Abstract
The objective of this study is to estimate the reference values for the lower limb peripheral nerves in adults.
The demographics and physical characteristics of 69 adult healthy volunteers were evaluated and recorded. The estimated reference values and their correlations with the age, weight, height, body mass index (BMI) were evaluated.
The cross sectional area reference values were obtained at 5 predetermined sites for 3 important lower limb peripheral nerves. Our CSA values correlated significantly with age, weight, and BMI. The normal reference values for each nerve were as follows: Tibial nerve at the popliteal fossa 19 mm2 ± 6.9, tibial nerve at the level of the medial malleolus 12.7 mm2 ± 4.5, common peroneal nerve at the popliteal fossa 9.5 mm2 ± 4, common peroneal nerve fibular head 8.9 mm2 ± 3.2, sural nerve 3.5 mm2 ± 1.4.
The reference values for the lower limb peripheral nerves were identified. These values could be used for future management of peripheral nerve disorders.
Keywords: lower limb, peripheral nerve, reference values, ultrasound
1. Introduction
In the last 10 years, modern high-resolution ultrasound has gained more popularity in the diagnosis of diseases related to the peripheral nervous system. Peripheral nerve sonography emerged as an efficient imaging diagnostic tool, beside electromyography and nerve conduction studies. This was supported by its cheap price, dynamic ability, and ability to examine the whole course of the nerve, together with the contra-lateral side at the same time. Ultrasound is also well tolerated by patients due to its simplicity and noninvasive quick nature. Utilization of peripheral nerve sonography still needs more knowledge about its full capabilities, and to draw attention toward its side compared with magnetic resonance imaging.
Currently, the cross sectional area (CSA) of a peripheral nerve is the most accepted parameter as a reference for the size of a specific nerve, where increased CSA notifies pathology. In addition to traumatic injuries, a high demand for advanced high resolution imaging tool is increasing, such as entrapment disorders, inherited neuromuscular disorders, and immune-mediated neuropathies. Reference values are critical for differentiating normal from different inherited and acquired pathologies.[1–3]
The CSA reference values for lower limb peripheral nerves were studied, in several research projects, either as part of a study for the whole body peripheral nerves,[4–8] or as a study for the lower limb nerves,[9,10] or as a single nerve.[11] Visualization of the lower limb peripheral nerves is usually more difficult than upper limb nerves likely due to their deep location and more complex anatomy.[3] The aim of this study is to establish normal CSA reference values for selected lower limb peripheral nerves, in healthy subjects.
2. Methods
2.1. Participants
The current study is a cross-sectional case control study conducted at a university hospital. The study protocol and patients’ informed consent were approved by the institutional review boards. The study was conducted in accordance with the Declaration of Helsinki and was consistent with the international conference on harmonization and good clinical practice. Each patient signed a written informed consent before enrollment and before any study-related procedure.
Sixty-nine healthy adult volunteers all of them from the Asian population, 20 to 70 years old, were recruited from October 2015 to May 2016, at a university hospital. For each participant, the age, height, weight, and body mass index (BMI) were recorded before ultrasound scanning. Neuromuscular diseases and other systemic diseases that may affect the peripheral nerves were excluded by history, clinical examination, and appropriate investigations.
2.2. Technique
The ultrasound scanning of the scanned nerves was carried out using Philips ultrasound diagnostic scanner, (Epic 7 version 1.5, Ultrasound system: Philips, Bothell, WA) using a L18-5 MHZ linear transducer. An experienced radiologist (MAB), with 10 years experience in neuromuscular ultrasound, performed all ultrasound scans and another examiner (Dr Ahmed Abodonya), with 3 year experience in neurosonography reviewed the images for diagnostic image quality. Each examination was performed bilaterally and for 3 times to assess for intrarater reliability. To minimize anisotropy, the probe was positioned in a perpendicular position to the nerve. Minimal pressure was exerted on the probe to optimize image quality. In each subject 5 sites were scanned [10 bilaterally].
Based on anatomic landmarks, the CSA was measured in the following sites: The first site is for the tibial nerve at the posterior aspect of the popliteal fossa, after division from the sciatic nerve, posterior to the popliteal vessels. Second site is for the tibial nerve posterior to the medial malleolus in relation to the posterior artery and vein. The third site is for the common peroneal nerve at the popliteal fossa, where it lies lateral to the tibial nerve in the popliteal fossa. The fourth site is for the common peroneal nerve lateral to the fibular head. The fifth site is for the sural nerve at the lateral aspect of the distal leg, lateral to the lesser saphenous vein (Fig. 1). The power and color Doppler modes were used to properly identify nerves at their sites (Figs. 2–6).
