Abstract
Objective
This study compared trends in racial-ethnic disparities in mental health care access among whites, blacks, Hispanics, and Asians by using the Institute of Medicine definition of disparities as all differences except those due to clinical appropriateness, clinical need, and patient preferences.
Methods
Racial-ethnic disparities in mental health care access were examined by using data from a nationally representative sample of 214,597 adults from the 2004–2012 Medical Expenditure Panel Surveys. The main outcome measures included three mental health care access measures (use of any mental health care, any outpatient care, and any psychotropic medication in the past year).
Results
Significant disparities were found in 2004-05 and in 2011-12 for all three racial-ethnic minority groups compared with whites in all three measures of access. Between 2004 and 2012, black-white disparities in any mental health care and any psychotropic medication use increased, respectively, from 8.2% to 10.8% and from 7.6% to 10.0%. Similarly, Hispanic-white disparities in any mental health care and any psychotropic medication use increased, respectively, from 7.9% to 10.2% and 6.7% to 9.4%.
Conclusions
No reductions in racial-ethnic disparities in access to mental health care were identified between 2004 and 2012. For blacks and Hispanics, disparities were exacerbated over this period. Clinical interventions that improve identification of symptoms of mental illness, expansion of health insurance, and other policy interventions that remove financial barriers to access may help to reduce these disparities.
Keywords: Disparities, mental health, access to care, Research/service delivery, Utilization patterns and review, Ethnic groups
In 2003, the Institute of Medicine (IOM) published Unequal Treatment, which served to elevate racial-ethnic health care disparities to the forefront of clinical and policy attention (1). Eliminating health care disparities was also cited as one of the overarching goals of Healthy People 2010 and 2020 (2,3). Despite these efforts, disparities in mental health care remain wider than in most other areas of health care services (4), and mental illness remains as one of the highest health burdens for minority populations (5). Previous studies of trends found that although overall rates of mental health treatment increased, gaps in access to mental health treatment between blacks, Latinos, and non-Latino whites (hereafter referred to as whites) were sustained (6,7). In addition, Hispanic-white and black-white disparities were exacerbated in access to mental health care (8). However, information regarding trends in mental health disparities beyond 2006 is limited. Updating our knowledge of trends in these disparities—and including Asian-white disparities—is critical for understanding whether efforts to decrease disparities have been fruitful. Such an update also provides a baseline for future studies evaluating the impact of the Affordable Care Act (ACA) on reducing these disparities.
Since 2004, there have been significant shifts in the magnitude of expenditures and sources of payment for inpatient, outpatient, and medication therapies for mental illness in the United States. Growth in mental health care spending by private payers decelerated significantly in 2007–2009 compared with 2004–2006; state and local mental health care spending showed negative growth while federal mental health care spending accelerated (9). During this time, major psychiatric medications, such as sertraline, risperidone, and quetiapine, came off patent (2006, 2007, and 2011, respectively) and prices decreased. Access to less expensive medications is one explanation for growth in psychotropic medication use in the overall U.S. population (10). The impact of these overall trends on disparities in psychotropic medication use is unclear.
In the scant literature evaluating Asian-white mental health care disparities, Asian Americans demonstrate lower rates of any type of mental health-related service use than the general population (11) and are less likely than whites to report being assessed, counseled, and recommended medications by specialty care providers (12,13). To our knowledge, no studies have tracked Asian-white mental health care disparities over time.
In this study, we analyzed trends in disparities in access to mental health care between 2004 and 2012, comparing whites with blacks, Hispanics, and Asians. We used methods that implement the IOM definition of racial-ethnic health care disparity, which defines disparities as differences between racial-ethnic minority groups and whites that are attributable to socioeconomic factors and insurance but not to clinical need and treatment preferences (8).
Methods
Data
Data are from a nationally representative sample of noninstitutionalized U.S. civilians, including blacks, Hispanics, Asians, and non-Hispanic whites ages 18 and over from the 2004–2012 Medical Expenditure Panel Survey (MEPS) (N=214,597). In multivariate models, we assessed trends across two periods (2004–2005 and 2011–2012), combining two years at the beginning and end to increase sample size and the robustness of these results. We estimated trends in three measures of access to mental health services in the past year: having any mental health care, any outpatient mental health care, and any psychotropic medication. Mental health events include treatment provided by a mental health care specialist (psychiatrist, psychologist, counselor, or social worker) or primary care provider for a disorder covered by ICD-9 codes 291, 292, or 295–314 (14) (a range that covers both substance use disorders and mental disorders); fills of prescribed medicine linked with one of these ICD-9 codes; or fills of prescribed medicine considered to be a psychotropic drug according to the Multum drug classification system (15). This methodology has been shown to have strong sensitivity (88%) to provider reports of treatment of behavioral health disorders (16).
As in previous studies (8,17,18), independent variables were grouped into those related to clinical need (adjusted for in the disparity predictions and considered to be “allowable differences”) and non-need variables (not adjusted for in the predictions and considered to be “unallowable differences”). Need variables included the Kessler-6 scale of psychological distress (19) and the two-item Patient Health Questionnaire (20), self-reported mental health status (excellent, very good, good, fair, or poor), and the score on the mental health component of the 12-item Short Form Health Survey (SF-12) health status instrument (21). Other need variables were the physical health component of the SF-12, gender, age, and reporting any functional limitation in working at a job, doing housework, or going to school; these were adjusted for in the estimation because they were considered to be allowable differences highly correlated with mental illness (22,23). Non-need variables were education level, income level, region of the country, and insurance coverage.
