Abstract
Background:
Chronic pelvic inflammation disease (PID) is a difficult-to-treat gynecological disorder with complex etiologies. Acupuncture has been applied widely for treating chronic pelvic inflammation or chronic pelvic pain symptoms in China. The aim of this review is to undertake a systematic review to estimate the effectiveness and safety of acupuncture on chronic PID.
Methods:
A literature search will be conducted electronically with date up to October 2018 in MEDLINE, Cochrane Library, EBASE, and CNKI databases, using combination subject terms of chronic pelvic pain (or chronic pelvic inflammation, and chronic pelvic pain symptoms, etc.) and acupuncture related treatment. Also duplicates will be removed. The primary outcomes consisted of improvement rate and pain relief. Secondary outcomes include the recurrence rate and side effects, such as pneumothorax, bleeding, serious discomfort, subcutaneous nodules, and infection. Systematic reviews and databases will be searched for randomized controlled trials on acupuncture for chronic PID with acupuncture treatment will be included. Cochrane RevMan V5.3.5 risk of bias assessment tool will be implemented for risk of bias evaluation, data synthesis, meta-analyses, and subgroup analysis while condition is met. Mean difference (MD), standard mean difference (SMD), and dichotomous data will be used to present continuous outcomes.
Results:
This study will generate a comprehensive review of current evidence of acupuncture for chronic pelvic inflammation diseases.
Conclusion:
The study will provide updated evidence to evaluate the effectiveness and side effects of acupuncture for chronic pelvic inflammation disease.
PROSPERO registration number:
CRD42018087950.
Keywords: acupuncture, chronic pelvic inflammation disease, chronic pelvic pain, depression, protocol, systematic review
1. Introduction
1.1. Description of the condition
Chronic pelvic inflammatory disease (PID)[1–3] is common dysfunction characterized by lower urinary tract symptoms and abdominal pain. It is easy to relapse after treatment, and up to one-third of women with PID[4] could develop chronic pelvic pain. In China, chronic PID is also a common disease in traditional Chinese medicine (TCM) gynecological clinic, accounting for 20% of all outpatient appointments in women's health services.[5] Moreover, estimated 4% to 20% of women between the ages of 15 and 50 experience chronic pelvic inflammatory disease (CPID).[6] In the United States, PID is estimated to occur in over 750,000 US women annually and generates annual costs of around US$4.2 billion[7] for healthcare.
About 25% of women with PID will experience long-term sequelae,[8] including annexitis, irregular menstrual, infertility, ectopic pregnancy, or chronic pelvic pain. Further, women suffering from PID have a 6 to 8 risk of infertility.[9]
According to the US Centers for Disease Control and Prevention (CDC) guidelines,[10,11] PID is a clinical condition involves infection of microorganisms from reproductive system to contiguous tissues. It also comprises complicated inflammation of annexitis[12], salpingitis[13], and pelvic peritonitis.[14] Therefore, diagnosis of PID requires a careful analysis of the history and a thorough medical examination. Most cases of PID result from incomplete and delayed treatments of acute pelvic inflammation. The etiological factors may include polymicrobial infection, pelvic musculoskeletal disorders, and psychoneurological causes.[15] According to a GP's guide to PID,[16] the effective diagnostic method is laparoscopy, which shows inflamed fallopian tubes in PID. In clinic, PID should be suspected when low abdominal pain is associated with adnexal or uterine pain. In this case, pelvic ultrasonography is necessary to exclude ovarian abscess.[17] Microbiological diagnosis involves vaginal and endocervical sampling for bacteriological analysis. And the presence of many poly-microbe supports a diagnosis of reproductive system infection.[18] In general, sexually acquired chlamydia trachomatis and Neisseria gonorrhoeae[19] are common causes. The infection and inflammation of the reproductive organs (the uterus, fallopian tubes, and ovaries) can then transmit to lower genital tract structure.[20] Untreated PID[21] can lead to serious consequences including irregular menstruation, tubal occlusion infertility, pelvic adhesion syndrome, pelvic congestion syndrome, abscess formation, etc.