Figure 1.
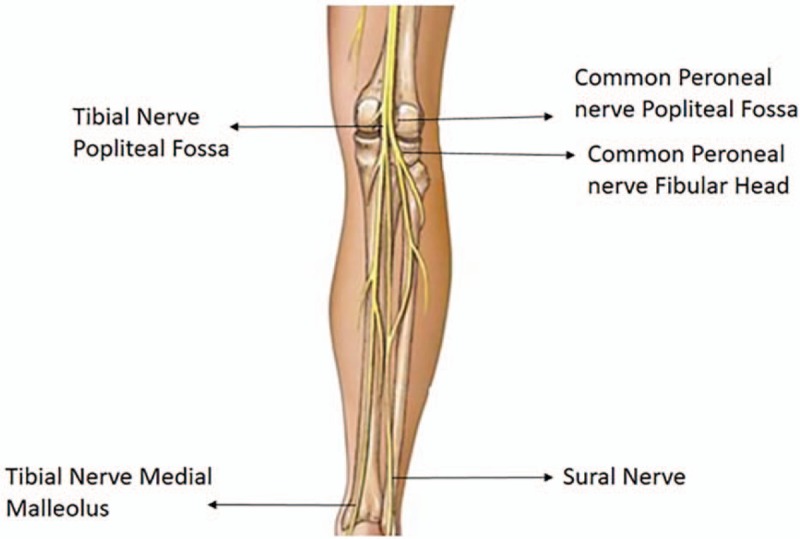
Anatomical landmarks used for obtaining CSA measurements for the lower limb nerves at our study. CSA = cross-sectional area.
Figure 2.
Short axis scan of the tibial nerve at the popliteal fossa related to the popliteal vessels.
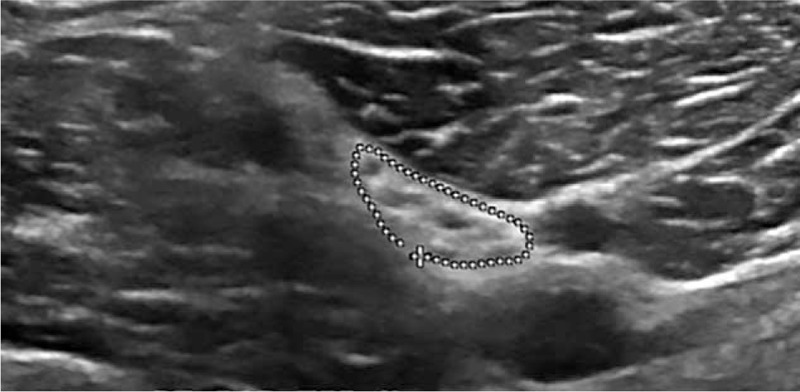
Figure 6.
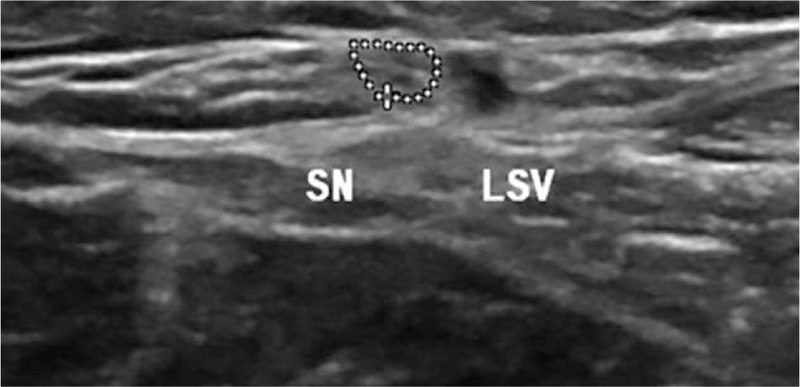
Short axis scan of the sural nerve at the distal leg lateral to the lesser saphenous vein.
Figure 3.

Short axis scan of the tibial nerve at the level of the medial malleolus.
Figure 4.

Short axis scan of the common fibular nerve at the popliteal fossa.
Figure 5.

Short axis scan of the common fibular nerve level of the fibular head.
2.3. Statistical analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 21 software (SPSS Inc, Chicago, IL). All data were presented as mean ± standard deviation (SD) and range. The mean CSA were compared between both the sides using the Wilcoxon signed rank test. The correlations between the CSA of the scanned nerves; age, weight, height and BMI were evaluated using Pearson correlation coefficient (r). A P value of < .05 was considered significant.