Applying the IOM Definition of Disparity
As defined by the IOM in Unequal Treatment and implemented in prior studies (18,24–26), disparities in care are differences observed for racial-ethnic minority groups that are not due to differences in clinical appropriateness, clinical need, or patient preferences. That is, if racial-ethnic minority groups have lower rates of mental illness and thus receive less care, then the health care system should not be held accountable for this part of the racial-ethnic difference in treatment. Differences due to socioeconomic factors, however, contribute to the disparity and should be considered as unallowable differences, reflecting a view that differences in care due to socioeconomic factors, such as income, education, and employment, are unjustifiable and that health systems should be accountable for such differences. Unfortunately, the MEPS data set does not contain measures of fully informed preferences for mental health care, and thus there is no adjustment for patient preferences.
Implementing the IOM definition of disparity calls for a three-step process that includes model estimation, transformation of the distributions of clinical appropriateness and need to be equivalent across racial-ethnic groups, and outcome prediction.
Model Estimation
In the first step, a logistic regression model of any mental health service use in the past year (or any psychotropic medication or outpatient mental health service use) was estimated, adjusting for the main effects of race-ethnicity and time (indicators of 2004–2005 and 2011–2012) as well as race × time interaction terms and need and non-need variables (as defined above).
Adjustment for Mental Health Status and Disparity Prediction
To adjust for allowable differences, we applied the rank-and-replace method to an index of need variables in the model (described in more detail elsewhere [18,24]). This index was created by fitting a model of mental health care utilization and summing the products of the mental health status variables’ parameter estimates and values. This is similar to a model-based prediction, except socioeconomic characteristics, race-ethnicity variables, and the constant were excluded from the prediction. Blacks, Hispanics, Asians, and whites were then ranked according to their index scores, and the values of black, Hispanic, and Asian individuals were adjusted to equal the equivalently ranked white individuals.
In the final step, predicted service use for each racial-ethnic group and time period were calculated by using the sum of the products of the coefficients from the original model and the adjusted need values and then transforming the result back to the percentage-point scale. Disparities were then calculated by subtracting predictions for whites from those for racial-ethnic minority groups for each of the dependent variables within each time period, and trends were evaluated by comparing these disparities across the two periods.
Variance Estimation
We estimated variances for all analyses, accounting for the complex study design, nonresponse rates of the MEPS, and standardized stratum and primary sampling unit variables across pooled years (27). Variance estimates for disparity trend comparisons were calculated by using the balanced repeated-replication procedure. This method of measuring standard errors repeats the estimation process used for the full sample with a set of subsamples of the population, each of which is half of the full sample size (28). All analyses were conducted with Stata, version 13 (29).
Results
Significant differences in trends were identified in some but not all explanatory variables between 2004–2005 and 2011–2012 (Table 1). Compared with trends for whites, trends for blacks showed slightly improved mental health status, Asian education levels generally decreased, and marriage rates among Hispanics decreased. Unadjusted rates of access to any mental health care showed that white respondents consistently reported higher rates of access than any other racial-ethnic group in each year from 2004 to 2012 (Figure 1). Rates of access for whites increased from 16% in 2004 to 20% in 2012, rates for Asians increased slightly from 3% to 5%, and rates for blacks and Hispanics increased from 7% to 10% and from 8% to 9%, respectively.
