Abstract
Background:
High-viscosity cement (HVC) has been gradually applied in percutaneous vertebroplasty (PVP) and percutaneous kyphoplasty (PKP). Although HVC has been reported to reduce cement leakage, different opinions exist. To assess the complications of HVC in cement leakage in the treatment of vertebral compression fractures and to evaluate the clinical effect of HVC compared with low-viscosity cement (LVC).
Methods:
EMBASE, PubMed, Science Direct, Google Scholar and Cochrane Library databases were comprehensively searched from their inception to August 2017. Two researchers independently searched for articles and reviewed all retrieved studies. Forest plots were used to illustrate the results. The Q-test and I2 statistic were employed to evaluate between-study heterogeneity. Potential publication bias was assessed by funnel plot.
Results:
HVC reduced the occurrence of cement leakage (risk ratio (RR) = 0.38, 95% confidence interval (CI) = 0.29 to 0.51, P < 0.00001), especially in the disc space (RR = 0.45, 95% CI = 0.45 to 0.80, P = 0.007) and the vein (RR = 0.54, 95% CI = 0.35 to 0.85, P = 0.008) but not in the intraspinal space (RR = 0.48, 95% CI = 0.19 to 1.23, P = 0.13) or the paravertebral area (RR = 0.63, 95% CI = 0.32 to 1.22, P = 0.17). No significant differences in the visual analogue scale (VAS), Oswestry Disability Index (ODI), injected cement volume or adjacent vertebral fracture were noted between HVC and LVC (P > 0.05).
Conclusion:
Compared with LVC, HVC results in a reduced incidence of cement leakage for the treatment of vertebral compression fractures, especially in the disc space and vein but not in the intraspinal space or the paravertebral area. In addition, HVC yields the same satisfactory clinical effect as LVC.
Keywords: cement leakage, high-viscosity cement, low-viscosity cement, meta-analysis, vertebral compression fracture, vertebroplasty
1. Introduction
Vertebral compressive fractures (VCFs) are a common type of fracture in the elderly. VCFs are caused mainly by osteoporosis or malignant tumors and can result in back pain, loss of mobility, spinal deformities, neural compromise, and even paralysis.[1–4] Traditional therapies include long-term bed rest, analgesics, physiotherapy, and classical open surgery. However, some accompanying complications of long-term bed rest, such as bedsores, urinary infection, pneumonia, malnutrition, deep vein thrombosis, and even stroke, may gradually emerge.[5] Classical open surgery also has risks, including bleeding, surgical trauma, slow postoperative recovery, and the possibility of screw loosening and even revision.
In recent years, percutaneous vertebroplasty (PVP) and percutaneous kyphoplasty (PKP) have gradually been applied to the treatment of VCFs. These treatments have the advantages of minimal invasiveness, fast recovery, pain relief, and vertebral collapse prevention.[6,7] However, cement leakage occurs at a frequency as high as 30% to 70% in PVP or PKP procedures.[8–10] Although most leaks are clinically asymptomatic,[10] these leaks increase the risk of pulmonary embolism and neurological complications.[11,12] If leakage into the vessels causes thermal damage to the vessels, pulmonary embolism or even death, leakage into the intraspinal space may compress the spinal cord, resulting in functional disorder of the segments or even paralysis.[13,14] Therefore, cement leakage has received extensive attention from researchers. Some researchers believe that cement viscosity is the main factor of leakage and that increasing the viscosity can greatly reduce cement leakage.[15,16] For instance, Zhang et al[16] conducted a prospective study that included 32 patients with severe osteoporotic vertebral compression fractures and found that high-viscosity cement (HVC) exhibited reduced leakage compared with low-viscosity cement (LVC). In addition, a retrospective cohort study also revealed that PVP with HVC exhibited a reduced cement leakage rate.[17] However, some researchers held a different view that there was no significant difference in the cement leakage rate between HVC and LVC.[18,19] In addition, the results of numerous studies based on the locations of cement leakage, such as leakage into the paravertebral area, the venous system, the disc space, and the intraspinal space, also differed. A prospective cohort study reported that no differences were found in the intraspinal space, paravertebral area or peripheral vein, except for the disc space.[20] Another prospective cohort study indicated that, compared with LVC, HVC reduced cement leakage into the disc space, and the reduction in the venous leak obtained with HVC was highly significant.[21] Wiese et al[22] found that the venous cement leakage of HVC was significantly reduced compared with that of LVC, whereas this difference was statistically insignificant regarding disc space leakage. In addition, we conducted a retrospective cohort study to confirm that HVC reduced the leakage of the paravertebral area and vein but not the disc or intraspinal space.[23] However, no differences were observed in cement leakage of the vein, disc, paravertebral, or intraspinal space in a retrospective cohort study.[19]
Consequently, to investigate the differences in cement leakage and the different locations of leakage between HVC and LVC in the treatment of VCFs and to evaluate their clinical efficacy, we conducted a systematic review and meta-analysis.
2. Materials and methods
2.1. Search strategy
Two of the authors comprehensively searched all relevant literature from electronic databases, including EMBASE, PubMed, Science Direct, Google Scholar, and Cochrane Library, from their inception to August 2017 without restriction of regions or languages. Prospective randomized controlled trials (RCTs) and cohort (prospective and retrospective) studies were searched using the following key terms: osteoporosis, VCFs, HVC, LVC, vertebroplasty, and kyphoplasty. Moreover, the reference lists of the related literature were also used to expand the search. Any disagreement between the 2 investigators was resolved by consensus with a third reviewer.