Meanwhile, many cases of PID are reported as functional or psychosomatic disorders.[22] And the cause has never been found. Although presentations vary according to the cause and severity of the disease, it is commonly characterized by noncyclical abdominal pain, dysmenorrhea, lumbosacral pain, and lingering leucorrhea, etc.[23]
Although the etiology and pathogenesis are still unclear, many clinical practice guidelines have been developed worldwide. The International Union against Sexually Transmitted Infections (IUSTI) and the CDC has recommended antibiotic therapies,[24] which cover Chlamydia trachomatis, Neisseria gonorrhoeae, and anaerobic bacteria, administered intravenously, intramuscularly, or orally. However, PID is polymicrobial in etiology.[25] So a disadvantage of this strategy is technical problems that limit the possibility of specific bacteria culture from deep pelvic infections. Although broad-spectrum combination antimicrobial therapy is recommended, uncertainties regarding the effectiveness of antimicrobial therapy exist. Further, there has been accumulating evidence that antibiotics potentially have a number of undesired side effects including gastrointestinal disorders, cutaneous reactions, the potential severity of hepatic side effects and it can produce resistant variants[26]; for surgery, patients with PID are not routinely referred for physical therapy until the condition is found to be resistant to antibiotic therapy.[27] Meanwhile, surgical operations have been reported of little benefit, and indications for surgery should be carefully considered to avoid iatrogenic damage in uterus; for other routine therapies of tranquilizers and hormone, they can only relieve symptoms for short term and lack of long-term follow-up.[28]
Obviously, although therapies of antibiotics, surgery, and hormone have been tested to be effective in short term, full evaluation of recurrent rate and the risks of long-term squeal is not available. In general, current medical treatment cannot give permanent therapeutic effects for chronic PID.[29] As a result, the patient may suffer from repeated attacks, making the disease intractable.
1.2. Description of the intervention
Considering the side reaction in antibiotics and the high risk and narrow use of surgery, more clinicians have applied complementary and alternative therapy including TCM to cure chronic pelvic inflammation disease.[30,31]
Acupuncture has been widely used in Chinese clinical practice. It uses very fine needles to stimulate specified acupuncture points. If qualified acupuncturists perform it properly, acupuncture is a safe treatment without any side effects. Acupuncture is used to treat a range of conditions, such as myofacial pain, muscle disorders, and neurological disorders.[32,33]
A study showed there were 1088 articles of chronic PID using TCM in CNKI database by 2012, and most of the methods were herbs and acupuncture.[34–37]
1.3. How the intervention might work?
Acupuncture provides overall coordination, helping to achieve the state of relative equilibrium of body and mind. Guided by the TCM theory of differential diagnosis and treatment,[38,39] we believe chronic pelvic inflammation is mostly caused by invasion of pathogenic heat or dampness and blood circulation disorder leading to lower abdominal pain and other symptoms. Acupuncture is reported to invigorate blood circulation, relieve pain, prevent and treat hemorheologic disorder.[40,41]
1.4. Why it is important to conduct this review?
Characterized by easy operation, durable and strong stimulation, and long interval between each treatment, acupuncture has been broadly used to treat chronic pelvic inflammation.[42–44] It is an easy applicable method without side effect in long-term sequel. The needle can work as an effective painkiller, invigorate the channel-qi, remove the tissues, and generate the new.[45,46] Despite lack of effectiveness evaluated and normative management plan, most Chinese TCM hospitals have conducted acupuncture to treat chronic PID based on their own experience. To estimate the safety and effect appeared to be especially important, and it is also necessary to provide a treatment suggestion based on current evidences.
1.5. Objectives
The primary aims of this systematic review are to estimate the effectiveness and safety of acupuncture on chronic PID and formulate a treatment suggestion. We will focus on treating the pain itself and the underlying cause. Combination of drug therapy with medications with different mechanisms of action may improve therapeutic results.
2. Methods
2.1. Study registration
PROSPERO registration number is CRD42018087950. This protocol report is structured according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols (PRISMA-P) statement guidelines.[47]
2.2. Inclusion criteria for study selection
2.2.1. Types of study
To evaluate the curative effects of acupuncture on chronic PID, this review is confined to RCTs comparing acupuncture with a control group, which contained drug, no treatment, placebo, diet and exercise therapy, and other types of acupuncture including fine needles, fire needling, electronic needling, ear auricular pressure treatment, acupoint pressure, and so forth. It is deemed a randomized study if the trial stated the “randomization” phrase, and the blinding is not restricted. Besides, Chinese and English publications are the limitation of language. The animal mechanism studies, case reports, self-pre- and postcontrol, or non-RCTs are excluded.