TABLE 1.
Past-year use of mental health care reported in 2004–2005 and 2011–2012, by racial-ethnic groupa
| Variable | White | Black | Hispanic | Asian | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 2004–2005 | 2011–2012 | 2004–2005 | 2011–2012 | 2004–2005 | 2011–2012 | 2004–2005 | 2011–2012 | |
| (N=25,864) | (N=22,938) | (N=7,006) | (N=10,614) | (N=11,440) | (N=14,388) | (N=2,125) | (N=4,177) | |
| Any mental health care (%) | 16.3 | 19.5 | 7.7 | 9.2 | 7.9 | 8.7* | 3.7 | 4.9* |
| Age (%) | ||||||||
| 18–24 | 11.4 | 11.0 | 15.5 | 15.8 | 18.6 | 18.0 | 12.0 | 11.7 |
| 25–34 | 15.8 | 15.3 | 19.7 | 18.7 | 26.3 | 24.3 | 24.0 | 22.7 |
| 35–44 | 18.4 | 15.3 | 21.2 | 17.4 | 23.1 | 21.5 | 22.2 | 21.2 |
| 45–54 | 19.8 | 18.8 | 19.3 | 19.3 | 15.2 | 16.8* | 17.4 | 18.0 |
| 55–64 | 15.5 | 18.0 | 12.1 | 15.1 | 8.7 | 10.4 | 12.4 | 13.4 |
| 65–74 | 9.7 | 11.9 | 7.0 | 8.2 | 5.0 | 5.4* | 7.2 | 8.1 |
| ≥75 | 9.3 | 9.7 | 5.1 | 5.5 | 3.3 | 3.6 | 4.9 | 5.0 |
| Female (%) | 51.8 | 51.6 | 55.0 | 55.0 | 48.6 | 49.9 | 52.1 | 54.0 |
| Married (%) | 58.7 | 56.7 | 35.2 | 32.8 | 53.7 | 47.2* | 64.6 | 61.1 |
| Mental health status (%) | ||||||||
| Excellent | 37.5 | 35.4 | 36.5 | 38.9* | 35.2 | 36.3 | 42.3 | 42.8 |
| Very good | 32.0 | 31.7 | 27.9 | 27.2 | 30.5 | 30.7 | 30.2 | 30.1 |
| Good | 23.4 | 25.0 | 26.8 | 25.1* | 27.6 | 26.0 | 23.1 | 22.7 |
| Fair | 5.6 | 6.4 | 7.0 | 7.1 | 5.4 | 6.0 | 3.6 | 3.7 |
| Poor | 1.6 | 1.5 | 1.8 | 1.7 | 1.3 | 1.0 | .9 | .8 |
| Any limitation of activity (%) | 29.7 | 29.6 | 27.4 | 25.8 | 18.1 | 16.4 | 15.3 | 13.9 |
| SF-12 (M±SE score)b | ||||||||
| Mental component summary | 50.9±.1 | 50.9±.1 | 50.4±.2 | 51.2±.2* | 50.3±.2 | 50.7±.1 | 51.8±.4 | 52.4±.2 |
| Physical component summary | 49.5±.1 | 49±.1 | 48.5±.2 | 48.2±.2 | 50.8±.2 | 50.5±.2 | 51.5±.3 | 50.8±.3 |
| Kessler-6 (M±SE score)c | 3.5±0 | 3.5±.1 | 3.6±.1 | 3.4±.1 | 3.8±.1 | 3.4±.1 | 3.2±.1 | 2.8±.1 |
| PHQ-2 (M±SE score)d | .7±.01 | .7±.01 | .8±.03 | .8±.02 | .8±.02 | .7±.02 | .7±.05 | .6±.03 |
| Insurance status (%) | ||||||||
| Private | 77 | 72.5 | 58.8 | 53.0 | 46.6 | 43.5 | 71.4 | 67.9 |
| Medicaid | 6.5 | 7.6 | 19.4 | 22.6 | 16.1 | 18.2 | 11.9 | 12.3 |
| Medicare | 21.0 | 24.2 | 15.9 | 17.6 | 9.6 | 10.5 | 12.5 | 13.5 |
| Uninsured | 9.7 | 10.0 | 17.4 | 17.9 | 34.6 | 34.3 | 13.1 | 15.2 |
| Income (% of federal poverty level) (%) | ||||||||
| <100 | 8.0 | 9.2 | 20.8 | 22.9 | 17.7 | 20.2 | 7.1 | 11.1 |
| 100–125 | 3.0 | 3.7 | 5.9 | 6.6 | 7.7 | 7.2 | 3.0 | 4.0 |
| 126–200 | 11.1 | 11.6 | 17.6 | 16.5 | 21.2 | 21.8 | 12.3 | 12.4 |
| 201–400 | 30.9 | 30.4 | 31.6 | 30.2 | 32.9 | 30.9 | 31.7 | 27.1 |
| >400 | 47.0 | 45.1 | 24.1 | 23.8 | 20.4 | 19.9 | 45.9 | 45.4 |
| Education (%) | ||||||||
| Less than high school graduate | 14.4 | 33.6 | 24.6 | 40.2 | 45.8 | 52.0 | 15.1 | 37.1* |
| High school graduate | 32.7 | 20.8 | 35.5 | 24.3 | 27.7 | 21.6* | 21.5 | 14.1* |
| Some college | 24.1 | 19.9 | 24.4 | 20.7 | 15.8 | 15.6* | 19.2 | 14.8 |
| College graduate | 28.8 | 25.7 | 15.6 | 14.9 | 10.8 | 10.7* | 44.2 | 34.0* |
| Region (%) | ||||||||
| Northeast | 20.0 | 19.4 | 17.0 | 16.5 | 14.6 | 14.5 | 20.7 | 20.2 |
| Midwest | 26.4 | 25.7 | 18.0 | 17.4 | 8.0 | 8.3 | 10.4 | 11.8 |
| South | 33.8 | 35.2 | 55.9 | 57.4 | 36.1 | 36.4 | 19.5 | 21.1 |
| West | 19.7 | 19.7 | 9.1 | 8.8 | 41.4 | 40.8 | 49.4 | 47.0 |
| Employed (%) | 67.4 | 64.3 | 64.7 | 59.1 | 67.2 | 64.1 | 68.0 | 65.4 |
Based on data from the Medical Panel Expenditure Survey. Calculations were weighted to be representative of the entire U.S. population over age 18.
12-item Short Form Health Survey. Possible scores on the components range from 0 to 100, with higher scores indicating better health.
Possible scores range from 0–24, with higher scores indicating greater psychological distress.
Two-item Patient Health Questionnaire. Possible scores range from 0 to 6, with higher scores indicating more depressive symptoms.
p<.05 for the comparison of the difference in absolute percentage-point trends between the racial-ethnic minority group and whites
Figure 1. Unadjusted trends in any mental health care by race/ethnicity 2004-2012a, b, c.