2.2. Inclusion and exclusion criteria
The inclusion criteria were as follows: RCTs and cohort studies; vertebral augmentation with HVC and LVC as exposure; cement leakage as the main outcome; results including means and standard deviations or dichotomous data, or the inclusion of sufficient information to derive the latter. Exclusion criteria were as follows: repeated or overlapped publications; reviews; basic science experiments; animal or cadaver studies; and studies with unavailable data.
2.3. Data extraction
Two reviewers used a standardized form and extracted relevant information from each eligible study independently. Information included study name (first author), publication year, study location, study design, study population, sample size, surgical methods, VCF levels, vertebrae of cement leakage, cement leakage locations, visual analog scale (VAS), Oswestry Disability Index (ODI), and adjacent vertebral fracture. Locations of cement leakage were categorized as the paravertebral area, the intraspinal space, the disc space, and the peripheral vein based on information presented in the articles. Short- and long-term follow-up periods were defined as 1 to 3 and 6 to 12 months, respectively.
2.4. Quality assessment
The methodological quality of all included studies was assessed with the Newcastle–Ottawa scale (NOS) and Cochrane review criteria. The NOS, which has a score of 0 to 9 (allocated as stars), was used to assess cohort studies, and a high-quality study had 6 or more stars.[24,25] Cochrane review criteria were used to assess RCT studies. Cochrane review criteria can be used to assess the risk of bias of an RCT study and consists of random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias.[26]
2.5. Ethical statement
All results and analyses were from previous published studies, thus no ethical approval and patient consent are required.
2.6. Statistical analysis
All statistical analyses were performed with Review Manager 5.3. All continuous variables of the included studies were pooled to a mean difference (MD) and a 95% confidence interval (CI). The risk ratio (RR) and 95% CI were determined for dichotomous variables. P < .05 indicated a significant difference. Heterogeneity was measured with the Q-test and the I2 statistic, and P < .10 and I2 > 50% indicated high heterogeneity.[27,28] If significant heterogeneity existed between studies, a random-effects model was used. Otherwise, the fixed-effects model was used.[29] Sensitivity analysis was used to test the source of high heterogeneity by removing the study. Subgroup analysis was performed based on the surgical methods, locations of cement leakage, and follow-up. A funnel plot was used to identify potential publication bias.
3. Results
3.1. Search results
A total of 272 relevant articles were obtained in the initial literature search. After removing duplicate studies and irrelevant and incomplete data, 7 studies were included (Fig. 1).
Figure 1.
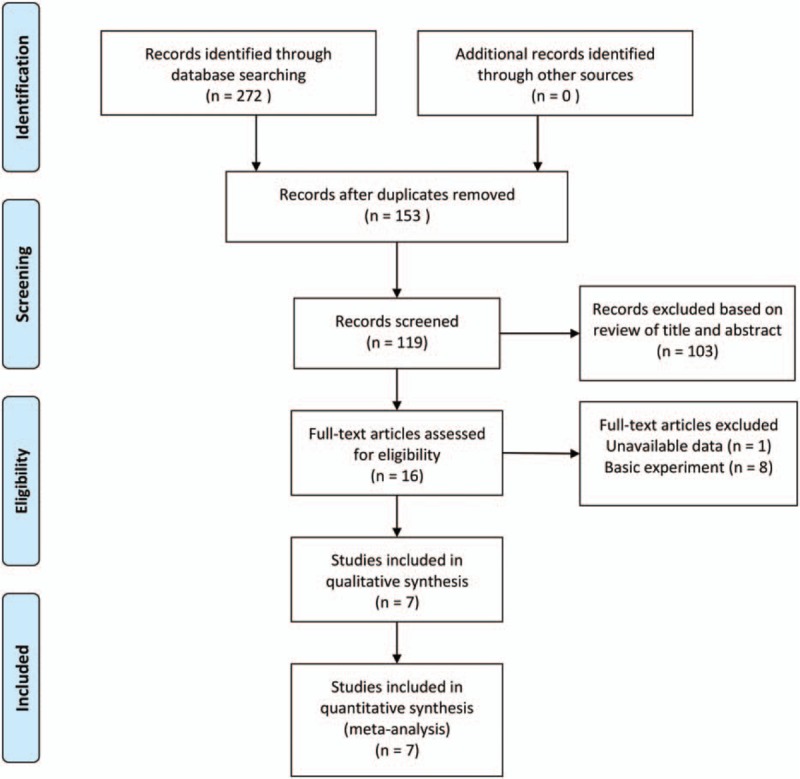
Summary of the article selection and exclusion process.
3.2. Characteristics of included studies and quality assessment
Two RCTs (1 meeting abstract and 1 full text)[16,22] and 5 cohort studies (3 prospective and 2 retrospective)[17,18,20,21,23] with a total of 490 patients and 712 vertebral bodies were included in this meta-analysis. Relevant information on these studies is presented in Table 1.
Table 1.
Characteristics of included studies.