2.2.2. Types of participants
It included the participants with no limitation of age, type of chronic PID, including specified and unknown causes. The definitions of chronic pelvic inflammation disease or chronic pelvic pain, or chronic abdominal disorder are included. Patients with acute medical conditions or pregnancy are excluded.
2.2.3. Types of intervention
The review comprises clinical trials with the treatment of acupuncture. We will study the types of acupuncture including fine needle, floating needle, electro-acupuncture, let bleeding, acupoint injection, fire needle, needle knife, and acupressure. Studies to compare the effect of different acupuncture therapies will be excluded.
2.2.4. Types of outcome measures
The primary outcomes consisted of improvement rate and pain relief. Secondary outcomes include the recurrence rate and side effects, such as pneumothorax, bleeding, serious discomfort, subcutaneous nodules, and infection. Systematic review and will be performed independently.
2.3. Data sources
A literature search will be conducted up to October 2018 in the databases of MEDLINE, Cochrane Library, EBSCO, Web of Science, EBASE, Springer, WHO International Clinical Trials Registry Platform (ICTRP), CNKI, Wanfang, CBM, and VIP. The item of RCT is also chosen in the corresponding databases in the languages of Chinese and English.
2.4. Search strategy
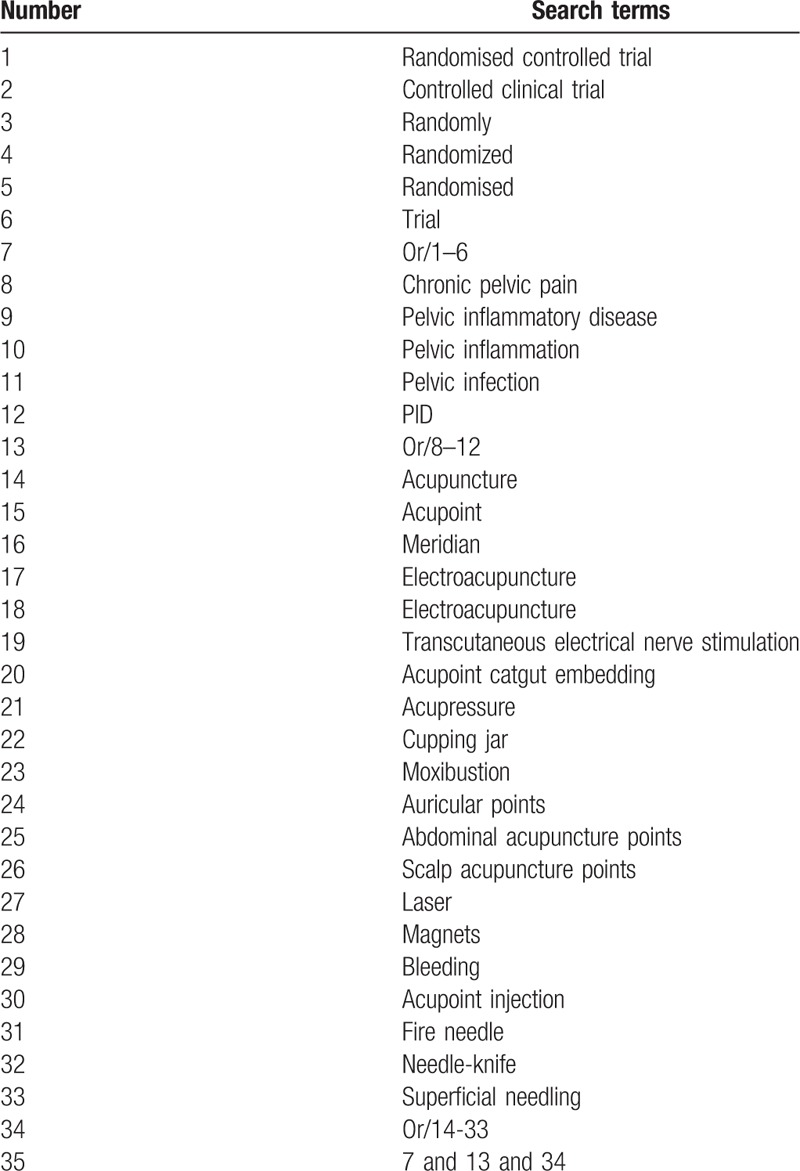
The following search keyword or combination subject terms are used: RCT (controlled clinical trial); acupuncture (e.g., “acupuncture” or “body acupuncture” or “scalp acupuncture” or “manual acupuncture” or “auricular acupuncture”, and “electro- acupuncture” or “fire needling”; chronic pelvic inflammation disease; chronic pelvic pain (e.g., “chronic pelvic pain” or “chronic pelvic ache” or “chronic pelvic disorder” and “chronic pelvic illness”); and chronic abdominal disorder. For Chinese databases, these searching terms will be accurately translated. The search strategies for Medline are summarized in Table 1.