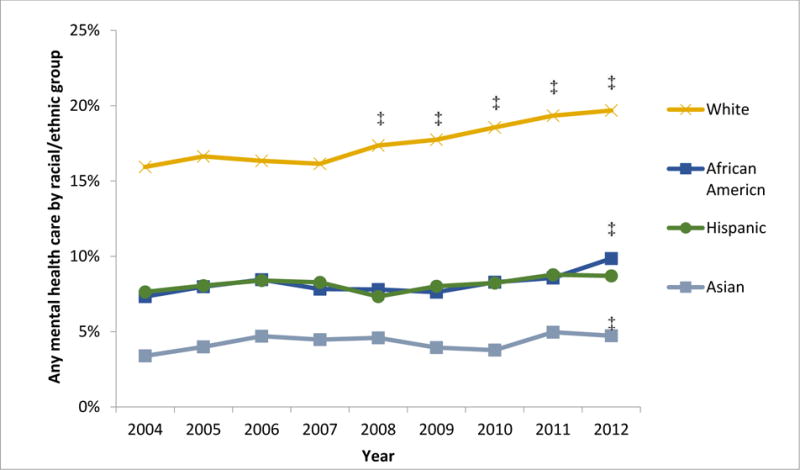
aData: 2004-2012 Medical Expenditure Panel Surveys
bN= 214, 597
cAll differences between whites and blacks, Hispanics, and Asians are significant (p<.05)
‡Any mental health care of black/Hispanic/Asian and whites in the marked year is significantly different from the same group’s values in 2004
Table 2 presents our main disparity predictions. [Regression model output is presented in an online supplement to this article.] After adjustment for clinical need, significant disparities were noted among all three racial-ethnic minority groups (black, Hispanic, and Asian) compared with whites in all three measures of access to mental health care in the periods 2004–2005 and 2011–2012. Assessing differences in disparities over time, between 2004–2005 and 2011–2012, black-white disparities in any mental health care and any psychotropic medication use increased, respectively, from 8.2% to 10.8% and from 7.6% to 10.0%. Similarly, Hispanic-white disparities in any mental health care and any psychotropic medication use increased, respectively, from 8.4% to 10.9% and 7.3% to 10.3%. These exacerbations of disparities over time were statistically significant in both absolute and relative terms. No significant trends in black-white or Hispanic-white disparities in any outpatient mental health service use were identified, nor was there a significant change in Asian-white disparities in the three measures of access to mental health care. These trends in adjusted disparities were similar when all years of data between 2004 and 2012—as opposed to just the end points—were used (results available on request).
TABLE 2.
Trends in disparities in past-year use of mental health care reported in 2004–2005 and 2011–2012, by racial-ethnic groupa
| Variable | White | Black | Hispanic | Asian | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| % | SEb | % | SEb | Disparity | SEb | % | SEb | Disparity | SEb | % | SEb | Disparity | SEb | |
| Any mental health care | ||||||||||||||
| 2004–2005 | 16.3 | .004 | 8.0 | .007 | −8.2 | .009 | 7.9 | .006 | −8.4 | .006 | 5.7 | .01 | −10.6 | .01 |
| 2011–2012 | 19.2 | .007 | 8.4 | .01 | −10.8 | .01 | 8.3 | .009 | −10.94 | .01 | 8.9 | .02 | −10.4 | .02 |
| Difference between years | 3.0* | .008 | .4 | .009 | .4 | .009 | 3.1 | .02 | ||||||
| Difference in disparities | −2.6* | .01 | −2.6* | .01 | .2 | .02 | ||||||||
| Outpatient care | ||||||||||||||
| 2004–2005 | 8.8 | .003 | 5.2 | .006 | −3.6 | .007 | 4.7 | .004 | −4.1 | .005 | 4.1 | .009 | −4.8 | .009 |
| 2011–2012 | 9.4 | .006 | 4.5 | .006 | −4.8 | .008 | 4.7 | .007 | −4.6 | .009 | 5.2 | .01 | −4.2 | .02 |
| Difference between years | .6 | .006 | −.6 | .006 | 0 | .007 | 1.2 | .01 | ||||||
| Difference in disparities | −1.2 | .008 | −.6 | .009 | .6 | .02 | ||||||||
| Prescription medication | ||||||||||||||
| 2004–2005 | 13.8 | .003 | 6.2 | .006 | −7.6 | .008 | 6.5 | .006 | −7.3 | .006 | 3.5 | .009 | −10.3 | .009 |
| 2011–2012 | 17.1 | .007 | 7.1 | .009 | −10.0 | .01 | 6.8 | .009 | −10.3 | .01 | 7.4 | .02 | −9.7 | .02 |
| Difference between years | 3.3* | .008 | .9 | .008 | .3 | .009 | 4.0* | .02 | ||||||
| Difference in disparities | −2.4* | .01 | −3.0* | .01 | .7 | .02 | ||||||||
Source: 2004–2005 and 2011–2012 Medical Expenditure Panel Survey. Implementation of the Institute of Medicine definition of disparity requires adjustment for clinical need and allows for mediation of racial-ethnic disparities through socioeconomic status factors. Clinical need variables are self-reported mental health status, physical and mental health components of the 12-item Short-Form Health Survey, the Kessler-6, the two-item Patient Health Questionnaire, age, sex, marital status, and limitation of activity.