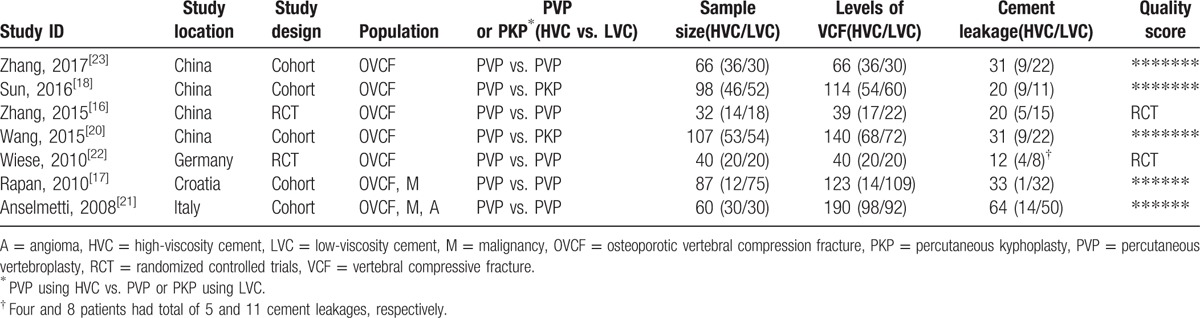
The methodological quality of the included RCT studies was assessed using Cochrane review criteria. One RCT[16] was of moderate quality, and another study[22] was of low quality because it was a meeting abstract (Fig. 2). All cohort studies were assigned 6 or more stars; therefore, these studies were considered high quality (Table 1).
Figure 2.
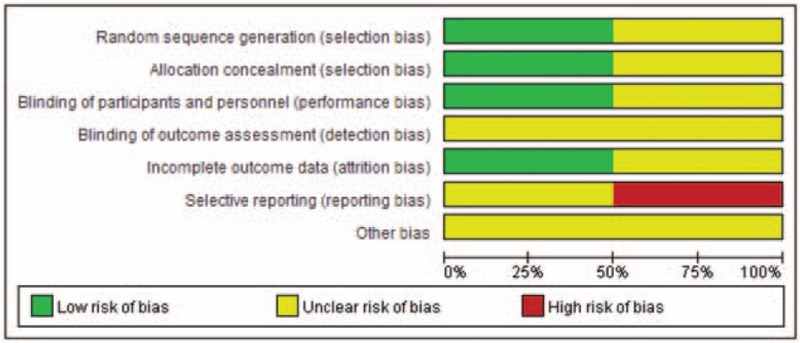
Risk of bias graph of the 2 RCT studies. RCT = randomized controlled trials.
3.3. Primary outcome: Cement leakage
A total of 307 and 405 vertebrae were present in the HVC and LVC groups, which included 51 and 160 cases of cement leakage, respectively. The pooled results revealed that HVC reduced the occurrence of cement leakage (RR = 0.38, 95% CI = 0.29–0.51, P < .00001) (Fig. 3). We also performed a subgroup analysis based on PVP with HVC and PVP or PKP with LVC. HVC reduced cement leakage for either PVP using HVC versus PKP using LVC (RR = 0.59, 95% CI = 0.35–0.99, P = .05) (P = .05 was considered to indicate a significant difference because it was on the margin of statistics, and the diamond was located on the left side of the invalid line without crossing) or PVP using HVC versus PVP using LVC (RR = 0.32, 95% CI = 0.23–0.45, P < .00001) (Fig. 4). The results of another subgroup analysis based on locations of cement leakage indicated that the leakages of the vein (RR = 0.54, 95% CI = 0.35–0.85, P = .008) and the disc space (RR = 0.45, 95% CI = 0.45–0.80, P < .007) in the HVC group were significantly reduced compared with those in the LVC group; the leakages of the intraspinal space (RR = 0.48, 95% CI = 0.19–1.23, P = .13) and the paravertebral area (RR = 0.63, 95% CI = 0.32–1.22, P = .17) were not significantly reduced (Fig. 5).
Figure 3.
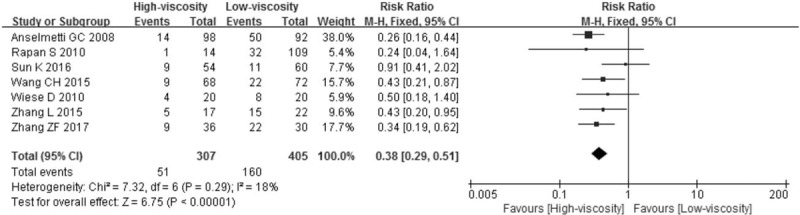
Cement leakage between the HVC and LVC. HVC = high-viscosity cement, LVC = low-viscosity cement.
Figure 4.
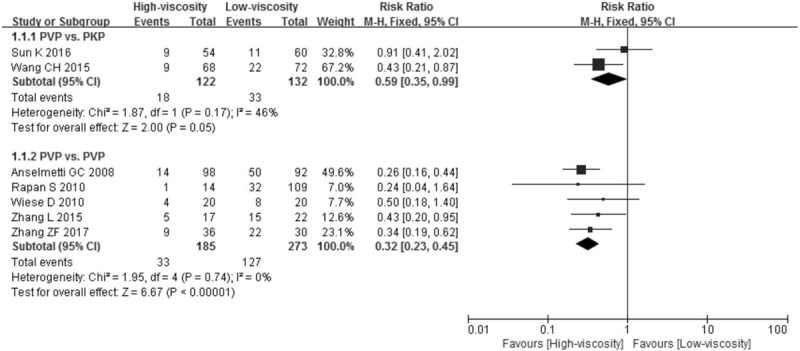
Subgroup analysis of cement leakage based on different surgical methods.
Figure 5.