Table 1.
Medline search strategy.
2.5. Data collection and analysis
2.5.1. Selection of studies
Each literature of title and abstract is scanned by 2 reviewers (YC and YCY) who have been trained and gained certifications in Chinese Cochrane Centre. All relevant articles of full text are investigated. When the 2 reviewers cannot agree on the selection process through consultations, the third reviewer (TPG) will ultimately make the decision. The primary selection process is shown in a PRISMA flow chart (Fig. 1)
Figure 1.
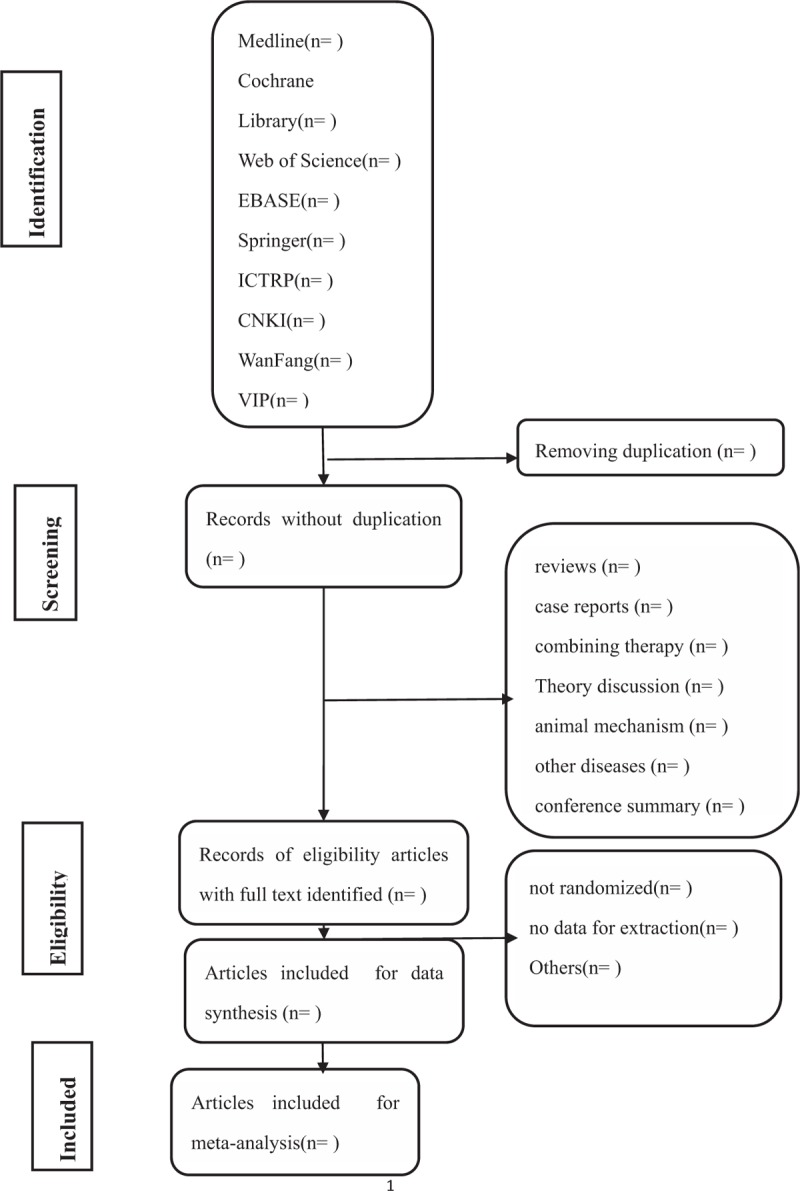
Flow diagram of studies identified.