Standard errors were calculated by using balanced repeated-replication methodology.
p<.05
Discussion
Little progress was made in reducing disparities in access to mental health care for blacks, Hispanics, and Asians compared with whites between 2004 and 2012. This was true for access to any type of mental health care, outpatient mental health visits, and psychotropic medication use, even after adjustment for racial-ethnic differences in clinical need. In the case of blacks and Hispanics, disparities in rates of access to any mental health care and any psychotropic medication were exacerbated over this period in absolute and relative terms. Asians had persistently lower rates of access to care across this period.
The widening disparities in any mental health care among blacks and Latinos were predominantly driven by significant increases in psychotropic medication use among whites but not among blacks and Latinos. Only small increases in outpatient mental health care were noted among whites. Changes in ED and inpatient use for psychiatric diagnoses represented only a small percentage of total mental health services (less than 1% of the study population used these services). Our findings are consistent with analyses of national trends showing that use of prescription drugs, as well as antidepressants, increased broadly in the United States from 1999 to 2012 (30). That blacks and Latinos did not participate in this increasing trend in psychotropic medication use may be due in part to the persistently higher uninsured rates among blacks (19% in 2012) and especially Hispanics (29%), compared with whites (11%) (31).
Continued access disparities are of high clinical and public health significance given that persons from racial-ethnic minority groups, although generally having similar levels of mental illness prevalence as whites (32), have greater persistence (33) and severity of mental illness (34), and because reducing racial-ethnic disparities in access to mental health care has been shown to lead to savings in expenditures for acute medical care (35). The findings are similar to results from previous trends studies, which used data ending in 2004, that showed little progress toward reducing mental health care disparities for racial-ethnic minority groups (7,8,36). This suggests that calls to reduce mental health care disparities have not been successful (1,37–39). These findings come at a time when renewed debate on racial inequality and social justice has given rise to increased discussion among health professionals that has identified inequality not only as a social justice issue but also as a public health problem, with tangible population and individual health consequences (40–43).
Our results may be explained by primary care providers’ continued problems with detection of psychological distress among Asians, blacks, and Hispanics, compared with whites (44,45), suggesting that improved provider training in recognizing symptoms among racial-ethnic minority groups and standardized screening might help to improve provider recognition. Increasing managed care penetration (46) and the supply of specialty providers in racially segregated communities (46,47) has been shown to be associated with decreases in racial-ethnic access disparities. Integrated health care initiatives may serve to address issues of recognition and provider supply through the colocation and cross-training of mental health professionals and primary care providers (48) and the provision of mental health treatment by physician extenders, such as nurse practitioners and case managers (49).
Financial and insurance barriers continue to interfere with access to high-quality care among racial-ethnic minority groups (50), because persons from minority groups are more likely to report financial burden as a barrier to mental health treatment (51). Medicare and Medicaid policies could begin to reverse these persistent trends, given that persons from racial-ethnic minority groups are more likely to have low incomes, to be Medicaid beneficiaries, and to be dually eligible for Medicare and Medicaid benefits (52–54). Expanding Medicaid eligibility in states that have opted out of ACA Medicaid expansion, increasing primary care provider or specialist service reimbursement for Medicaid beneficiaries, and decreasing copays in these programs may reduce financial barriers to accessing care.
A secondary finding of note is that although disparities in access to mental health care worsened or persisted between 2004 and 2012, unadjusted mean scores on mental health scales did not change or even improved over time among racial-ethnic minority groups. Future research identifying the impact of access disparities on mental health outcomes is warranted, with attention to effects both at the mean and across the distribution of persistence and severity.
Disparities were consistently wider for Asian Americans than for any other racial-ethnic group. Asian Americans tend to report psychiatric symptoms only when they become severe and may report these symptoms in physical or psychosomatic terms, such as loss of sleep and fatigue (55). Increasing clinician awareness of psychosomatic symptoms may improve recognition and treatment of mental illness among Asian Americans. Some barriers to mental health treatment may be more salient for Asian-American adults (11), including cognitive processes (for example, failure to identify emotional distress as mental illness worthy of treatment), affective issues (for example, shame or stigma), cultural value differences (for example, possible conflicts between collectivist values and the individual orientation of psychotherapy) (56), and fear of the stigma of mental illness, resulting in a reluctance to report psychiatric symptoms (57,58). In some Asian cultures, receiving treatment outside the family may be perceived as shameful, disgraceful, or a violation of the family hierarchical model (58).
There is a need for future research to identify appropriate measures of fully informed preferences (1,59) and to isolate the portion of patient preferences related to past experiences of discrimination (60). For example, categorizing Asian-white differences in cultural values as disparities may not be true to the IOM definition if these factors represent patient preferences (for example, a preference among Asians to treat mental illness with traditional or alternative medicines). However, differences in values could also be regarded as unallowable differences: Asian communities may receive less information about the efficacy of mental health care, and Asian Americans with mental illness may experience double external stigma from the majority group both for being a member of a racial-ethnic minority group and for living with mental illness (61). Preferences for type of treatment may also play an important yet underexamined role. If persons from minority groups prefer psychotherapy over medication and face a shortage of trained psychotherapists—and if researchers should adjust for this preference—then our analysis overestimates the disparity in access to any mental health care. On the contrary, we are likely to underestimate disparities by not adjusting for greater preferences for receiving care from primary care providers among patients from minority groups (62,63) given that there is a relatively greater availability of such providers compared with specialist mental health providers.