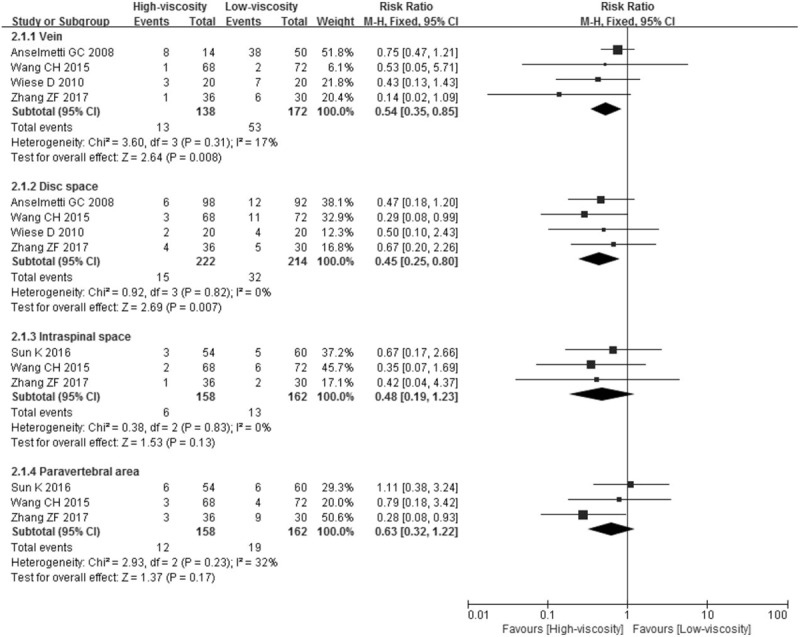
Subgroup analysis of cement leakage based on different locations of cement leakage.
3.4. Secondary outcomes: VAS, ODI, injected cement volume, and adjacent vertebral fracture
We extracted all available VAS and ODI in the included studies and then summarized them as preoperative, within 7 days postoperatively, short- and long-term follow-up. For the VAS, the results revealed no significant difference at the preoperative time point (MD = 0.07, 95% CI = −0.15 to 0.28, P = .55), within 7 days postoperatively (MD = −0.10, 95% CI = −0.27 to 0.06, P = .22) or at long-term follow-up (MD = 0.09, 95% CI = −0.11 to 0.28, P = .39), whereas differences were present at the short-term follow-up (MD = 0.29, 95% CI = 0.10–0.47, P = .003) (Fig. 6).
Figure 6.
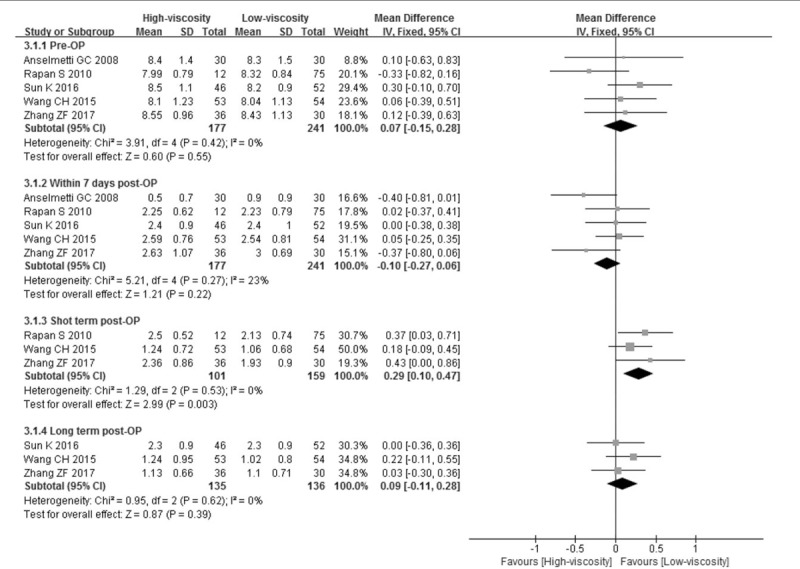
Visual analog scale at the preoperative and postoperative follow-up.
Regarding the ODI, similar results were also observed in this subgroup analysis. No differences were found between HVC and LVC at the preoperative time point (MD = −1.60, 95% CI = −3.85 to 0.65, P = .16), within 7 days postoperatively (MD = 0.10, 95% CI = −2.12 to 2.32, P = .93), or at short-term (MD = −0.15, 95% CI = −1.70 to 1.41, P = .85) or long-term follow-up (MD = 0.12, 95% CI = −1.25 to 1.50, P = .86) (Fig. 7).
Figure 7.
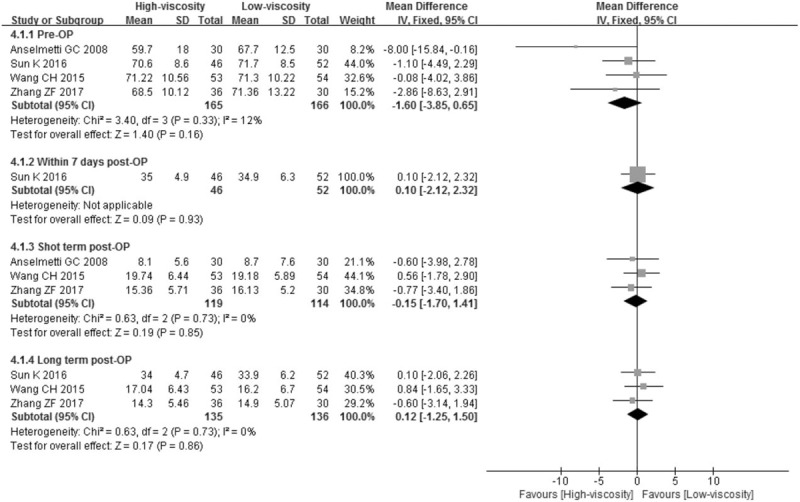
Oswestry Disability Index at the preoperative and postoperative follow-up.