2.5.2. Data extraction and management
The extracted information includes descriptions of studies, characteristics of participants, interventions of both the observation group and control group, quality, randomization, allocation concealment and blinding methods, outcome measures, main outcomes, adverse effects, duration of follow-up, type and source of financial support, and the Standards for Reporting Interventions in Controlled Trials of Acupuncture (STRICTA) checklist.
2.5.3. Assessment of risk of bias and reporting of study quality
Risk of bias is used to evaluate the quality of study with the Cochrane Collaboration's risk-of-bias assessment method and complete the STRICTA checklist for the included studies. The decision of risk is made by 2 reviewers (YHJ and NX). If inconsistent results appear, the final decisions will be made by the third author (TPG). For missing or ambiguous data, we will try to contact the author as possible, and for duplicate publication we only select the original.
2.5.4. Measures of treatment effect
Mean differences (MDs) with 95% confidence intervals (95% CIs) will be used to analyze continuous data. Other forms of data will be changed into MD values. Risk ratio with 95% CIs will be used to analyze dichotomous data. If significant heterogeneity is detected, a random-effects model will be used.
2.5.5. Unit of analysis issues
The analysis will focus on patients in randomized studies. If more than one acupuncture objective is used, we will conduct separate multiple meta-analyses for each treatment objective. If multiple nonacupuncture control groups are included, pooled analyses of the control groups against the intervention group will be used.
2.5.6. Management of missing data
If there are missing or incomplete data for the primary results, we will contact the corresponding authors for the missing data. If the missing data cannot be obtained, it will be excluded from analysis.
2.5.7. Assessment of heterogeneity
Review Manager (version 5.1, the Nordic Cochrane Centre, Copenhagen, Denmark) is applied to assess curative effect and publication bias. Forest plot is used to illustrate the relative strength of curative effect. Meanwhile, the funnel plot will picture the publication bias visually as the number of trials is more than 10. If significant heterogeneity is detected, a random-effects model will be used.
2.5.8. Assessment of reporting biases
If more than 10 trials are included, funnel plots will be used to assess reporting biases. If funnel plot asymmetry is detected, the reasons will be analyzed.
2.5.9. Data synthesis
We will use RevMan for all statistical analyses. If considerable heterogeneity is observed, a random-effects model with 95% CIs will be used to analyze pooled effect estimates. If necessary, subgroup analysis will be performed with careful consideration of each subgroup.
2.5.10. Subgroup analysis
A subgroup analysis will be performed according to control intervention and different outcomes.
2.5.11. Sensitivity analysis
A sensitivity analysis will be performed according to the following criteria: sample size, heterogeneity qualities, and statistical model (random-effects or fixed-effects model).
3. Discussion
Chronic PID comprises symptoms of pain and disorders in the lower abdomen (uterus, ovaries, fallopian tubes, and cervix). Sequelae may include fever, irregular menstruation, sterility, immunological dysfunction, and mental disorders.[48]
Potential etiologies for chronic PID may vary[49] individually. Proved causes include polymicrobial infection, nonbacterial infection, autoimmunity, and pelvic floor muscle dysfunction. And many cases are diagnosed with unknown pathogen.
Having the effect of promoting metabolism circulation, balancing, improving immunity, purifying meridian, and harmonizing qi and blood,[50,51] traditional Chinese acupuncture has shown to be effective and safe with potent operability, low cost, and, safety, especially suitable for chronic PID results from nonbacterial infection, autoimmunity, neurological dysfunction and pelvic floor muscle dysfunction and with unknown causes. Many chronic PID cases are reported with the clinical diagnosis of blood circulation problem in different degree. Acupuncture has been proved to stimulate blood circulation, improve permeability of the cellular membranes, and accelerate absorption of inflammation.[50] Therefore, it can be used to treat chronic and refractory pelvic disorders.[51]
A present review suggests that a significantly positive benefit is obtained from the administration of acupuncture therapy.[52] The use of acupuncture for symptoms of chronic PID symptoms should be considered, although further evidence from placebo controlled RCTs is required.
