Brenkel IJ. Total hip replacement in morbidly obese patients with osteoarthritis: results of a prospectively matched study. J Bone Joint Surg Br. 2010. August;92(8):1066-71. [DOI] [PubMed] [Google Scholar]
- 20.Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, Holt HL, Solomon DH, Yelin E, Paltiel AD, Katz JN. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009. June 22;169(12):1113-21; discussion 1121–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996. March 20;275(11):858-65. [PubMed] [Google Scholar]