The injected cement volume for PVP using HVC was reduced compared with that for PKP using LVC (MD = −0.81, 95% CI = −0.90 to −0.72, P < .00001), but no significant difference was noted between PVP using HVC and PVP using LVC (MD = −0.19, 95% CI = −0.47 to 0.10, P = .20) (Fig. 8).
Figure 8.
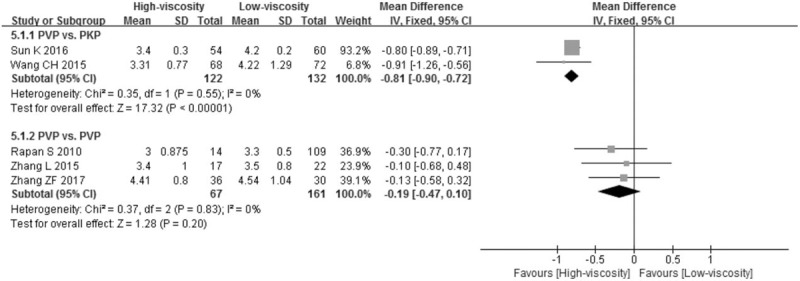
Subgroup analysis of injected cement volume based on different surgical methods.
Adjacent vertebral fractures were present in 4 studies. The pooled results revealed that 4 and 2 vertebral fractures were observed in the HVC and LVC groups, respectively (MD = 1.68, 95% CI = 0.37–7.67, P = .50) (Fig. 9).
Figure 9.
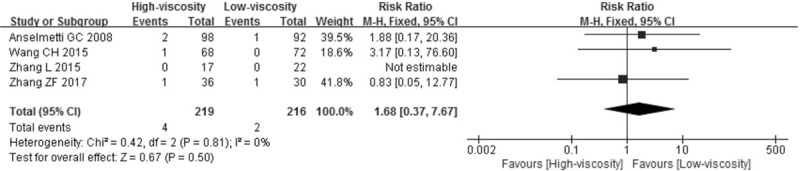
Adjacent vertebral fracture.
3.5. Sensitivity analysis and publication bias
Sensitivity analysis was not performed because heterogeneity was low in all our meta-analyses. Figure 10 presents a funnel plot based on different locations of cement leakage, indicating slight asymmetry.
Figure 10.
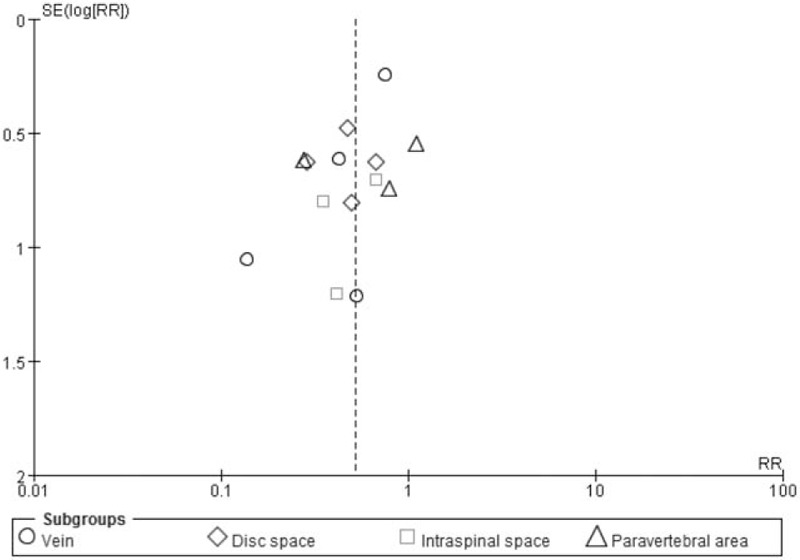
Funnel plot.
4. Discussion
This is the first meta-analysis of studies comparing the effect of HVC and LVC for the treatment of VCFs. This study of 490 patients with 712 vertebrae revealed that HVC reduced cement leakage, especially in the disc space and the peripheral vein but not in the intraspinal space or the paravertebral area. In addition, no difference in the injected cement volume was noted between PVP using HVC and PVP using LVC, but a difference was observed between PVP using HVC and PKP using LVC. Regarding the VAS and ODI, both HCV and LVC could provide pain relief and life quality improvement, and no difference was observed between these factors at the postoperative follow-up, except the VAS of the postoperative short-term follow-up. Four of 219 vertebrae in the HVC group and 2 of 216 in the LVC group incurred adjacent vertebral fractures, and no significant differences were noted between the groups.
