Abstract
The purpose of this meta-analysis is to investigate whether statin is a key therapy for myocardial infarction (MI) by comparing all randomized controlled trials that appraised the effects of statin on risk of MI.
Pubmed, Embase, and Medline databases (up to December 2016) were used to search all related articles. Using the data from 18 available publications, we examined the efficacy in treating or reducing the risk of MI by using random-effects models of odds ratio (OR) comparing the highest with the lowest category.
Statins have demonstrated efficacy in treating or reducing the risk of MI (OR = 0.73, 95% confidence interval = 0.58–0.93, P = .010).
This meta-analysis suggests that statin have light efficacy in treating or reducing the risk of MI patients.
Keywords: meta-analysis, myocardial infarction, statin
1. Introduction
The Global Status Report states that cardiovascular disease (CAD) has caused more and more deaths.[1] Myocardial infarction (MI) is the most serious and fatal result of CAD. The main nosogenesis is the extensive necrosis of cardiomyocytes caused by prolonged ischemia.[2] The development of CAD is a long-time process that suffered from erosion of endothelium to narrowing of artery. On the contrary, MI is an emergency and much more serious. It suddenly happens in a few minutes when the oxygen supply is blocked, and results in myocardial cell death in a few hours. Therefore, the prevention and reconstruction of the occluded artery is the key factor for MI.[3]
The treatment of statins for the prevention of recurrent MI has been demonstrated in several randomized controlled trials.[4] Statins is an inhibitor of hydroxymethylglutaryl-CoA reductase, and it is identified to have pleiotropic effects, such as anti-inflammatory and antithrombotic properties and antioxidant effects.[5–7] Therefore, statins are regarded as an important agent for the prevention of MI. Some studies showed that statin pretreatment is associated with a significant reduction in MI. However, other clinical studies showed that early use of statin did not reduce the occurrence of MI.[8,9] Therefore, a more comprehensive analysis of benefits of statin for MI is needed. Thus, we performed a meta-analysis of 18 randomized controlled trials to reevaluate the efficacy of statin treatment to prevent MI in patients.
2. Material and methods
2.1. Publication search
We obtained relevant randomized controlled trials from Pubmed, Embase, and Chinese biomedicine database that were treated with statin and MI. For the computer searches, we used the following key words: “statin,” “Atorvastatin,” “Rosuvastatin,” “Pravastatin,” “Myocardial infarction,” or “MI,” in the title or abstract, and was limited by “clinical trials, randomized controlled trial-” published in English between 2005 and 2017. Studies contained available data that showed the association of statin treatment in MI. Among the studies with overlapping data published by the same author, only the complete study was included in this meta-analysis. Furthermore, included studies had to show their results as an odds ratio (OR) and 95% confidence interval (95% CI).
2.2. Data extraction and classification
For each study characteristics, data were extracted, including the first author, publication year, type of statin, type of study design, sample characteristics, sample size and OR, and risk estimates with corresponding 95% CI.
2.3. Statistical analysis
The measure of effect of interest is the OR and the corresponding 95% CI. We showed all results as OR for simplicity and quantified the association of statin treatment in MI, using random-effects models of OR comparing the highest with the lowest category. The summary OR estimates were obtained from random effects models.[10]
For all analyses, P < .05 were considered significant. Publication bias was assessed by a Begg-adjusted rank correlation test (funnel plot method) and Egger linear regression asymmetry test.[11] All mate-analyses were carried out using Stata software (version 9.0; Stata Corporation, College Station, TX).
2.4. Ethical approval
Ethical approval was waived or not necessary. Because we did not make any clinical research in this manuscript, we just collected the data from available publications.