This study had several limitations. First, we adjusted for differences in clinical appropriateness and need across racial-ethnic groups by using available mental health measures in the MEPS that have high sensitivity and specificity for mental illness (19–21); however, these are not gold-standard diagnostic measures. Second, we had little information on disparities in the quality of care once persons were in treatment. Third, geographic information in the MEPS is limited to identification of four U.S. regions. Thus our analysis did not allow us to consider the important role of state- and community-level differences found in prior studies of mental health care disparities (46,64). Fourth, the MEPS excludes homeless individuals and those in institutions and does not accurately measure undocumented immigrant status (which would be a large barrier to access). Fifth, our analysis predated the main implementation of the ACA, which should improve access to mental health care and reduce disparities because it aims to increase insurance coverage, contribute resources for establishing mental health clinics to communities with large racial-ethnic minority populations, and invest in a more diverse mental health care workforce.
Despite these limitations, we present evidence that little progress has been made between 2004 and 2012 in reducing mental health care access disparities in the United States. Persons from racial-ethnic minority groups, even after analyses adjusted for clinical need, continued to access mental health care at lower rates than whites. For Hispanics and blacks, this gap in access increased between 2004 and 2012 for any mental health care and psychotropic medications. Given stagnant progress in reducing disparities and increases in disparities for some populations, renewed attention to identifying interventions that improve access to mental health care for racial-ethnic minority groups is urgently needed. In addition, given the breadth of access disparities, clinically oriented interventions that improve the quality of mental health care for minority populations should also be evaluated to understand their broader impact on future community rates of access to care.
Conclusions
Renewed policy and clinical efforts are needed to respond to racial-ethnic disparities in access to mental health care, which remained steady or widened between 2004 and 2012. Growth in black-white and Hispanic-white mental health care disparities over this period appears to have been driven primarily by differential access among these groups to psychotropic medications over this period.
Acknowledgments
Research reported in this publication was supported by the Agency for Healthcare Research and Quality (R01 HS021486 PI Cook) and the National Institute Of Mental Health (T32 MH019733). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality or the National Institutes of Health.
Footnotes
The authors report no financial relationships with commercial interests.
Contributor Information
Dr. Benjamin Lê Cook, Department of Psychiatry, Harvard Medical School, Cambridge
Dr. Nhi-Ha Trinh, Department of Psychiatry, Massachusetts General Hospital, Boston
Zhihui Li, Department of Global Health and Population, Harvard School of Public Health, Boston
Sherry Shu-Yeu Hou, Center for Multicultural Mental Health Research, Cambridge Health Alliance, Cambridge, Massachusetts
Dr. Ana Progovac, Center for Multicultural Mental Health Research, Cambridge Health Alliance and the Department of Health Care Policy, Harvard Medical School, Boston
References
- 1.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Healthy People 2010 Initiative. Washington, DC: US Department of Health and Human Services; 2000. [Google Scholar]
- 3.Healthy People 2020. Washington, DC: US Department of Health and Human Services, Office of Disease Prevention and Health Promotion; 2010. https://www.healthypeople.gov. Accessed Feb 6, 2015. [Google Scholar]
- 4.National Healthcare Disparities Report, 2012. Rockville, Md: Agency for Healthcare Research and Quality; 2012. [Google Scholar]
- 5.Dankwa-Mullan I, Rhee KB, Williams K, et al. The science of eliminating health disparities: summary and analysis of the NIH summit recommendations. American Journal of Public Health. 2010;100(suppl 1):S12–S18. doi: 10.2105/AJPH.2010.191619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blanco C, Patel SR, Liu L, et al. National trends in ethnic disparities in mental health care. Medical Care. 2007;45:1012–1019. doi: 10.1097/MLR.0b013e3180ca95d3. [DOI] [PubMed] [Google Scholar]
- 7.Stockdale SE, Lagomasino IT, Siddique J, et al. Racial and ethnic disparities in detection and treatment of depression and anxiety among psychiatric and primary health care visits, 1995–2005. Medical Care. 2008;46:668–677. doi: 10.1097/MLR.0b013e3181789496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cook BL, McGuire T, Miranda J. Measuring trends in mental health care disparities, 2000 2004. Psychiatric Services. 2007;58:1533–1540. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- 9.Levit KR, Mark TL, Coffey RM, et al. Federal spending on behavioral health accelerated during recession as individuals lost employer insurance. Health Affairs. 2013;32:952–962. doi: 10.1377/hlthaff.2012.1065. [DOI] [PubMed] [Google Scholar]
- 10.Frank RG, Goldman HH, McGuire TG. Trends in mental health cost growth: an expanded role for management? Health Affairs. 2009;28:649–659. doi: 10.1377/hlthaff.28.3.649. [DOI] [PubMed] [Google Scholar]