According to Cochrane method, this research is based on the existing clinical RCT evidence analysis at home and abroad, retrieving and screening the main electronic literature database with evidence of evidence-based medicine, to better guide clinical practice.
Author contributions
Conceptualization: T. Guo, N. Xu, T. Guo, Y. Chen.
Methodology: N. Xu, Y. Yuan.
Software: T. Guo.
Supervision: T. Guo.
Validation: T. Guo, Y. Jin.
Writing – original draft: T. Guo, Y. Chen, Y. Yuan.
Footnotes
Abbreviations: CDC = Centers for Disease Control and Prevention, CNKI= China National Knowledge Infrastructure, ICTRP = International Clinical Trials Registry Platform, IUSTI = The International Union against Sexually Transmitted Infections, MD = mean difference, NRS = numerical rating scale, PID = pelvic inflammation disease, PRISMA-P = Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocols, RCTs = randomized controlled trials, standard and ideal search, SMD = standard mean difference, STRICTA = the Standards for Reporting Interventions in Controlled Trials of Acupuncture, TCM = traditional Chinese medicine, WHO = World Health Organization.
Ethics and dissemination: There is no requirement of ethical approval and it will be in print or disseminated by electronic copies.
YC and YY are the first co-author to this paper.
This paper is funded by Yunnan province experts academician workstation—Liang Fanrong experts workstation project (No.: 2017-3), and Yunnan Provincial Science and Technology Department—Applied Basic Research Joint Special Funds of Yunnan University of Traditional Chinese Medicine (No.: 2017FF117-011).
The authors have no conflicts of interest to disclose.
References
- [1].Nickel JC, Freedland SJ, Castro-Santamaria R, et al. Chronic prostate inflammation predicts symptom progression in chronic prostatitis/chronic pelvic pain (CP/CPPS) patients. J Urol 2017;198:122–8. [DOI] [PubMed] [Google Scholar]
- [2].Chung SD, Chang CH, Hung PH, et al. Correlation between bladder pain syndrome/interstitial cystitis and pelvic inflammatory disease. Medicine 2015;94:e1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Greydanus DE, Dodich C. Pelvic inflammatory disease in the adolescent: a poignant, perplexing, potentially preventable problem for patients and physicians. Curr Opin Pediatr 2015;27:92–9. [DOI] [PubMed] [Google Scholar]
- [4].Denenberg R. AIDS and women's health—a column to answer your questions. Sidahora 1995;1995:21. [PubMed] [Google Scholar]
- [5].Zhao wenjie, Huang Guoqi Progress on clinical study of acupuncture treatment for chronic pelvic inflammation. Acupunct Tuina (English) 2008;6:251–6. [Google Scholar]
- [6].Fan LL, Yu WH, Liu XQ, et al. A meta-analysis on effectiveness of acupuncture and moxibustion for chronic pelvic inflammatory disease. Zhen Ci Yan Jiu 2014;39:156–63. [PubMed] [Google Scholar]
- [7].Armed Forces Health Surveillance Center (AFHSC). Acute pelvic inflammatory disease, active component, U.S. Armed Forces, 2002–2011. MSMR 2012;19:11–3. [PubMed] [Google Scholar]
- [8].Newkirk GR. Pelvic inflammatory disease: a contemporary approach—includes patient information handout. Am Fam Physician 1996;53:1127–35. [PubMed] [Google Scholar]
- [9].Beerthuizen RJ. Pelvic inflammatory disease in intrauterine device users. Eur J Contracept Reprod Health Care 1996;1:237–43. [DOI] [PubMed] [Google Scholar]
- [10].Balamuth F, Hayes K, Mollen C, et al. The epidemiology of pelvic inflammatory disease in a pediatric emergency department. J Adolesc Health 2012;50:S17–17. [Google Scholar]
- [11].Spanish AI. Chronic pelvic inflammation, clinical aspects & treatment. El Día Médico 1959;31:962. [PubMed] [Google Scholar]