3. Results
3.1. Characteristics of studies for meta-analysis
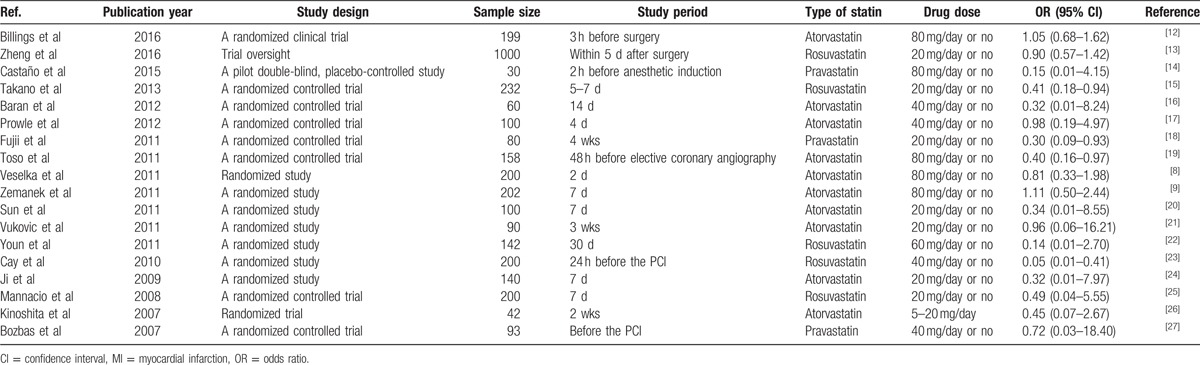
A total of 18 publications were identified for inclusion statin in the MI (Table 1).[12–27] Among the 18 studies, 10 described treatment with atorvastatin, 5 with rosuvastatin, and the other 3 treatment with pravastatin. All studies compared a statin with placebo. Of the18 placebo-controlled studies, 16 showed that statins were effective in reducing the incidence of MI.
Table 1.
The distribution and ORs (95% CI) for studies on MI and statin.
3.2. Statin and MI
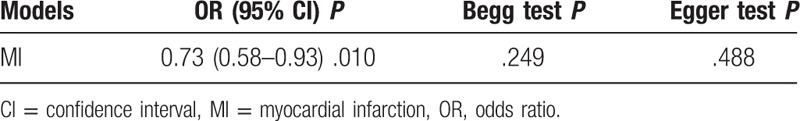
The association of statin treatment of MI was identified in 18 studies, including comparisons of atorvastatin versus placebo, rosuvastatin versus Placebo, and pravastatin versus placebo (Table 1). Pooled estimates showed a statistically significant 27% reduction in the risk of MI with statin (OR = 0.73, 95% CI 0.58–0.93, P = .010) (Fig. 1, Table 2). These data indicate that statin was associated with a reduction in MI.
Figure 1.
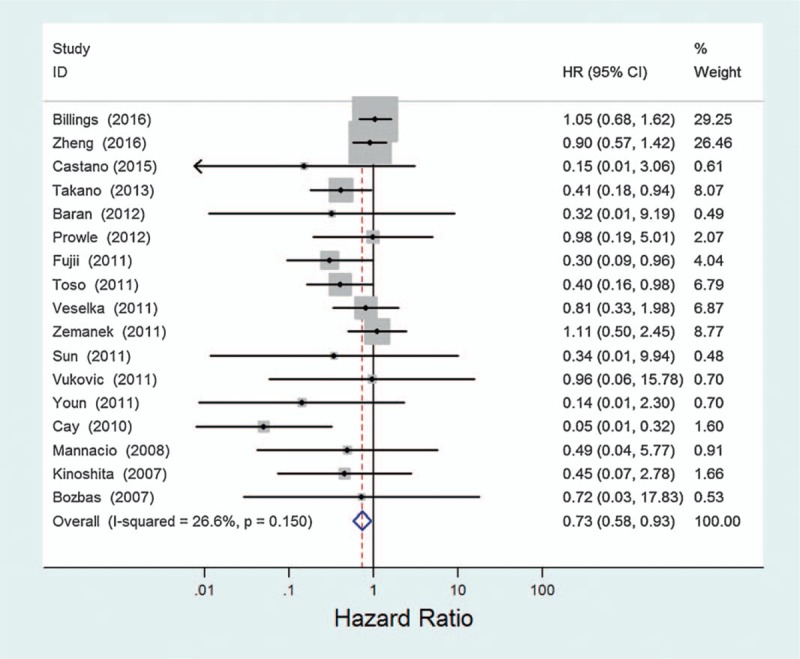
Estimated odds ratio (OR) of risk for MI under statin therapy.
Table 2.
Summary ORs and 95% CI for statin and MI.
4. Discussion
Our meta-analysis suggests that statins have demonstrated efficacy in treating or reducing the risk of MI. Statins have a little protective effect for MI, with a 27% lower risk in MI. The intense inhibition of hydroxymethylglutaryl-CoA reductase function precipitated by statin therapy can lead to inhibition of buildup of plaque.
Although the exact mechanisms underlying the early protective effects of statin in cardiovascular events remain undetermined, the statin still contains pleiotropic effect, which includes anti-inflammation, anti-platelet aggregation, and plaque stability.[28,29] Studies suggested that a reduction of MI injury after statin treatment is associated with attenuated inflammatory response.[30] This may be the reason that patient with acute coronary syndromes may benefit most from statins therapy before MI. In addition, animal studies also showed that cardioprotection of statin reloading before ischemia can be restored.[31] This suggested that statin treatment is needed to reach the desired pleiotropic effects.