3. Results
During the recruitment period we studied 69 healthy adult volunteers with a mean age of 38.33 ± 12.13 years (range: 20–73). The mean height was 161.48 ± 9.8 (range 144–183) and weight 77.14 ± 18.4 (range 44–128). Table 1 shows different descriptive statistics, mean reference values of the scanned nerves together with their reference range. Table 2 shows correlations between age, weight height, and BMI, and CSA reference values of the lower limb nerves. The interrater reliability calculations showed an overall intraclass correlation coefficient of 0.81. We compared the CSA values of the 5 scanned sites at the right and left sides, no significant differences were noted. No significant statistical gender specific could be noted at our study. Significant positive statistical correlation with age is noted at all the scanned nerves except for the sural nerve. Significant positive statistical correlation with weight and BMI was noted. No significant statistical correlation was noted in relation to height. The normal reference values for each nerve were as follows: Tibial nerve at the popliteal fossa 19 mm2 ± 6.9, tibial nerve at the level of the medial malleolus 12.7 mm2 ± 4.5, common peroneal nerve at the popliteal fossa 9.5 mm2 ± 4, common peroneal nerve fibular head 8.9 mm2 ± 3.2, sural nerve 3.5 mm2 ± 1.4.
Table 1.
Descriptive statistics, mean reference values of the scanned nerves together with their reference range.
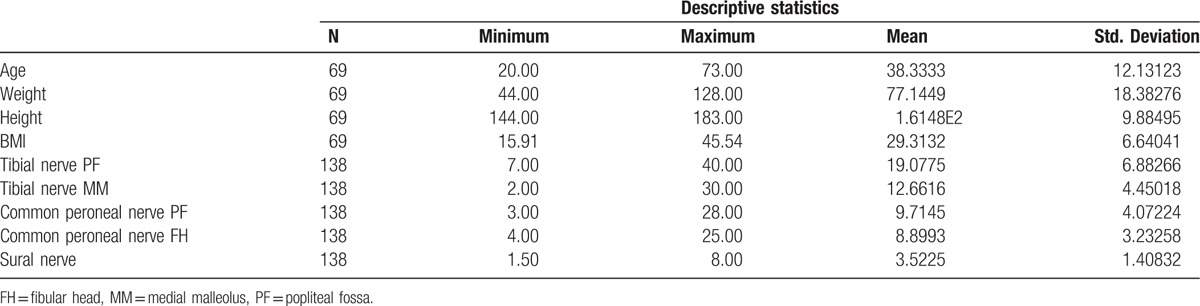
Table 2.
Correlations between age, weight height, and BMI, and CSA reference values of the lower limb nerves.

4. Discussion
Comparing our results with Qrimli et al,[4] slight differences were noted for the sural and common peroneal nerves, with similar noted for the tibial nerve at the medial malleolus. As for Seok et al study,[10] our results showed slight difference for the common peroneal nerve in both sites, similar results for the tibial nerve at the medial malleolus, some difference for the tibial nerve in the popliteal fossa, and slight difference for the sural nerve. Compared with the Kerasnoudis et al study,[7] significant difference was observed for the tibial nerve at both the sites. Comparable results were noted for both the sites of the common peroneal nerve, and for the sural nerve. As for the Boehm et al study,[5] slight difference was observed for the tibial nerve at the medial malleolus and the sural nerve. Similar values were obtained for the common peroneal nerve at the fibular head. Compared with the Cartwright et al study,[8] significant difference was noted for the tibial nerve at the popliteal fossa, slight differences for the tibial nerve at the medial malleolus, common peroneal nerve and sural nerve. Considering demographic factors, our results were very similar to the Qrimli et al study,[4] different from the study of the Tagliafico et al study,[9] regarding height, and coinciding with the Seok et al study,[10] regarding weight and BMI. In general, we obtained the CSA reference values for 5 important sites of 3 lower limb peripheral nerves, our results correlated positively with weight, BMI, and age, whereas no significant statistical correlation could be noted with height and gender. The results obtained in this study could be useful in the diagnosis of different inherited and acquired pathologies of lower limb peripheral nerves, such as tarsal tunnel syndrome.,[12] however, other diseases such as charcot Marie tooth need additional study of the upper limb nerves in addition to lower limb nerves by high-resolution ultrasound to obtain more informative study.[13] We recommend standardized protocol with fixed predetermined sites for the examination of the lower limb peripheral nerves, as an important future need, in addition to clinical and neurophysiologic assessment.