- [12].Peipert JF, Ness RB, Soper DE, et al. Association of lower genital tract inflammation with objective evidence of endometritis. Infect Dis Obstet Gynecol 2000;8:83–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Price MJ, Ades AE, Welton NJ, et al. Pelvic inflammatory disease and salpingitis: incidence of primary and repeat episodes in England. Epidemiol Infect 2017;145:208–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Secord ER. The treatment of acute pelvic inflammation in the female. Can Med Assoc J 1921;11:910. [PMC free article] [PubMed] [Google Scholar]
- [15].Binder I, Ophoven AV. Die Komplexität chronischer Beckenschmerzen am Beispiel der Interstitiellen Zystitis. Aktuelle Urologie 2008;39:289–96. [DOI] [PubMed] [Google Scholar]
- [16].Jones I. A GP's guide topelvic inflammatory disease. Med Today 2004;5:35–42. [Google Scholar]
- [17].Phelan MB, Valley VT, Mateer JR. Pelvic ultrasonography. Emerg Med Clin North Am 1997;15:789. [DOI] [PubMed] [Google Scholar]
- [18].Simhan HN, Caritis SN, Krohn MA, et al. Decreased cervical proinflammatory cytokines permit subsequent upper genital tract infection during pregnancy. Am J Obst Gynecol 2003;189:560–7. [DOI] [PubMed] [Google Scholar]
- [19].Papp JR, Schachter J, Gaydos CA, et al. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae—2014. MMWR Recomm Rep 2014;63:1–9. [PMC free article] [PubMed] [Google Scholar]
- [20].Peters M. Pelvic infection. BMA A-Z Fam Med Encycl 2004;10:264. [Google Scholar]
- [21].Beagley BW. Untreated infections lead to PID and tubal infertility Infections—2002. Fertility Weekly 2010;8:3–4. [Google Scholar]
- [22].Frangenheim H, Kkeindienst W. Chronic pelvic disease of unknown origin. J Reprod Med 1974;13:23–6. [PubMed] [Google Scholar]
- [23].Walker HK, Hall WD, Hurst JW. Pelvic Pain—Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed.1990;Boston: Butterworths, 1–2; Chapter 171. [PubMed] [Google Scholar]
- [24].Johnson RE, Newhall WJ, Papp JR, et al. Screening tests to detect chlamydia trachomatis and neisseria gonorrhoeae infections—2002. Infect Dis Clin Pract 2002;11:1–38. [PubMed] [Google Scholar]
- [25].Peterson HB, Walker CK, Kahn JG, et al. Pelvic inflammatory disease. Key treatment issues and options. JAMA 1992;39:2605. [DOI] [PubMed] [Google Scholar]
- [26].Couce A, Blázquez J. Side effects of antibiotics on genetic variability. FEMS Microbiol Rev 2009;33:531–8. [DOI] [PubMed] [Google Scholar]
- [27].Milingos S, Protopapas A, Kallipolitis G, et al. Endometriosis in patients with chronic pelvic pain: is staging predictive of the efficacy of laparoscopic surgery in pain relief? Gynecol Obstet Invest 2006;62:48. [DOI] [PubMed] [Google Scholar]
- [28].Hassan S, Muere A, Einstein G. Ovarian hormones and chronic pain: a comprehensive review. Pain 2014;155:2448–60. [DOI] [PubMed] [Google Scholar]
- [29].Zhen HL, Wang Y, Liu XJ. Observation on therapeutic effect of warming needle moxibustion on chronic pelvic inflammation of cold-damp stagnation type. Chin Acupunct Moxibustion 2008;28:736. [PubMed] [Google Scholar]
- [30].Zhang MJ, Chu KD, Shi YL. Clinical study on treatment of chronic prostatitis/chronic pelvic pain syndrome by three different TCM principles. Chin J Integr Tradit Western Med 2007;27:989. [PubMed] [Google Scholar]
- [31].Huang YX, Xue SQ. Analysis on the significance of pelvic hemodynamics in efficacy evaluation of TCM treatment for chronic pelvic inflammation. Chin J Integr Tradit Western Med 2007;27:932. [PubMed] [Google Scholar]
- [32].Yuan J, Fang J, Mei LI. Clinical observation on migraine due to hemorheological abnormality in the treatment of acupuncture therapy according to TCM differentiation of syndromes. Hebei J Tradit Chin Med 2004;29:175–9. [Google Scholar]