In summary, our meta-analysis provided some support for the hypothesis that statins have demonstrated efficacy in treating or reducing the risk of MI. However, the number of studies is not enough and we just analyze the data of OR. Future well-designed, large studies might be necessary and should consider the interrelations between different statins.
5. Author contributions
Data curation: H. Zhang, Y. Zhang, Y. Wang.
Software: L. Yin, L. Zhang.
Writing – original draft: X. Han.
Writing – review & editing: B. Li.
Footnotes
Abbreviations: CAD = cardiovascular disease, CI = 95% confidence interval, MI = myocardial infarction, OR = odds ratio.
The authors declare that they have no competing interests.
References
- [1].Mendis S, Davis S, Norrving B. Organizational update: the world health organization global status report on noncommunicable diseases 2014; one more landmark step in the combat against stroke and vascular disease. Stroke 2015;46:e121–2. [DOI] [PubMed] [Google Scholar]
- [2].Weintraub WS, Daniels SR, Burke LE, et al. American Heart Association Advocacy Coordinating C, Council on Cardiovascular Disease in the Y, Council on the Kidney in Cardiovascular D, Council on E, Prevention, Council on Cardiovascular N, Council on A, Thrombosis, Vascular B, Council on Clinical C, and Stroke C. Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association. Circulation 2011;124:967–90. [DOI] [PubMed] [Google Scholar]
- [3].Thygesen K, Alpert JS, Jaffe AS, et al. Writing Group on behalf of the Joint E S C A A H A W H F T F f t U D o M I. Third universal definition of myocardial infarction. Glob Heart 2012;7:275–95. [DOI] [PubMed] [Google Scholar]
- [4].Baigent C, Keech A, Kearney PM, et al. Cholesterol Treatment Trialists C. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005;366:1267–78. [DOI] [PubMed] [Google Scholar]
- [5].Macin SM, Perna ER, Farias EF, et al. Atorvastatin has an important acute anti-inflammatory effect in patients with acute coronary syndrome: results of a randomized, double-blind, placebo-controlled study. Am Heart J 2005;149:451–7. [DOI] [PubMed] [Google Scholar]
- [6].Sanguigni V, Pignatelli P, Lenti L, et al. Short-term treatment with atorvastatin reduces platelet CD40 ligand and thrombin generation in hypercholesterolemic patients. Circulation 2005;111:412–9. [DOI] [PubMed] [Google Scholar]
- [7].Wagner AH, Kohler T, Ruckschloss U, et al. Improvement of nitric oxide-dependent vasodilatation by HMG-CoA reductase inhibitors through attenuation of endothelial superoxide anion formation. Arterioscler Thromb Vasc Biol 2000;20:61–9. [DOI] [PubMed] [Google Scholar]
- [8].Veselka J, Zemanek D, Hajek P, et al. Effect of two-day atorvastatin pretreatment on the incidence of periprocedural myocardial infarction following elective percutaneous coronary intervention: a single-center, prospective, and randomized study. Am J Cardiol 2009;104:630–3. [DOI] [PubMed] [Google Scholar]
- [9].Zemanek D, Branny M, Martinkovicova L, et al. Effect of seven-day atorvastatin pretreatment on the incidence of periprocedural myocardial infarction following percutaneous coronary intervention in patients receiving long-term statin therapy. A randomized study. Int J Cardiol 2013;168:2494–7. [DOI] [PubMed] [Google Scholar]
- [10].DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177–88. [DOI] [PubMed] [Google Scholar]
- [11].Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Billings FTt, Hendricks PA, Schildcrout JS, et al. High-dose perioperative atorvastatin and acute kidney injury following cardiac surgery: a randomized clinical trial. JAMA 2016;315:877–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Zheng Z, Jayaram R, Jiang L, et al. Perioperative rosuvastatin in cardiac surgery. N Engl J Med 2016;374:1744–53. [DOI] [PubMed] [Google Scholar]
- [14].Castano M, Gonzalez-Santos JM, Lopez J, et al. Effect of preoperative oral pravastatin reload in systemic inflammatory response and myocardial damage after coronary artery bypass grafting. A pilot double-blind placebo-controlled study. J Cardiovasc Surg (Torino) 2015;56:617–29. [PubMed] [Google Scholar]