In this systematic assessment, 2 RCTs and 5 cohort studies met the predefined eligibility criteria in assessing the cement leakage of HVC and LVC for VCFs. In 1 included RCT,[16] the authors did not specify whether the outcomes were blinded, so the decision was an unclear risk. In addition, the outcome data of this study were incomplete. Patients were followed up at 3 days and 3, 12, and 18 months after surgery in the methods. However, the authors only described VAS and ODI data at 18 months after surgery, and other time points were not described in the results. Therefore, we determined that this study had a high risk. Based on the Cochrane scoring criteria,[26] the study was considered a moderate quality article. Another RCT study with a meeting abstract,[22] which only presented data of cement leakage, did not describe blinding or other relevant information. Therefore, the study was judged as an unclear risk and a low-quality article. In the 5 cohort studies, NOS was used to assess the quality of literature, and studies that achieved 6 or more stars were considered high quality. Among these studies, 3 articles attained 7 stars,[18,20,23] and the others attained 6 stars.[17,21] Therefore, these articles were judged as high-quality studies because the information in these articles met the NOS criteria.
Cement leakage was presented in the 7 included studies. Among them, the locations of cement leakage were classified in 5 studies but were not classified in 2 studies. Based on the classification of the 5 studies, we divided the locations into the paravertebral area, the intraspinal space, the disc space, and the vein. If the same location of the leakage had different names, then the above classification was used. For instance, Wang et al[20] defined the epidural space as a location of leakage. We considered that the intraspinal space included the epidural space; therefore, it was classified as intraspinal space.
The pooled results indicated that compared with LVC, HVC was associated with a reduced incidence of cement leakage. In a retrospective study in which a total of 422 cases (221 were treated for osteoporosis and 201 for malignancy) with 846 vertebrae were treated with the application of HVC into the vertebral body, Rapan et al[30] confirmed that HVC combined with PVP minimized the risk of cement leakage. However, in another retrospective cohort study, 92% and 91% of patients had no to mild leakage in the PVP with HVC and PKP with LVC groups, respectively, and no significant differences were noted between the groups.[19] We believe that the bias was derived from the fact that PKP using LVC was used as a control for comparison. PKP technology consists of distraction using a balloon in the fractured vertebral body first followed by the injection of bone cement. Therefore, the pressure within the vertebral body is small, and leakage does not occur easily. In addition, a cadaver study based on a comparison of HVC and LVC revealed that cement leakage of the cortical, endplate, vessel, and canal did not significantly differ. A statistically significant difference between these procedures was only noted for less severe leakage through the endplates (P = .02) and a trend toward less severe extravasation through vessels (P = .06).[31]
Three important factors may influence the movement of cement into and out of the vertebral body.[32] Bone- and fracture-related parameters: Yeom et al[33] revealed that cortical fracture of the vertebral body is the main cause of leakage. Injection methods: Although the procedure has been standardized, accidental puncture of the endplate or the cortical of the vertebral body during surgery may result in cement leakage. Cement properties: Regarding the properties, the diffusion of cement within the vertebral body should be a “uniformly expanding cloud” rather than the “fingers of a glove,” which indicates that cement should uncontrollably spread due to lower resistance paths in the vertebral body.[34] HVC spreads more uniformly than LVC and therefore reduces the risk of leakage,[34] and these results were also confirmed by another in vitro experiment.[35] Another influential factor is the timing of the injection. The injection is very difficult when the LVC has already become extremely viscous. If the LVC is not yet viscous upon injection, the loose cement may easily diffuse and leak outside. However, HVC allows for a longer injection time and therefore an easier injection, which greatly reduces the probability of leakage caused by injection timing.
Our findings confirmed that the incidence of venous leakage for HVC was reduced when compared with that for LVC. This result was also confirmed by an in vitro experiment in which a correlation between cement viscosity and venous leakage was noted.[34] In addition, some researchers believed that vein embolism with a gelatin sponge within the vertebral body could effectively prevent venous leakage. However, this technique is more complex and increased the number of surgical procedures, resulting in some limitations in the clinical application.[36] Although some studies demonstrated that the main reason for the disc leakage was endplate fracture,[37] we considered that cement viscosity remains an important factor. The pressure difference between the inside and outside of the endplate fracture is larger based on the existence of the intervertebral disc. Thus, the lower viscosity cement would easily go through endplate fracture into the disc. However, this pressure difference was not obvious in both sides of the cortical fracture given the existence of a certain space outside of the fracture, such as intraspinal space. Thus, cement viscosity was not a major factor of leakage. These factors might explain why cement was easier to leak into the paravertebral area and intraspinal space, and a study confirmed that cement is likely to leak into these areas.[33]
Information regarding follow-up for the VAS and ODI was provided in 5[17,18,20,21,23] and 4[18,20,21,23] studies, respectively. We defined 1 to 3 months as short term and 6 to 12 months as long term based on the data presented in the studies.[38] The pooled results revealed no difference between HVC and LVC, indicating that cement viscosity did not affect the clinical effect. However, a significant difference was observed in the postoperative short-term follow-up for VAS possibly due to the small sample size. In addition, no difference in the injected cement volume was noted between the procedures, except PVP with HVC versus PKP with LVC. We considered that injected cement volume and cement viscosity were not directly related to the above difference but were related to surgical methods. In our series, no difference in adjacent vertebral fractures was noted between the groups (P = .50). Studies reported that adjacent vertebral fractures were mainly caused by disc leakage[39–41]; however, this is not a consistent finding.[42]
This meta-analysis had the following limitations that must be considered. First and foremost, our analysis included a number of cohort studies, which might result in selective and performance bias due to the absence of random allocation, allocation concealment, and blinding. The bias might cause statistical heterogeneity; however, high heterogeneity was not present in our meta-analysis. Second, only 2 RCTs met enrollment criteria, and the quality of 1 RCT included in a meeting abstract was quite low.