- 11.Abe-Kim J, Takeuchi DT, Hong S, et al. Use of mental health-related services among immigrant and US-born Asian Americans: results from the National Latino and Asian American Study. American Journal of Public Health. 2007;97:91–98. doi: 10.2105/AJPH.2006.098541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meyer OL, Saw A, Cho YI, et al. Disparities in assessment, treatment, and recommendations for specialty mental health care: patient reports of medical provider behavior. Health Services Research. 2015;50:750–767. doi: 10.1111/1475-6773.12261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu Y, Okuda M, Hser Y, et al. Twelve-month Prevalence of Psychiatric Disorders and Treatment-Seeking Among Asian Americans/Pacific Islanders in the United States: Results From the National Epidemiological Survey on Alcohol and Related Conditions. Bethesda, Md: National Institute on Alcohol Abuse and Alcoholism; 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zuvekas SH. Trends in mental health services use and spending, 1987–1996. Health Affairs. 2001;20:214–224. doi: 10.1377/hlthaff.20.2.214. [DOI] [PubMed] [Google Scholar]
- 15.Lexicon-Drug Product and Disease Listings, 2009. Denver: Cerner Multum; 2009. http://www.multum.com. [Google Scholar]
- 16.Machlin S, Cohen J, Elixhauser A, et al. Sensitivity of household-reported medical conditions in the Medical Expenditure Panel Survey. Medical Care. 2009;47:618–625. doi: 10.1097/MLR.0b013e318195fa79. [DOI] [PubMed] [Google Scholar]
- 17.Lê Cook B, Barry CL, Busch SH. Racial/ethnic disparity trends in children’s mental health care access and expenditures from 2002 to 2007. Health Services Research. 2013;48:129–149. doi: 10.1111/j.1475-6773.2012.01439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lê Cook B, McGuire TG, Lock K, et al. Comparing methods of racial and ethnic disparities measurement across different settings of mental health care. Health Services Research. 2010;45:825–847. doi: 10.1111/j.1475-6773.2010.01100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 20.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire–2: validity of a two-item depression screener. Medical Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 21.Ware J, Kosinski M, Keller S. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. Boston: New England Medical Center, Health Institute; 1995. [Google Scholar]
- 22.Artazcoz L, Benach J, Borrell C, et al. Unemployment and mental health: understanding the interactions among gender, family roles, and social class. American Journal of Public Health. 2004;94:82–88. doi: 10.2105/ajph.94.1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mackenzie CS, Gekoski WL, Knox VJ. Age, gender, and the underutilization of mental health services: the influence of help-seeking attitudes. Aging and Mental Health. 2006;10:574–582. doi: 10.1080/13607860600641200. [DOI] [PubMed] [Google Scholar]
- 24.Cook BL, McGuire TG, Zaslavsky AM. Measuring racial/ethnic disparities in health care: methods and practical issues. Health Services Research. 2012;47:1232–1254. doi: 10.1111/j.1475-6773.2012.01387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cook BL, McGuire TG, Meara E, et al. Adjusting for health status in non-linear models of health care disparities. Health Services and Outcomes Research Methodology. 2009;9:1–21. doi: 10.1007/s10742-008-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McGuire TG, Alegria M, Cook BL, et al. Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Services Research. 2006;41:1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.MEPS HC-036: 1996-2004 Pooled Estimation File. Rockville, Md: Agency for Healthcare Research and Quality; 2005. [Google Scholar]
- 28.MEPS HC-036BRR: 1996-2004 Replicates for Calculating Variances File. Rockville, Md: Agency for Healthcare Research and Quality; 2006. [Google Scholar]
- 29.Stata Statistical Software 9.0. College Station Tex: Stata Corp; 2005. [Google Scholar]
- 30.Kantor ED, Rehm CD, Haas JS, et al. Trends in prescription drug use among adults in the United States From 1999–2012. JAMA. 2015;314:1818–1831. doi: 10.1001/jama.2015.13766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.DeNavas-Walt C, Proctor BD, Smith JC. Current Population Reports, P60-245, Income, Poverty, and Health Insurance Coverage in the United States: 2012. Washington, DC: US Census Bureau; 2013. [Google Scholar]
- 32.Breslau J, Aguilar-Gaxiola S, Kendler KS, et al. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychological Medicine. 2006;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Breslau J, Kendler KS, Su M, et al. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychological Medicine. 2005;35:317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams DR, González HM, Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Archives of General Psychiatry. 2007;64:305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 35.Cook BL, Liu Z, Lessios AS, et al. The costs and benefits of reducing racial-ethnic disparities in mental health care. Psychiatric Services. 2015;66:389–396. doi: 10.1176/appi.ps.201400070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Blanco C, Patel SR, Liu L, et al. National trends in ethnic disparities in mental health care. Medical Care. 2007;45:1012–1019. doi: 10.1097/MLR.0b013e3180ca95d3. [DOI] [PubMed] [Google Scholar]
- 37.National Healthcare Disparities Report, 2014. Rockville, Md: Agency for Healthcare Research and Quality; 2014. [Google Scholar]
- 38.Koh HK. A 2020 vision for healthy people. New England Journal of Medicine. 2010;362:1653–1656. doi: 10.1056/NEJMp1001601. [DOI] [PubMed] [Google Scholar]