- [15].Takano H, Ohba T, Yamamoto E, et al. Usefulness of rosuvastatin to prevent periprocedural myocardial injury in patients undergoing elective coronary intervention. Am J Cardiol 2013;111:1688–93. [DOI] [PubMed] [Google Scholar]
- [16].Baran C, Durdu S, Dalva K, et al. Effects of preoperative short term use of atorvastatin on endothelial progenitor cells after coronary surgery: a randomized, controlled trial. Stem Cell Rev 2012;8:963–71. [DOI] [PubMed] [Google Scholar]
- [17].Prowle JR, Calzavacca P, Licari E, et al. Pilot double-blind, randomized controlled trial of short-term atorvastatin for prevention of acute kidney injury after cardiac surgery. Nephrology (Carlton) 2012;17:215–24. [DOI] [PubMed] [Google Scholar]
- [18].Fujii K, Kawasaki D, Oka K, et al. The impact of pravastatin pre-treatment on periprocedural microcirculatory damage in patients undergoing percutaneous coronary intervention. JACC Cardiovasc Interv 2011;4:513–20. [DOI] [PubMed] [Google Scholar]
- [19].Toso A, Leoncini M, Maioli M, et al. Short-term high-dose atorvastatin for periprocedural myocardial infarction prevention in patients with renal dysfunction. J Cardiovasc Med (Hagerstown) 2011;12:318–21. [DOI] [PubMed] [Google Scholar]
- [20].Sun Y, Ji Q, Mei Y, et al. Role of preoperative atorvastatin administration in protection against postoperative atrial fibrillation following conventional coronary artery bypass grafting. Int Heart J 2011;52:7–11. [DOI] [PubMed] [Google Scholar]
- [21].Vukovic PM, Maravic-Stojkovic VR, Peric MS, et al. Steroids and statins: an old and a new anti-inflammatory strategy compared. Perfusion 2011;26:31–7. [DOI] [PubMed] [Google Scholar]
- [22].Youn YN, Park SY, Hwang Y, et al. Impact of high-dose statin pretreatment in patients with stable angina during off-pump coronary artery bypass. Korean J Thorac Cardiovasc Surg 2011;44:208–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Cay S, Cagirci G, Sen N, et al. Prevention of peri-procedural myocardial injury using a single high loading dose of rosuvastatin. Cardiovasc Drugs Ther 2010;24:41–7. [DOI] [PubMed] [Google Scholar]
- [24].Ji Q, Mei Y, Wang X, et al. Effect of preoperative atorvastatin therapy on atrial fibrillation following off-pump coronary artery bypass grafting. Circ J 2009;73:2244–9. [DOI] [PubMed] [Google Scholar]
- [25].Mannacio VA, Iorio D, De Amicis V, et al. Effect of rosuvastatin pretreatment on myocardial damage after coronary surgery: a randomized trial. J Thorac Cardiovasc Surg 2008;136:1541–8. [DOI] [PubMed] [Google Scholar]
- [26].Kinoshita M, Matsumura S, Sueyoshi K, et al. Randomized trial of statin administration for myocardial injury: is intensive lipid-lowering more beneficial than moderate lipid-lowering before percutaneous coronary intervention? Circ J 2007;71:1225–8. [DOI] [PubMed] [Google Scholar]
- [27].Bozbas H, Yildirir A, Mermer S, et al. Does pravastatin therapy affect cardiac enzyme levels after percutaneous coronary intervention? Adv Ther 2007;24:493–504. [DOI] [PubMed] [Google Scholar]
- [28].Buffon A, Liuzzo G, Biasucci LM, et al. Preprocedural serum levels of C-reactive protein predict early complications and late restenosis after coronary angioplasty. J Am Coll Cardiol 1999;34:1512–21. [DOI] [PubMed] [Google Scholar]
- [29].Delhaye C, Maluenda G, Wakabayashi K, et al. Long-term prognostic value of preprocedural C-reactive protein after drug-eluting stent implantation. Am J Cardiol 2010;105:826–32. [DOI] [PubMed] [Google Scholar]
- [30].Patti G, Chello M, Gatto L, et al. Short-term atorvastatin preload reduces levels of adhesion molecules in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Results from the ARMYDA-ACS CAMs (Atorvastatin for Reduction of MYocardial Damage during Angioplasty-Cell Adhesion Molecules) substudy. J Cardiovasc Med (Hagerstown) 2010;11:795–800. [DOI] [PubMed] [Google Scholar]
- [31].Mensah K, Mocanu MM, Yellon DM. Failure to protect the myocardium against ischemia/reperfusion injury after chronic atorvastatin treatment is recaptured by acute atorvastatin treatment: a potential role for phosphatase and tensin homolog deleted on chromosome ten? J Am Coll Cardiol 2005;45:1287–91. [DOI] [PubMed] [Google Scholar]