In summary, compared with LVC, HVC results in a reduced incidence of cement leakage for the treatment of vertebral compression fractures, especially in the disc space and peripheral vein but not in the intraspinal space or the paravertebral area. In addition, HVC yields the same satisfactory clinical effect as LVC.
5. Author contributions
Data curation: D-H. Liu, Y-H. Feng, C-L. Xie.
Formal analysis: H. Huang.
Methodology: H. Huang.
Project administration: F. Jiao.
Writing – review & editing: Z-F. Zhang.
Footnotes
Abbreviations: CI = confidence interval, HVC = high-viscosity cement, LVC = low-viscosity cement, MD = mean difference, NOS = Newcastle–Ottawa scale, ODI = Oswestry Disability Index, PKP = percutaneous kyphoplasty, PVP = percutaneous vertebroplasty, RCT = randomized controlled trial, RR = risk ratio, VAS = visual analog scale, VCF = vertebral compressive fracture.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Kim KW, Cho KJ, Kim SW, et al. A nation-wide, outpatient-based survey on the pain, disability, and satisfaction of patients with osteoporotic vertebral compression fractures. Asian Spine J 2013;7:301–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Venmans A, Klazen CA, Lohle PN, et al. Natural history of pain in patients with conservatively treated osteoporotic vertebral compression fractures: results from VERTOS II. AJNR Am J Neuroradiol 2012;33:519–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lee YK, Jang S, Jang S, et al. Mortality after vertebral fracture in Korea: analysis of the National Claim Registry. Osteoporos Int 2012;23:1859–65. [DOI] [PubMed] [Google Scholar]
- [4].Sakuma M, Endo N, Oinuma T, et al. Incidence of osteoporotic fractures in Sado, Japan in 2010. J Bone Miner Metab 2014;32:200–5. [DOI] [PubMed] [Google Scholar]
- [5].Yi X, Lu H, Tian F, et al. Recompression in new levels after percutaneous vertebroplasty and kyphoplasty compared with conservative treatment. Arch Orthop Trauma Surg 2014;134:21–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Evans AJ, Jensen ME, Kip KE, et al. Vertebral compression fractures: pain reduction and improvement in functional mobility after percutaneous polymethylmethacrylate vertebroplasty retrospective report of 245 cases. Radiology 2003;226:366–72. [DOI] [PubMed] [Google Scholar]
- [7].Watts NB, Harris ST, Genant HK. Treatment of painful osteoporotic vertebral fractures with percutaneous vertebroplasty or kyphoplasty. Osteoporos Int 2001;12:429–37. [DOI] [PubMed] [Google Scholar]
- [8].Venmans A, Klazen CA, van Rooij WJ, et al. Postprocedural CT for perivertebral cement leakage in percutaneous vertebroplasty is not necessary—results from VERTOS II. Neuroradiology 2011;53:19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurg 2003;98:21–30. [DOI] [PubMed] [Google Scholar]
- [10].Schmidt R, Cakir B, Mattes T, et al. Cement leakage during vertebroplasty: an underestimated problem? Eur Spine J 2005;14:466–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Majd ME, Farley S, Holt RT. Preliminary outcomes and efficacy of the first 360 consecutive kyphoplasties for the treatment of painful osteoporotic vertebral compression fractures. Spine J 2005;5:244–55. [DOI] [PubMed] [Google Scholar]
- [12].Padovani B, Kasriel O, Brunner P, et al. Pulmonary embolism caused by acrylic cement: a rare complication of percutaneous vertebroplasty. AJNR Am J Neuroradiol 1999;20:375–7. [PMC free article] [PubMed] [Google Scholar]
- [13].Hulme PA, Krebs J, Ferguson SJ, et al. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine (Phila Pa 1976) 2006;31:1983–2001. [DOI] [PubMed] [Google Scholar]
- [14].Chen HL, Wong CS, Ho ST, et al. A lethal pulmonary embolism during percutaneous vertebroplasty. Anesth Analg 2002;95:1060–2. [DOI] [PubMed] [Google Scholar]
- [15].Ruger M, Schmoelz W. Vertebroplasty with high-viscosity polymethylmethacrylate cement facilitates vertebral body restoration in vitro. Spine (Phila Pa 1976) 2009;34:2619–25. [DOI] [PubMed] [Google Scholar]
- [16].Zhang L, Wang J, Feng X, et al. A comparison of high viscosity bone cement and low viscosity bone cement vertebroplasty for severe osteoporotic vertebral compression fractures. Clin Neurol Neurosurg 2015;129:10–6. [DOI] [PubMed] [Google Scholar]
- [17].Rapan S, Jovanovic S, Gulan G, et al. Vertebroplasty—high viscosity cement versus low viscosity cement. Coll Antropol 2010;34:1063–7. [PubMed] [Google Scholar]
- [18].Sun K, Liu Y, Peng H, et al. A comparative study of high-viscosity cement percutaneous vertebroplasty vs. low-viscosity cement percutaneous kyphoplasty for treatment of osteoporotic vertebral compression fractures. J Huazhong Univ Sci Technol Med Sci 2016;36:389–94. [DOI] [PubMed] [Google Scholar]