- [33].Liu WH. TCM acupuncture-moxibustion: contributing to human health. World J Acupunct Moxibustion 2017;27:1. [Google Scholar]
- [34].Pei LI, Yang Q, Chen A. Clinical observation on chronic pelvic inflammation disease treated by enema with traditional Chinese medicine (TCM). J Chengdu Univ Tradit Chin Med 2004;27:14–5. [Google Scholar]
- [35].Wen H, Ren F, Houqian XU, et al. Systemic review of treatment for chronic pelvic inflammatory disease by TCM enema and oral administration of TCM. Western J Tradit Chin Med 2014;27:76–9. [Google Scholar]
- [36].Tang HR, Cheng JX. Curative effect of TCM-WM therapy on secondary infertility due to chronic pelvic inflammatory disease. Matern Child Health Care China 2005;12:1457–8. [Google Scholar]
- [37].Ai-Zhu LI, He F, Huang HM, et al. Curative effect of TCM-WM therapy on chronic pelvic inflammatory disease. Hebei Med 2007;13:45–7. [Google Scholar]
- [38].Hopwood V. Chapter 11—TCM theory in modern medicine. Acupunct Physiother 2004;2004:233–47. [Google Scholar]
- [39].Zheng MF. The guidance of TCM theory to the clinic application of particular points in acupuncture and moxibustion. J Fujian Coll Tradit Chin Med 2004;6:34–6. [Google Scholar]
- [40].Sun Z. A study of relation between rheumatoid arthritis (RA) and blood stasis—the effect of acupuncture promoting blood circulation to remove blood stasis. Acupunct Res 1995;20:71. [PubMed] [Google Scholar]
- [41].Cheng L, Wu K, Qie Z. Role of “qi” in reaching affected area using acupuncture in “promoting blood circulation to remove blood stasis”. Chin J Mod Devel Tradit Med 1990;10:209. [PubMed] [Google Scholar]
- [42].Yang ME, Mao X, Wang PY. Clinical observation of combined acupuncture and herbs in treating chronic pelvic inflammation. Acupuncture and Tuina (English) 2009;7:339–42. [Google Scholar]
- [43].Ozel S, Arslan H, Tufan ZK, et al. Acupuncture in the treatment of chronic pelvic pain secondary to pelvic inflammatory disease. Acupunct Med 2011;29:317–8. [DOI] [PubMed] [Google Scholar]
- [44].Qu F, Zhou J. Treating chronic pelvic inflammation with acupuncture. Oriental Med J 2006;14:18. [Google Scholar]
- [45].Jin Y. Acupuncture with long Dan Xie Gan Tang to treat 36 cases of chronic pelvic inflammation. Geburtshilfe Frauenheilkunde 2007;67:55–7. [Google Scholar]
- [46].Hao X, Niu M, Zheng W, et al. Efficacy comparison between Zhang abdomen acupuncture and traditional acupuncture in treating chronic pelvic inflammatory disease. Chin Arch Tradit Chin Med 2016;34:2016–8. [Google Scholar]
- [47].Shamseer L, Moher D, Clarke M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;350:g7647. [DOI] [PubMed] [Google Scholar]
- [48].Duarte R, Fuhrich D, Ross JD. A review of antibiotic therapy for pelvic inflammatory disease. Int J Antimicrob Agents 2015;46:272–7. [DOI] [PubMed] [Google Scholar]
- [49].Bartley JM, Carrico DJ, Gilleran JP, et al. Chronic pelvic pain in women: common etiologies and management approach recommendations. Clin Pract 2013;10:89–102. [Google Scholar]
- [50].Chen R, Nickel JC. Acupuncture ameliorates symptoms in men with chronic prostatitis/chronic pelvic pain syndrome. Urology 2003;61:1156–9. [DOI] [PubMed] [Google Scholar]
- [51].Honjo H, Kamoi K, Naya Y, et al. Effects of acupuncture for chronic pelvic pain syndrome with intrapelvic venous congestion: Preliminary results. Int J Urol 2004;11:607–12. [DOI] [PubMed] [Google Scholar]
- [52].Posadzki P, Zhang J, Lee MS, et al. Acupuncture for chronic nonbacterial prostatitis/chronic pelvic pain syndrome: a systematic review. J Androl 2012;33:15. [DOI] [PubMed] [Google Scholar]