- 39.Healthy People 2010 Conference Edition (Online) Washington, DC: US Department of Health and Human Services; 2000. http://wwwhealthgov/healthypeople/Document/defaulthtm. [Google Scholar]
- 40.Martin SA, Harris K, Jack BW. The health of young African American men. JAMA. 2015;313:1415–1416. doi: 10.1001/jama.2015.2258. [DOI] [PubMed] [Google Scholar]
- 41.Bauchner H. Race, poverty, and medicine in the United States. JAMA. 2015;313:1423. doi: 10.1001/jama.2015.2262. [DOI] [PubMed] [Google Scholar]
- 42.Wong WF, LaVeist TA, Sharfstein JM. Achieving health equity by design. JAMA. 2015;313:1417–1418. doi: 10.1001/jama.2015.2434. [DOI] [PubMed] [Google Scholar]
- 43.Bassett MT. #BlackLivesMatter: a challenge to the medical and public health communities. New England Journal of Medicine. 2015;372:1085–1087. doi: 10.1056/NEJMp1500529. [DOI] [PubMed] [Google Scholar]
- 44.Borowsky SJ, Rubenstein LV, Meredith LS, et al. Who is at risk of nondetection of mental health problems in primary care? Journal of General Internal Medicine. 2000;15:381–388. doi: 10.1046/j.1525-1497.2000.12088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chung H, Teresi J, Guarnaccia P, et al. Depressive symptoms and psychiatric distress in low income Asian and Latino primary care patients: prevalence and recognition. Community Mental Health Journal. 2003;39:33–46. doi: 10.1023/a:1021221806912. [DOI] [PubMed] [Google Scholar]
- 46.Cook BL, Doksum T, Chen CN, et al. The role of provider supply and organization in reducing racial/ethnic disparities in mental health care in the US. Social Science and Medicine. 2013;84:102–109. doi: 10.1016/j.socscimed.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dinwiddie GY, Gaskin DJ, Chan KS, et al. Residential segregation, geographic proximity and type of services used: evidence for racial/ethnic disparities in mental health. Social Science and Medicine. 2013;80:67–75. doi: 10.1016/j.socscimed.2012.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Unützer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 49.Miranda J, Duan N, Sherbourne C, et al. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Services Research. 2003;38:613–630. doi: 10.1111/1475-6773.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Galea S, Vlahov D. Urban health: evidence, challenges, and directions. Annual Review of Public Health. 2005;26:341–365. doi: 10.1146/annurev.publhealth.26.021304.144708. [DOI] [PubMed] [Google Scholar]
- 51.Ojeda VD, Bergstresser SM. Gender, race-ethnicity, and psychosocial barriers to mental health care: an examination of perceptions and attitudes among adults reporting unmet need. Journal of Health and Social Behavior. 2008;49:317–334. doi: 10.1177/002214650804900306. [DOI] [PubMed] [Google Scholar]
- 52.State Health Facts. Distribution of Medicare Beneficiaries by Race/Ethnicity. Washington, DC: Kaiser Family Foundation; 2014. [Google Scholar]
- 53.State Health Facts. Dual Eligible Beneficiaries by Race/Ethnicity. Washington, DC: Kaiser Family Foundation; 2011. [Google Scholar]
- 54.Jacobson G, Huang J, Neuman T, et al. Wide Disparities in the Income and Assets of People on Medicare by Race and Ethnicity: Now and in the Future. Washington, DC: Kaiser Family Foundation; 2013. [Google Scholar]
- 55.Lin JY, Shrout P, Yang F, et al. Measurement bias in the screener questions for the depression section of the Composite International Diagnostic Interview. 2009 Unpublished. [Google Scholar]
- 56.Leong FTL, Lau ASL. Barriers to providing effective mental health services to Asian Americans. Mental Health Services Research. 2001;3:201–214. doi: 10.1023/a:1013177014788. [DOI] [PubMed] [Google Scholar]
- 57.Leong FT, Lau AS. Barriers to providing effective mental health services to Asian Americans. Mental Health Services Research. 2001;3:201–214. doi: 10.1023/a:1013177014788. [DOI] [PubMed] [Google Scholar]
- 58.Inman AG, Yeh C. Stress and coping. In: Leong F, Inman G, Ebreo A, et al., editors. Handbook of Asian American Psychology. Thousand Oaks, Calif: Sage; 2006. [Google Scholar]
- 59.Ashton CM, Haidet P, Paterniti DA, et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? Journal of General Internal Medicine. 2003;18:146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cooper-Patrick L, Powe NR, Jenckes MW, et al. Identification of patient attitudes and preferences regarding treatment of depression. Journal of General Internal Medicine. 1997;12:431–438. doi: 10.1046/j.1525-1497.1997.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gary FA. Stigma: barrier to mental health care among ethnic minorities. Issues in Mental Health Nursing. 2005;26:979–999. doi: 10.1080/01612840500280638. [DOI] [PubMed] [Google Scholar]
- 62.Cooper-Patrick L, Gallo JJ, Powe NR, et al. Mental health service utilization by African Americans and whites: the Baltimore Epidemiologic Catchment Area Follow-Up. Medical Care. 1999;37:1034–1045. doi: 10.1097/00005650-199910000-00007. [DOI] [PubMed] [Google Scholar]
- 63.Miranda J, Cooper LA. Disparities in care for depression among primary care patients. Journal of General Internal Medicine. 2004;19:120–126. doi: 10.1111/j.1525-1497.2004.30272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Horvitz-Lennon M, Alegría M, Normand SL. The effect of race-ethnicity and geography on adoption of innovations in the treatment of schizophrenia. Psychiatric Services. 2012;63:1171–1177. doi: 10.1176/appi.ps.201100408. [DOI] [PMC free article] [PubMed] [Google Scholar]