- [19].Georgy BA. Clinical experience with high-viscosity cements for percutaneous vertebral body augmentation: occurrence, degree, and location of cement leakage compared with kyphoplasty. AJNR Am J Neuroradiol 2010;31:504–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wang CH, Ma JZ, Zhang CC, et al. Comparison of high-viscosity cement vertebroplasty and balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Pain Physician 2015;18:E187–94. [PubMed] [Google Scholar]
- [21].Anselmetti GC, Zoarski G, Manca A, et al. Percutaneous vertebroplasty and bone cement leakage: clinical experience with a new high-viscosity bone cement and delivery system for vertebral augmentation in benign and malignant compression fractures. Cardiovasc Intervent Radiol 2008;31:937–47. [DOI] [PubMed] [Google Scholar]
- [22].Wiese D, Alhashash M, Böhm H. Prospective randomised study about the influence of bone cement viscosity on cement leakage comparing high with low viscosity bone cement in thoracolumbar osteoporotic vertebral fractures treated with percutaneous vertebroplasty. Eur Spine J 2010;19:1994. [Google Scholar]
- [23].Zhang Z, Yang J, Jiang H, et al. An update comparison of high-viscosity cement and low-viscosity cement vertebroplasty in the treatment of osteoporotic thoracolumbar vertebral compression fractures. Int J Surg 2017;43:126–30. [DOI] [PubMed] [Google Scholar]
- [24].Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Int J Surg 2014;12:1500–24. [DOI] [PubMed] [Google Scholar]
- [25].Nagar VR, Birthi P, Grider JS, et al. Systematic review of radiofrequency ablation and pulsed radiofrequency for management of cervicogenic headache. Pain Physician 2015;18:109–30. [PubMed] [Google Scholar]
- [26].Furlan AD, Malmivaara A, Chou R, et al. 2015 Updated method guideline for systematic reviews in the Cochrane back and neck group. Spine (Phila Pa 1976) 2015;40:1660–73. [DOI] [PubMed] [Google Scholar]
- [27].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [28].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. Bmj 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated September 2008]. 2008. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/375/CN-00871375/frame.html. Accessed August 8, 2017. [Google Scholar]
- [30].Rapan S, Krnic K, Rapan V, et al. Application of high viscosity bone cement in vertebroplasty for treatment of painful vertebral body fracture. Med Glas (Zenica) 2016;13:148–53. [DOI] [PubMed] [Google Scholar]
- [31].Lador R, Liberman S, Ben-Galim P, et al. A cadaver study to compare vertebral augmentation with a high-viscosity cement to augmentation with conventional lower-viscosity cement. J Spinal Disord Tech 2013;26:68–73. [DOI] [PubMed] [Google Scholar]
- [32].Loeffel M, Ferguson SJ, Nolte LP, et al. Vertebroplasty: experimental characterization of polymethylmethacrylate bone cement spreading as a function of viscosity, bone porosity, and flow rate. Spine (Phila Pa 1976) 2008;33:1352–9. [DOI] [PubMed] [Google Scholar]
- [33].Yeom JS, Kim WJ, Choy WS, et al. Leakage of cement in percutaneous transpedicular vertebroplasty for painful osteoporotic compression fractures. J Bone Joint Surg Br 2003;85:83–9. [DOI] [PubMed] [Google Scholar]
- [34].Baroud G, Crookshank M, Bohner M. High-viscosity cement significantly enhances uniformity of cement filling in vertebroplasty: an experimental model and study on cement leakage. Spine (Phila Pa 1976) 2006;31:2562–8. [DOI] [PubMed] [Google Scholar]
- [35].Habib M, Serhan H, Marchek C, et al. Cement leakage and filling pattern study of low viscous vertebroplastic versus high viscous confidence cement. SAS J 2010;4:26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Bhatia C, Barzilay Y, Krishna M, et al. Cement leakage in percutaneous vertebroplasty: effect of preinjection gelfoam embolization. Spine (Phila Pa 1976) 2006;31:915–9. [DOI] [PubMed] [Google Scholar]
- [37].Tanigawa N, Kariya S, Komemushi A, et al. Cement leakage in percutaneous vertebroplasty for osteoporotic compression fractures with or without intravertebral clefts. AJR Am J Roentgenol 2009;193:W442–5. [DOI] [PubMed] [Google Scholar]
- [38].Wang H, Sribastav SS, Ye F, et al. Comparison of percutaneous vertebroplasty and balloon kyphoplasty for the treatment of single level vertebral compression fractures: a meta-analysis of the literature. Pain Physician 2015;18:209–22. [PubMed] [Google Scholar]
- [39].Chen WJ, Kao YH, Yang SC, et al. Impact of cement leakage into disks on the development of adjacent vertebral compression fractures. J Spinal Disord Tech 2010;23:35–9. [DOI] [PubMed] [Google Scholar]
- [40].Ahn Y, Lee JH, Lee HY, et al. Predictive factors for subsequent vertebral fracture after percutaneous vertebroplasty. J Neurosurg Spine 2008;9:129–36. [DOI] [PubMed] [Google Scholar]
- [41].Lin EP, Ekholm S, Hiwatashi A, et al. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol 2004;25:175–80. [PMC free article] [PubMed] [Google Scholar]
- [42].Syed MI, Patel NA, Jan S, et al. Intradiskal extravasation with low-volume cement filling in percutaneous vertebroplasty. AJNR Am J Neuroradiol 2005;26:2397–401. [PMC free article] [PubMed] [Google Scholar]