4.1. Study limitations
The present study has some limitations. It did not include smaller nerves such as lateral cutaneous femoral nerve, saphenous and obturator nerves. Also intranerve CSA variability was not included.
5. Author contributions
Conceptualization: M.A. Bedewi, M. Kotb, S. Kamal, G. Mahmoud, K. Aldossari, S. Swify.
Data curation: M.A. Bedewi, S. Kamal, G. Mahmoud, K. Aldossari, A. Alqabbani.
Formal analysis: M.A. Bedewi, A. Abodonya.
Investigation: M.A. Bedewi, M. Kotb, S. Kamal, G. Mahmoud.
Methodology: M.A. Bedewi, A. Abodonya, M. Kotb, S. Kamal, G. Mahmoud.
Project administration: M.A. Bedewi, M. Kotb, S. Swify.
Resources: M.A. Bedewi, K. Aldossari, S. Swify.
Software: M.A. Bedewi, A. Alqabbani.
Supervision: M.A. Bedewi, M. Kotb, S. Kamal, K. Aldossari, S. Swify.
Validation: M.A. Bedewi, G. Mahmoud, A. Alqabbani, S. Swify.
Visualization: M.A. Bedewi, M. Kotb, S. Kamal.
Writing – original draft: M.A. Bedewi, A. Alqabbani.
Writing – review & editing: M.A. Bedewi, M. Kotb, S. Kamal.
Acknowledgment
The authors are grateful to the Deanship of Scientific Research at Prince Sattam bin Abdulaziz University.
Footnotes
Abbreviations: BMI = body mass index, CSA = cross-sectional area.
The authors have no conflicts of interest to disclose.
References
- [1].Padua L, Hobson-Webb LD. Ultrasound as the first choice for peripheral nerve imaging? Neurology 2013;80:1626–7. [DOI] [PubMed] [Google Scholar]
- [2].Tagliafico AS. Peripheral nerve imaging: not only cross-sectional area. World J Radiol 2016;8:726–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Beekman R, Visser LH. High-resolution sonography of the peripheral nervous system—a review of the literature. Eur J Neurol 2004;11:305–14. [DOI] [PubMed] [Google Scholar]
- [4].Qrimli M, Ebadi H, Breiner A, et al. Reference values for ultrasonograpy of peripheral nerves. Muscle Nerve 2016;53:538–44. [DOI] [PubMed] [Google Scholar]
- [5].Böhm J, Scheidl E, Bereczki D, et al. High-resolution ultrasonography of peripheral nerves: measurements on 14 nerve segments in 56 healthy subjects and reliability assessments. Ultraschall in der Medizin 2014;35:459–67. [DOI] [PubMed] [Google Scholar]
- [6].Rasenack M, Décard BF, Schädelin S, et al. Ultrasonographic reference values for peripheral nerves and nerve roots in the normal population of children and adolescents: study protocol for an observational-prospective trial. BMJ Open 2016;6:e014662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kerasnoudis A, Pitarokoili K, Behrendt V, et al. Cross sectional area reference values for sonography of peripheral nerves and brachial plexus. Clin Neurophysiol 2013;124:1881–8. [DOI] [PubMed] [Google Scholar]
- [8].Cartwright MS, Passmore LV, Yoon JS, et al. Cross-sectional area reference values for nerve ultrasonography. Muscle Nerve 2008;37:566–71. [DOI] [PubMed] [Google Scholar]
- [9].Tagliafico A, Cadoni A, Fisci E, et al. Reliability of side-to-side ultrasound cross-sectional area measurements of lower extremity nerves in healthy subjects. Muscle Nerve 2012;46:717. [DOI] [PubMed] [Google Scholar]
- [10].Seok HY, Jang JH, Won SJ, et al. Cross-sectional area reference values of nerves in the lower extremities using ultrasonography. Muscle Nerve 2014;50:564–70. [DOI] [PubMed] [Google Scholar]
- [11].Kim JY, Song S, Park HJ, et al. Diagnostic cutoff value for ultrasonography of the common fibular neuropathy at the fibular head. Ann Rehabil Med 2016;40:1057–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Doneddu PE, Coraci D, Loreti C, et al. Tarsal tunnel syndrome: still more opinions than evidence. Status of the art. Neurol Sci 2017;38:1735–9. [DOI] [PubMed] [Google Scholar]
- [13].Padua L, Coraci D, Lucchetta M, et al. Different nerve ultrasound patterns in charcot-marie-tooth types and hereditary neuropathy with liability to pressure palsies. Muscle Nerve 2018;57:E18–23. [DOI] [PubMed] [Google Scholar]


